Abstract
Background
The therapeutic efficacy of intra-articular mesenchymal stem cells (MSCs) injection for patients with osteoarthritis (OA) currently exhibits inconsistency, and the underlying mechanism remains elusive. It has been postulated that the immunomodulatory properties and paracrine activity of MSCs might be influenced by the inflammatory micro-environment within osteoarthritic joints, potentially contributing to this observed inconsistency.
Methods
Adipose-derived MSCs (ADSCs) were isolated from SD rats and pre-treated with Toll-like receptor 3 (TLR3) agonist Poly I:C or Toll-like receptor 4 (TLR4) agonist LPS. The pre-treated ADSCs were then co-cultured with IL-1β-induced osteoarthritic chondrocytes using a Transwell system to analyze the paracrine effect of ADSCs on reversing the osteoarthritic phenotype of chondrocytes.
Results
RT-PCR and Western blot analysis revealed that Poly I:C and LPS pre-treatments up-regulated the expression of IL-10 and IL-6 in ADSCs, respectively. Furthermore, only Poly I:C-preconditioned ADSCs significantly promoted proliferation while inhibiting apoptosis in IL-1β-treated chondrocytes. Additionally, Poly I:C-preconditioned ADSCs downregulated MMP13 expression while upregulating aggrecan and collagen II expression levels in IL-1β-treated chondrocytes.
Conclusions
TLR3 activation polarizes ADSCs into an immunomodulatory phenotype distinct from TLR4 activation, exerting differential effects on reversing the osteoarthritic phenotype of chondrocytes; thus indicating that MSCs’ paracrine effect regulated by TLRs signaling impacts the efficacy of intra-articular MSCs injection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is characterized by dysfunction of adult articular cartilage and represents the most prevalent form of joint disease. It leads to damage in the articular cartilage, potentially resulting in arthralgia, joint deformation, and limited mobility in patients [1, 2]. Despite the identification of risk factors such as genetics, age, and joint injury associated with OA development, there remains a lack of understanding in the mechanisms of its initiation and progression [3, 4]. It is widely accepted that the inflammatory micro-environment within the joint cavity plays a crucial role in the occurrence and development of OA [5]. In this inflammatory micro-environment, inflammatory cytokines promote chondrocyte activation and induce production of matrix metalloproteinases (MMPs). These MMPs further contribute to degradation of chondrocytes’ extracellular matrix, leading to injury and degeneration of cartilage tissue [6, 7].
With the advancement of regenerative medicine, mesenchymal stem cells (MSCs) hold promising prospects for the regeneration and repair of OA cartilage injuries [8, 9]. Among these approaches, adipose-derived MSCs (ADSCs) offer advantages including easy accessibility, high cell abundance, and robust proliferation capacity [10, 11]. It has been demonstrated that ADSCs can enhance extracellular matrix synthesis of chondrocytes, stimulate their proliferation rate and modulate the inflammatory micro-environment [12, 13]. Consequently, ADSCs hold great potential for regeneration and repair of cartilage injury. However, multiple clinical follow-up studies have indicated that although intra-articular injection of MSCs, including ADSCs, has therapeutic effects such as improving joint function and alleviating pain, there is significant difference in efficacy with an unclear specific mechanism [14,15,16]. This limitation severely hampers their clinical translation. Apart from the heterogeneity of MSCs caused by donor source and in vitro amplification processes [17, 18], the impact of the inflammatory micro-environment on ADSCs immunomodulatory phenotype may be a crucial determinant contributing to changes in clinical efficacy.
The impact of the inflammatory micro-environment following tissue injury on the immunoplasticity of MSCs has been extensively demonstrated, and the adaptive modifications in the immunomodulatory function of MSCs play a pivotal role in regulating inflammation progression and facilitating tissue repair [19, 20]. Further investigations have revealed that the activation of Toll-like receptors (TLRs) on MSCs membranes is a pivotal process influencing their immunoplasticity within the inflammatory micro-environment [21, 22]. Damage-associated molecular patterns (DAMPs) or pathogen-associated molecular patterns (PAMPs) present in this micro-environment induce plastic changes in MSCs’ immunoregulatory functions by activating distinct TLRs [22, 23]. Among these, TLR4 activation leads to polarization of MSCs towards a pro-inflammatory phenotype characterized by IL-6 secretion, while TLR3 activation results in polarization towards an anti-inflammatory phenotype dominated by IL-10 secretion [24]. Additionally, Duan. et al. discovered that pre-treatment of synovial MSCs with a TLR4 agonist led to an upregulation of let-7b-miR content in extracellular vesicles (EVs), resulting in enhanced cartilage repair in mouse models of OA [25]. Li. et al. also demonstrated that pre-treated bone marrow mesenchymal stem cells (BMSCs) with TLR4 agonists increased tumor necrosis factor α-stimulator gene-6 protein content in EVs and significantly enhanced their therapeutic effect [26]. These findings suggest that TLRs activation induces heterogeneous secretion of EVs by MSCs, leading to distinct therapeutic effects. Therefore, we hypothesize that the inflammatory micro-environment of OA may modulate the immunophenotype and paracrine activity of MSCs through TLRs activation, thereby resulting in observed inconsistency in the efficacy of intra-articular MSCs injection.
In this study, our objective was to investigate whether the activation of TLR3 or TLR4 could modulate the immunomodulatory phenotype of ADSCs and exert distinct paracrine effects on reversing the osteoarthritic phenotype of chondrocytes. To achieve this, ADSCs were pre-treated with specific agonists for TLR3 or TLR4 to induce polarization towards an immunomodulatory phenotype. Subsequently, we validated the paracrine effects of these pre-treated ADSCs on reverting the osteoarthritic phenotype of IL-1β-pre-treated chondrocytes using a Transwell co-culture model.
