Abstract
Studies investigating the association between glutathione S-transferase P1 (GSTP1) gene polymorphism and bladder cancer (BC) risk have reported conflicting results. In order to clarify the effect of GSTP1 polymorphism on the BC susceptibility, we conducted an updated system review of published epidemiology studies to provide more precise evidence. We performed a systematic search of PubMed, EMBASE, and China National Knowledge Infrastructure (CNKI). 20 studies with 4,428 BC cases and 5,457 controls were identified. The combined analyses based on all studies showed that there was a significant difference in the genotype distribution in GSTP1(A313G) polymorphism between BC cases and controls not only in Asians (GG vs. AA + AG, OR = 1.59, 95 % CI = 1.01–2.51) but also in Caucasians (GG vs. AA + AG, OR = 1.51, 95 % CI = 1.11–2.06). Upon stratification for smoking status, we observed no statistically significant difference in genotype distribution of GSTP1 in ever-smokers. Combination of the high-risk genotypes (GSTM1 null + GSTT1 null + GSTP1 313 A/G or G/G) demonstrated further increase in the BC risk (OR = 6.64, 95 %CI = 3.63–12.16). This meta-analysis suggests that GSTP1 313 G/G polymorphism is a strong predisposing risk factor for BC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bladder cancer (BC) is one of the most common urological malignancies in the worldwide, with an increasing incidence and death rate nowadays [1, 2]. An estimated 386,300 new cases of BC occurred worldwide in 2008, with 150,200 deaths annually [1]. The highest BC incidence rates are found in Western Europe and North America. In European countries, there were an estimated 0.14 million new cases of BC and 0.05 million deaths from these health care problems in 2008 [3]. Therefore, early identification of persons at risk and early detection of BC are the most appropriate means of prevention, and hence contribute to the improvement of the BC patient’s diagnosis and treatment.
In recent years, a large number of epidemiology studies have suggested that many genetic polymorphisms can affect the BC susceptibility [4–10]. And it is now commonly accepted that the cause of BC is a multi-factorial interaction of environmental triggers (e.g., exposure to certain chemicals, smoking, chronic urinary tract infections) and genetic susceptibility.
Glutathione S-transferases (GSTs) are members of a multi-gene family of isoenzymes expressed in almost all living organisms [11]. As the most important phase II metabolizing enzymes, GSTs catalyse the conjugation of potentially damaging chemical mutagens and protect against the products of oxidative stress [12, 13]. They are involved in the metabolism of many xenobiotics in mammals, including an array of environmental carcinogens and endogenously derived reactive oxygen species [12, 14]. Based on sequence similarities, human cytosolic GSTs superfamily have been grouped into at least 8 distinct classes, called GST α, μ, κ, π, σ, ω, θ, and ζ [15]. Functional polymorphism has been identified in the Glutathione S-transferase P1 (GSTP1) gene coding for GST-π. The GSTP1 A313G polymorphism may result in an amino acid variation of isoleucine/valine at codon 105 in the protein (Ile105Val). GSTP1 allelic variants may lead to increased organism highly susceptible to oxidative DNA damage and to the accumulation of DNA base adducts, which can allow tumor cells to acquire various other oncogenic genetic alterations in urinary bladder carcinogenesis.
Over the past few decades, a great number of studies were performed to clarify the true association between GSTP1 A313G polymorphism and BC risk, especially among Caucasians. However, previous case–control studies investigating the association have reported conflicting results. In order to investigate the real effect of GSTP1 polymorphism on the risk of developing BC, we conducted an updating meta-analysis from the available studies to better compare results between epidemiological studies.
Materials and methods
Literature search strategy
We did a systematic search in the following electronic databases: PubMed (1950 to August 2012), EMBASE (1950 to August 2012), and China National Knowledge Infrastructure (CNKI) (1979 to August 2012). The following key words were used: (“glutathione S-transferase” OR “GST” OR “GSTP1” OR “rs1695” OR “Ile105Val” OR “A313G”) AND (“bladder” OR “urinary” OR “urocyst” OR “urotheli*”) AND (“adenocarcinoma*” OR “carcinoma*” OR “cancer*” OR “tumour*” OR “tumor*” OR “neoplasm*”). No language restriction was used. The reference lists of the selected papers were screened by hand for potentially relevant new articles.
