Abstract
The clinical efficacy of haloperidol in the treatment of psychosis has been limited by its tendency to cause parkinsonian-like motor disturbances such as bradykinesia, muscle rigidity and postural instability. Oxidative stress-evoked neuroinflammation has been implicated as the key neuropathological mechanism by which haloperidol induces loss of dopaminergic neurons and motor dysfunctions. This study was therefore designed to evaluate the effect of Jobelyn® (JB), an antioxidant supplement, on haloperidol-induced motor dysfunctions and underlying molecular mechanisms in male Swiss mice. The animals were distributed into 5 groups (n = 8), and treated orally with distilled water (control), haloperidol (1 mg/kg) alone or in combination with each dose of JB (10, 20 and 40 mg/kg), daily for 14 days. Thereafter, changes in motor functions were evaluated on day 14. Brain biomarkers of oxidative stress, proinflammatory cytokines (tumor necrosis factor-alpha and interleukin-6), cAMP response-element binding protein (CREB), mitogen-activated protein kinase (MAPK) and histomorphological changes were also investigated. Haloperidol induces postural instability, catalepsy and impaired locomotor activity, which were ameliorated by JB. Jobelyn® attenuated haloperidol-induced elevated brain levels of MDA, nitrite, proinflammatory cytokines and also boosted neuronal antioxidant profiles (GSH and catalase) of mice. It also restored the deregulated brain activities of CREB and MAPK, and reduced the histomorphological distortions as well as loss of viable neuronal cells in the striatum and prefrontal cortex of haloperidol-treated mice. These findings suggest possible benefits of JB as adjunctive remedy in mitigating parkinsonian-like adverse effects of haloperidol through modulation of CREB/MAPK activities and oxidative/inflammatory pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a neurological disorder due to progressive degeneration of nigrostriatal dopaminergic neurons and development of fibrillar cytoplasmic inclusions of α-synuclein (McCormack et al. 2002; Qian et al. 2010; Schapira and Jenner 2011). The death of nigrostriatal dopaminergic neuron leads to loss of dopamine, and thus the manifestations of motor symptoms such as bradykinesia, muscular rigidity and postural imbalance (Qian et al. 2010; McCormack et al. 2002). Epidemiological data have established a linear relationship between exposures to environmental toxicants such pesticides (rotenone) and herbicides (paraquat), and the genesis of PD (McCormack et al. 2002). For example, high prevalence of PD has been reported in farmers who were exposed to pesticides and herbicides (McCormack et al. 2002). Incidentally, administration of rotenone and paraquat is being used to replicate the neuropathological features of PD in experimental animals (Dauer and Przedborski 2003; Bezard and Przedborski 2011; Alabi et al. 2019; Alam and Schmidt 2002). However, prolonged antipsychotic medications such as haloperidol are also known to induce extrapyramidal adverse effects akin to symptomatology of PD (Andreassen and Jorgensen 2000; Saeed et al. 2017; Zhuravliova et al. 2007; Sykes et al. 2017).
Indeed, the clinical efficacy of haloperidol for the treatment of psychosis has been severely compromised by its tendency to cause motor disturbances such as bradykinesia, muscle rigidity and postural instability, which are the most common debilitating symptoms of PD (Zhuravliova et al. 2007; Saeed et al. 2017; Sykes et al. 2017; Waku et al., 202). Haloperidol is also known to produce abnormal movements such as oral dyskinesia in animals, which has been linked to morphological alterations in distinct brain regions especially the striatum (Kelley et al. 1997; Halliday et al. 1999; Andreassen and Jorgensen 2000). However, catalepsy is one of the most prominent neurobehavioral deficits of haloperidol widely measured in laboratory animals due to its similarity to the symptoms of PD (Zhuravliova et al. 2007; Sykes et al. 2017; Waku et al. 2021). Catalepsy has been described as a state of bradykinesia and muscle rigidity, in which the animal cannot correct externally imposed abnormal postures (Sykes et al. 2017; Waku et al. 2021).
Oxidative stress, resulting from alterations of the mitochondrial electron transport chain, has been proposed as the main neuropathological mechanism through which haloperidol induces loss of dopaminergic neurons and extrapyramidal adverse effects (Saeed et al. 2017; Cadet and Kahler,1994; Casey 2000; Post et al. 2002). Indeed, several studies have shown that haloperidol-induced neuronal damage is due to activation of reactive oxygen species (ROS) formation and reductions in the intracellular concentrations of glutathione (Shivakumar and Ravindranath 1993; Post et al. 1998, 2002; Yokoyama et al. 1998). The clinical symptoms of PD appear only when dopaminergic neuronal cell death exceeds a critical threshold of over 70% of striatal nerve terminals and increased oxidative stress has been implicated as the key mediator of haloperidol-induced neuronal cell death (Saeed et al. 2017). Oxidative stress-induced neuronal injury is known to be further aggravated by the release of inflammatory mediators, thus, linking neuroinflammation and oxidative stress as co-conspirators in the pathology of PD (Sutachan et al. 2012; Taylor et al. 2013). The findings of reduced antioxidant molecules, high concentration of oxidized lipids and protein in the brains of individuals with PD further confirmed the key role of oxidative stress in the pathology of this illness. Thus, the co-administration of agents with potent antioxidant property with haloperidol, might prevent the debilitating motor symptoms in psychotic patients on prolonged haloperidol medication. This supposition is based on the understanding that the inhibition of oxidative stress will prevent the multiple offensive mediators involved in haloperidol-induced neuronal cell death, which constitute the well-known concept of neuroprotection (Qian et al. 2010; Post et al. 1998; Schapira and Olanow 2004).
Jobelyn® (JB) is an African-based dietary supplement derived from the polyphenol-rich leaf sheath of Sorghum bicolor (Gramineae) that has been reported to exhibit wide range of neurobiological activities. For example, anti-amnesic, antioxidant and neuroprotective activities of JB have been established in various animal models (Umukoro et al. 2013; Oyinbo et al. 2015). It was also shown to antagonize psychotic-like symptoms induced by amphetamine and apomorphine without causing cataleptic adverse effect in mice (Omogbiya et al. 2013). In addition, we further reported that JB ameliorated neurological deficits induced by ischemic stroke in rats through neuroprotective mechanisms relating to antioxidant effect and downregulation of nuclear factor Kappa-B expression (Umukoro et al. 2018a, b). Recently, we also showed that JB extended the life span and improves motor dysfunction via augmentation of antioxidant status in Drosophila melanogaster exposed to lipopolysaccharide (John et al. 2022). Besides, HPLC investigations have shown that JB has biologically active constituents such as apigenidin, proapigenidin, apigenin, luteolin and naringenin (Geera et al. 2012; Benson et al., 2013; Makanjuola et al. 2016), which have been reported to exhibit neuroprotection and anti-neuroinflammation through various molecular mechanisms (Lou et al. 2014; Li et al. 2016; Zhang et al. 2017; Umukoro et al. 2018a, b; Olugbemide et al. 2021). The findings that JB and its phyto-constituents possess potent antioxidant and neuroprotective activities suggest that it might protect against haloperidol-induced neuronal cell death and motor dysfunctions, and thus reducing its debilitating motor symptoms in psychotic patients. This study was therefore designed to evaluate the ameliorative and neuroprotective effects of JB on haloperidol-induced motor dysfunctions, and underlying molecular mechanisms in male Swiss mice.