Materials and methods
Cells isolation and characterization
This study was approved by the Laboratory Animal Welfare and Ethics Committee of the Third Military Medical University (AMUWEC20223809). ADSCs and chondrocytes were isolated from 2-week-old SD rats (n = 2, provided by the Third Military Medical University Laboratory Animal Center). After euthanizing the rats, adipose tissue was extracted from the abdomen and subsequently digested using 0.1% collagenase type I (BioFroxx, 1904MG100) to isolate ADSCs. Articular cartilage tissue was extracted from the knee joint and subsequently digested using 0.2% collagenase type II (BioFroxx, 2275MG100) to isolate chondrocytes. Both types of cells were cultured in DMEM/F12 complete medium containing 10% Fetal Bovine Serum (Gibco, 10,091,155) and 1% Penicillin–Streptomycin (Beyotime, C0222) in a CO2 incubator with a concentration of 5% at a temperature of 37 ℃. The medium was changed every other day. The cells were subcultured with trypsin–EDTA solution (Biosharp, BL512A) when they reached approximately 80% confluency. Passage 5 ADSCs and Passage 1 chondrocytes were used for subsequent experiments.
The abilities of osteogenic differentiation, adipogenic differentiation, chondrogenic differentiation of ADSCs were induced using the Rat Adipose-derived Mesenchymal Stem Cells Osteogenic Differentiation Kit (OriCell, RAXMD-90021), the Rat Adipose-derived Mesenchymal Stem Cells Adipogenic Differentiation Kit (OriCell, RAXMD-90031), and the Rat Adipose-derived Mesenchymal Stem Cells Chondrogenic Differentiation Kit (OriCell, RAXMD-90041), respectively. After the induction, the cells were fixed with 4% paraformaldehyde (Biosharp, BL539A), and respectively stained with Alizarin Red, Oil red O, and Alcian Blue.
TLR3 and TLR4 activation in ADSCs
In order to induce the different immunomodulatory phenotype, ADSCs were grown to 90–95% confluence and incubated with Poly I:C (10 μg/mL [27]; Sigma-Aldrich, P0913), or LPS (5 μg/mL [26]; Sigma-Aldrich, L6143) in DMEM/F12 at 37 ℃ for 1 h, respectively. Cells were then washed thoroughly with a complete cell culture medium before being using in the different assays described in the following.
Quantitative real-time PCR
ADSCs were thoroughly washed with PBS, and total RNA was extracted using the TRIzol™ Reagent (Invitrogen, A33250) following the manufacturer’s instructions. The RNA concentration was measured with a NanoDrop 2000 spectrophotometer (Thermo Scientific). cDNA was synthesized using ReverTra Ace® qPCR RT Master Mix (TOYOBO, FSQ-301) and Quantitative real-time PCR (RT-PCR) was performed using TB Green® Fast qPCR Mix (Takara, RR430A) on the CFX96 Connect real-time system (Bio-Rad). GAPDH was regarded as a reference gene, the relative expression level of the mRNAs was computed using the 2−ΔΔCt method. The primer (Sangon Biotech) sequences used for amplification are presented in Table 1.
Western blot
The proteins were harvested from cell lysates using RIPA (Beyotime, P0013B) and the protein concentrations were measured using a BCA protein assay kit (Beyotime, P0010S). Loading buffer (Beyotime, P0015) was added to the cell lysate and boiled at 100 ℃ for 10 min. The lysates were separated on SDS/PAGE (10% gel). The proteins on the gels were transferred to a PVDF membrane (Millipore, 3,010,040,001). The blots were probed with primary antibodies specific to type II collagen (Affinity, AF0135), aggrecan (Affinity, DF7561), MMP-13 (Affinity, AF5355), IL-6 (ZEN-BIOSCIENC, 500,286), IL-10 (ZEN-BIOSCIENC,502,171), β-actin (Affinity, AF7018), and anti-rabbit IgG secondary antibody (Affinity, S0001). The labeled bands were subsequently detected by multi-color fluorescence chemiluminescence imaging system (Vilber). For each sample, band intensities were normalized to β-actin. All experiments were repeated three times.
Co-culture of ADSCs and chondrocytes
To examine the paracrine effect of pre-treated ADSCs on reversing the osteoarthritic phenotype of chondrocytes, five co-culture experimental groups were designed: chondrocytes treated with vehicle (Control group), chondrocytes treated with IL-1β (10 ng/mL, PeproTech, 400-01B, IL-1β group), co-culture of ADSCs and IL-1β treated chondrocytes (IL-1β + ADSC group), co-culture of Poly I:C pre-treated ADSCs with IL-1β treated chondrocytes (IL-1β + ADSCPolyI:C group), co-culture of LPS pre-treated ADSCs with IL-1β treated chondrocytes (IL-1β + ADSCLPS group).
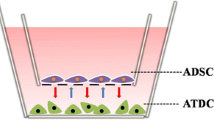
As shown in Fig. 3A, the ADSCs were seeded into the upper chamber of Transwell (NEST, 725,001, 723,001). After pre-treatment described above, the ADSCs were washed with 1 × PBS. Subsequently, the upper chamber was transferred to the plate (NEST, 703,001, 702,001) or confocal dish (NEST, 801,006) containing an equivalent number of chondrocytes for co-culture. The co-culture system was incubated at 37 ℃ in a cell incubator with a CO2 concentration of 5% for a duration of 24 h. For proliferation and immunofluorescence assays, 24-well plates seeded with 1 × 104 chondrocytes/well and 24-well Transwell seeded with 2 × 104 ADSCs/well were used. For the apoptosis and western blot assay, 6-well plates seeded with 1 × 106 chondrocytes/well and 6-well Transwell seeded with 2 × 106 ADSCs/well were used.