Furthermore, if more than one paper was published with identical author using the same case series, we selected the research with more sample size [14].
Inclusion and exclusion criteria
The criteria employed to select studies for this systematic review were as follows: (i) independent epidemiological studies (for humans only); (ii) a clear description of GSTP1 polymorphism in BC cases and controls. The exclusion criteria were: (i) not an original paper (e.g., review or letter etc.); (ii) duplicate publications; (iii) no control.
Data extraction
Two investigators (Ke Wu and Xianding Wang) independently extracted all the data from each study. Differences were resolved by a third investigator (Yiping Lu). The following data were extracted (please see Table 1): First author’s name, Publication year, Country, Design of study (hospital or population based case–control study), Majority race of study population, Number of cases and controls with different GSTP1 genotypes.
Statistical analysis
Statistical analyses were conducted by use of STATA 11.0 (Stata-Corp LP, College Station, TX, USA) and Review Manager 5.1.6 (Cochrane Collaboration, Oxford, UK). A fixed- or random- effects model was used to calculate pooled effect estimates depending on statistical heterogeneity. The crude odds ratios (ORs) were pooled using the random-effects model (DerSimonian Laird method) when statistical heterogeneity was found(P < 0.05).
Also, subgroup analyses were performed on the basis of race, design of study and smoking behavior, and so on. Publication bias was assessed by visual inspection of funnel plots, the Begg’s rank correlation method and the Egger’s weighted regression method [16, 17]. In this study, P < 0.05 was considered statistically significant, and all statistical tests were two sided.
Results
Study characteristics
The literature search was updated on August 1st, 2012. The search terms resulted in 742 articles. At last, 20 studies (19 in English and 1 in Chinese) with 4,428 BC cases and 5,457 controls were identified (please see Table 1 and Fig. 1) [18–37].
Overall analysis
The pooled results based on all studies showed a statistically significant link between GSTP1 A313G polymorphism and BC risk (GG vs. AA +AG: OR = 1.50, 95 % CI = 1.13–2.00; AA vs. AG+GG: OR = 0.82, 95 % CI = 0.70–0.95) (Table 2, Fig. 2). Because the test for heterogeneity between eligible studies was significant (P < 0.001, I 2 = 64.4 %), the random-effects model was performed for the data analysis.
Furthermore, Begg’s rank correlation method and Egger’s weighted regression method were used to assess publication bias. Finally, we found that there was no evidence of publication bias in GSTP1 A313G polymorphism studies (P Begg = 0.09, P Egger = 0.15) (Figs. 3, 4).
Ethnic origin (Asians and Caucasians) and control sources (hospital-based and population-based)
When stratifying by race, the combined ORs for GSTP1 A313G polymorphism (GG vs. AA+AG) were 1.59 (95 % CI = 1.01–2.51, P = 0.04) in the analysis among Asians, and 1.51 (95 % CI = 1.11–2.06, P = 0.01) in the analysis among Caucasians. Stratifying this meta-analysis by control sources, we also found a significant difference between GSTP1 genotype and BC susceptibility in studies with population-based controls. In hospital-based studies, GSTP1 A313G variants (AG or GG) showed a marked increase in BC risk with an OR of 1.26 (95 % CI = 1.03–1.53), compared to individuals carrying AA genotype, used as reference category.
Smoking status (ever-smokers and non-smokers)
Considering that smoking is a risk factor for BC, and that GST genes are involved in the metabolism of various carcinogens present in smoke [7], further analyses according to smoking status of subjects were performed. Only five studies provided the raw data on the relationship between smoking and BC risk. We found that smoking did not modify the association between the GSTP1 polymorphism and BC risk (AA vs. GG: OR = 0.9, 95 % CI = 0.53–1.53, P = 0.69) in ever-smokers (Table 3).
