Abstract
In this study, hyaluronic acid-functionalized disulfide hollow mesoporous silica nanoparticles (HMSN-NH2-HA) were synthesized as an anticancer drug delivery system. In this regard, hyaluronic acid, a natural ligand for cluster of differentiation-44 (CD44) receptors overexpressed on the surface of tumor cells, was covalently grafted onto the HMSNs. The nanoparticles were characterized using various techniques, such as transmission electron microscopy (TEM), dynamic light scattering (DLS), and Fourier transform infrared spectroscopy (FTIR). Doxorubicin hydrochloride (DOX) was loaded into HMSN-NH2-HA as a model medication. The in vitro drug release was evaluated in different medium conditions and was analyzed by high-performance liquid chromatography. Cellular viability and the localization of nanoparticles were evaluated by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay and confocal microscopy. The in vivo release of DOX in BALB/c mice was investigated by ex vivo images obtained by fluorescence microscopy. The TEM images of HMSNs revealed hollow spheres with an average size of approximately 150 nm. After grafting the HMSNs with hyaluronic acid, the hydrodynamic size of nanoparticles increased to 197 nm, and the zeta potential changed from − 40 to − 18 mV. The half inhibitory concentration (IC50) of HMSN-NH2-HA@DOX and HMSN@DOX for MDA-MB-231 cells after 48 h was 0.32 and 0.21 µg/ml, respectively. Ex vivo biodistribution analysis showed that the tumor-to-nontumor ratio was higher in the HMSN-NH2-HA@DOX group compared to the DOX group. This nanoparticle could provide new opportunities for DOX tumor delivery owing to its biodegradability, controlled release, and targeting behavior.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is reported as the second leading cause of death after cardiovascular diseases. Conventional chemotherapies have various disadvantages, such as the lack of selectivity, multidrug resistance, and poor aqueous drug solubility (Moorthi et al. 2011; Mansoori et al. 2017; Narvekar et al. 2014). In recent years, nano-drug delivery systems have gained growing attention to enhance efficacy and reduce the unwanted side effects of chemotherapies. It should be noted that the disposition and pharmacokinetics of chemotherapy agents might alter after loading into nanoparticles (Fanciullino et al. 2013; Abbasi et al. 2021; Mosleh-shirazi et al. 2021). For instance, pegylated liposomal doxorubicin reduces cardiotoxicity compared to conventional doxorubicin hydrochloride (DOX) formulations. Abraxane, albumin-bound paclitaxel, enhances the solubility of paclitaxel without the need for further traditional solubilizers.
One approach for designing nano-drug delivery systems is to use mesoporous silica nanoparticles (MSNs), which are generally smaller than 200 nm in diameter. The MSNs have been synthesized in different shapes with diverse pore sizes, namely mobile crystalline material (MCM-41) and Santa Barbara Amorphous (SBA-15) (Narayan and Nayak 2018). A variety of compounds, such as small molecules, DNAs, proteins, and even iron oxide nanoparticles, can be carried by MSNs (Narayan and Nayak 2018; Wang et al. 2015; Watermann and Brieger 2017; Hai et al. 2018; Xu et al. 2019). In several studies chitosan (Khoee et al. 2017), alginate sodium (Zhou et al. 2010), hyaluronic acid (Zhang et al. 2016), and poly(2-(diethylamino)ethyl methacrylate) (Sun et al. 2010) have been attached to the surface of the pore entrances of these nanoparticles as gatekeepers to prevent the early leakage of loaded agents (Wen et al. 2017). Surface functionalization may lead to better control of the release rate of the loaded compound due to sensitivity to stimuli, including pH, temperature, redox state, or enzymatic reactions, depending on the nanoparticle design.
Hollow mesoporous silica nanoparticles (HMSNs) are a new generation of MSNs formed using a selective etching method, in which the inner core of MSNs is removed, while the outer shell remains. Both hydrophilic and hydrophobic medications can be loaded on different parts of HMSNs, such as the inner cavity and outer shell, as shown in our previous research (Kabiri et al. 2021). Disulfide-based HMSNs are uniform spherical nanoparticles that can be degraded with intracellular glutathione and specific enzymes called thioredoxins after the endocytosis process (Hadipour Moghaddam et al. 2018). Hyaluronic acid (HA), a linear biocompatible polysaccharide, is a good candidate for designing a targeted drug delivery system, which can bind to cluster of differentiation-44 (CD44) receptors overexpressed in aggressive triple-negative breast cancer cells (Goodarzi et al. 2014, 2011; Saadat et al. 2014; Shabani Ravari et al. 2016). It can also reduce the burst release of the loaded compound in the pore channels of HMSNs to optimize the controlled release delivery system.
The rapid release of hydrophilic medicines, namely DOX from nanocarriers, is one of the downsides of such medications (Zhang et al. 2015). The hydrophilicity of nanoparticles is another essential consideration when administering them intravenously (Fang et al. 2020). It is possible for nanoparticles coated with hydrophilic polymers to remain in blood circulation for many hours (Ramadan et al. 2014). However, the reticuloendothelial system rapidly eliminates hydrophobic nanoparticles (Almalik et al. 2017). With this background in mind, the present study aimed to develop hyaluronic acid-functionalized disulfide hollow mesoporous silica nanoparticles (HMSN-NH2-HA) as a novel drug delivery system for DOX. Moreover, DOX-loaded HMSN-NH2-HA are compared to free DOX regarding in vitro cellular toxicity and ex vivo biodistribution.