Materials and methods
Laboratory animals
Male Swiss mice (22–25 g) used in the study were purchased from the Central Animal House, University of Ibadan, Ibadan, Nigeria. They were acclimated in the Department of Pharmacology and Therapeutics Animal Holding Facility for one week before the commencement of the study. They were housed in polycarbonates fabricated animal cages with free access to standard rodent pellet diet (Vital feeds®, Jos, Nigeria) and water ad libitum. The ethical principles established by the National Institutes of Health Guide for the Care and Use of Laboratory Animals (NIH Publications No. 8523, revised 2011) were followed.
Drugs and chemicals
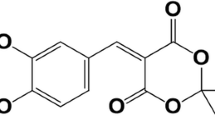
Jobelyn® (Health Forever Products Ltd, Lagos, Nigeria and haloperidol (Sigma-Aldrich, St. Louis, USA) were used in the study. Reagents used include: trichloroacetic acid (TCA) (Burgoyne Burbidges & Co., Mumbai, India), thiobarbituric acid (TBA) (Sigma-Aldrich, St. Louis, USA), Ellman Reagent [5′, 5′-Dithiobis- (2-nitrobenzoate) DTNB] (Sigma-Aldrich, St. Louis, MO, USA) and hydrogen peroxide (H2O2) (BDH Chemicals Ltd., Poole, England). ELISA kits include tumor necrosis factor–alpha (TNF-α) and interleukin-6 (IL-6) from Bio Legend (USA), CREB ELISA Kit (Cat. No. EM0951) and MAPK ELISA Kit (Cat. No. EM1199) from Wuhan Fine Biotech Co., Ltd, China.
Drug preparation
Haloperidol was prepared according to the procedure earlier described (Ben-Azu et al. 2018a), whereas the method described by Omorogbe et al. 2018 was followed in preparation of JB. Briefly, haloperidol and JB were dissolved in distilled water on the experimental day. The dose of 1 mg/kg of haloperidol used in this study was chosen according to our previous studies wherein we observed significant cataleptic behavior resulting from degeneration of cortical pyramidal neurons (Ben-Azu et al. 2018b, c, d, 2019). The doses of 10, 20 and 40 mg/kg used for this study were selected based on the findings of Omorogbe et al. 2018.
Treatments and experimental design
Male Swiss mice were randomly distributed into 5 groups (n = 8). Mice in group 1 were given distilled water (control), group 2 also received distilled water (haloperidol-control) while groups 3–5 had JB (10, 20 and 40 mg/kg, p.o.), daily for 14 days. Thirty minutes after each daily oral treatment, mice in groups 2–6 were given haloperidol (1 mg/kg, p.o). The changes in motor functions were assessed on day 14. The brain biomarkers of oxidative stress, proinflammatory cytokines (tumor necrosis factor-alpha and interleukin-6), CREB, MAPK and histomorphological changes were also determined (Table 1).
Behavioral procedures
Open field test
The animals were placed individually in the center of the open field chamber (72 cm×72 cm×36 cm). Then, the number of lines crossed were recorded by a trained blinded observer for a period of 5 min as previously described (Ben-Azu., 2018a).
Catalepsy test
The effect of JB on haloperidol-induced catalepsy was investigated according to the modified version as earlier described (Costall et al., 1974). The test was done by gently placing the fore limbs of each animal on a horizontal plane wood surface (H = 6 cm; W = 4 cm; L = 16 cm) and the duration of akinesia (period of time the animal remained in one position, before initiating any active movement) in seconds was recorded.
Walk beam test
This test is commonly used for evaluating motor coordination and postural stability in rodents and the procedure earlier described by Omorogbe et al. (2018) was adopted in this study. The walk beam consists of one-metre (100 cm) long beam with a flat surface of width 15 by 7.5 mm elevated to a height of 40 cm between two wooden supports. Beginning at the 15-mm mark, the mice were placed individually on the unsheltered end and allowed to traverse across the beam to the other end. The number of paw slips and distance travelled was recorded for a period of 5 min (Omorogbe et al. 2018).
Pole test
The pole test is a simple model for assessing motor function in rodents and the test is premised on the ability of the mouse to orient itself downwards and descend to the base of the pole when positioned head-up on top of a 60-cm pole of 1-cm diameter. Mice were assessed for the times taken to turn their entire body downwards towards the base (turn time) and descend without sliding (descent time) as earlier described (Saeed et al. 2017).
Preparation of brain tissues for biochemical assays
The animals (n = 5) were euthanized using diethyl ether and each of the isolated brain was weighed and rinsed with 10% w/v sodium phosphate buffer (0.1 M; pH 7.4). Then, each brain tissue was homogenized and centrifuged, and supernatant collection was done using previous established procedures (Ben-Azu et al. 2018a).
Assay for oxidative stress parameters and nitrite content
The level of MDA was estimated in the brain tissue using the thiobarbituric reacting substance (TBARS) assay (Ohkawa et al. 1979). The brain concentrations of MDA were calculated as previously described (Ohkawa et al. 1979) and expressed as µmol MDA/g tissue. The nitrite content was determined using the protocol described by Green et al. (1981). The absorbance was read at 540 nm and the nitrite content was then estimated from the standard curve of sodium nitrite (0–100 M). The GSH content was estimated as earlier described (Moron et al. 1979) and expressed as µM GSH/g tissue. Catalase activity was estimated using the procedure of Goth (1991) and expressed as µmoles of hydrogen peroxide decomposed per min per mg protein (Unit/mg protein). The method of Misra and Fridovich (1972) was followed for the assay of SOD activity (Unit/mg protein). Protein concentration was determined using the procedure of Lowry et al. (1951).
Estimation of TNF-α, IL-6, MAPK and CREB levels
The levels of TNF-α, IL-6, MAPK and CREB in the brain’s supernatants were measured based on the manufacturer’s protocols. They were measured using specific mouse TNF-α (Bio Legend ELISA MAX™ Deluxe kit, USA), IL-6 (BioLegend ELISA MAX™ Deluxe kit, USA), CREB (Wuhan Fine Biotech Co., Ltd, China) and MAPK (Wuhan Fine Biotech Co., Ltd, China). The measurements were done at room temperature in accordance to manufacturers’ instructions using Microplate reader (LT-4500, UK) at 450 nm. The TNF-α, IL-6, CREB, and MAPK concentrations from each brain tissue was extrapolated from their standard curves. The levels of TNF-α and IL-6 were expressed as pg/mg protein while CREB, and MAPK concentrations were presented as ng/mg protein.