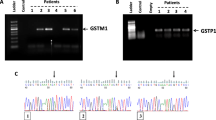
Combination of genotypes
Combination of the two high-risk genotypes (G allele of GSTP1 genotype and GSTM1 null or GSTT1 null) revealed that the risk increased up to 2.64 times (95 % CI = 1.90–3.65; P < 0.0001) for GSTP1 and GSTM1 and 2.39 times (95 % CI = 1.54–3.70, P < 0.0001) for GSTP1 and GSTT1 genotype.
Four studies reported the combination genotypes of GSTP1, GSTM1 and GSTT1 in subjects. We found that individuals with risk genotypes (null genotypes of GSTM1 and GSTT1 and the 313 AG/GG of GSTP1) had considerably increased BC susceptibility (OR = 6.64, 95 % CI = 3.63–12.16, P < 0.00001) compared with those who had non-risk genotypes (positive genotypes of GSTM1 and GSTT1 and 313 A/A genotype of GSTP1). All the results are presented in Tables 4, 5.
Discussion
Nowadays, the exact mechanisms of bladder tumorigenesis remain unknown. There is a growing realization that the development of BC is caused by a complex interaction of both genetic and environmental factors. Procarcinogens are mainly metabolized by various metabolizing enzymes in the human body. Interindividual variations in the genetic and cellular mechanisms of detoxification of carcinogenic chemicals, such as sequence variations in genes coding for the GSTs family, might potentially confer different degrees of risk to BC [5].
Until recently, a number of studies on the polymorphisms of xenobiotic-metabolizing enzymes and BC risk have been reported, especially for GSTP1 [7, 8, 35, 38]. In 1997, Harries et al. [18] firstly reported the association between the GSTP1 A313G polymorphism and BC risk among individuals from the Edinburgh area. Following this first report, similar studies were conducted in different countries by other researchers. However, studies investigating the association have reported conflicting results. Moreover, most of these studies were based on relatively small sample sizes.
As a powerful statistical method, meta-analysis can help to summarize the effect size results from numerous independent epidemiology studies and to provide more reliable outcomes. In 2007, there has been only one meta-analysis that suggested that, as compared with GSTP1 Ile/Ile, the unadjusted summary OR for GSTP1 Ile/Val and Val/Val was 1.44 (95 % CI = 1.17–1.77) [39]. However, some limitations were found in the statistical data in this prior meta-analysis: (i) in Katoh et al. [40] study , the sample included 106 cases who were the patients with urothelial cancer (not just bladder cancer); (ii) more than one included study was performed by identical research team using the same case series [41–44]. The duplicated data of these studies should not be included in prior meta-analysis. On the other hand, another nine studies have investigated the association between GSTP1 polymorphism and BC susceptibility over the last nearly 6 years. As a result, an updated meta-analysis is needed.
We found that significant associations between GG genotype of GSTP1 and BC risk in all subjects (Asians and Caucasians), suggesting that carriers of homozygous variant in GSTP1 lack enzyme activity. However, there was no association between GSTP1 313 GG genotype and BC susceptibility in hospital-based case–control study (HCC). As for HCC, selection bias may not be avoidable, and the subjects may not be representative of the general population [35]. The data on hospital controls could provide relatively lower risk estimates if the diseases of the controls were associated with the gene variant being studied [9]. Therefore, further studies based on population design are necessary. In addition, differences between study designs were also reported in prior studies concerning GSTs genotypes at cancer risk [12].
When stratified according to gender, we found that a significant association between G allele of GSTP1 genotype (heterozygous or homozygous variant) and BC risk among male, but not female. The inconsistent findings may be due to the following two reasons: the genetic background of female is distinguished from that of male, and risk of the same kind of disease is obviously different [45]; there is only one research team that published the original data (90 cases and 77 controls) about GSTP1 AG+GG genotype and BC risk among female [43]. Because of the limited sample size and power, results from this stratified analysis should be considered with caution.
