Abstract
Background
To investigate the effect of plasma-derived extracellular vesicles (EVs) or conventional medium in fertilization and early embryo development rate in mice.
Methods and results
MII oocytes (matured in vivo or in vitro conditions) were obtained from female mice. The extracellular vesicles were isolated by ultracentrifugation of plasma and were analyzed and measured for size and morphology by dynamic light scattering (DLS) and transmission electron microscopy (TEM). By western blotting analysis, the EVs proteins markers such as CD82 protein and heat shock protein 90 (HSP90) were investigated. Incorporating DiI-labeled EVs within the oocyte cytoplasm was visible at 23 h in oocyte cytoplasm. Also, the effective proteins in the early reproductive process were determined in isolated EVs by western blotting. These EVs had a positive effect on the fertilization rate (P < 0.05). The early embryo development (8 cell, morula and blastocyst stages) was higher in groups supplemented with EVs (P < 0.01).
Conclusion
Our findings showed that supplementing in vitro maturation media with EVs derived- plasma was beneficial for mice’s embryo development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For the first time, Extracellular Vesicles (EVs) were detected 56 years ago in plasma [1]. Other studies found that other biological fluids, such as milk, urine, semen, and follicular fluid, possess these vital and effective particles [2]. The general definition of EVs represents a heterogeneous population of nanovesicles (microvesicles) with < 1000 nm diameter. The EVs are divided into at least three categories: As first, exosomes (EXOs) with a 30–100 nm diameter are released from the fusion of multicellular bodies with the plasma membrane. The second category consist of microvesicles released from a small section of the plasma membrane. While the third category includes apoptotic bodies released from dying cells [3]. Because there are overlaps in the density, cargo, and size of these different nanoparticles, determining the precise type of nanoparticles extracted from different cell types or body fluids is difficult [4]. The typical EVs contain proteins, genetic materials (such as mRNA and DNA), and lipids enclosed by lipid membrane bilayers [5]. Among these vesicles, exosomes can transport molecular cargo a and other biological particles to the recipient cells [6, 7]. These vesicles have recently been recognized as a novel intercellular communication system and play key roles in cellular functions [8]. Today, EVs’ protein particles have been extensively evaluated for their role in triggering signaling cascades in target cells. In recent decades, human and animal infertility has been treated by Assisted Reproductive Technologies (ARTs). ART techniques such as In Vitro Fertilization (IVF) could be an efficient tool for understanding early embryonic development [9]. Despite tremendous improvements in ARTs in recent years, the case of in vitro mammal embryo production development differs from in vivo conditions in the physiologic process [10]. The competence of the female gamete plays a key role in determining the stage of embryonic development [11]. This event can be apprised by its ability to arrive at cytoplasmic maturation together with nuclear maturation [12]. In Vitro Maturation (IVM) of immature oocytes is a necessary technique used in developmental biology and ART research. It is also an impressive treatment that has reported significant results in pregnancy rates [13].
In most mammals and in the IVM process, immature oocytes are collected in an immature Germinal Vesicle (GV) stage from the ovaries in a certain condition. This process allows the re-initiation of the meiotic resumption of oocytes and makes them achieve the meiotic competence stage of Metaphase II (MII). This current IVM media is an unappropriated oocyte maturation in mammal species because, in these conditions, the oocytes stay away from their specific physiological environment, including follicular fluid secretions [14]. Therefore and overall, in vitro development (IVD) after IVF has lower embryonic development than in vivo-derived embryos [15]. Improving embryo culture media is needed to overcome present differences in developmental and quality potential differences between Vitro- and Vivo-derived embryos [16].
Many reproductive proteins (Fig. 1) are effective in fertilization, including various proteins needed to attach to the transparent layer and regulate its glycoprotein structure [17]. The completion of fertilization in mammals requires different membrane fusion in which other membrane proteins are involved. Reproductive physiology-related proteins include myosin 9 (MYH9), annexin A (ANXA) protein family, the tetraspanin membrane protein family (CD9 and CD81), and heat shock protein 8 (HSPA8). These proteins play a vital role (Fig. 1) in sperm and oocyte fertilization [18]. According to recent investigations, EVs have been vital components in regulating gamete or embryo interactions in the oviduct [19]. Emerging pieces of evidence show that EVs-mediated cell-to-cell communication can help oocyte maturation [20], sperm penetration into the oocyte, and embryo development. However, in numerous reports, EVs’ functions in reproductive events have remained unexplored so far [21]. Recent studies imply EVs derived from reproductive tracts play a critical role in gamete maturation and fertilization. Also these vesicles help achieve in vitro embryos with similar development stage levels to in vivo embryos [16].