Preparation of brain tissues for histology
Mice (n = 3) in the respective treatment groups were anaesthetized with ether. Thereafter, the mice were perfused, and their brains were harvested, and fixed with 10% phosphate buffered formaldehyde. The brains were then subjected to the routine method for paraffin wax embedment to obtain paraffin wax embedded tissue blocks. Given that haloperidol was previously reported to cause degeneration of the nigrostriatal pathway and cortical pyramidal neurons of the prefrontal cortex (PFC) and hippocampus (Ben-Azu et al. 2019; Osacka et al. 2022), transverse sections (5–6 μm thick) of the striatum, PFC and hippocampal (cornu ammonis 3, CA1) regions were obtained with the aid of microtome (Leica, Germany) and the sections were fixed on glass slides. Viable neuronal cells were estimated using research microscope (Olympus CH (Japan) at x 960 magnification and graticule, and quantified as earlier described (Ben-Azu et al. 2019, 2022). Viable neurons were regarded as well rounded-shaped, intact cytoplasmic cells, without obvious distortions (Emokpae et al. 2020).
Statistical analysis
After normality and homogeneity data checks, data were expressed as mean ± S.E.M (standard error of mean) and analyzed using Graph Pad Prism software version 9.00. Statistical analysis of data was done using one-way ANOVA, followed by Bonferroni post-hoc test. P-values less than 0.05 (p < 0.05) were considered statistically significant.
Results
Jobelyn® ameliorates haloperidol-induced motor dysfunctions in mice
The effects of JB on haloperidol-induced motor impairments in mice are shown in Fig. 1A-D. One-way ANOVA showed that there were significant differences between treatment groups: number of lines crossed, distance traversed, and duration of catalepsy. Bonferroni post-hoc test revealed that haloperidol significantly reduced locomotor activity and distance traversed on the walk beam when compared with controls (Fig. 1A-B). It also produced a significant (p < 0.001) increase in the duration of catalepsy and impaired turning and descending behavior of mice in the vertical pole test when compared with controls (Fig. 1C-D). As shown in Fig. 1A-D, JB attenuated impairment of locomotor activity and motor incoordination induced by haloperidol in mice.
Jobelyn® (JB) ameliorates haloperidol (HAL)-induced motor impairments in mice subjected to open-field (A), walk beam (B), wood block (C) and pole (D) tests. Bars represent the mean ± S.E.M of 8 animals per group. ##p < 0.01, ###p < 0.001 compared to control group, *p < 0.05, *p < 0.01, ***p < 0.001 compared to HAL group (one-way ANOVA followed by Bonferroni post-hoc test)
Jobelyn® increases brain antioxidant enzymes in mice exposed to haloperidol
One-way ANOVA and post-hoc tests indicate that administration of haloperiol (1 mg/kg, p.o.) caused a significant decrease in CAT activity. However, no significant change was observed in the levels of SOD activity in comparison with controls (Fig. 2A-B). Notably, JB (40 mg/kg, p.o.) significantly increased CAT (p < 0.01) activity relative to haloperidol (Fig. 2A).
Jobelyn® restores altered brain contents of GSH, MDA and nitrite in mice exposed to haloperidol
The effects of JB on brain concentrations of GSH, MDA and nitrite in mice exposed to haloperidol are shown in Fig. 3A-C. One-way ANOVA analysis showed that there were significant differences between treatment groups: GSH, MDA and nitrite (Fig. 3A-C). As presented in Fig. 3A-C, haloperidol significantly increased MDA and nitrite brain contents accompanied by depletion of GSH in haloperidol-treated animals. However, JB (40 mg/kg, p.o.) significantly decreased MDA and nitrite, and elevated GSH brain concentrations of mice exposed to haloperidol (Fig. 3A-C).
JB attenuates haloperidol HAL-induced oxidative and nitrergic stress in mice brains: Glutathione, GSH (A), malondialdehyde, MDA, (B) and nitrite (C). Bars represent the mean ± S.E.M of 5 animals / group. #p < 0.05, ##p < 0.01, ###p < 0.001 compared to control group; *p < 0.05, **p < 0.01 compared to HAL group (one-way ANOVA followed by Bonferroni post-hoc test)
Jobelyn® reduces brain contents of TNF-α and IL-6 in haloperidol-treated mice
Administration of haloperidol (1 mg/kg, p.o.) significantly increased TNF-α and IL-6 levels when compared with controls (Fig. 4A-B). Jobelyn® (20 and 40 mg/kg, p.o.) significantly (p < 0.05, p < 0.01) reduced the increased TNF-α concentration in mice brains treated with haloperidol (1 mg/kg, p.o.) in comparison with haloperidol group (Fig. 4A). As regards IL-6, JB (40 mg/kg, p.o.) significantly reduced brain concentration of IL-6 when compared with haloperidol group (Fig. 4B).
JB reduces brain concentrations of tumor necrosis factor-alpha (TNF-α) (A) and interleukin-6 (IL-6) (B) in mice exposed to HAL. Each column represents the mean ± S.E.M of 5 animals / group. ###p < 0.001 compared to control group; *p < 0.05, **p < 0.01 compared to HAL group (one-way ANOVA followed by Bonferroni post-hoc test). HAL = Haloperidol, JB = Jobelyn®. Tumor necrosis factor-alpha = TNF-α, Interleukin-6 = IL-6.
Jobelyn® modulates brain CREB and MAPK activities in mice treated with haloperidol
Haloperidol significantly decreased CREB levels when compared with control (Fig. 5A). But, JB (20 and 40 mg/kg, p.o.) significantly up-regulated CREB activity when compared with haloperidol group (Fig. 5A). As shown in Fig. 5B, haloperidol significantly increased MAPK activity (p < 0.001) when compared with control, which was significantly (p < 0.05) down-regulated by JB (40 mg/kg, p.o.).
JB up-regulates cAMP response-element binding protein (A) and reduces mitogen-activated protein kinase (B) activities in brains of mice exposed to HAL. Bars represent the mean ± S.E.M of 5 animals / group. #p < 0.05, ###p < 0.001 compared to control group; *p < 0.05, **p < 0.01 compared to HAL group (one-way ANOVA followed by Bonferroni post-hoc test). cAMP response-element binding protein = CREB, Mitogen-activated protein kinase = MAPK, HAL = Haloperidol, JB = Jobelyn®.