Materials and methods
Materials
Tetraethyl orthosilicate (TEOS), bis [3-(triethoxysilyl)propyl] disulfide (BTESPD), cetyltrimethylammonium chloride (CTAC, 25 wt%), triethylamine (TEA), 3-aminopropyltriethoxysilane (APTES), N-hydroxysuccinimide (NHS), 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide hydrochloride (EDC·HCl), sodium chloride, sodium carbonate, sodium hyaluronate (HA) (MW = 25 kDa), 4′,6-diamidino-2-phenylindole dihydrochloride (DAPI), propidium iodide (PI), and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) were purchased from Merck (Germany). Fetal bovine serum (FBS), trypsin–EDTA, RPMI 1640 medium, and annexin V–FITC apoptosis detection kit were purchased from GIBCO (UK) and used as received. MDA-MB-231 (human breast adenocarcinoma) and 4T1 (murine mammary carcinoma) cells were obtained from Pasteur Institute of Iran (Tehran, Iran). Deionized water was used in all experiments.
Preparation of HMSNs
The HMSNs were synthesized based on the sol–gel method, as described previously (Chen et al. 2014). In a round-bottom flask, 35.7 ml of absolute ethanol, 5 ml of deionized water, and 0.8 ml of ammonia solution (0.25 w/v) were mixed. The resultant solution was stirred well at room temperature. Next, 1 ml of TEOS was dropped into the solution. The solution was allowed to react for 1 h; nanoparticles were centrifuged at 21,000 rpm for 17 min and were washed with ethanol and water several times. Finally, nanoparticles were suspended in 20 ml of water. The obtained nanoparticles were added to a mixture of 40 ml of water, 4 g of CTAC, and 54 µl of TEA and were stirred at room temperature for 1 h before the addition of a mixture of 210 µl of TEOS and 90 µl of BTESPD. Afterwards, the mixture was blended for 1 h at 80 \(^\circ\) C to form mesoporous silica-coated SiO2 nanoparticles and was cooled down to 50 °C. The procedure was followed by the addition of 1272 mg of Na2CO3 and constant stirring for 1 h to synthesize HMSNs. The nanoparticles were suspended in a solution of 1% NaCl in methanol. The suspension was stirred at room temperature for 24 h, and the procedure was repeated three times to remove CTAC. The obtained nanoparticles were centrifuged at 21,000 rpm for 17 min and were washed with ethanol and water several times.
Preparation of HMSN-NH2
The nanoparticles obtained from the previous step were dispersed in 30 ml of anhydrous toluene and sonicated before adding 350 µl of APTES and then were refluxed overnight to synthesize HMSN-NH2 nanoparticles. The nanoparticles were thoroughly washed with toluene and ethanol and kept in absolute ethanol for further studies.
Preparation of HMSN-NH2-HA
The HMSN-NH2 nanoparticles (30 mg) were dispersed in 10 ml of deionized water. EDC (52.8 mg) and NHS (97.8 mg) were dissolved in 1.5 ml of deionized water separately and were added to 30 mg of HA aqueous solution (10 ml), followed by stirring at room temperature for 24 h. In the next step, the solution of nanoparticles was well sonicated and added to the activated HA solution. Next, pH was set at 9 with TEA, and the solution was stirred at 38 °C for 24 h. Finally, the HA-grafted HMSNs (HMSN-NH2-HA) were centrifuged at 21,000 rpm for 17 min, washed with water three times, and freeze-dried.
Physicochemical characterization of nanoparticles
Fourier transform infrared (FTIR) spectroscopy of the nanoparticles was characterized by FTIR (PerkinElmer Frontier, UK). The morphology of HMSNs and HMSN-NH2-HA was analyzed by transmission electron microscopy (TEM, JEM-1400, Japan). Nanoparticle suspension was dropped onto a 200-mesh carbon-coated copper grid and was dried at room temperature before the TEM observations. Moreover, a dynamic laser light scattering instrument (DLS, Malvern Instruments Ltd, UK) was used to measure the size and zeta potential of the nanoparticles. Thermogravimetric analysis-derivative thermogravimetry (TGA-DTG) was carried out on a Mettler Toledo Gas Controller GC 100 TGA instrument at a heating rate of 10 °C/min from room temperature to 600 °C under a nitrogen atmosphere. Brunauer–Emmett–Teller (BET) and Barrett-Joyner-Halenda (BJH) measurements were performed to obtain the surface areas and pore-size distributions of HMSNs.
Drug loading and release studies
In this step, 4 mg of HMSN-NH2-HA was dispersed in 2 mg/ml of DOX aqueous solution and was stirred for 72 h in light-sealed vials. Next, DOX-loaded nanoparticles were separated by centrifugation at 10,000 rpm for 10 min and were washed with water. The amount of DOX in the supernatant was determined by validated high-performance liquid chromatography (HPLC). Chromatographic separation was accomplished at room temperature by a C18 column (12.5 cm × 4.6 mm × 5 µm) with a mobile phase of 2% acetic acid and acetonitrile (70%:30% v/v). The UV/visible detector was set at 242 nm, and the flow rate was 1 ml/min.