Immunofluorescence staining
After co-culture, chondrocytes were fixed in 4% paraformaldehyde (Biosharp, BL539A) at room temperature for 30 min and then blocked with QuickBlock blocking buffer (Beyotime, P0260) for 2 h, and (Beyotime, P0096) for 30 min at room temperature. The cells were incubated with primary antibodies of type II collagen, aggrecan, MMP-13 (all antibody information is as described above) overnight at 4 °C. After thorough washing, the cells were incubated with secondary antibodies (Alexa Fluor 488-labeled Goat Anti-Rabbit IgG (H + L)) (Beyotime, A0423) for 90 min at room temperature. The nucleus was co-stained with DAPI Staining Solution (Beyotime, C1005) for 10 min at room temperature. Next, the cells were observed using the Laser confocal microscope (ZEISS LSM780). The relative fluorescence unit was analyzed using ZEN software (version 2012). Three randomly selected images of each group were used for statistical analysis (total fluorescence intensity of target protein/number of nuclei).
Assays for cell proliferation and apoptosis
After co-culture, the CCK8 reagent (Beyotime, C0037) was added to the culture system. After a 2-h incubation period in a 5% CO2 incubator at 37 ℃, cell proliferation was assessed by measuring the absorbance at 450 nm using a microplate reader (Thermo Fisher Scientific). For apoptotic analysis, cells were washed with ice-cold PBS (Biosharp, BL302A) and subsequently detached using 0.25% Trypsin–EDTA (Gibco, 25,300,120). The cells were then collected by centrifugation at 4 °C, resuspended in ice-cold PBS. Subsequently, Annexin V-FITC and Propidium Iodide (Absin, abs50001) were added following the provided instructions. Next, the cells were analyzed using flow cytometry (BD LSRFortessa™).
Statistical analysis
Data were expressed as mean ± SD by using GraphPad prism software (version 9.0). All samples were repeated three times. Two different groups were compared by independent-sample t-test, and multiple group comparisons were performed by one way ANOVA with Tukey’s post hoc test. The statistical significance among multiple ranked data was analyzed by Kruskal–Wallis test and Nemenyi test. In all cases, results were considered statistically significant when P < 0.05.
Results
Isolation and identification of ADSCs
The process of isolating ADSCs from the abdominal adipose tissue of rats is illustrated in Fig. 1A. The multi-directional differentiation potential of ADSCs was demonstrated by Alizarin Red staining for osteogenic induction, Oil Red O staining for adipogenic induction, and Alcian Blue staining for chondrogenic induction. It was observed that osteogenically-induced ADSCs (Fig. 1B), adipogenically-induced ADSCs (Fig. 1C), and chondrogenically-induced ADSCs (Fig. 1D) exhibited distinct positive staining characteristics.
ADSCs exhibit distinct immunomodulatory phenotypes after being pre-treated with Poly I:C or LPS
Following the aforementioned protocol, ADSCs were respectively pre-treated with TLR3 agonists Poly I:C or TLR4 agonists LPS. The cells displayed typical fibroblastic shape regardless of pre-treatment as shown in Fig. 2A. PCR results demonstrated that compared with the control group, pre-treatment with Poly I:C resulted in an up-regulation of TLR3 (P < 0.0001) and IL-10 (P < 0.0001) expression in ADSCs, while having no impact on the expression of TLR4 (P > 0.05) and IL-6 (P > 0.05). On the other hand, pre-treatment with LPS up-regulated the expression of TLR4 (P < 0.0001) and IL-6 (P < 0.0001), down-regulated the expression of TLR3 (P < 0.05), while had no impact on the expression of IL-10 mRNA (P > 0.05) (Fig. 2B, C).
The ADSCs exhibit polarization into anti-inflammatory or pro-inflammatory immunomodulatory phenotypes following pre-treatment with Poly I:C or LPS. A ADSCs represented fibroblastic morphology after pre-treatment with Poly I:C or LPS. Scale bar = 200μm B Relative expressions of TLR3, TLR4, IL-6, IL-10 determined by RT-PCR. ***P < 0.001, ****P < 0.0001. C Western blot of IL-6 and IL-10, and semi-quantitative analysis of IL-6 (D), IL-10 (E). *P < 0.05, **P < 0.01
The validation was further reinforced through Western blot results (Fig. 2D). Western blot data indicated that compared with the control group, the protein level of IL-10 was significantly up-regulated (P < 0.01) in ADSCs pre-treated with Poly I:C, while IL-6 was not significantly up-regulated (P > 0.05). In addition, compared with the control group, the expression of IL-6 was significantly up-regulated(P < 0.01) in ADSCs pre-treated with LPS, while IL-10 was not significantly up-regulated (P > 0.05) (Fig. 2E, F). These results indicated that Poly I:C pre-treatment induced TLR3 activation and promoted the polarization of ADSCs towards an anti-inflammatory immunoregulatory phenotype characterized by IL-10 secretion, while LPS pre-treatment induced TLR4 activation and promoted the polarization of ADSCs towards a pro-inflammatory immunoregulatory phenotype characterized by IL-6 secretion.
ADSCs pre-treated with LPS or Poy I:C exhibit distinct effects on apoptosis inhibition and proliferation promotion in IL-1β-treated chondrocytes
The ADSCs were pre-treated with either Poly I:C or LPS, and subsequently co-cultured with IL-1β-induced osteoarthritic chondrocytes for 24 h, as shown in Fig. 3A. The data from the CCK8 experiment revealed that IL-1β exerted a substantial inhibitory effect on the proliferation of chondrocytes (P < 0.0001). Both the ADSCs and the Poly I:C-pre-treated ADSCs displayed a remarkable enhancement in the rate of chondrocyte proliferation (all P < 0.0001), while the LPS-pre-treated ADSCs failed to stimulate such growth (P > 0.05). Notably, compared with the ADSCs, the Poly I:C-pre-treated ADSCs exhibited a more pronounced promotion of chondrocyte proliferation (P < 0.01) (Fig. 3B).