The schematic diagram of the proposed biological functions of reproductive proteins. These proteins can bind to gametes. Following binding to sperm, they enhance sperm capacitation, motility, and viability. Also, these can increase sperm-egg binding, decrease polyspermy, increase penetration and fertilization rates of sperm, and enhance embryo quality
Blood plasma contains a large amount of protein and essential substances and high concentrations of EVs, such as exosomes [22]. The components of EVs’ protein have been investigated in detail because of their role in signaling cascades. Transporting proteins via EVs may form the bioactivity of target cells in tissues [23]. In recent years, the therapeutic effects of plasma-derived EVs have been observed in various diseases, including cardiac and autoimmune diseases (e.g., rheumatoid arthritis and diabetes) [24]. EV-based treatment significantly reduces inflammation and compared to other treatments, is non-toxic with fewer side effects [25]. Also, some observe that in cardiac disorder, the cardioprotective components could be transferred by these vesicles to cardiomyocyte [24]. In addition, in the previous study, the present authors demonstrated the beneficial role of these EVs in improving oocyte maturation [20]. Because of the similarity of plasma and follicular fluid [26], we hypothesized these EVs may be utilized as a supplement to culture media during the IVM of mice oocytes and IVD stages of mice embryos.
Methods
Study design and embryo culture
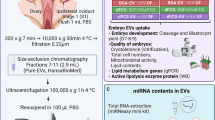
Oocytes were obtained from BALB/c mice (8- to 10-week-old). All mice (n = 7) used in this experiment were purchased from the animal house of the Tabriz University of Medical Sciences. All animals were housed in standard laboratory mice cages and were given food and water ad libitum. Mice were maintained under 12 h light: dark cycle. The implemented methods in the present study were approved by the Tabriz University of Medical Sciences’ Committee on Animal Experimentation (ethics number: IR.TBZMED.VCR.REC.1398.289) and in accordance with the National Institute of Health’s Laboratory Animals Guidelines (8th edition, 2011). After collecting oocytes by rupturing the follicles (n = 440), the following three types of MII stage oocytes of the mouse (Fig. 2) were used: (1) MII stage oocytes matured in vivo (MII oocytes); (2) GV stage oocytes that matured in vitro by EVs supplementation (IVM1oocytes); (3) GV stage oocytes that matured in vitro without EVs supplementation (IVM2oocytes). For MII oocytes retrieval, female mice were superovulated (intraperitoneal) with 10 IU of human menopausal gonadotropin (HMG; NV Organon, The Netherlands), followed by an injection of 10 IU of human chorionic gonadotropin (hCG; NV Organon, The Netherlands) 48 h later. The ovulated oocytes were recovered from oviducts 24 h post-hCG. Then, COCs were washed with PBS. Only mature oocytes (MII stage) were selected under a stereomicroscope (Olympus-Japan). The COCs were washed twice with PBS and then placed into microdrops (25mL) immersed in mineral oil (Sigma Aldrich, USA). The microdropes contained conventional medium (MEM alpha medium) with 75 mg/ ml penicillin (Sigma-Aldrich, USA) and 50 mg/ml streptomycin sulfate (Sigma-Aldrich, USA). The IVM1 and IVM2 oocytes were retrieved following in vitro maturation of GV oocytes under different culture medium conditions, as mentioned in the previous study [20]. Briefly, COCs were released from female mice, and COCs in an immature oocyte were selected for culture. COCs were washed and cultured in microdrop of MEM alpha medium (with penicillin and streptomycin sulfate). The mouse oocytes matured in vitro in the presence (IVM1oocytes) or absence (IVM2oocytes) of EVs.
The schematic representation overview of the experimental design provides the in vitro matured oocytes (IVM1 and IVM2 oocytes) and in vivo matured oocytes (MII oocytes). The matured oocytes were distributed in four groups for In Vitro Fertilization (IVF) supplemented by 10 µg protein/ml plasma-derived extracellular vesicles or without
MII oocytes were fertilized using motile spermatozoa from BALBC mice. Initially, sperm were collected from the cauda epididymis of the male BALBC mice (≥ 9 weeks old) and were selected by swim-up processing. The pellet of sperm cells was re-suspended at fertilization medium (Ham’s F10 medium [Irvine Scientific, Santa Ana, CA]). Then pellets supplemented with 4 mg/ml BSA for capacitation) for 60 min at 37 °C with 5% CO2 humidified atmosphere. After capacitation, sperm was added to a 50 µl microdrop of fertilization medium (Ham’s F10 medium) supplemented with 1 mM pyruvate and 100 µg/ml streptomycin and penicillin. The medium was supplemented with or without EVs considering differential groups for fertilization.