Drug loading (DL) and Encapsulation efficiency (EE) were determined using Eqs. (1) and (2
The release profile of DOX was evaluated at the pH of 7.2 and 5 in fresh phosphate buffer saline (PBS), simulating the pH of blood and endosomes, respectively. The release profile of DOX was analyzed with the sample and separate method (SS) to simulate the release of an intravenous drug delivery system. One mg of HMSN-NH2-HA@DOX was added to 30 ml of each medium. The suspension remained under constant stirring at 150 rpm and 37 °C. Aliquots were taken at specific time points (1, 3, 6, 24, 30, and 48 h), replaced by fresh PBS, and centrifuged at 10,000 rpm for 20 min. The amount of DOX in the supernatants was measured by HPLC as mentioned above. All measurements were performed in triplicates.
Cellular cytotoxicity
The MTT assay was performed on the MDA-MB-231 human breast adenocarcinoma cell line to assess cytotoxicity. The cells were seeded in a 96-well cell culture plate with a density of 1 × 105 cells per well and were incubated in 5% CO2 at 37 °C for 24 h. After media removal, the cells were treated in four different groups of free DOX, HMSN-NH2-HA, HMSN-NH2-HA@DOX, and control. About 48 h later, 50 µl of 0.5 mg/ml MTT solution was added to each well and was incubated for 4 more hours. Next, the formed formazan crystals were dissolved in 150 µl of DMSO. The plate was agitated for 15 min to ensure the crystals were dissolved fully. Finally, the absorbance of each well was analyzed using a microplate reader at 570 nm, and data were reported as the mean of triplicate. Half inhibitory concentration (IC50) was calculated for MDA-MB-231 cells using the online tool Quest Graph™ IC50 calculator (AAT Bioquest, Inc., Sunnyvale, CA, USA) (Bioquest Inc et al. 2021).
Intracellular localization
The MDA-MB-231 cells were incubated at a density of ~ 1 × 105 cells per well in a six-well plate in DMEM medium with 10% fetal bovine serum (FBS, Gibco, UK) and 1% antibiotics (penicillin–streptomycin, 10,000 U/ml) at 37 °C for 24 h. The cells were treated with 1 ml of free DOX and HMSN-NH2-HA@DOX (1 µg/ml) and were incubated for another 4 h. Afterwards, the medium was removed, cells were washed with 1 ml of PBS several times, fixed with formaldehyde (4%), stained with 500 μl of DMEM containing 50 μl of DAPI, and incubated for 20 min. Finally, the cells were observed with confocal laser scanning microscopy (Nikon C1-si, Japan).
Cellular uptake
The MDA-MB-231 cells were seeded in a six-well plate in a DMEM medium with 10% FBS and 1% antibiotics (penicillin–streptomycin, 10,000 U/ml) at a density of ~ 1 × 105 cells/well. Then, the media were incubated with 1 ml of free DOX and HMSN-NH2-HA@DOX (1 µg/ml). After 4 h, the medium was discarded, and PBS was used for washing the cells. After trypsinization, the cells were collected by centrifugation at 1000 rpm for 5 min and were washed with PBS several times. The fluorescent intensity of MDA-MB-231 cells treated with DOX and HMSN-NH2-HA@DOX was examined by flow cytometry. Untreated cells were used as control cells.
Cell death mechanisms
First, MDA-MB-231 cells were seeded into a 6-well plate at a concentration of 2 × 105 cells per well. Following incubation for 24 h, cells were treated with a solution containing DOX (positive control) or HMSN-NH2-HA@ DOX (1 µg/ml). Afterwards, the culture medium was discarded, and the cells were washed twice with PBS. Based on the previous protocols (Khosravian et al. 2016), and after monolayer trypsinization, the FITC-labeled Annexin V was added to each well. Cells were incubated at room temperature on the shaker (100 rpm) for 15 min in darkness. In the next step, the PI stock solution was added to each well. Finally, the cells were incubated for 5 more minutes and were washed twice with PBS. The cytometric analysis was carried out using the FACSCalibur flow cytometer (Becton Dickinson, USA), and the data were analyzed by the WinMDI 2.9 software.
Biodistribution analysis of DOX
Six female BALB/c mice (25 ± 2 g, 6–8 weeks old) were purchased from the Pasteur Institute of Tehran, Iran. Breast tumors were developed by the subcutaneous injection of 4T1 murine mammary carcinoma cells (4 × 105) into the right shoulder of the mice. After 2 weeks, the mice were divided randomly into two groups (n = 3) of DOX or HMSN-NH2-HA@DOX. Next, 100 µl of 10 mg/kg DOX was injected via tail vein into each group. The mice were sacrificed after 24 h, and the major organs (i.e., liver, spleen, heart, lung, and kidney) and tumor were collected for ex vivo tissue imaging. The samples were fixed and preserved in 10% formalin solution for 24–72 h and were then embedded in paraffin. The tissue specimens were cut into ∼5 μm sections by a microtome and were placed on silane slides. The slides were deparaffined, followed by staining the nuclei with DAPI. After 20 min, the samples were washed with PBS, and glycerol and PBS solution were added. Afterwards, the tissue slices were directly placed in a sample holder, covered with a coverslip, and observed with a fluorescence microscope (Olympus, Japan). Software ImageJ was used to calculate mean fluorescent intensity in the nuclei. Animal experiments are authorized by the Ethics Committee of Tehran University of Medical Sciences.