The ADSCs pre-treated with LPS or Poly I:C exhibit distinct effects on inhibiting apoptosis and promoting proliferation in IL-1β-induced chondrocytes. A Flowchart of co-culture. B Effects of ADSCs pre-treated with LPS or Poy I:C on cell proliferation rate of chondrocytes. ****P < 0.0001, compared with the IL-1β group. ##P < 0.01, compared with the IL-1β + ADSC group. C, D Effect of ADSCs pre-treated with LPS or Poy I:C on apoptosis of chondrocytes was detected by flow cytometry and the result of statistical analysis (D)****P < 0.0001, compared with the IL-1β group. #P < 0.05, compared with the IL-1β + ADSC group. The different colors of the bar chart represent group information, respectively
The results of apoptotic analysis demonstrated that IL-1β significantly augmented the proportion of apoptotic chondrocytes (P < 0.0001). Both the ADSCs and the Poly I:C-pre-treated ADSCs exhibited effective reduction in the proportion of apoptotic chondrocytes (all P < 0.0001), whereas the LPS-pre-treated ADSCs did not exhibit such an effect (P > 0.05). The Poly I:C-pre-treated ADSCs exhibited a superior capacity in suppressing chondrocyte apoptosis when compared with the ADSCs. (P < 0.05) (Fig. 3C, D).
LPS or Poy I:C pre-treated ADSCs exert distinct effects on reversing osteoarthritic phenotype of IL-1β treated chondrocytes
The expression of MMP13, aggrecan, and collagen II serves as indicators for catabolic and anabolic processes in cartilage degradation, enabling the assessment of osteoarthritic phenotype of chondrocytes [28]. Immunofluorescence results demonstrated that IL-1β stimulation significantly increased MMP13 expression in chondrocytes, and simultaneously reducing the expression of aggrecan and collagen II (all P < 0.0001). Co-culture with the ADSCs effectively suppressed MMP13 expression (P < 0.001) and upregulated aggrecan (P < 0.01) and collagen II (P < 0.01) expression compared with the IL-1β group; more pronounced effects in downregulating MMP13 expression was observed when the ADSCs were pre-treated with Poly I:C (P < 0.05), as well as upregulating aggrecan (P < 0.01) and collagen II (P < 0.01) expression compared with the IL-1β + ADSC group. Conversely, LPS-pre-treated ADSCs only exhibited a decrease in MMP13 expression (P < 0.05), without a significant enhancement in aggrecan and collagen II levels compared with the IL-1β group (Fig. 4).
Immunofluorescence detection of MMP13, aggrencan and collagen II expressions in IL-1β-induced chondrocytes following co-culture with ADSCs pre-treated with LPS or Poly I: C. ADSCs were seeded at a density of 2 × 104 cells/well in Transwell. Chondrocytes were seeded at a density of 1 × 104 cells/well in the confocal dish. A Representative immunofluorescence images of MMP13(yellow), Aggrencan (green) and Collagen II (Orange). Nuclei were stained with DAPI (blue). Scale bar = 10μm. Three fields were randomly selected from each sample for quantification. All experiments were repeated independently at least three biological replicates. B–D Relative expression level of MMP13 (B), Aggrecan (C), Collagen II (D). *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001, compared with the IL-1β group. #P < 0.05, ##P < 0.01, compared with the IL-1β + ADSC group. The different colors of the bar chart represent group information, respectively
Western blot results also demonstrated that LPS-pre-treated ADSCs were unable to effectively reverse the up-regulation of MMP13 and down-regulation of aggrecan and collagen II in chondrocytes induced by IL-1β (all P < 0.0001). Compared to the IL-1β group, Compared to the IL-1β group, co-culture with the ADSCs resulted in a reduction in MMP13 expression (P < 0.05), an increase in aggrecan expression (P < 0.01), but did not restore collagen II expression (P > 0.05).In contrast, Poly I:C-pre-treated ADSCs exhibited a more significant inhibition in MMP13 expression (P < 0.05), and more significantly increased expression of both aggrecan (P < 0.001) and collagen II (P < 0.001) when compared with the ADSCs (Fig. 5).
Protein expression levels of MMP13, aggrencan and collagen II in IL-1β-induced chondrocytes following co-culture with ADSCs pre-treated with LPS or Poly I: C. ADSCs were seeded at a density of 2 × 106 cells/well in Transwell. Chondrocytes were seeded at a density of 1 × 106 cells/well in the 6-well plate. A Representative Western blot of MMP13, aggrecan, collagen II. β-actin was served as a loading control for western blots (MMP13, aggrecan, collagen II). B–D Relative expression level of MMP13 (B), aggrecan (C), collagen II (D). All experiments were repeated independently at least three biological replicates. *P < 0.05, **P < 0.01, ****P < 0.0001, compared with the IL-1β group. #P < 0.05, ###P < 0.001, compared with the IL-1β + ADSC group. The different colors of the bar chart represent group information, respectively
Discussion
In this study, we observed that the activation of TLR3, rather than TLR4, augmented the capacity of ADSCs in reversing the osteoarthritic phenotype of chondrocytes in vitro. This finding implies that the inflammatory micro-environment in osteoarthritic joint modifies the immunomodulatory phenotype and paracrine effects of MSCs through TLRs signaling pathways, thereby influencing the therapeutic efficacy of intra-articular MSC injection.