Jobelyn® improves histomorphological distortions and neuronal cell viability of haloperidol-treated mice
The photomicrographs of the effect of JB on haloperidol-induced histomorphological changes and density of viable cells of the striatum, PFC and hippocampus (CA1) of mice are shown in plate and Fig. 6. Nissyl staining revealed that haloperidol (1 mg/kg, p.o.) caused a severe morphological atrophy of neurons of the striatum and PFC (Fig. 6). Also, haloperidol induced a significant increase in the population of pyknotic neurons in the striatum and PFC when compared to control, which were prevented by JB (20 and 40 mg/kg, p.o.) (Fig. 7). However, no significant changes were observed in the CAI region of the hippocampus following treatments with haloperidol relative to control (Figs. 6 and 7).
Representative photomicrographs of the effect of JB on the striatum, prefrontal cortex (PFC) and hippocampus (CA1) of mice brains treated with HAL: In the striatum and PFC, control slides revealed no atrophic lesions but normal multiple neuronal cells patterns. Haloperidol (HAL) (1 mg/kg) slides show population of neurons with atrophy, dark chromatin nuclei and pyknosis. Jobelyn® (JB) (10 mg/kg) + haloperidol (1 mg/kg) slides show moderate atrophy and neuronal deaths. JB (20 and 40 mg/kg) + HAL (1 mg/kg) slides showed cells with no observable atrophy and lesions having increased population of viable cells. However, in the hippocampus, control slide showed no atrophic lesions but normal multiple neuronal cells without pyknosis. But, in JB (10 mg/kg) + HAL (1 mg/kg) slides there were mild atrophy with increased population of normal neuronal cells. In the JB (20 and 40 mg/kg) + HAL (1 mg/kg) slides, no observable atrophy was found. Black arrow indicates normal neurons with no atrophy; red arrow indicates pyknotic neurons with atrophy. Nissyl stain: x400. Calibration bar = 0.01 mm (10 μm) for all figures
Densitometric score of the effects of jobelyn® (JB) on the histomorphology of the striatum, prefrontal cortex (PFC) and hippocampus of mice treated with haloperidol (HAL). Bars represent the mean ± S.E.M of 3 animals / group. ###p < 0.001 compared to control group; *p < 0.05 compared to HAL group (one-way ANOVA followed by Bonferroni post-hoc test)
Discussion
Oxidative stress, resulting from alterations of the mitochondrial electron transport chain, has been proposed as the main neuropathological mechanism through which haloperidol induces loss of dopaminergic neurons and extrapyramidal adverse effects (Saeed et al. 2017; Cadet and Kahler 1994; Casey 2000; Post et al. 1998). Indeed, several studies have shown that haloperidol-induced neuronal damage is due to activation of reactive oxygen species (ROS) formation and depletion of intracellular concentrations of glutathione (Post et al., 1996; Post et al. 2002; Shivakumar and Ravindranath 1993; Yokoyama et al., 1993. Thus, it has been proposed that the reduction of oxidative stress overload through administration of free radical scavengers might be a rational approach in mitigating the adverse effects of prolonged haloperidol therapy (Post et al. 1998; Schapira and Olanow 2004; Qian et al. 2010), hence, the use of JB in this study. The data obtained from this study showed that haloperidol produced impairment of motor functions as evidenced by reduced locomotor activity, increased cataleptic period and postural instability in mice. However, treatment with JB ameliorated the parkinsonian-like motor symptoms induced by haloperidol in mice.
Earlier studies have shown that administration of haloperidol to laboratory animals induced parkinsonian-like disorders such as catalepsy and postural instability (Saeed et al. 2017; Sharma et al. 2017; Waku et al. 2021). Catalepsy is described as the inability of an animal to correct an externally imposed posture (Saeed et al. 2017; Waku et al. 2021). A normal animal is known to correct itself immediately after being placed in an abnormal position whereas a cataleptic animal remains in the imposed posture for a longer period of time (Waku et al. 2021). Thus, cataleptic state is a reflection of motor dysfunction leading to difficulty in initiating voluntary movement as exhibited by patients with PD. The finding that JB attenuated the cataleptic disorder induced by haloperidol suggests that it might mitigate the motor disturbances caused by prolonged use of this medication by psychotic patients.
The vertical pole test, walk beam model and open filed test were further used to evaluate the effects of JB on motor deficits induced by haloperidol in mice. The pole test, which was originally developed to evaluate bradykinesia in mice is based on the tendency of rodents to orient themselves downwards and descend the pole without sliding off (Saeed et al. 2017). The vertical pole test is often used to measure the sensorimotor function of rodents, which is another key neurological function, grossly impaired in patients with PD (Saeed et al. 2017). The result of this study is in agreement with earlier investigations (Waku et al. 2021), which showed that mice treated with haloperidol exhibited difficulty in orienting downwards and descending from the pole suggesting significant motor impairments. On the other hand, it was only the highest dose of JB that showed improvement in the ability of the animals treated with haloperidol to orient themselves downwards. Meanwhile, the doses of JB attenuated the impaired descending behavior induced by haloperidol. These findings suggest that JB at relevant doses might ameliorate motor incoordination produced by haloperidol in mice. The effects of JB on postural stability and fine motor coordination were further assessed in mice treated with haloperidol by challenging them to walk on the rod in the walk beam test. The distance traverse on the beam and the number of foot slips were monitored. Although haloperidol impaired movement in the walk beam test, it did not affect foot slips, which might be connected with muscle rigidity. Also, JB did not cause foot slips but it reverses the locomotor deficit produced by haloperidol on the walk beam at high doses. In the open field test, haloperidol in a similar characteristic manner, as reported in several studies, produced marked decrease in locomotion (Zhuravliova et al. 2007; Saeed et al. 2017; Sykes et al. 2017; Waku et al. 2021). Besides, haloperidol was also reported to produce abnormal movement such oral dyskinesia in animals, which was linked to morphological alterations of specific brain regions especially the striatum (Kelley et al. 1997; Halliday et al. 1999; Andreassen and Jorgensen 2000). However, JB at high doses improved the locomotor activity compromised by haloperidol in mice. Thus, the findings that JB reversed motor impairment produced by haloperidol suggest its possible benefit as adjunctive remedy in mitigating motor disturbances in patients on prolonged haloperidol therapy.