The co-incubation of sets of 20–25 oocytes (total oocytes = 110 per group) with 1.5 ˟ 105 spermatozoa cell mL-1 was performed under equilibrated mineral oil for 20 h at 37 °C with a 5% CO2 humidified atmosphere. IVF was performed in four groups: MII + EVs group: for MII oocytes by EVs supplementation; IVM1 + EVs group: for IVM1oocytes by EVs supplementation; In vivo control group: for MII oocytes without EVs supplementation (only supplemented by conventional medium); In vitro control group: for IVM2oocytes without EVs supplementation (only supplemented by conventional medium) (Fig. 2). Condition medium in IVM1 + EVs and MII + EVs groups was supplemented with EVs (10 µg protein/ml). 24 h after IVF (day 2), the fertilization rate was evaluated based on the number of MII oocytes reaching the 2-cell stage. The early embryo developmental rate was investigated by quantifying the percentages of 8-cell, morula, and blastocyst stages. Developmental rates of the embryo were observed at 44 h (day 3), 74 h (day 4), and day 5 of culture. The development rate was defined as the percentage of embryos that achieved the development scale in relation to the initial count of MII oocytes. 440 oocytes in three IVF replicates were evaluated.
Blood samples collection and EVs extraction
According to the previous methods, small EVs with a size of 30 to 150 nm were collected from plasma [27]. Whole blood samples of the hearts of 3 months old female mice (in proestrus cycle; n = 5) were collected in EDTA Vacutainer tubes (FLmedical, Italy) (Fig. 3A). They were centrifuged (Olympus, Tokyo, Japan) at 1,800 × g for 15 min at 4 °C, and the collected plasma was immediately stored at − 80 °C. The standard procedure of the differential ultracentrifugation method was utilized for EVs extraction. Then, the plasma was diluted (1:4 with PBS) and centrifuged again (Olympus, Tokyo, Japan) (1,000 × g) for 30 min at 4 °C to remove residual cells and then centrifuged (12,000 × g) for 30 min. Afterward, a supernatant was filtered (using a 0.22-µm filter) and ultracentrifuged (Beckman Optima TLX ultracentrifuge, Ramsey, US) (110,000 × g) for 1 h at 4 °C to obtain EVs’ pellets (Fig. 3B). Afterward, the pellets were washed and centrifuged (110,000 × g) for 1 h and then re-suspended in PBS. The EVs’ protein level was evaluated using a bicinchoninic acid protein assay kit (BCA) (Thermo Fisher Scientific, MA, USA).
EVs analysis
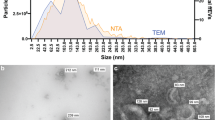
Transmission electron microscopy
The rounded shape and diameter range of the EVs were identified using a Transmission Electron Microscope (TEM, Zeiss, Germany). The 300-mesh grids coated with formvar were exposed to EVs droplets for 12 min at room temperature (RT). The samples were negatively stained by Uranyl Acetate (2%) (UA 2%) and allowed to dry at RT. Then, the grids were observed on a Zeiss 100 kV.
Western blot analysis
Plasma-derived EVs were examined by western blot analysis to investigate the expression of EV-specific protein markers (CD82 and HSP90) and one negative protein marker (Grp94). These EVs’ samples were investigated for proteins with practical function during fertilization, such as MYH9, CD9, HSPA8, and ANXA5.
Santa Cruz Biotechnology (CA, USA) supplied the primary antibodies (anti-CD82, anti-HSP90, anti-MYH9, anti-HSPA8, anti-CD9 and anti-ANXA5 antibodies), and secondary antibodies (mouse anti-rabbit IgG-HRP) for western blotting analysis. The EVs’ samples were lysed for 50 min in the lysis buffer. The supernatants were centrifuged for 10 min. The protein concentration was determined using the BCA protein assay kit. Then, the proteins (25 µg) were loaded into SDS-polyacrylamide gels (10%), electrophoresed, and transferred to polyvinyl difluoride membranes. The membranes were blocked with Bovine Serum Albumin (BSA [3%]) in PBS and incubated with primary antibodies (mentioned above) overnight. After a day, these membranes were washed and then incubated with a secondary antibody for an hour. The blots were developed with a chemiluminescence detection system (Pierce ECL, Thermo Fisher Scientific). Ultimately, immunoreactive bands were scanned utilizing the image j software (Fiji).
Dynamic light scattering size analysis
The size distribution by number, zeta potential, and polydispersity index (PdI) of these vesicles was investigated by Dynamic Light Scattering (DLS) measurements on a Nano Zetasizer ZEN 3600 (Malvern, UK). Dispersion technology software (version 6.01) (Malvern Instruments, UK) was used for analysis. In this method of nanoparticle examination, no sample preparation is required, and the sample is easily measured in the solution. The evaluation of the device is based on the interaction of light with particles, which is the light scattered by the nanoparticles in the suspension that specifies the particle’s diameter. Before measurement, each EV′ sample was sonicated at 4 ° C for 15 min to dissolve the EV aggregates. The samples were diluted in filtered PBS solution a (1: 5 diluted) and then loaded into the cuvette of Nano ZS.