MSCs are derived from the mesoderm during embryonic development and represent a population of adult stem cells characterized by their capacity for self-renewal and ability to differentiate into multiple cell lineages [29, 30]. According to the definition provided by the International Association of Cell Therapy, the morphology of MSCs resembles that of fibroblasts, and they can be induced to undergo osteogenic, adipogenic, and chondrogenic differentiation under specific conditions [31, 32]. Our obtained ADSCs also meet these criteria (Fig. 1). Moreover, MSCs have the capability to synthesize, endogenously express, and secrete an extensive range of bioactive molecules including growth factors, cytokines, regulatory factors, signal peptides, and extracellular vesicles like exosomes. These bioactive molecules play important roles in mediating paracrine effects on adjacent cells, thereby influencing their biological processes [33, 34]. There have been quite a few studies on the paracrine effects of MSCs. For example, Ling et al. discovered that FGF2, IGF-1, HGF, and other bioactive factors were detectable in the conditioned medium of human amniotic MSCs cultured in vitro. Furthermore, administration of the conditioned medium demonstrated a reduction in ovarian damage in rats compared with that observed with direct injection of human amniotic MSCs [35]. Similarly, Chen et al. demonstrated that hydrogels incorporating conditioned medium derived from human umbilical cord MSCs effectively enhanced the viability of injured human umbilical vein endothelial cells and human skin fibroblasts in vitro, as well as promoted re-epithelialization, collagen deposition, and angiogenesis in rat models of type I and type II diabetic foot ulcers, compared with hydrogels loaded with human umbilical cord MSCs [36]. In our study, we employed the advantage of the Transwell system in facilitating indirect intercellular communication through micropores in the semipermeable membrane to effectively observe the paracrine effect of ADSCs on chondrocytes (Fig. 3A).
The occurrence of OA is accompanied by the emergence of an inflammatory micro-environment, and persistent chronic inflammation serves as the pivotal factor that promotes further degeneration of articular cartilage [37]. Within this micro-nvironment, TLRs play a critical role in the early detection and promotion of adaptive immunophenotypic transformation of MSCs, with TLR3 and TLR4 being the most extensively investigated [38, 39]. Vega-Letter et al. demonstrated that pre-treatment of BMSCs with the TLR3 ligand Poly I:C resulted in a decrease in the differentiation and activation of Th1 and Th17 lymphocytes, indicating an anti-inflammatory phenotype. Conversely, pre-treatment of BMSCs with the TLR4 ligand LPS promoted CD3+ T cell proliferation and enhanced the differentiation of Th1 and Th17 cells, exhibiting a pro-inflammatory phenotype [40]. Additionally, the study conducted by Gadi et al. revealed that neuropeptide pituitary adenylyl cyclase activating peptide could activate TLR3 and induce BMSCs to secrete higher levels of anti-inflammatory factors such as IL-2, IL-3, IL-4, IL-27, IP10, IL-1Ra, RANTES, SDF-1, CCL2, CCL-1 and G-CSF. Conversely, pro-inflammatory factors, including IL-17α, IL-1α and soluble ICAM-1, were down-regulated in response to this activation process, resulting in the promotion of an anti-inflammatory phenotype [41]. However, it is worth noting that the condition of TLRs activation might vary the immunomodulatory phenotype of MSCs. Flavio et al. observed that exposure of BMSCs to LPS (500 ng/mL) for 1 h resulted in decreased levels of NO/iNOS and attenuated immunosuppressive capacity. However, following a 48-h exposure to LPS (500 ng/mL), BMSCs exhibited significantly enhanced immunosuppressive ability on T cell proliferation and increased Tregs [42]. Our findings confirmed that activation of TLR3 enhanced the secretion of the anti-inflammatory cytokine IL-10 by ADSCs, indicating an anti-inflammatory phenotype. In contrast, activation of TLR4 promoted the secretion of the pro-inflammatory cytokine IL-6 by ADSCs, demonstrating a pro-inflammatory phenotype. Although the detailed cytokine expression pattern needs further investigation, the obtained results are in line with previous studies, providing support for the effective implementation of our pre-treatment protocol to activate either TLR3 or TLR4 and induce distinct immunomodulatory phenotypes in ADSCs (Fig. 2).
MSCs therapy has emerged as extensive research in the field of regenerative medicine. Autologous and allogeneic MSCs derived from various tissues have shown minimal adverse reactions in the treatment of OA, demonstrating promising potential for alleviating clinical symptoms and facilitating cartilage regeneration [43]. However, there is considerable inconsistency in the therapeutic effect of intra-articular MSCs injections across different studies [18]. Chahal et al. reported that single intra-articular injection of autologous BMSCs improved the symptoms of patients with OA [44], while Matas et al. suggested that symptom improvement of multiple injections was superior to single injection [45]. Our findings indicated that TLR3-activated ADSCs enhanced efficacy by promoting proliferation, inhibiting apoptosis, and reversing the osteoarthritis phenotype of chondrocytes. This observation indicated that, in addition to injection dosage and MSCs lineages, modification in paracrine action by TLRs could be a crucial factor contributing to the uncertain efficacy of MSCs upon their introduction into the joint cavity. However, it is important to note that the therapeutic outcome of intra-articular MSCs injections also depends on chondrogenic differentiation of MSCs. Fu et al. discovered that factors secreted by osteoarthritic cartilage promoted chondrogenic differentiation of human infrapatellar fat pad MSCs [46]. The study conducted by Ma et al. demonstrated that EVs derived from articular chondrocytes augmented the chondrogenic differentiation of human umbilical cord MSCs through the induction of autophagy [47].These findings suggested that crosstalk between osteoarthritic chondrocytes and MSCs might also influence the therapeutic outcome of intra-articular MSCs injections and require further investigation.