It has been known that smoking is one of the main independent risk factors for BC risk, accounting for half of the cases in male and nearly 35 % in female [46]. GSTs are involved in the metabolism of the multiple carcinogens contained in tobacco smoke, so subgroup analyses by smoking were performed. In our study, no statistically significant difference in genotype distribution of GSTP1 in ever-smokers was found. The possible reason we though is that the GSTs are a family of enzymes responsible for the detoxification of a wide range of chemical carcinogens, so even though only one gene of GST family linked a variant, the GSTs-activity is unlikely to have a significant down-effect on metabolic clearance. Moreover, other environmental factors such as diet, living habit and occupational exposure may affect this association.
Some studies also examined the combination effects of unfavorable GSTs. Our meta-analysis suggests that the GSTP1 polymorphism and its combination with GSTM1, and GSTT1 may be associated with BC risk. Therefore, gene–gene interactions might be primarily involved in the genetic susceptibility for BC, which could be explained by various substrates used by different GSTs inducing resulting in combined action [37, 47, 48]. We assume that the subjects possessing Val allele of GSTP1 and null allele of GSTM1 and GSTT1 have higher BC susceptibility mainly due to reduced detoxification of carcinogens [28].
There are some limitations in our study: First of all, relatively small sample size and significant heterogeneity were observed in some sub-analyses. Second, because of the lack of individual patient data, we could not perform an adjustment estimate. Third, because many environmental factors may affect the BC susceptibility, all our findings may be due to the context of the genetic background and interacting with multiple environmental factors. Finally, meta-analysis is just a statistical test that is subject to many methodological restrictions [8, 45, 49].
In conclusion, our study suggested that GSTP1polymorphism is associated with a high increase in the risk of BC. Also, the combination of three risk GSTs genotypes is strong predisposing risk factor for BC. No significant gene–smoking interaction association was found for the GSTP1 variant in the risk of BC in ever-smokers. Because heterogeneity among the included studies was extreme, the results of this meta-analysis may be confirmed by additional well-designed, high-quality case control studies with larger populations.
References
Jemal A, Bray F, Center MM et al (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Chang CH, Chang CL, Tsai CW et al (2009) Significant association of an XRCC4 single nucleotide polymorphism with bladder cancer susceptibility in Taiwan. Anticancer Res 29:1777–1782
Ferlay J, Parkin DM, Steliarova-Foucher E (2010) Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer 46:765–781
Ovsiannikov D, Selinski S, Lehmann ML et al (2012) Polymorphic enzymes, urinary bladder cancer risk, and structural change in the local industry. J Toxicol Environ Health A 75:557–565
Gong M, Dong W, An R (2012) Glutathione S-transferase T1 Polymorphism Contributes to Bladder Cancer Risk: a Meta-Analysis Involving 50 Studies. DNA Cell Biol 31:1187–1197
Zhang R, Xu G, Chen W et al (2011) Genetic polymorphisms of glutathione S-transferase M1 and bladder cancer risk: a meta-analysis of 26 studies. Mol Biol Rep 38:2491–2497
Salinas-Sanchez AS, Sanchez–Sanchez F, Donate-Moreno MJ et al (2011) Polymorphic deletions of the GSTT1 and GSTM1 genes and susceptibility to bladder cancer. BJU Int 107:1825–1832
Moore LE, Baris DR, Figueroa JD et al (2011) GSTM1 null and NAT2 slow acetylation genotypes, smoking intensity and bladder cancer risk: results from the New England bladder cancer study and NAT2 meta-analysis. Carcinogenesis 32:182–189