Plasma-derived EVs uptake testing
Plasma-derived EVs were stained by Dil dye (Invitrogen, Paisley, UK). First, 5 µl Dil (1µM Dil) was incubated with 60 µl of total EVs (rehydrated in PBS) for 15 min at 37 °C. The excess dye was removed by centrifugation of labeled EVs at 110,000 g for 60 min. Then, the pellets were washed (twice in PBS). Freshly collected mice COCs were co-incubated in 25 µl droplets of the medium, supplemented by labeled EVs. The oocytes were imaged under a fluorescence microscope (Labomed, NY, USA) after 16, 23, and 30 h of co-incubation at 37 °C.
Statistical analysis
The effect of EV supplementation during fertilization and early embryonic development stages was analyzed by one-way analysis of variance (ANOVA) using version 9 GraphPad analysis software. The assumptions of normality of the residual variances were evaluated using the Shapiro–Wilk test. Variances homogeneity was assessed by the Levene test. The means of the groups were compared at a significance level of p < 0.05. These data came from three replicate experiments.
Results
EVs characterization
Using ultracentrifugation, EVs were isolated from the plasma of female mice. EVs characterizations such as size, morphology, and protein markers were analyzed respectively by Dynamic Light Scattering (DLS), Transmission Electron Microscopy (TEM), and western blotting. TEM results showed EVs in plasma and the round membrane populations and heterogeneous nanovesicles (30–150 nm in diameter) that were determined in the plasma-derived EVs (Fig. 4A). Western blotting was performed in plasma-derived EVs for protein markers (Fig. 4B). Plasma-derived EVs were positive for CD82 and HSP90 proteins recognized exosomal protein markers, and Grp78, an endoplasmic reticulum protein (negative marker). DLS measurements showed an average exosome diameter of 30 and 73 nm. A peak corresponding to diameter was noted at 46.32 nm, and the associated PdI was 0.251. DLS results also revealed a negative zeta potential of -7.86 mV for plasma-derived nanovesicles, indicating the exosome particles’ electric charge (Fig. 4C).
The characterization of plasma-derived extracellular vesicles. (A). Transmission Electron Microscopy (TEM). Rounded nanovesicles were isolated from mice plasma. TEM observations of EVs represented the bilipid layer structures by a single membrane with a 30–100 nm size resembling exosomes. The Arrowheads detect the exosomes. Scale bar = 100 nm. (B). Western blotting analysis. The Western blot assay of EVs protein markers (CD82 and HSP90 antibodies) and negative protein markers (Grp78) in small EVs. The CD82 and HSP90 protein expressions in EVs were indicated by western blotting. (C). Dynamic light scattering measurements. Size-determining results of these nanovesicles represented a peak of heterogeneous populations. Also, the particle size was approximately 39.8 nm (number: 96.8%), and the zeta potential was − 7.85 mV, corresponding to plasma EVs
EVs internalization
EVs’ internalization was evaluated by fluorescence microscopy, and DiI-labeled EVs were incorporated by cumulus cells after 16 h and as mentioned in the previous study [20]. However, EVs’ uptake in the oocyte cytoplasm was not detected after 16 h of culture (Fig. 5A). Incorporating EVs within the oocyte cytoplasm was visible after 23 h incubation (Fig. 5B). Moreover, 30 h after the initiation of IVM, Dil-labeled EVs internalization was detected to be abundant within cells next to the zona pellucida and oocyte cytoplasm (Fig. 5C).
Incorporation of Dil-labeled EVs (red spots) by oocytes (O). (A). EVs, labeled with Dil dye, are seen within the cumulus cells under fluorescent microscopy after 16 h of IVM but not in the oocyte cytoplasm. (B). EVs are incorporated within the cumulus cell mass and into oocyte cytoplasm after 23 h of culture. (C). Oocyte with abundant incorporation of EVs in its cytoplasm and the cells of corona radiata since 30 h of incubation. Arrowheads indicate some aggregation of EVs (A). Scale bar = 50 μm
Differential reproductive protein profile in plasma-derived EVs
Western blotting analysis showed that EVs also expressed reproductive physiology protein (Fig. 6), myosin 9 (MYH9), membrane trafficking process protein (ANXA5), CD9 and Heat Shock Protein 8 (HSPA8). Also, the western blotting EVs protein markers results indicted expression of CD81 and HSP70 proteins (the effective proteins in the reproduction process) in previous study [20].
Developmental competence of MII oocytes
Effects on preimplantation embryos’ developmental stages were identified at the two-cell, eight-cell (Fig. 7A), morula (Fig. 7B) and blastocyst stages (Fig. 7B). A significant increase was observed in the percentage of embryos’ developmental stage using plasma-derived EVs.