Conclusion
In summary, our study demonstrated that activation of TLR3 and TLR4 in vitro resulted in modifications to the immunomodulatory phenotype of ADSCs, exhibiting distinct effects on reversing the osteoarthritic phenotype of chondrocytes. These findings suggest that activation of TLRs can induce alterations in the immunomodulatory phenotype and paracrine effects of MSCs within the inflammatory micro-environment of OA. The observation we present here have significant implications for investigating the relationship between phenotypic regulation and functional aspects of MSCs, and also provide a very meaningful reference for stabilizing and improving the efficacy of MSCs therapy for OA in the future.
Data availability
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
References:
Katz JN, Arant KR, Loeser RF (2021) Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA, J Am Med Assoc 325(6):568–578. https://doi.org/10.1001/jama.2020.22171
Safiri S, Kolahi A, Smith E, Hill C, Bettampadi D, Mansournia MA, Hoy D, Ashrafi-Asgarabad A, Sepidarkish M, Almasi-Hashiani A, Collins G, Kaufman J, Qorbani M, Moradi-Lakeh M, Woolf AD, Guillemin F, March L, Cross M (2020) Global, regional and national burden of osteoarthritis 1990–2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis 79(6):819–828. https://doi.org/10.1136/annrheumdis-2019-216515
Abramoff B, Caldera FE (2020) Osteoarthritis. Med Clin North Am 104(2):293–311. https://doi.org/10.1016/j.mcna.2019.10.007
Quicke JG, Conaghan PG, Corp N, Peat G (2022) Osteoarthritis year in review 2021: epidemiology & therapy. Osteoarthritis Cartilage 30(2):196–206. https://doi.org/10.1016/j.joca.2021.10.003
Sanchez-Lopez E, Coras R, Torres A, Lane NE, Guma M (2022) Synovial inflammation in osteoarthritis progression. Nat Rev Rheumatol 18(5):258–275. https://doi.org/10.1038/s41584-022-00749-9
Labinsky H, Panipinto PM, Ly KA, Khuat DK, Madarampalli B, Mahajan V, Clabeaux J, Macdonald K, Verdin PJ, Buckner JH, Noss EH (2020) Multiparameter analysis identifies heterogeneity in knee osteoarthritis synovial responses. Arthritis Rheumatol 72(4):598–608. https://doi.org/10.1002/art.41161
Zheng L, Zhang Z, Sheng P, Mobasheri A (2021) The role of metabolism in chondrocyte dysfunction and the progression of osteoarthritis. Ageing Res Rev 66:101249. https://doi.org/10.1016/j.arr.2020.101249
Naji A, Eitoku M, Favier B, Deschaseaux F, Rouas-Freiss N, Suganuma N (2019) Biological functions of mesenchymal stem cells and clinical implications. Cellular and molecular life sciences : CMLS 76(17):3323–3348. https://doi.org/10.1007/s00018-019-03125-1
Xu X, Xu L, Xia J, Wen C, Liang Y, Zhang Y (2023) Harnessing knee joint resident mesenchymal stem cells in cartilage tissue engineering. Acta Biomater 168:372–387. https://doi.org/10.1016/j.actbio.2023.07.024
Lee WS, Kim HJ, Kim KI, Kim GB, Jin W (2019) Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: a phase iib, randomized, placebo-controlled clinical trial. Stem Cells Transl Med 8(6):504–511. https://doi.org/10.1002/sctm.18-0122
Song Y, Wang N, Shi H, Zhang D, Wang Q, Guo S, Yang S, Ma J (2023) Biomaterials combined with adscs for bone tissue engineering: current advances and applications. Regen. Biomater. 10:rbad83. https://doi.org/10.1093/rb/rbad083
Bhattacharjee M, Escobar IJ, Kan HM, Shah S, Otsuka T, Bordett R, Barajaa M, Nagiah N, Pandey R, Nair LS, Laurencin CT (2022) Injectable amnion hydrogel-mediated delivery of adipose-derived stem cells for osteoarthritis treatment. Proc Natl Acad Sci U S A 119(4):e2120968119. https://doi.org/10.1073/pnas.2120968119
Yan B, Lv S, Tong P, Yan L, Chen Z, Zhou L, Yuan Q, Guo L, Shan L (2022) Intra-articular injection of adipose-derived stem cells ameliorates pain and cartilage anabolism/catabolism in osteoarthritis: preclinical and clinical evidences. Front Pharmacol 13:854025. https://doi.org/10.3389/fphar.2022.854025
Hwang JJ, Rim YA, Nam Y, Ju JH (2021) Recent developments in clinical applications of mesenchymal stem cells in the treatment of rheumatoid arthritis and osteoarthritis. Front Immunol 12:631291. https://doi.org/10.3389/fimmu.2021.631291
Wei P, Bao R (2022) Intra-articular mesenchymal stem cell injection for knee osteoarthritis: mechanisms and clinical evidence. Int J Mol Sci 24(1):59. https://doi.org/10.3390/ijms24010059
Copp G, Robb KP, Viswanathan S (2023) Culture-expanded mesenchymal stromal cell therapy: does it work in knee osteoarthritis? A pathway to clinical success. Cell Mol Immunol 20(6):626–650. https://doi.org/10.1038/s41423-023-01020-1
Galipeau J, Sensébé L (2018) Mesenchymal stromal cells: clinical challenges and therapeutic opportunities. Cell Stem Cell 22(6):824–833. https://doi.org/10.1016/j.stem.2018.05.004