Statistical analysis
The experiment results are shown as mean ± standard deviation (SD) recorded at least three times for each experiment. All statistical analyses were performed with GraphPad Prism 8 (La Jolla, CA, USA).
Results and discussion
Synthesis and characterization of nanoparticles
In brief, TEOS, BTESPD, and CTAC ionic surfactant were employed to synthesize mesoporous silica shells as the silica precursor, disulfide-containing silica precursor, and stimulators of regular hexagonal formation, respectively. The removal of the inner silica core and cavitation stimulation was accomplished using sodium carbonate. Salt in the methanol mixture was utilized to eliminate surfactant from nanoparticles. Amine-containing HMSNs were created by the chemical reaction between APTES and nanoparticles. Finally, EDC/NHS-activated hyaluronic acid was conjugated to HMSNs. The shape and uniformity of HMSN-NH2-HA were investigated by TEM microscopy. As could be seen in Fig. 1, 2-HA was hollow and spherical with an average size of 200 nm. Following modification with hyaluronic acid, a tiny increase in the outer shell of HMSNs is expected and no noticeable aggregation was observed in the TEM image.
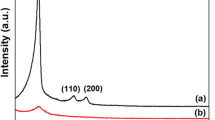
The hydrodynamic size of HMSNs and HMSN-NH2 was 170±5 nm and 184±8 nm, respectively (Fig. 2). The polydispersity index (PDI) was 0.14 and 0.24, showing the narrow size distribution of nanoparticles. The negatively charged surface of hollow mesoporous silica, measured as zeta potential, changed to a positive charge by amine group modification (−40±4 mV vs. +30±5 mV). The hydrodynamic size and zeta potential of HMSN-NH2-HA changed to 197 nm (PDI=0.3) (Fig. 2) and -18±2.5 mV, respectively. The PDI of 0.3 is an indicator of uniform size distribution with sufficient electrostatic repulsion inhibiting aggregation. The charge reversal of nanoparticles showed a successful modification of HMSNs. Furthermore, BET and BJH were used to calculate the specific surface area and pore size distribution of nanoparticles. The BET isotherm showed a typical type IV adsorption-desorption pattern confirming a mesoporous structure. The surface area and BJH pore diameter were 180.43 m2/g and 2.44 nm, respectively. After HA modification, the pore volume decreased from 0.48 to 0.27 m3/g. The HMSN-NH2-HA shows a lower surface area relative to HMSNs because of the presence of HA on its surface.
The FTIR spectrum of unmodified hollow mesoporous silica showed a sharp absorbance peak at 1089 cm-1 and medium peaks at 796 and 466 cm-1, which are attributed to the Si–O–Si stretch of silica and the absorbance peaks at 1637 and 3432 cm-1 assigned to the surface hydroxyl groups of mesoporous silica. The peaks at 2851 and 2921 cm-1 might result from the C-H stretching vibrations of CTAC before CTAC removal from HMSNs. These peaks disappeared after the extraction of CTAC with NaCl/methanol mixture. The propyl group of APTES grafted onto MCM-41 displayed three peaks around 2855, 2925, and 1482 cm-1, which could be assigned to the stretching and bending vibrations of CH in (CH2)3NH2. The NH2 functional group presence leads to a broader band for OH stretching vibration around 3435 cm-1. The signal corresponding to the C=O stretch (amide I) at 1649 cm-1 is related to amide bond formation, indicating that the HA polymer grafting could be merged with the mesoporous silica surface hydroxyl bond (Fig. 3)
In order to determine the amount of hyaluronic acid grafted on the HMSNs surface, TGA was carried out from room temperature to 600 °C under nitrogen flow. The weight difference between HMSNs and HMSN-NH2-HA was about 7%, resulting from functionalization on the surface of disulfide HMSNs (Fig. 4). Hyaluronic acid and organic groups in HMSN-NH2-HA were shown to undergo three main decomposition steps evidenced by exothermic peaks at around 224 °C, 353 °C, and 524 °C in the DTG measurements (inset in Fig. 4)
DOX loading and in vitro release studies
In order to study the loading of DOX in the resulting nanoparticles, the amount of unloaded DOX in the supernatant was measured by HPLC. The EE of HMSN-NH2-HA after 48 and 72 h of mixing was 46.59%±10.25% and 73.47%±8.01%, respectively. The DL of HMSN-NH2-HA after 48 and 72 h of mixing was 17.66%±2.84% and 24.73%±2.8%, respectively. It can be seen that, by increasing the loading time, the amount of EE and DL augmented significantly. On the other hand, after 24 h of incubation, the reduction of doxorubicin in the supernatant was negligible. Therefore, 72 h was selected as the ideal period to load DOX. The release profiles of DOX from HMSN-NH2-HA at the pH of 7.2 and 5 are shown in Fig. 5. The results showed that about 4.05%±0.61% and 8.79%±1.9% of the loaded DOX was released in 48 h at pH = 7.2 and 5 in the PBS, respectively. The latter difference was statistically significant (P < 0.05). In addition, neither of these profiles shows the burst release of DOX under neutral or mildly acidic conditions within 48 h.