Although haloperidol-induced parkinsonian-like syndromes have been ascribed to antagonism of nigrostriatal dopaminergic pathway, oxidative stress-mediated degeneration of dopaminergic neurons is known to play a prominent role in the decline of motor functions (Eyles et al. 1997; Sagara 1998; Post et al. 2002; Saeed et al. 2017; Saadullah et al. 2022; Saleem et al. 2022). Specifically, the neurotoxicity of haloperidol has been reported to be initiated by its cationic metabolites, which are transported by organic cation transporters to several brain regions such as substantia nigra, striatum, caudate nucleus and hippocampus (Eyles et al. 1997; Halliday et al. 1999; Post et al. 2002). In the dopaminergic neurons, these reactive metabolites inhibit mitochondrial complex I, thereby leading to induction of oxidative stress and neurodegeneration (Eyles et al. 1997; Post et al. 2002). Indeed, several studies have established increased activation of oxidative and nitrergic pathways as the main offenders of peroxidative neuronal cell death of the nigrostriatal dopaminergic and other neuronal pathways (Shivakumar and Ravindranath 1993; Halliday et al. 1999). In consonant with earlier studies, our data revealed that haloperidol increased whole brain MDA and nitrite concentrations, and promotes depletion of neuronal antioxidant molecules (GSH, catalase and SOD) suggesting activation of oxidative/nitrergic pathways as previously reported (Saadullah et al. 2022; Saleem et al. 2022). It has been reported that the parkinsonian-like symptoms only occur when dopaminergic neuronal cell death exceeds a critical threshold of about 70% of the striatal nerve terminals (Saeed et al. 2017). Several studies have also established increased susceptibility of dopaminergic neurons to oxidative stress, and inflammatory insults in haloperidol-induced motor dysfunctions (Post et al. 1998, 2002; Halliday et al. 1999; Saeed et al. 2017). Thus, oxidative stress-induced neuronal injury is further aggravated by the secondary release of inflammatory mediators suggesting the involvement of both oxidative and inflammatory pathways as co-conspirators in haloperidol-induced loss of dopaminergic neurons and onset of motor disorders (Saeed et al. 2017; Halliday et al. 1999; Post et al. 2002; Ben-Azu et al. 2018b, 2019). Although we did not measure the levels of oxidative stress markers after haloperidol treatment in discrete brain regions particularly in the striatum, which controls motor function, our data also support the previous findings of reduced antioxidant molecules, high concentrations of MDA/nitrite and proinflammatory cytokines, in the brains of mice treated with haloperidol (Ben-Azu et al. 2018a, 20018b). However, it is pertinent to note that oral administration of JB restores the deregulated levels of MDA/nitrite, antioxidant molecules, and proinflammatory cytokines, which might be related to mitigation of the extrapyramidal adverse effects of haloperidol in mice.
The MAPK and CREB pathways have been implicated in the regulation of a variety of cellular functions such as proliferation, differentiation, survival, and death of neuronal cells, and are known to be affected by proinflammatory cytokines and cellular stressors such as oxidative stress (Wang et al. 2013; Chen et al. 2016; Mansour et al. 2018; Tong et al. 2018). It has been reported that deviation from the strict regulation of MAPK and CREB signaling pathway leads to the development of neurological disorders such as Alzheimer’s disease, depression and PD (Wang et al. 2013; Mansour et al. 2018). The role of these signaling pathways in the neuropathology of PD has been further confirmed by the findings that rotenone, which is also an inhibitor of the mitochondrial complex I like haloperidol, activate microglial cells through the MAPK pathway and depletes CREB to cause dopaminergic neuronal damage in substantia nigra that ultimately results in parkinsonism (Chen et al. 2016; Mansour et al. 2018; Tong et al. 2018). More specifically, the response of neurons to activation of microglia promotes oxidative stress, neuroinflammation, and apoptosis, which eventually contribute to the death of dopaminergic neurons and progression of the disease (Chen et al. 2016; Mansour et al. 2018). Moreover, it has been reported that montelukast, which is a leukotriene receptor antagonist, exerted neuroprotective effects in the rotenone-induced PD animal model through the attenuation of MAPK activity (Mansour et al. 2018). In another study, minocycline was also shown to protects against rotenone-induced neurotoxicity via upregulation of CREB expressions (Sun et al. 2019). These findings strongly indicate that MAPK stimulation and downregulation of CREB contribute to rotenone’s neurotoxicity in animal models of PD (Thomas et al. 2018; Sun et al. 2019). Incidentally, our data also showed increased activity of MAPK and reduced levels of CREB in brains of mice exposed to haloperidol, suggesting the likely involvement of these signaling pathways in haloperidol-induced neurotoxicity. But interestingly, mice that were treated with both JB and haloperidol had reduced MAPK and elevated CREB activity, indicating possible robust neuroprotection against dopaminergic neurodegeneration via downstream antioxidant/anti-inflammatory mechanisms.
Activation of MAPK activity and loss of neuroprotective function of CREB have been implicated in the increased oxidative-stress-mediated neuronal cell death that characterized the neuropathology of AD and PD (Mansour et al. 2018; Tong et al. 2018; Thomas et al. 2018; Sun et al. 2019; Behl et al. 1995). The deletion of CREB has been shown to cause non-specific neuronal cell death and progressive neurodegeneration in the hippocampus and striatum, which typified neurodegenerative diseases (Tong et al. 2018; Saura and Cardinaux 2017). The findings from this study further confirm that haloperidol causes pyknosis and atrophy of cytoarchitecture of the PFC, hippocampus and striatum of mice brains, as evidenced by the histological studies we performed. The histomorphometric studies showed that haloperidol caused neuronal cell loss and decreased population of viable neuronal cells in the PFC, hippocampus and striatum. The findings that these changes were associated with increased MAPK and reduced CREB suggest the possible involvement of these signaling molecules in haloperidol-induced loss of viable neuronal cells and motor dysfunctions in mice. Previous studies have also shown that histopathological changes and activation of transcriptional pathway that are associated with decreased neuronal cell viability occurred after chronic administration of haloperidol in experimental models (Post et al. 1998; Noh et al. 2000). However, in the intervention studies, high doses of JB attenuated haloperidol-induced loss of neuronal cells of the PFC, hippocampus and striatum of mice suggesting neuroprotection. It is pertinent to state that several studies have also reported that JB exhibited neuroprotective activity and preserved neuronal cells against oxidative and inflammatory insults in various animal models (Oyinbo et al. 2015; Umukoro et al. 2018a, b; Omorogbe et al. 2018). Unsurprisingly, HPLC investigations have shown that JB contains biologically active phytochemicals such as apigenidin, proapigenidin, apigenin, luteolin and naringenin (Geera et al. 2012; Benson et al., 2013; Makanjuola et al. 2016), many of which have been reported to exhibit various molecular mechanisms relevant for neuroprotection and anti-neuroinflammation functions (Lou et al. 2014; Li et al. 2016; Zhang et al. 2017; Umukoro et al. 2018a, b; Olugbemide et al. 2021). However, more studies are necessary to establish the roles of MAPK and CREB in the neuroprotective functions of JB against haloperidol-induced neurodegeneration and motor dysfunctions in mice.
Conclusion
The results of this investigation suggest that JB improves motor dysfunctions induced by haloperidol via neuroprotective mechanisms relating to antioxidant/anti-inflammatory and modulation of CREB and MAPK pathways, and may be of benefit as adjunctive remedy in reversing the parkinsonian-like adverse effects of haloperidol.