Jiang Z, Li C, Wang X (2011) Glutathione S-transferase M1 polymorphism and bladder cancer risk: a meta-analysis involving 33 studies. Exp Biol Med 236:723–728
Cantor KP, Villanueva CM, Silverman DT et al (2010) Polymorphisms in GSTT1, GSTZ1, and CYP2E1, disinfection by-products, and risk of bladder cancer in Spain. Environ Health Perspect 118:1545–1550
Simic T, Savic-Radojevic A, Pljesa-Ercegovac M et al (2009) Glutathione S-transferases in kidney and urinary bladder tumors. Nat Rev Urol 6:281–289
Chen B, Cao L, Zhou Y et al (2010) Glutathione S-transferase T1 (GSTT1) gene polymorphism and gastric cancer susceptibility: a meta-analysis of epidemiologic studies. Dig Dis Sci 55:1831–1838
Chen B, Zhou Y, Yang P et al (2010) Glutathione S-transferase M1 gene polymorphism and gastric cancer risk: an updated analysis. Arch Med Res 41:558–566
Zhou Y, Li N, Zhuang W et al (2009) Glutathione S-transferase P1 gene polymorphism associated with gastric cancer among Caucasians. Eur J cancer 45:1438–1442
Lo HW, Ali-Osman F (2007) Genetic polymorphism and function of glutathione S-transferases in tumor drug resistance. Curr Opin Pharmacol 7:367–374
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Harries LW, Stubbins MJ, Forman D et al (1997) Identification of genetic polymorphisms at the glutathione S-transferase Pi locus and association with susceptibility to bladder, testicular and prostate cancer. Carcinogenesis 18:641–644
Peluso M, Airoldi L, Magagnotti C et al (2000) White blood cell DNA adducts and fruit and vegetable consumption in bladder cancer. Carcinogenesis 21:183–187
Steinhoff C, Franke KH, Golka K et al (2000) Glutathione transferase isozyme genotypes in patients with prostate and bladder carcinoma. Arch Toxicol 74:521–526
Toruner GA, Akyerli C, Ucar A et al (2001) Polymorphisms of glutathione S-transferase genes (GSTM1, GSTP1 and GSTT1) and bladder cancer susceptibility in the Turkish population. Arch Toxicol 75:459–464
Ma QW, Lin GF, Chen JG et al (2002) Polymorphism of glutathione S-transferase T1, M1 and P1 genes in a Shanghai population: patients with occupational or non-occupational bladder cancer. Biomed Environ Sci 15:253–260
Hung RJ, Boffetta P, Brennan P et al (2004) GST, NAT, SULT1A1, CYP1B1 genetic polymorphisms, interactions with environmental exposures and bladder cancer risk in a high-risk population. Int J Cancer 110:598–604
Broberg K, Bjork J, Paulsson K et al (2005) Constitutional short telomeres are strong genetic susceptibility markers for bladder cancer. Carcinogenesis 26:1263–1271
Cao W, Cai L, Rao JY et al (2005) Tobacco smoking, GSTP1 polymorphism, and bladder carcinoma. Cancer 104:2400–2408
Garcia-Closas M, Malats N, Silverman D et al (2005) NAT2 slow acetylation, GSTM1 null genotype, and risk of bladder cancer: results from the Spanish Bladder Cancer Study and meta-analyses. Lancet 366:649–659
Saad AA, O’Connor PJ, Mostafa MH et al (2005) Glutathione S-transferase M1, T1 and P1 polymorphisms and bladder cancer risk in Egyptians. Int J Biol Markers 20:69–72
Srivastava DS, Mishra DK, Mandhani A et al (2005) Association of genetic polymorphism of glutathione S-transferase M1, T1, P1 and susceptibility to bladder cancer. Eur Urol 48:339–344
Xing DL (2006) Association study of polymorphisms in the human drug metabolism enzyme gene and bladder cancer risk. Zhengzhou Daxue 12:1–61
Kopps S, Angeli-Greaves M, Blaszkewicz M et al (2008) Glutathione S-transferase P1 ILE105Val polymorphism in occupationally exposed bladder cancer cases. J Toxicol Environ Health A 71:898–901
Yuan JM, Chan KK, Coetzee GA et al (2008) Genetic determinants in the metabolism of bladder carcinogens in relation to risk of bladder cancer. Carcinogenesis 29:1386–1393