The in vitro results indicated that HMSN-NH2-HA is suitable as a drug delivery system for hydrophilic medicines. Although earlier studies suggested that encapsulation should be performed before HA modification, our results showed that hyaluronic acid chains did not act as a barrier to DOX entrapment in HMSNs. While previous research focused on mesoporous cores, our group demonstrated that hollow cores, such as disulfide HMSNs, can have a higher capacity for the loading of hydrophilic medications than solid counterparts. The functionalization of silanol groups with -NH2 does not affect the loading capacity of DOX as a hydrophilic agent. Therefore, it could be concluded that hydrophilic drugs are loaded in the large inner cavity of HMSNs. The latter finding is consistent with the notion that hydrophilic and lipophilic compounds can be loaded in distinct parts, such as the inner cavity or surface of HMSNs, simultaneously (Jahns et al. 2019). The release profile without an initial burst release is preferable for intravenously administered drug delivery systems. The release study verified that DOX molecules were not entrapped in the HA chains and our carrier is a controlled release system.
Cytotoxicity studies
The cytotoxicity of HMSN-NH2-HA in the range of 10–100 µg/ml in MDA-MB-231 cells was evaluated using the MTT assay after incubation for 24 and 48 h. MDA-MB-231 cells were chosen because of being CD44-positive. As shown in Fig. 6, HMSN-NH2-HA had time-dependent and concentration-dependent toxicity against MDA-MB-231 cells, where approximately 79.86% ± 6.62% and 52.35% ± 0.68% of MDA-MB-231 cells were still viable at 100 µg/ml after 24 and 48 h, respectively. The cytotoxicity assays demonstrated that HMSN-NH2-HAs had little toxicity to the cells in the desired concentrations (Shao et al. 2015)
In the next step, the cytotoxicity of DOX (in the range of 0.02–2 μg/ml) and DOX loaded in the nanoparticles (HMSN@DOX and HMSN-NH2-HA@DOX) were compared in MDA-MB-231 cells after 48 h of incubation at 37 °C (Fig. 7). Although the percent viability of MDA-MB-231 cells for DOX and HMSN@DOX was statistically different at higher concentrations, the results showed no significant difference between DOX and HMSN-NH2-HA@DOX in toxicity at different concentrations after 48 h of incubation (Fig. 7). The IC50 of DOX, HMSN@DOX, and HMSNs-NH2-HA@DOX in MDA-MB-231 cells after incubation for 48 h was 0.58, 0.21, and 0.32 µg/ml, respectively, revealing that DOX is less cytotoxic to MDA-MB-231 cells than HMSN@DOX and HMSNs-NH2-HA@DOX.
Comparison of DOX, HMSN@DOX, and HMSN-NH2-HA@DOX toxicity in MDA-MB-231 cells via MTT assay after 48 h. Error bars are the standard deviations of three experiments. Asterisks show a significant difference between the two groups (* and *** were considered P value ≤ 0.05 and P value ≤ 0.001, respectively)
Cellular uptake and subcellular localization
The delivery of DOX into the nucleus is essential for successful antitumor activity, especially when loaded in nanoparticles (Toniolo et al. 2018). The localization of DOX alone and DOX-loaded nanoparticles in MDA-MB-231 cells was examined by confocal microscopy in the present study. As illustrated in Fig. 8, both DOX and DOX loaded in HMSN-NH2-HA were able to be localized into the nuclei of the cells.
The uptake of DOX and HMSN-NH2-HA@DOX in MDA-MB-231 cells was quantified by flow cytometry to confirm the results of confocal microscopy (Fig. 9). The flow cytometry results showed that the same amount of DOX loaded in HMSN-NH2-HA was accumulated in MDA-MB-231 cells after 24 h incubation compared to DOX alone. DOX could be released eventually following the degradation of HMSN-NH2-HA inside the cancer cells (Zhai et al. 2012).
Death mechanisms of MDA-MB-231 cells
The death mechanisms of MDA-MB-231 cells treated with DOX and HMSN-NH2-HA@DOX after 24 h of incubation were evaluated by flow cytometry. The HMSN-NH2-HA@DOX induced early apoptosis, late apoptosis, and necrosis in 15.6%, 5.14%, and 0.28% of the cells, respectively (Fig. 10C). Moreover, DOX induced early apoptosis, late apoptosis, and necrosis in 13.4%, 4.76%, and 0.42% of the cells, respectively (Fig. 10B). The comparison of the results of these two samples with control (Fig. 10A) showed a similarity in the rate of early and late apoptosis for DOX and HMSN-NH2-HA@DOX with the same DOX concentration (0.5 µg/ml) after 24 h of incubation. However, the level of necrosis was negligible.