Zhou T, Yuan Z, Weng J, Pei D, Du X, He C, Lai P (2021) Challenges and advances in clinical applications of mesenchymal stromal cells. J Hematol Oncol 14(1):24. https://doi.org/10.1186/s13045-021-01037-x
Theeuwes WF, van den Bosch MHJ, Thurlings RM, Blom AB, van Lent PLEM (2021) The role of inflammation in mesenchymal stromal cell therapy in osteoarthritis, perspectives for post-traumatic osteoarthritis: a review. Rheumatology (Oxford) 60(3):1042–1053. https://doi.org/10.1093/rheumatology/keaa910
Liu X, Zhou Z, Zeng WN, Zeng Q, Zhang X (2023) The role of toll-like receptors in orchestrating osteogenic differentiation of mesenchymal stromal cells and osteoimmunology. Front Cell Dev Biol 11:1277686. https://doi.org/10.3389/fcell.2023.1277686
Abdi J, Rashedi I, Keating A (2018) Concise review: tlr pathway-mirna interplay in mesenchymal stromal cells: regulatory roles and therapeutic directions. Stem cells (Dayton, Ohio) 36(11):1655–1662. https://doi.org/10.1002/stem.2902
Shirjang S, Mansoori B, Solali S, Hagh MF, Shamsasenjan K (2017) Toll-like receptors as a key regulator of mesenchymal stem cell function an up-to-date review. Cell Immunol 315:1–10. https://doi.org/10.1016/j.cellimm.2016.12.005
Li Y, Huang L, Cai Z, Deng W, Wang P, Su H, Wu Y, Shen H (2019) A study of the immunoregulatory function of tlr3 and tlr4 on mesenchymal stem cells in ankylosing spondylitis. Stem Cells Dev 28(20):1398–1412. https://doi.org/10.1089/scd.2019.0039
Rivera-Cruz CM, Figueiredo ML (2023) Evaluation of human adipose-derived mesenchymal stromal cell toll-like receptor priming and effects on interaction with prostate cancer cells. Cytotherapy 25(1):33–45. https://doi.org/10.1016/j.jcyt.2022.09.009
Duan A, Shen K, Li B, Li C, Zhou H, Kong R, Shao Y, Qin J, Yuan T, Ji J, Guo W, Wang X, Xue T, Li L, Huang X, Sun Y, Cai Z, Liu W, Liu F (2021) Extracellular vesicles derived from lps-preconditioned human synovial mesenchymal stem cells inhibit extracellular matrix degradation and prevent osteoarthritis of the knee in a mouse model. Stem Cell Res Ther 12(1):427. https://doi.org/10.1186/s13287-021-02507-2
Li C, Li X, Shi Z, Wu P, Fu J, Tang J, Qing L (2022) Exosomes from lps-preconditioned bone marrow mscs accelerated peripheral nerve regeneration via m2 macrophage polarization: involvement of tsg-6/nf-κb/nlrp3 signaling pathway. Exp Neurol 356:114139. https://doi.org/10.1016/j.expneurol.2022.114139
Vega-Letter AM, Kurte M, Fernandez-O’Ryan C, Gauthier-Abeliuk M, Fuenzalida P, Moya-Uribe I, Altamirano C, Figueroa F, Irarrazabal C, Carrion F (2016) Differential tlr activation of murine mesenchymal stem cells generates distinct immunomodulatory effects in eae. Stem Cell Res Ther 7(1):150. https://doi.org/10.1186/s13287-016-0402-4
Latourte A, Kloppenburg M, Richette P (2020) Emerging pharmaceutical therapies for osteoarthritis. Nat Rev Rheumatol 16(12):673–688. https://doi.org/10.1038/s41584-020-00518-6
Soliman H, Theret M, Scott W, Hill L, Underhill TM, Hinz B, Rossi FMV (2021) Multipotent stromal cells: one name, multiple identities. Cell Stem Cell 28(10):1690–1707. https://doi.org/10.1016/j.stem.2021.09.001
Andrzejewska A, Lukomska B, Janowski M (2019) Concise review: mesenchymal stem cells: from roots to boost. Stem Cells 37(7):855–864. https://doi.org/10.1002/stem.3016
Ceccariglia S, Cargnoni A, Silini AR, Parolini O (2020) Autophagy: a potential key contributor to the therapeutic action of mesenchymal stem cells. Autophagy 16(1):28–37. https://doi.org/10.1080/15548627.2019.1630223
Lan T, Luo M, Wei X (2021) Mesenchymal stem/stromal cells in cancer therapy. J Hematol Oncol 14(1):195. https://doi.org/10.1186/s13045-021-01208-w
Ferreira JR, Teixeira GQ, Santos SG, Barbosa MA, Almeida-Porada G, Goncalves RM (2018) Mesenchymal stromal cell secretome: influencing therapeutic potential by cellular pre-conditioning. Front Immunol 9:2837. https://doi.org/10.3389/fimmu.2018.02837
Ragni E, Perucca Orfei C, De Luca P, Colombini A, Viganò M, de Girolamo L (2020) Secreted factors and ev-mirnas orchestrate the healing capacity of adipose mesenchymal stem cells for the treatment of knee osteoarthritis. Int J Mol Sci 21(5):1582. https://doi.org/10.3390/ijms21051582
Ling L, Feng X, Wei T, Wang Y, Wang Y, Wang Z, Tang D, Luo Y, Xiong Z (2019) Human amnion-derived mesenchymal stem cell (had-msc) transplantation improves ovarian function in rats with premature ovarian insufficiency (poi) at least partly through a paracrine mechanism. Stem Cell Res Ther 10(1):46. https://doi.org/10.1186/s13287-019-1136-x
Chen J, Liu Y, Zhang J, Yang Y, Liang H, Li T, Yan L, Zhou L, Shan L, Wang H (2023) External application of human umbilical cord-derived mesenchymal stem cells in hyaluronic acid gel repairs foot wounds of types i and ii diabetic rats through paracrine action mode. Stem Cells Transl Med 12(10):689–706. https://doi.org/10.1093/stcltm/szad050