The role of treatment conditions (+ EVs or -EVs) in fertilization of mature oocyte (in vivo or in vitro)
Fertilization can be simulated by both types of MII oocyte (matured in vivo or in vitro). Thus, the effects of treatment conditions in the fertilization rate, by quantifying the frequency of 2-cell embryos (among the total MII-stage oocytes) in each group was determined. To evaluate the treatment contribution during insemination, 2-cell-stage embryos (the percentage) related to the total MII-stage oocytes were quantified. It was found that treatment with plasma-derived EVs in the insemination media enhanced the fertilization percentages. As a result, in the IVM1 + EVs and MII + EVs groups, supplementing insemination media with plasma-derived EVs caused a higher fertilization percentage than in their control groups (Fig. 8). Also in similar treatment conditions, the data suggested that the in vivo-matured oocytes reached a higher fertilization outcome than in vitro-matured oocytes. After insemination with spermatozoa, the MII + EVs group showed the highest fertilization percentage than IVM1 + EVs group. The lowest result of fertilization percentages (P < 0.01) was detected in the IVM oocytes of the In vitro control group (Fig. 8).
Preimplantation development of matured oocytes in the presence (+) or absence (-) of Extracellular Vesicles (EVs). The two-cell stage embryos’ percentage (number of embryos at the two-cell stage/number of activated MII oocytes) 24 h after activation. Data indicated the mean ± SEM of at least three independent experiments. The asterisk represents significance (p < 0.05). *** significant at (p < 0.001); **** significant at (p < 0.0001)
The role of treatment conditions (+ EVs or -EVs) in embryo development
To find the effect of treatment conditions methods to embryonic development, the embryo percentages were quantified from each stage (Table 1). The highest embryo development percentage belonged to MII + EVs oocytes in the 8-cell, morula and blastocyst stages (80 ± 1.15%, 61.13 ± 2.99% and 50.65 ± 0.93% respectively). In the IVM1 + EVs group, the 8-cell stage (60 ± 2.88%) was significantly lower than the MII + EVs group. But in the morula and blastocyst stages (53.36 ± 1.26% and 46.11 ± 1.11% respectively) that no difference was noted. The lowest embryo development percentage was observed in the IVM oocytes in the In vitro control group (P < 0.01) (Fig. 9A, B and C).
Supplemented groups by plasma-derived EVs enhanced the developmental potential of embryos (MII + EVs and IVM1 + EVs groups). (A). The embryos’ percentage attaining the eight-cell stage (number of embryos at the eight-cell stage/number of 2-cell stage embryos) 44 h after activation; (B). The embryos’ percentage reaching to the morula stage (number of embryos at the morula stage/number of 2-cell stage embryos) after 74 h of culture. (C). The embryos’ percentage reaching to the blastocyst stage (number of embryos at the blastocyst stage/number of 2-cell stage embryos) after 5 days of culture. * Significant at (p < 0.05); ** significant at (p < 0.01); *** significant at (p < 0.001); **** significant at (p < 0.0001); ns = non-significant
In other words, in the MII oocytes (MII + EVs compared with In vivo control groups), the treatment by plasma-derived EVs during insemination significantly affected embryo development (P < 0.01) (Table 1). In IVM oocytes (IVM1 + EVs compared with In vitro control groups), similar results were achieved for the 8-cell stage, morula and blastocyst stages (Fig. 9). As a result, the absence of plasma-derived EVs treatment decreased embryo development.
In totally, the treatment by plasma-derived EVs effectively increased the percentage of embryo development. It indicated, adding plasma-derived EVs to the IVF media caused the embryos to have more and better development. Despite the difference in MII oocytes no significant difference was observed in the morula and blastocyst stages between the IVM1 + EVs and MII + EVs groups (p > 0.05). The blastocyst stage was reached by 9.18 ± 2.40% of embryos in the In vitro control group and 20 ± 1.15% of those in the In vivo control group (Fig. 9C). Overall, adding plasma-derived exosomes significantly affected fertilization and embryo development percentages after IVF compared to the untreated controls (Table 1).