Evaluation of MDA-MB-231 cells death mechanisms treated with A control, B DOX, and C HMSN-NH2-HA@DOX after incubation for 24 h. The figure represents living cells at the lower left quadrant, early apoptotic cells at the lower right quadrant, late apoptotic cells in the upper right quadrant, and necrotic cells in the upper left quadrant
Endocytosis seemed to play a remarkable role in the entry of nanoparticles into the cells, while uptake could occur through other non-receptor pathways, such as macropinocytosis, especially in the first 24 h of incubation (Hillaireau and Couvreur 2009; Shapero et al. 2011). These findings show that HMSN-NH2-HA does not cause cell membrane rupture and DOX could be released after entering the cells without any influence on its activity.
Biodistribution analysis of DOX
Intrinsic fluorescence of DOX was used for tracking the amount of DOX distributed in the main organs of tumor-bearing mice after the intravenous injection of DOX and DOX@HMSNs-NH2-HA via tail veins. As demonstrated in Fig. 11, at 24 h, the fluorescence signals of DOX in the group of DOX@ HMSNs-NH2-HA in all organs were weaker than that of DOX except in the tumors. In addition, the results of the quantitative analysis showed that the mean fluorescence intensity of tumor tissue in the DOX@ HMSNs-NH2-HA group was 1.3-fold higher than that of DOX and the mean fluorescence intensity of other organs in the DOX@HMSNs-NH2-HA group were approximately ∼0.6 lower than that of DOX at 24 h after injection (Fig. 12). Statistical analysis revealed a significant difference in the fluorescent intensity between two groups in each organ. These findings are supported by other researchers (Ghosh et al. 2021).
According to an earlier study, the phagocytic organs, such as the spleen and liver, are the major sites of the accumulation of MSNs and mesoporous silica/hydroxyapatite nanoparticles (Hao et al. 2015). Our in vivo results revealed that HMSN-NH2-HA@DOX could avoid the reticuloendothelial system and preferentially accumulate in tumors. The mentioned observation was in agreement with the fact that CD44 ligand, HA, enhanced active targeting for CD44-positive cancer cells, namely 4T1 and MDA-MB-231 (Xu et al. 2020).
We found that the renal disposition of HMSN-NH2-HA@DOX is less than DOX at 24 h postinjection. This would be beneficial for delivering anticancer agents via the enhanced permeability and retention effect. Another interesting report illustrated the impact of shape on the fate of intravenously administered nanoparticles. Spherical nanoparticles tend to accumulate in the reticuloendothelial system (RES) organs to a great extent. The number of particles sized 700 nm–3 µm, which can distribute in non-RES organs, declines constantly as the diameter increases. This observation is in good agreement with our results and indicates the influence of size on the biodistribution of nanoparticles (Decuzzi et al. 2010). However, to fully understand the impact of nanoparticles, they should be tracked independently, and the antitumor efficacy of our delivery system can be studied in the future.
Conclusion
A CD44-targeted drug delivery system was successfully prepared by conjugating hyaluronic acid on the surface of disulfide HMSNs. The amount of DOX loaded on HMSN-NH2-HA@DOX was 24.73%±2.8%, and the highest obtained release was 8.79%±1.9% within 48 h (PBS, pH=5). The HMSN-NH2-HA had time-dependent and concentration-dependent toxicity against MDA-MB-231 cells. Limited loading capacity of mesoporous silica nanoparticles and early drug leakage has been expected to pose a severe problem for the rapid transition of MSNs to the pharmaceutical market. The advantage of this system is the ability to carry hydrophilic drugs to breast tumors through intravenous administration. Hyaluronic acid may not only play a role in regulating the release of hydrophilic drugs from HMSNs but also serves as a targeting moiety and increases the biocompatibility of these nanoparticles. The current study highlighted the potential applications of hyaluronic acid-coated HMSNs for drug delivery purposes.
References
Abbasi M, Hafez S, Hadi M, Jamali K, Moeini Z, Jangjou A, Izadpanah P, Mohammad A (2021) Microporous and mesoporous materials mesoporous silica nanoparticle : heralding a brighter future in cancer nanomedicine, microporous mesoporous mater. 319 110967. https://doi.org/10.1016/j.micromeso.2021.110967.
Almalik A, Benabdelkamel H, Masood A, Alanazi IO, Majrashi MA, Alfadda AA, Alghamdi WM, Alrabiah H (2017) Hyaluronic acid coated chitosan nanoparticles reduced the immunogenicity of the formed protein corona. Sci Rep 7(1):1–9. https://doi.org/10.1038/s41598-017-10836-7
AAT Bioquest, Inc, Quest GraphTM IC50 Calc. https://www.aatbio.com/tools/ic50-calculator (accessed July 5, 2021).