Data Availability
The datasets generated during analyses of the experimental results related to the current study are available from the corresponding author on reasonable request.
Abbreviations
- JB:
-
Jobelyn(R)
- PD:
-
Parkinson’s disease
- TBA:
-
Thiobarbituric acid
- DTNB:
-
[5′, 5′-Dithiobis- (2-nitrobenzoate)
- TCA:
-
Tichloroacetic acid
- HAL:
-
Haloperidol
- GSH:
-
Glutathione
- MDA:
-
Malondialdehyde
- CREB:
-
cAMP response-element binding protein
- MAPK:
-
Mitogen-activated protein kinase
References
Alabi AO, Ajayi AM, Ben-Azu B, Bakre G, Umukoro S (2019) Methyl jasmonate abrogates rotenone-induced parkinsonian-like symptoms through inhibition of oxidative stress, release of pro-inflammatory cytokines, and down-regulation of immnopositive cells of NF-κB and α-synuclein expressions in mice. Neurotoxicol 74:172–183. https://doi.org/10.1016/j.neuro.2019.07.003
Alam A, Schmidt WJ (2002) Rotenone destroys dopaminergic neurons and induces parkinsonian symptoms in rats. Behav Brain Res 136:317–324. https://doi.org/10.1016/s0166-4328(02)00180-8
Andreassen OA, Jorgensen HA (2000) Neurotoxicity associated with neuroleptic-induced oral dyskinesia in rats: implication for tardive dyskinesia. Prog Neurobiol 61:525–541. https://doi.org/10.1016/s0301-0082(99)00064-7
Behl C, Rupprecht R, Skutella T, Holsboer F (1995) Haloperidol-induced cell death-mechanism and protection with vitamin E in vitro. NeuroReport 7:360–364
Ben-Azu B, Aderibigbe AO, Omogbiya IA, Ajayi AM, Owoeye O, Olonode ET, Iwalewa EO (2018a) Probable mechanisms involved in the antipsychotic-like activity of morin in mice. Biomed Pharmacother 105:1079–1090. https://doi.org/10.1016/j.biopha.2018.06.057
Ben-Azu B, Aderibigbe AO, Eneni AO, Ajayi AM, Umukoro S, Iwalewa EO (2018b) Morin attenuates neurochemical changes and increased Oxidative/nitrergic stress in brains of mice exposed to ketamine: Prevention and reversal of Schizophrenia-like symptoms. Neurochemical Res 43:1745–1755. https://doi.org/10.1007/s11064-018-2590-z
Ben-Azu B, Aderibigbe AO, Ajayi AM, Eneni A-EO, Umukoro S, Iwalewa EO (2018c) Involvement of GABAergic, BDNF and Nox-2 mechanisms in the prevention and reversal of ketamine- induced schizophrenia-like behavior by morin in mice. Brain Res Bull 139:292–306
Ben-Azu B, Aderibigbe AO, Omogbiya IA, Ajayi AM, Iwalewa EO (2018d) Morin pretreatment attenuates Schizophrenia-Like Behaviors in Experimental Animal Models. Drug Res (stuttg) 68:159–167
Ben-Azu B, Aderibigbe AO, Ajayi AM, Eneni AO, Omogbiya IA, Owoeye O et al (2019) Morin decreases cortical pyramidal neuron degeneration via inhibition of neuroinflammation in mouse model of schizophrenia. Int Immunopharmacol 70:338–345. https://doi.org/10.1016/j.intimp.2019.02.052
Ben-Azu B, Adebayo OG, Jarikre TA, Oyovwi MO, Edje KE, Omogbiya IA, Eduviere AT, Moke EG, Chijioke BS, Odili OS, Omondiabge OP, Oyovbaire A, Esuku DT, Ozah EO, Japhet K (2022) Taurine, an essential β-amino acid insulates against ketamine-induced experimental psychosis by enhancement of cholinergic neurotransmission, inhibition of oxidative/nitrergic imbalances, and suppression of COX-2/iNOS immunoreactions in mice. Metab Brain Dis 37(8):2807–2826. https://doi.org/10.1007/s11011-022-01075-5
Benson KF, Beaman JL, Ou B, Okubena A, Okubena O, Jensen GS (2013) West african Sorghum bicolor leaf sheaths have anti-inflammatory and immune-modulating properties in vitro. J Med Food 16:230–238. https://doi.org/10.1089/jmf.2012.0214
Bezard E, Przedborski S (2011) A tale on animal models of Parkinson’s disease. Mov Disord 26:993–1002. https://doi.org/10.1002/mds.23696
Cadet JL, Kahler LA (1994) Free radical mechanisms in schizophrenia and tardive dyskinesia. Neurosci Biobehav Rev 18:457–467. https://doi.org/10.1016/0149-7634(94)90001-9
Casey DE (2000) Tardive dyskinesia: pathophysiology and animal models. J Clin Psychiatry 61:5–9
Chen WW, Zhang X, Huang WJ (2016) Role of neuroinflammation in neurodegenerative diseases (review). Mol Med Rep 13:3391–3396. https://doi.org/10.3892/mmr.2016.4948
Costall B, Naylor RJ (1974) On catalepsy and catatonia and the predictability of the cataleptic test for neuroleptics activity. Psychopharmacologia 34:233–241. https://doi.org/10.1007/BF00421964
Dauer W, Przedborski S (2003) Parkinson’s disease: mechanisms and models. Neuron 39:889–909. https://doi.org/10.1016/j.taap.2018.09.012
Emokpae O, Ben-Azu B, Ajayi AM, Umukoro S (2020) D-Ribose-L-cysteine attenuates lipopolysaccharide-induced memory deficits through inhibition of oxidative stress, release of proinflammatory cytokines and nuclear factor-kappa B expression in mice. Naunyn Schmiedebergs Arch Pharmacol 393:909–925. https://doi.org/10.1007/s00210-019-01805-0
Eyles DW, Avent KM, Stedman TJ, Pond M (1997) Two pyridinium metabolites of haloperidol are present in the brain of patients at post-mortem. Life Sci 60:529–534. https://doi.org/10.1016/s0024-3205(96)00656-x
Geera B, Ojwang LO, Awika JM (2012) New highly stable dimeric 3-deoxyanthocyanidin pigments from sorghum bicolor leaf sheath. J Food Sci 77:C566–C572
Goth L (1991) A simple method for determination of serum catalase activity and revision of reference range. Clin Chim Acta 196:143–151. https://doi.org/10.1016/0009-8981(91)90067-m
Green LC, Tannenbaum SR, Goldman P (1981) Nitrate synthesis in the germfree and conventional rat. Science 212:56–58. https://doi.org/10.1126/science.6451927
Halliday GM, Pond SM, Cartwright H, McRitchie DA, Castagnoli N, Van der Shyf CJ (1999) Clinical and neuropathological abnormalities in baboons treated with HPTP, tetrahydropyridine analog of haloperidol. Exp Neurol 158:155–163. https://doi.org/10.1006/exnr.1999.7090