Discussion
Recently, EVs have been reported as key elements in body fluids, which play a critical role in modulating different signaling pathways and communication among multiple target cells [28]. There is evidence that plasma-derived EVs are strongly involved in treating diseases such as heart failure, hepatic disorder, etc [29]. The results were indicated that the treatment by EVs in IVF protocols can be a valid strategy for improving mouse in vitro embryo production. Following IVF, the percentage of 2-cell embryos was higher IVM1 + EVs group in the compared to the two control groups but lower when compared to the MII + EVs group. According to the earlier study, the percentages of metaphase II oocytes in the IVM condition were significantly higher for EVs’ supplemented group when compared to conventionally matured oocytes. In vitro, EVs’ treatment in embryo culture improves embryo quality in cattle [30]. The previous study demonstrated that sperm-oocyte binding and recognition proteins increased fertilization rate, including CD9 and CD81 [31]. EVs were analyzed for different reproductive proteins, such as reproductive physiology protein (MYH9), membrane trafficking process protein (ANXA5), and a member of the tetraspan membrane proteins family (CD9). Analysis by western blotting showed the presence of MYH9, CD9, HSPA8, and ANXA5 in EVs; which all of these proteins are involved in interactions between gamete-oviduct. OVGP1 and MYH9 in EVs, as critical reproductive proteins, are necessary for both gamete interactions [32]. It was hypothesized that MYH9 could perform these functional results via EVs, possibly by binding to the ZP, and in this way, EVs increase monospermic fertilization. Further experiments are required to detect the vital roles (polyspermy reduction and ZP hardening) of the MYH9-OVGP1 couple. It has been reported that the EVs supplementation (derived-oviduct fluid) of embryo culture improves the blastocyst rate in bovine and murine [33]. Annexins are sperm-binding proteins; in different species responsible for fertilization and arrangement of sperm storage and with this sperm selection, it improves ART [34]. CD9 and CD81 belong to the tetraspanin family and play a vital role in sperm-oocyte interaction and fusion in mice. The CD9-containing EVs are released from the oocyte and facilitate sperm-oocyte fusion by transferring them to the spermatozoa head [35]. The CD81 protein is especially localized in the ZP zone, and the inhibition of CD81 protein expression on the oocyte surface in mice causes a 40% female fertility reduction. According to the studies, HSPA8 increases in vitro sperm viability in bulls and sperm of other animals and improves sperm quality and IVF efficiency [36]. This study hypothesizes that these proteins presented in the plasma-derived EVs could improve sperm-oocyte fusion and with ANXA5 protein, they prevent incomplete interactions between sperm and oocyte.
An interesting point is that despite different maturation methods, the percentage of the morula and blastocyst stages did not show any difference between the IVM1 + EVs and MII + EVs groups. IVF with in vivo-matured oocytes has shown an excellent embryo stage, which might be illustrated by the higher quality of embryos obtained from the in vivo maturation of oocytes. Oocyte meiotic maturation was considered as an oocyte quality control marker. This vital process involves several processes, such as stages of the germinal vesicle, germinal vesicle breakdown, metaphase I, and then metaphase II arrest until fertilization [37]. According to the findings, the percentage of different embryo levels was significantly higher in MII oocytes in the same treatment condition than in IVM oocytes. IVM of oocytes deprives them of the conditions of the normal follicular environment and subsequently reduces developmental levels compared to the in vivo maturation of oocytes [38]. The in vitro spontaneous nuclear resumption maturation prevents oocytes from achieving synchronous nuclear and cytoplasmic maturation [39]. Several differences have been noted in regulating genes between in vivo or in vitro culturing settings of oocytes. In vitro maturation conditions could disturb protein synthesis, increasing gene expression and compensation [40]. Preventing a spontaneous resumption of oocyte nuclear maturation (in vitro) synchronously permits obtaining cytoplasmic and nuclear maturation, which results in increased oocyte developmental competence [39]. Comparing the MII oocyte obtained following superovulation (in vivo) and the IVM oocyte shows that many genes are highly expressed in the IVM oocyte [41]. Failing to acquire the follicular environment probably causes inadequate in vitro maturation conditions. This incompetence has been clarified by poor cytoplasmic maturation of oocytes [42]. Adding EVs in the IVM medium for 24 h changed the resumption of oocyte meiosis more effectively. Also synchronization of oocytes′ nuclear and cytoplasmic maturation consequently occurred and embryonic development increased [43]. The plasma-derived EVs created the typical levels of cytoplasmic and nuclear maturation in oocytes. These particles can mimic the in vivo condition of ovulation and significantly impact on embryo development. The results showed that supplementing IVF condition media with plasma-derived EVs benefited the embryo development of mice.