Chen F, Hong H, Shi S, Goel S, Valdovinos HF, Hernandez R, Theuer CP, Barnhart TE, Cai W (2014) Engineering of hollow mesoporous silica nanoparticles for remarkably enhanced tumor active targeting. Sci Rep 105. https://doi.org/10.1038/srep05080
Decuzzi P, Godin B, Tanaka T, Lee SY, Chiappini C, Liu X, Ferrari M (2010) Size and shape effects in the biodistribution of intravascularly injected particles. J Control Release 141:320–327. https://doi.org/10.1016/j.jconrel.2009.10.014
Fanciullino R, Ciccolini J, Milano G (2013) Challenges, expectations and limits for nanoparticles-based therapeutics in cancer : a focus on nano-albumin-bound drugs. Crit Rev Oncol / Hematol 88:504–513. https://doi.org/10.1016/j.critrevonc.2013.06.010
Fang J, Islam W, Maeda H (2020) Exploiting the dynamics of the EPR effect and strategies to improve the therapeutic effects of nanomedicines by using EPR effect enhancers. Adv Drug Deliv Rev 157:142–160. https://doi.org/10.1016/j.addr.2020.06.005
Ghosh S, Dutta S, Sarkar A, Kundu M, Sil PC (2021) Targeted delivery of curcumin in breast cancer cells via hyaluronic acid modified mesoporous silica nanoparticle to enhance anticancer efficiency. Colloids Surfaces B Biointerfaces 197:111404. https://doi.org/10.1016/j.colsurfb.2020.111404
Goodarzi N, Ghahremani MH, Amini M, Atyabi F, Ostad SN, ShabaniRavari N, Nateghian N, Dinarvand R (2014) CD44-targeted docetaxel conjugate for cancer cells and cancer stem-like cells: a novel hyaluronic acid-based drug delivery system. Chem Biol Drug Des 83:741–752. https://doi.org/10.1111/cbdd.12288
Goodarzi N, Ghahremani MH, Dinarvand R (2011) Targeting CD44 by hyaluronic acid-based nano drug delivery systems may eradicate cancer stem cells in human breast cancer. Iran J Med Hypotheses Ideas 5 1–5. https://ijmhi.tums.ac.ir/index.php/ijmhi/article/view/115
HadipourMoghaddam SP, Yazdimamaghani M, Ghandehari H (2018) Glutathione-sensitive hollow mesoporous silica nanoparticles for controlled drug delivery. J Control Release 282:62–75. https://doi.org/10.1016/j.jconrel.2018.04.032
Hai L, Jia X, He D, Zhang A, Wang T, Cheng H, He X, Wang K (2018) DNA-functionalized hollow mesoporous silica nanoparticles with dual cargo loading for near-infrared-responsive synergistic chemo-photothermal treatment of cancer cells. ACS Appl Nano Mater 1:3486–3497. https://doi.org/10.1021/acsanm.8b00657
Hao X, Hu X, Zhang C, Chen S, Li Z, Yang X, Liu H, Jia G, Liu D, Ge K, Liang XJ, Zhang J (2015) Hybrid mesoporous silica-based drug carrier nanostructures with improved degradability by hydroxyapatite. ACS Nano 9:9614–9625. https://doi.org/10.1021/nn507485j
Hillaireau H, Couvreur P (2009) Nanocarriers’ entry into the cell: relevance to drug delivery. Cell Mol Life Sci 66:2873–2896. https://doi.org/10.1007/s00018-009-0053-z
Jahns M, Warwas DP, Krey MR, Nolte K, König S, Fröba M, Behrens P (2019) Nanoporous hybrid core–shell nanoparticles for sequential release. J Mater Chem B 8(4):776–786. https://doi.org/10.1039/C9TB01846H
Kabiri F, Mirfakhraee S, Ardakani YH, Dinarvand R (2021) Hollow mesoporous silica nanoparticles for co-delivery of hydrophobic and hydrophilic molecules: mechanism of drug loading and release. J Nanopart Res 23:226. https://doi.org/10.1007/s11051-021-05332-z
Khoee S, Bafkary R, Fayyazi F (2017) DOX delivery based on chitosan-capped graphene oxide- mesoporous silica nanohybride as pH-responsive nanocarriers. J Sol-Gel Sci Technol 493–504. https://doi.org/10.1007/s10971-016-4213-y
Khosravian P, Ardestani MS, Khoobi M, Ostad SN, Dorkoosh FA, Javar HA, Amanlou M (2016) Mesoporous silica nanoparticles functionalized with folic acid/methionine for active targeted delivery of docetaxel. Onco Targets Ther 9:7315. https://doi.org/10.2147/OTT.S113815
Mansoori B, Mohammadi A, Davudian S, Shirjang S, Baradaran B (2017) The different mechanisms of cancer drug resistance : a brief review, Tabriz Univ. Med Sci 7:339–348. https://doi.org/10.15171/apb.2017.041
Moorthi C, Manavalan R, Kathiresan K (2011) Nanotherapeutics to overcome conventional cancer chemotherapy limitations. J Pharm Pharm Sci 14:67–77. https://doi.org/10.18433/j30c7d
Mosleh-shirazi S, Abbasi M, Shafiee M, Reza S, Mohammad A (2021) Renal clearable nanoparticles : an expanding horizon for improving biomedical imaging and cancer therapy. Mater Today Commun 26:102064. https://doi.org/10.1016/j.mtcomm.2021.102064
Narayan R, Nayak UY (2018) Mesoporous silica nanoparticles : a comprehensive review on synthesis and recent advances, 1–49. https://doi.org/10.3390/pharmaceutics10030118