John R, Abolaji AO, Adedara A, Ajayi AM, Aderibigbe AO, Umukoro S (2022) Jobelyn® extends the life span and improves motor function in Drosophila melanogaster exposed to lipopolysaccharide via augmentation of antioxidant status. Metabolic Brain Dis DOI. https://doi.org/10.1007/s11011-022-00919-4
Kelley JJ, Gao XM, Tamminga CA, Roberts RC (1997) The effect of chronic haloperidol treatment on dendritic spines in the rat striatum. Exp Neurol 146:471–478. https://doi.org/10.1006/exnr.1997.6552
Li R, Wang X, Qin T, Qu R, Ma S (2016) Apigenin ameliorates chronic mild stress-induced depressive behavior by inhibiting interleukin-1β production and NLRP3 inflammasome activation in the rat brain. Behav Brain Res 296:318–325. https://doi.org/10.1016/j.bbr.2015.09.031
Lou H, Jing X, Wei X, Shi H, Ren D, Zhang X (2014) Naringenin protects against 6-OHDA-induced neurotoxicity via activation of the Nrf2/ARE signaling pathway. Neuropharmacology 79:380–388. https://doi.org/10.1016/j.neuropharm.2013.11.026
Lowry OH, Rosenbrough NJ, Farr AL, Randall RJ (1951) Protein measurement with Folin phenol reagent. J Biol Chem 193:265–275
Makanjuola SBL, Dosunmu D, Ajonuma L, Ogundaini A, Okubena O (2016) Newly isolated compounds from west african Sorghum bicolor leaf sheaths Jobelyn® show potential in cancer immunosurveillance, 2016. J Cancer Res Therapy 4(4):31–37
Mansour RM, Ahmed MAE, El-Sahar AE, El Sayed NS (2018) Montelukast attenuates rotenone-induced microglial activation/p38 MAPK expression in rats: possible role of its antioxidant, anti-inflammatory and antiapoptotic effects. Toxicol Appl Pharmacol. https://doi.org/10.1016/j.taap.2018.09.012
McCormack AL, Thiruchelvam M, Manning-Bog AB, Thiffault C, Langston JW, Cory-Slechta DA, Di Monte DA (2002) Environmental risk factors and Parkinson’s disease: selective degeneration of nigral dopaminergic neurons caused by the herbicide paraquat. Neurobiol Dis 10:119–127. https://doi.org/10.1006/nbdi.2002.0507
Misra P, Fridovich I (1972) The role of superoxide anion in the autooxidation of epinephrine and a simple assay for superoxide dismutase. J Biol Chem 247:3170–3175
Moron MS, Depierre JW, Mannervik B (1979) Levels of glutathione, glutathione reductase and glutathione S-transferase activities in rat lung and liver. Biochim Biophys Acta 582:67–78. https://doi.org/10.1016/0304-4165(79)90289-7
Noh JS, Kang HJ, Kim EY, Sohn S, Chung YK, Kim SU, Gwag BJ (2000) Haloperidol-induced neuronal apoptosis: role of p38 and c-Jun-NH2-terminal protein kinase. J Neurochem 75:2327–2334. https://doi.org/10.1046/j.1471-4159.2000.0752327.x
Ohkawa HN, Ohishi dK, Yagi (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358. https://doi.org/10.1016/0003-2697(79)90738-3
Olugbemide AS, Ben-Azu B, Bakre AG, Ajayi AM (2021) Naringenin improves depressive- and anxiety-like behaviors in mice exposed to repeated hypoxic stress through modulation of oxido-inflammatory mediators and NF-kB/BDNF expressions. Brain Res Bull 169:214–227. https://doi.org/10.1016/j.brainresbull.2020.12.003
Omogbiya AI, Umukoro S, Aderibigbe AO, Bakre GA (2013) Jobelyn® pretreatment attenuates symptoms of psychosis in experimental models. Basic & Clinical Physiol & Pharmacol 24:331–336. https://doi.org/10.1515/jbcpp-2012-0073
Omorogbe O, Ajayi AM, Ben-Azu B, Oghwere EE, Adebesin A, Aderibigbe AO, Umukoro S (2018) Jobelyn® attenuates inflammatory responses and neurobehavioural deficits associated with complete Freund-adjuvant-induced arthritis in mice. Biomed Pharmacother 98:585–593. https://doi.org/10.1016/j.biopha.2017.12.098
Osacka J, Kiss A, Bacova Z, Tillinger A (2022) Effect of Haloperidol and Olanzapine on hippocampal cells’ proliferation in animal model of Schizophrenia. Int J Mol Sci 23:7711. https://doi.org/10.3390/ijms23147711
Oyinbo CA, Dare WN, Avwioro OG, Igbigbi PS (2015) Neuroprotective effect of Jobelyn® in the hippocampus of alcoholic rat is mediated in part by alterations in GFAP and NF protein expressions. Adv Biol Res 9(5):305–317
Post A, Holsboer F, Behl C (1998) Induction of NF-κB activity during haloperidol-induced oxidative toxicity in clonal hippocampal cells: suppression of NF-κB and neuroprotection by antioxidants. J Neurosci 15:8236–8246. https://doi.org/10.1523/JNEUROSCI.18-20-08236.1998
Post A, Rucker M, Ohl F, Holsboer F, Almeida OFX, Michaelidis TM (2002) Mechanisms underlying the protective potential of α-tocopherol (vitamin E) against haloperidol-associated neurotoxicity. Neuropsychparmacology 26:397–407. https://doi.org/10.1016/S0893-133X(01)00364-5
Qian L, Flood PM, Hong JS (2010) Neuroinflammation is a key player in Parkinson’s disease and a prime target for therapy. J Neural Transm 117:971–979. https://doi.org/10.1007/s00702-010-0428-1
Saadullah M, Arif S, Hussain L, Asif M, Khurshid U (2022) Dose Dependent Effects of Breynia cernua Against the Paraquat Induced Parkinsonism like Symptoms in Animals’ Model: In Vitro, In Vivo and Mechanistic Studies. Dose-response: a publication of International Hormesis Society, 20(3), 15593258221125478. https://doi.org/10.1177/15593258221125478
Saeed A, Shakir L, Khan MA, Ali A, Yousaf M, Zaidi AA (2017) Haloperidol induced Parkinson’s disease mice model and motor-function modulation with pyridine-3-carboxylic acid. Biomed Res Ther 4:1305–1317. https://doi.org/10.15419/bmrat.v4i05.169
Sagara Y (1998) Induction of reactive oxygen species in neurons by haloperidol. J Neurochem 71:1002–1012. https://doi.org/10.1046/j.1471-4159.1998.71031002.x
Saleem U, Hussain L, Shahid F, Anwar F, Chauhdary Z, Zafar A (2022) Pharmacological Potential of the Standardized Methanolic Extract of Prunus armeniaca L. in the Haloperidol-Induced Parkinsonism Rat Model. Evidence-based complementary and alternative medicine: eCAM, 2022, 3697522. https://doi.org/10.1155/2022/3697522