Conclusion
The results suggested the potential of plasma-derived EVs to be added to IVF media. Further studies on the EVs’ contents could help identify more factors in the EVs that indicate their potential aspects of oocytes, spermatozoa, and embryos.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Wolf P (1967) The nature and significance of platelet products in human plasma. Br J Haematol 13(3):269–288
Foster B, Balassa T, Benen T, Dominovic M, Elmadjian G, Florova V et al (2016) Extracellular vesicles in blood, milk and body fluids of the female and male urogenital tract and with special regard to reproduction. Crit Rev Clini Lab Sci 53(6):379–395
Gutjahr C, Parniske M (2013) Cell and developmental biology of arbuscular mycorrhiza symbiosis. Ann Rev cell Dev Biol 29:593–617
Lötvall J, Hill AF, Hochberg F, Buzás EI, Di Vizio D, Gardiner C et al (2014) Minimal experimental requirements for definition of extracellular vesicles and their functions: a position statement from the Int Soc for Extracell Vesicles. Taylor & Francis, p 26913
Kalra H, Drummen GP, Mathivanan S (2016) Focus on extracellular vesicles: introducing the next small big thing. Int J Mol Sci 17(2):170
Sitar S, Kejžar A, Pahovnik D, Kogej K, Tušek-Žnidarič M, Lenassi M et al (2015) Size characterization and quantification of exosomes by asymmetrical-flow field-flow fractionation. Anal Chem 87(18):9225–9233
Javadi M, Rad JS, Farashah MSG, Roshangar LJRS (2021) An insight on the role of altered function and expression of exosomes and microRNAs in female Reproductive desiease. Reprod Sci 6:1–13
Gholami Farashah MS, Javadi M, Mohammadi A, Soleimani Rad J, Shakouri SK, Roshangar LJMBR (2022) Bone marrow mesenchymal stem cell’s exosomes as key nanoparticles in osteogenesis and bone regeneration: Specific capacity based on cell type 49(12):12203-18
Rizos D, Clemente M, Bermejo-Alvarez P, de La Fuente J, Lonergan P, Gutiérrez‐Adán A (2008) Consequences of in vitro culture conditions on embryo development and quality. Reprod Domest Anim 43:44–50
Lonergan P, Fair TJT (2008) In vitro-produced bovine embryos—dealing with the warts. Thriogenol 69(1):17–22
Krisher RL (2013) In vivo and in vitro environmental effects on mammalian oocyte quality. Annu Rev Anim Bio Sci 1(1):393–417
Demyda S, Genero E (2011) Developmental competence of in vivo and in vitro matured oocytes: a review. Biotech Mol BiolRev 6(7):155–165
Hackney AC (2020) Hypogonadism in exercising males: dysfunction or adaptive-regulatory adjustment? Front in Endocrin 11
Lange-Consiglio A, Perrini C, Albini G, Modina S, Lodde V, Orsini E et al (2017) Oviductal microvesicles and their effect on in vitro maturation of canine oocytes. Reprod 154(2):167–180
DANG-NGUYEN TQ, Somfai T, Haraguchi S, Kikuchi K, Tajima A, Kanai Y et al (2011) In vitro production of porcine embryos: current status, future perspectives and alternative applications. Anim Sci J 82(3):374–382
Gervasi MG, Soler AJ, González-Fernández L, Alves MG, Oliveira PF, Martín-Hidalgo D (2020) Extracellular vesicles, the road toward the improvement of ART outcomes. Anim 10(11):2171
Avilés M, Coy P, Rizos D (2015) The oviduct: a key organ for the success of early reproductive events. Anim Front 5(1):25–31
Tannetta D, Dragovic R, Alyahyaei Z, Southcombe J (2014) Extracellular vesicles and reproduction–promotion of successful pregnancy. Cell Mol Immun 11(6):548–563
Alminana C, Tsikis G, Labas V, Uzbekov R, da Silveira JC, Bauersachs S et al (2018) Deciphering the oviductal extracellular vesicles content across the estrous cycle: implications for the gametes-oviduct interactions and the environment of the potential embryo. BMC Genom 19(1):1–27
Javadi M, Rad JS, Pashaiasl M, Farashah MSG, Roshangar L (2022) The effects of plasma-derived extracellular vesicles on cumulus expansion and oocyte maturation in mice. Reprod Biol 22(1):100593
Machtinger R, Laurent LC, Baccarelli AA (2016) Extracellular vesicles: roles in gamete maturation, fertilization and embryo implantation. Hum Reprod Update 22(2):182–193
Eitan E, Green J, Bodogai M, Mode NA, Bæk R, Jørgensen MM et al (2017) Age-related changes in plasma extracellular vesicle characteristics and internalization by leukocytes. Sci Rep 7(1):1–14
Colombo M, Raposo G, Théry C (2014) Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Ann Rev cell Dev Biol 30:255–289
Vicencio JM, Yellon DM, Sivaraman V, Das D, Boi-Doku C, Arjun S et al (2015) Plasma exosomes protect the myocardium from ischemia-reperfusion injury. J Am Coll Cardio 65(15):1525–1536
Farashah MSG, Javadi M, Rad JS, Shakouri SK, Dastmalchi SAS, Roshangar SNL (2023) Article Title: 17β-Estradiol-loaded exosomes for targeted drug delivery in osteoporosis: a comparative study of two loading methods running title: drug delivery with 17β-Estradiol-loaded exosomes. Ad Pharm Bullet 13:736