Narvekar M, Xue HY, Eoh JY, Wong HL (2014) Nanocarrier for poorly water-soluble anticancer drugs — barriers of translation and solutions, 15 822–833 https://doi.org/10.1208/s12249-014-0107-x
Ramadan MH, Prata JE, Kara O, Washburn NR (2014) Reducing protein adsorption with polymer-grafted hyaluronic acid coatings. Langmuir 30(25):7485–95. https://doi.org/10.1021/la500918p
Saadat E, Amini M, Khoshayand MR, Dinarvand R, Dorkoosh FA (2014) Synthesis and optimization of a novel polymeric micelle based on hyaluronic acid and phospholipids for delivery of paclitaxel, in vitro and in-vivo evaluation. Int J Pharm 475:163–173. https://doi.org/10.1016/j.ijpharm.2014.08.030
ShabaniRavari N, Goodarzi N, Alvandifar F, Amini M, Souri E, Khoshayand MR, HadavandMirzaie Z, Atyabi F, Dinarvand R (2016) Fabrication and biological evaluation of chitosan coated hyaluronic acid-docetaxel conjugate nanoparticles in CD44+ cancer cells. DARU J Pharm Sci 24:1–12. https://doi.org/10.1186/s40199-016-0160-y
Shao XR, Wei XQ, Song X, Hao LY, Cai XX, Zhang ZR, Peng Q, Lin YF (2015) Independent effect of polymeric nanoparticle zeta potential/surface charge, on their cytotoxicity and affinity to cells. Cell Prolif 48:465–474. https://doi.org/10.1111/cpr.12192
Shapero K, Fenaroli F, Lynch I, Cottell DC, Salvati A, Dawson KA (2011) Time and space resolved uptake study of silica nanoparticles by human cells. Mol Biosyst 7:371–378. https://doi.org/10.1039/c0mb00109k
Sun J, Hong C, Pan C (2010) Fabrication of PDEAEMA-coated mesoporous silica nanoparticles and pH-responsive controlled release. J Phys Chem C 114:12481–12486. https://doi.org/10.1021/jp103982a
Toniolo G, Efthimiadou EK, Kordas G, Chatgilialoglu C (2018) Development of multi-layered and multi-sensitive polymeric nanocontainers for cancer therapy: in vitro evaluation. Sci Rep 8:1–9. https://doi.org/10.1038/s41598-018-32890-5
Wang Y, Zhao Q, Han N, Bai L, Li J, Liu J, Che E, Hu L, Zhang Q, Jiang T, Wang S (2015) Mesoporous silica nanoparticles in drug delivery and biomedical applications, Nanomedicine Nanotechnology. Biol Med 11:313–327. https://doi.org/10.1016/j.nano.2014.09.014
Watermann A, Brieger J (2017) Mesoporous silica nanoparticles as drug delivery vehicles in cancer. Nanomaterials 7. https://doi.org/10.3390/nano7070189.
Wen J, Yang K, Liu F, Li H, Xu Y, Sun S (2017) Diverse gatekeepers for mesoporous silica nanoparticle based drug delivery systems. Chem Soc Rev 46:6024–6045. https://doi.org/10.1039/c7cs00219j
Xu C, Lei C, Yu C (2019) Mesoporous silica nanoparticles for protein protection and delivery. Front Chem 7:290. https://doi.org/10.3389/fchem.2019.00290
Xu H, Niu M, Yuan X, Wu K, Liu A (2020) CD44 as a tumor biomarker and therapeutic target. Exp Hematol Oncol 9:1–14. https://doi.org/10.1186/s40164-020-00192-0
Z P, Guo Y, Wang L, Lv P (2015) Transferrin-conjugated doxorubicin-loaded lipid-coated nanoparticles for the targeting and therapy of lung cancer. Oncol Lett 9(3):1065–1072. https://doi.org/10.3892/ol.2014.2840
Zhai W, He C, Wu L, Zhou Y, Chen H, Chang J (2012) Degradation of hollow mesoporous silica nanoparticles in human umbilical vein endothelial cells. J Biomed Mater Res Part B Appl Biomater 100(5):1397–1403. https://doi.org/10.1002/jbm.b.32711
Zhang J, Sun Y, Tian B, Li K, Wang L, Liang Y, Han J (2016) Multifunctional mesoporous silica nanoparticles modified with tumor-shedable hyaluronic acid as carriers for doxorubicin. Colloids Surf B Biointerfaces 144:293–302. https://doi.org/10.1016/j.colsurfb.2016.04.015
Zhou J, Romero G, Rojas E, Ma L, Moya S, Gao C (2010) Journal of Colloid and Interface Science Layer by layer chitosan / alginate coatings on poly ( lactide-co-glycolide ) nanoparticles for antifouling protection and Folic acid binding to achieve selective cell targeting. J Colloid Interface Sci 345:241–247. https://doi.org/10.1016/j.jcis.2010.02.004
Acknowledgements
This research has received a specific grant from the Tehran University of Medical Sciences (No. 285122). The authors would like to thank the Nanotechnology Research Center, Faculty of Pharmacy, Tehran University of Medical Sciences for their support.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interests in this paper.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mirfakhraee, S., Bafkary, R., Ardakani, Y.H. et al. Synthesis of hyaluronic acid-grafted hollow mesoporous silica nanoparticles as nano-carriers for anticancer drug delivery. J Nanopart Res 24, 100 (2022). https://doi.org/10.1007/s11051-022-05478-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-022-05478-4