Saura CA, Cardinaux J-R (2017) Emerging roles of CREB-regulated transcription coactivators in brain physiology and pathology. Trends Neurosci 40:720–733. https://doi.org/10.1016/j.tins.2017.10.002
Schapira AH, Jenner P (2011) Etiology and pathogenesis of Parkinson’s disease. Mov Disord 26:1049–1055. https://doi.org/10.1002/mds.23732
Schapira AH, Olanow CW (2004) Neuroprotection in Parkinson disease: mysteries, myths, and misconceptions. JAMA 291:358–364. https://doi.org/10.1001/jama.291.3.358
Sharma AK, Gupta S, Patel RK, Wardhan N (2017) Haloperidol-induced parkinsonism is attenuated by varenicline in mice. J Basic Clin Physiol Pharmacol. https://doi.org/10.1515/jbcpp-2017-0107
Shivakumar BR, Ravindranath V (1993) Oxidative stress and thiol modification induced by chronic administration of haloperidol. J Pharmacol Exp Ther 3:1137–1141
Sun C, Yun Wang M, Mo C, Song X, Wang S, Chen Y, Liu (2019) Minocycline protects against rotenone-induced neurotoxicity correlating with upregulation of Nurr1 in a Parkinson’s disease rat model. BioMed Res Inter Article ID 6843265, 7 pages, 2019. https://doi.org/10.1155/2019/6843265
Sutachan JJ, Casas Z, Albarracin SL, Stab BR, Samudio J, Gonzalez J, Morales L, Barreto GE (2012) Cellular and molecular mechanisms of antioxidants in Parkinson’s disease. Nutr Neurosci 15:120–126. https://doi.org/10.1179/1476830511Y.0000000033
Sykes DA, Moore H, Stott L, Holliday N, Javitch JA, Lane JR, Chariton SJ (2017) Extrapyramidal side effects of antipsychotics are linked to their association kinetics at dopamine D2 receptors. Nat Commun 8:763. https://doi.org/10.1038/s41467-017-00716-z
Taylor JM, Main BS, Crack PJ (2013) Neuroinflammation and oxidative stress: co-conspirators in the pathology of Parkinson’s disease. Neurochem Int 62:803–819. https://doi.org/10.1016/j.neuint.2012.12.016
Thomas T, Timmer M, Cesnulevicius K, Hitti E, Kotlyarov A, Gaestel M (2018) MAPKAP kinase 2-deficiency prevents neurons from cell death by reducing neuroinflammation–relevance in a mouse model of Parkinson’s disease. J Neurochem 105:2039–2052. https://doi.org/10.1111/j.1471-4159.2008.05310.x
Tong H, Zhang X, Meng X, Lu L, Mai D, Qu S (2018) Simvastatin inhibits activation of NADPH Oxidase/p38 MAPK pathway and enhances expression of antioxidant protein in Parkinson disease models. Front Mol Neurosci. https://doi.org/10.3389/fnmol.2018.00165
Umukoro S, Ugbomah A, Aderibigbe AO, Omogbiya AI (2013) Antioxidant property of Jobelyn as the possible mechanism underlying its anti-amnesic effect in rodents. Basic and Clinical Neurosci 4:42–49
Umukoro S, Ejiroghene EO, Ben-Azu B, Olatunde O, Ajayi MA, Omoregbe O, Okubena O (2018a) Jobelyn ameliorates neurological deficits in rats with ischemic stroke through inhibition of release of pro-inflammatory cytokines and NF-kB pathway. Pathophysiol 26:77–88. 10.1016/j.pathophys.2018a.10.002
Umukoro S, Kalejaye HA, Ben-Azu B, Ajayi AM (2018b) Naringenin attenuates behavioral derangements induced by social defeat stress in mice via inhibition of acetylcholinesterase activity, oxidative stress and release of pro-inflammatory cytokines. Biomed Pharmacother 105:714–723. 10.1016/j.biopha.2018b.06.016
Waku I, Magalhaes MS, Alves CO, de Oliveira RA (2021) Haloperidol-induced catalepsy as an animal model for parkinsonism: a systematic review of experimental studies. Eur J Neurosci 53(11):3743–3767. https://doi.org/10.1111/ejn.15222
Wang H, Zhang Y, Qiao M (2013) Mechanisms of extracellular signal-regulated kinase/cAMP response element-binding protein/brain-derived neurotrophic factor signal transduction pathway in depressive disorder. Neural Regen Res 8:843–852. https://doi.org/10.3969/j.issn.1673-5374.2013.09.009
Yokoyama H, Kasai N, Ueda Y, Niwa R, Konaka R, Mori N, Tsuchihashi N, Matsue T, Ohya-Nishiguchi H, Kamada H (1998) In vivo analysis of hydrogen peroxide and lipid radicals in the striatum of rats under long-term administration of a neuroleptic. Free Radic Biol Med 24:1056–1060. https://doi.org/10.1016/s0891-5849(97)00435-8
Zhang Y, Liu B, Chen X, Zhang N, Li G, Zhang LH, Tan LY (2017) Naringenin ameliorates behavioral dysfunction and neurological deficits in a d-galactose-induced aging mouse model through activation of PI3K/AKT/NRF2 pathway. Rejuvenation Res 20:462–472. https://doi.org/10.1089/rej.2017.1960
Zhuravliova E, Barbakadze T, Natsvlishvili N, Mikeladze DG (2007) Haloperidol induces neurotoxicity by the NMDA receptor downstream signaling pathway, alternative from glutamate excitotoxicity. Neurochemist Int 50:976–982. https://doi.org/10.1016/j.neuint.2006.09.015
Acknowledgements
Authors thank the technical staff of the Department of Pharmacology & Therapeutics, University of Ibadan, Nigeria for their assistance.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
SU and JA designed the study; JA and AMA did the experiments; SU and BB did the analysis and wrote the draft of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The ethical principles established by the National Institutes of Health Guide for the Care and Use of Laboratory Animals (NIH Publications No. 8523, revised 2011) were followed.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Umukoro, S., Ajayi, A.M., Ben-Azu, B. et al. Jobelyn® improves motor dysfunctions induced by haloperidol in mice via neuroprotective mechanisms relating to modulation of cAMP response-element binding protein and mitogen-activated protein kinase. Metab Brain Dis 38, 2269–2280 (2023). https://doi.org/10.1007/s11011-023-01253-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-023-01253-z