Noferesti SS, Sohel M, Hasan M, Hoelker M, Salilew-Wondim D, Tholen E et al (2015) Controlled ovarian hyperstimulation induced changes in the expression of circulatory miRNA in bovine follicular fluid and blood plasma. J Ovarian Res 8(1):1–16
Otani K, Yokoya M, Kodama T, Hori K, Matsumoto K, Okada M et al (2018) Plasma exosomes regulate systemic blood pressure in rats. Biochem Biophys Res Commun 503(2):776–783
Montecalvo A, Larregina AT, Shufesky WJ, Beer Stolz D, Sullivan ML, Karlsson JM et al (2012) Mechanism of transfer of functional microRNAs between mouse dendritic cells via exosomes. Blood J Am Soc Hematol 119(3):756–766
Yang PC (2018) Induced pluripotent stem cell (iPSC)–derived exosomes for precision medicine in heart failure. Circ Res 122(5):661–663
Cebrian-Serrano A, Salvador I, García‐Roselló E, Pericuesta E, Pérez‐Cerezales S, Gutierrez‐Adán A et al (2013) Effect of the bovine oviductal fluid on in vitro fertilization, development and gene expression of in vitro‐produced bovine blastocysts. Reprod Dom Anim 48(2):331–338
de Ferraz AMM, Carothers M, Dahal A, Noonan R, Songsasen M N (2019) Oviductal extracellular vesicles interact with the spermatozoon’s head and mid-piece and improves its motility and fertilizing ability in the domestic cat. Sci Rep 9(1):1–12
Alcântara-Neto A, Fernandez-Rufete M, Corbin E, Tsikis G, Uzbekov R, Garanina A et al (2020) Oviduct fluid extracellular vesicles regulate polyspermy during porcine in vitro fertilisation. Reprod Fertil Dev 32(4):409–418
Qu P, Zhao Y, Wang R, Zhang Y, Li L, Fan J et al (2019) Extracellular vesicles derived from donor oviduct fluid improved birth rates after embryo transfer in mice. Reprod Fertil Dev 31(2):324–332
Teijeiro JM, Munuce MJ, Caille AM, Zumoffen C, Marini PE (2017) Use of annexin V based sperm selection in assisted reproduction
Toshimori K (2011) Dynamics of the mammalian sperm membrane modification leading to fertilization: a cytological study. J Elec Micros 60(suppl1):S31–S42
Moein-Vaziri N, Phillips I, Smith S, Alminana C, Maside C, Gil MA et al (2014) Heat-shock protein A8 restores sperm membrane integrity by increasing plasma membrane fluidity. Reprod 147(5):719–732
Greenstein D (2005) Control of oocyte meiotic maturation and fertilization. The Online Rev of Elegans Biol, WormBook
Combelles CM, Fissore RA, Albertini DF, Racowsky C (2005) In vitro maturation of human oocytes and cumulus cells using a co-culture three-dimensional collagen gel system. Hum Reprod 20(5):1349–1358
Albuz F, Sasseville M, Lane M, Armstrong D, Thompson J, Gilchrist R (2010) Simulated physiological oocyte maturation (SPOM): a novel in vitro maturation system that substantially improves embryo yield and pregnancy outcomes. Hum Reprod 25(12):2999–3011
Zhang H-L, Xu Y, Ju J-Q, Pan Z-N, Liu J-C, Sun S-C (2021) Increased environment-related metabolism and genetic expression in the in vitro matured mouse oocytes by Transcriptome Analysis. Front Cell Dev Biol 9:171
Vanhoutte L, De Sutter P, Van der Elst J, Dhont M (2005) Clinical benefit of metaphase I oocytes. Reprod Biol Endocrin 3(1):1–6
Jones GM, Cram DS, Song B, Magli MC, Gianaroli L, Lacham-Kaplan O et al (2008) Gene expression profiling of human oocytes following in vivo or in vitro maturation. Hum Reprod 23(5):1138–1144
Pioltine EM, Machado MF, da Silveira JC, Fontes PK, Botigelli RC, Quaglio AEV et al (2020) Can extracellular vesicles from bovine ovarian follicular fluid modulate the in-vitro oocyte meiosis progression similarly to the CNP-NPR2 system? Theriogenol 157:210–217
Funding
This study was supported by grants from the Stem Cell Research Center, Tabriz University of Medical Sciences, Tabriz, Iran (Grant Number: 63134).
Author information
Authors and Affiliations
Contributions
Maryam Javadi and Leila Roshangar designed this study. Maryam Javadi and Mohammad Sadegh Gholami Farashah wrote the main manuscript text. Maryam Javadi prepared figures and analyzed the collected data. Jafar Soleimani Rad and Leila Roshangar edited the main text. All authors reviewed the manuscript and replied to revise.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in present study were approved by Tabriz University of Medical Sciences’ Committee on Animal Experimentation, ethical approval number: IR.TBZMED.VCR.REC.1398.289.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Javadi, M., Gholami Farashah, M., Roshangar, L. et al. Plasma-derived extracellular vesicles improve mice embryo development. Mol Biol Rep 51, 621 (2024). https://doi.org/10.1007/s11033-024-09500-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09500-x