Nedunchezhiyan U, Varughese I, Sun AR, Wu X, Crawford R, Prasadam I (2022) Obesity, inflammation, and immune system in osteoarthritis. Front Immunol 13:907750. https://doi.org/10.3389/fimmu.2022.907750
Squillace S, Salvemini D (2022) Toll-like receptor-mediated neuroinflammation: relevance for cognitive dysfunctions. Trends Pharmacol Sci 43(9):726–739. https://doi.org/10.1016/j.tips.2022.05.004
Hwang S, Sung DK, Kim YE, Yang M, Ahn SY, Sung SI, Chang YS (2023) Mesenchymal stromal cells primed by toll-like receptors 3 and 4 enhanced anti-inflammatory effects against lps-induced macrophages via extracellular vesicles. Int J Mol Sci 24(22):16264. https://doi.org/10.3390/ijms242216264
Vega-Letter AM, Kurte M, Fernández-O’Ryan C, Gauthier-Abeliuk M, Fuenzalida P, Moya-Uribe I, Altamirano C, Figueroa F, Irarrázabal C, Carrión F (2016) Differential tlr activation of murine mesenchymal stem cells generates distinct immunomodulatory effects in eae. Stem Cell Res Ther 7(1):150. https://doi.org/10.1186/s13287-016-0402-4
Tfilin M, Gobshtis N, Fozailoff D, Fraifeld VE, Turgeman G (2023) Polarized anti-inflammatory mesenchymal stem cells increase hippocampal neurogenesis and improve cognitive function in aged mice. Int J Mol Sci 24(5):4490. https://doi.org/10.3390/ijms24054490
Kurte M, Vega-Letter AM, Luz-Crawford P, Djouad F, Noel D, Khoury M, Carrion F (2020) Time-dependent lps exposure commands msc immunoplasticity through tlr4 activation leading to opposite therapeutic outcome in eae. Stem Cell Res Ther 11(1):416. https://doi.org/10.1186/s13287-020-01840-2
Morente-Lopez M, Mato-Basalo R, Lucio-Gallego S, Silva-Fernandez L, Gonzalez-Rodriguez A, De Toro FJ, Fafian-Labora JA, Arufe MC (2022) Therapy free of cells vs human mesenchymal stem cells from umbilical cord stroma to treat the inflammation in oa. Cell Mol Life Sci 79(11):557. https://doi.org/10.1007/s00018-022-04580-z
Chahal J, Gomez-Aristizabal A, Shestopaloff K, Bhatt S, Chaboureau A, Fazio A, Chisholm J, Weston A, Chiovitti J, Keating A, Kapoor M, Ogilvie-Harris DJ, Syed KA, Gandhi R, Mahomed NN, Marshall KW, Sussman MS, Naraghi AM, Viswanathan S (2019) Bone marrow mesenchymal stromal cell treatment in patients with osteoarthritis results in overall improvement in pain and symptoms and reduces synovial inflammation. Stem Cells Transl Med 8(8):746–757. https://doi.org/10.1002/sctm.18-0183
Matas J, Orrego M, Amenabar D, Infante C, Tapia-Limonchi R, Cadiz MI, Alcayaga-Miranda F, Gonzalez PL, Muse E, Khoury M, Figueroa FE, Espinoza F (2019) Umbilical cord-derived mesenchymal stromal cells (mscs) for knee osteoarthritis: repeated msc dosing is superior to a single msc dose and to hyaluronic acid in a controlled randomized phase i/ii trial. Stem Cells Transl Med 8(3):215–224. https://doi.org/10.1002/sctm.18-0053
Fu Z, Song X, Guo L, Yang L, Chen C (2019) Effects of conditioned medium from osteoarthritic cartilage fragments on donor-matched infrapatellar fat pad-derived mesenchymal stromal cells. Am J Sports Med 47(12):2927–2936. https://doi.org/10.1177/0363546519869241
Ma K, Zhu B, Wang Z, Cai P, He M, Ye D, Yan G, Zheng L, Yang L, Zhao J (2020) Articular chondrocyte-derived extracellular vesicles promote cartilage differentiation of human umbilical cord mesenchymal stem cells by activation of autophagy. J Nanobiotechnology 18(1):163. https://doi.org/10.1186/s12951-020-00708-0
Funding
The authors’ research work is funded by Chongqing Key Laboratory of Precision Medicine in Joint Surgery (grant: 425Z2138), Chongqing Excellent Scientist Project (grant: 425Z2W21), Chongqing Natural Science Foundation (grant: cstc2021jcyj-msxmX0135), and Chongqing Postdoctoral Research Project Special Fund (grant: 2021XM3033).
Author information
Authors and Affiliations
Contributions
Z.W, Z.F. and Y.M. collected data, Z.W. and Z.F. wrote the main manuscript text, Z.W., G.D. and X.W. prepared all figures, and X.G., G.C and L.Y. Supervised this study. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
All animal procedures were approved by the Laboratory Animal Welfare and Ethics Committee of Army Medical University (the Third Military Medical University) (AMUWEC20223809). Our experimental design, procedures, and methods of animal study are in accordance with the "General Principles for Experimental Animal Welfare" (GB/T 42011–2022). We have strictly followed the aforementioned regulations during our experimental procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wan, Z., Wang, X., Fu, Z. et al. Toll-like receptor activation regulates the paracrine effect of adipose-derived mesenchymal stem cells on reversing osteoarthritic phenotype of chondrocytes. Mol Biol Rep 51, 550 (2024). https://doi.org/10.1007/s11033-024-09499-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09499-1