Altayli E, Gunes S, Yilmaz AF et al (2009) CYP1A2, CYP2D6, GSTM1, GSTP1, and GSTT1 gene polymorphisms in patients with bladder cancer in a Turkish population. Int Urol Nephrol 41:259–266
Fontana L, Delort L, Joumard L et al (2009) Genetic polymorphisms in CYP1A1, CYP1B1, COMT, GSTP1 and NAT2 genes and association with bladder cancer risk in a French cohort. Anticancer Res 29:1631–1635
Grando JP, Kuasne H, Losi-Guembarovski R et al (2009) Association between polymorphisms in the biometabolism genes CYP1A1, GSTM1, GSTT1 and GSTP1 in bladder cancer. Clin Exp Med 9:21–28
Zhang R, Xu G, Chen W et al (2011) Genetic polymorphisms of glutathione S-transferase P1 and bladder cancer susceptibility in a Chinese population. Gene Test Mol Biomarkers 15:85–88
Lesseur C, Gilbert-Diamond D, Andrew AS et al (2012) A case-control study of polymorphisms in xenobiotic and arsenic metabolism genes and arsenic-related bladder cancer in New Hampshire. Toxicol Lett 210:100–106
Safarinejad MR, Safarinejad S, Shafiei N (2011) Association of genetic polymorphism of glutathione S-transferase (GSTM1, GSTT1, GSTP1) with bladder cancer susceptibility. Urol oncol. doi:10.1016/j.urolonc.2011.1011.1027
Goerlitz D, El Daly M, Abdel-Hamid M et al (2011) GSTM1, GSTT1 null variants, and GPX1 single nucleotide polymorphism are not associated with bladder cancer risk in Egypt. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 20:1552–1554
Kellen E, Hemelt M, Broberg K et al (2007) Pooled analysis and meta-analysis of the glutathione S-transferase P1 Ile 105Val polymorphism and bladder cancer: a HuGE-GSEC review. Am J Epidemiol 165:1221–1230
Katoh T, Kaneko S, Takasawa S et al (1999) Human glutathione S-transferase P1 polymorphism and susceptibility to smoking related epithelial cancer; oral, lung, gastric, colorectal and urothelial cancer. Pharmacogenetics 9:165–169
Ma Q, Lin G, Qin Y et al (2003) GSTP1 A1578G (Ile105Val) polymorphism in benzidine-exposed workers: an association with cytological grading of exfoliated urothelial cells. Pharmacogenetics 13:409–415
Mittal RD, Srivastava DSAM et al (2005) Genetic polymorphism of drug metabolizing enzymes (CYP2E1, GSTP1) and susceptibility to bladder cancer in North India. Asian Pac J Cancer Prev: APJCP 6:6–9
Gago-Dominguez M, Bell DA, Watson MA et al (2003) Permanent hair dyes and bladder cancer: risk modification by cytochrome P4501A2 and N-acetyltransferases 1 and 2. Carcinogenesis 24:483–489
Castelao JE, Yuan JM, Gago-Dominguez M et al (2004) Carotenoids/vitamin C and smoking-related bladder cancer. Int J Cancer 110:417–423
Chen B, Zhou Y, Yang P et al (2011) CDH1 −160C>A gene polymorphism is an ethnicity-dependent risk factor for gastric cancer. Cytokine 55:266–273
Zeng FF, Liu SY, Wei W et al (2010) Genetic polymorphisms of glutathione S-transferase T1 and bladder cancer risk: a meta-analysis. Clin Exp Med 10:59–68
Reszka E, Jablonowski Z, Wieczorek E et al (2011) GSTP1 mRNA expression in human circulating blood leukocytes is associated with GSTP1 genetic polymorphism. Clin Biochem 44:1153–1155
Pljesa-Ercegovac M, Savic-Radojevic A, Dragicevic D et al (2011) Enhanced GSTP1 expression in transitional cell carcinoma of urinary bladder is associated with altered apoptotic pathways. Urol Oncol 29:70–77
Chen B, Zhou Y, Yang P et al (2011) ERCC2 Lys751Gln and Asp312Asn polymorphisms and gastric cancer risk: a meta-analysis. J Cancer Res Clin Oncol 137:939–946
Conflict of interest
We declare that no conflict of interest exists for any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, K., Wang, X., Xie, Z. et al. Glutathione S-transferase P1 gene polymorphism and bladder cancer susceptibility: an updated analysis. Mol Biol Rep 40, 687–695 (2013). https://doi.org/10.1007/s11033-012-2109-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-012-2109-7