Abstract
The aim of this study was to examine and compare the effects of the acute administration of verapamil or amlodipine as representatives of the calcium channel blockers or nicorandil as a representative of the mitochondrial ATP-dependent potassium (KATP) channel opener to cardiac contractility, coronary flow, and oxidative stress markers on ischemia/reperfusion injury in the isolated rat heart. The hearts of adult male Wistar albino rats (n = 60 total, 12 per group) were divided into five groups, two controls (preconditioning with Krebs–Henseleit solution) and three experimental depending on acute administrated pharmacological agents (0,63 µmol/L of verapamil, 0,1 µmol/L of amlodipine, and 200 µmol/L of nicorandil). After stabilization and 5 min of preconditioning in experimental groups, hearts from I/R control and all experimental groups underwent global ischemia (20 min) and reperfusion (30 min). Hearts from sham group were continuously followed for 50 min, after stabilization period. Cardiodynamic parameters and coronary flow were recorded at the end of stabilization (S), at the last minute of pharmacological preconditioning (P) and at intervals of 5 min after global ischemia, during reperfusion, or in case of sham group during 20–50 min after stabilization. At the same intervals, we collected coronary venous effluent from which we spectrophotometrically measured the parameters of oxidative stress: the index of lipid peroxidation, superoxide anion radical, hydrogen peroxide, and nitrite. In summary, our findings clearly indicate that the blocking of the calcium channel or the activation of KATP may mediate the protective effect of myocardial preconditioning. The ex vivo results showed that all examined drugs after ischemia and reperfusion have beneficial cardioprotective properties associated with lower values of major pro-oxidative molecules. Obtained effects seem to be the most convincible in case of nicorandil.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prolonged heart ischemia (hypoxia) accompanied by a reperfusion (reoxygenation) involves irreversible damage of the cardiomyocytes, the vascular smooth muscle, the endothelium, and consequently, coronary circulation [1]. Several factors are responsible for cardiac dysfunction caused by ischemia/reperfusion (I/R) injury [2]. However, in the recent years it has become increasingly clear that the key contributing factors to heart failure during I/R injury are elevated production of reactive oxygen species (ROS) and a disturbance in ionic homeostasis, i.e., imbalance of Ca2+, Na+, and K+ [3]. During reperfusion, the reoxygenation of ischemic tissue leads to the overload of mitochondrial Ca2+, extracellular K+ accumulation, and re-normalization of intracellular and matrix pH values, followed by excessive ROS production [4,5,6]. Multiple mechanisms have been hypothesized to explain intracellular Ca2+ overload. Some authors emphasize the role of enhanced Ca2+ influx through a voltage-gated L-type Ca2+ channel or a Na+/Ca2+ exchanger, as well as the excessive release of Ca2+ from the sarcoplasmic reticulum via the ryanodine receptor type 2 [7, 8]. Taking into account dysfunction of the sarcoplasmic reticulum induced by myocardial I/R, the heart loses the ability to maintain intracellular Ca2+ ions and high cytosolic Ca2+ ions contributing to exacerbation of contractile function [9, 10]. The two general explanations are proposed for extracellular K+ accumulation: increased membrane conductance for K+ via activation of K+ channels, the most often mitochondrial ATP-dependent potassium (KATP) channel and K+ efflux coupled to lactate and inorganic phosphate efflux to balance transmembrane charge movement [11]. It is well known that loss of myocardial K+ causes shortening the plateau phase of the action potential and arrhythmogenesis during I/R [12].
Heart injury caused by I/R can be protected by ischemic preconditioning or by using various exogenous cardioprotective agents. Bearing in mind that the ischemic preconditioning is hardly feasible in clinical practice, the attention of the scientific public is focused on the pharmacological and non-pharmacological methods that would be used prior to coronary occlusion or global ischemia in order to reduce the size of myocardial infarction [7].
Regarding the above-mentioned mechanisms of I/R injury, it is clear that administration of the calcium channel blockers (CCBs) or the mitochondrial KATP channel openers before ischemia has positive effects on the heart during reperfusion [13,14,15]. However, to our best knowledge, it is still not possible to determine which of these two groups of drugs is more effective in heart preconditioning.
Therefore, the aim of this study was to examine and compare the effects of the acute administration of verapamil or amlodipine as representatives of the CCBs or nicorandil as a representative of the KATP channel opener to cardiac contractility, coronary flow, and oxidative stress markers on I/R injury in the isolated rat heart.
Materials and methods
Animals
Adult Wistar albino male rats (n = 60) weighing 180–200 g, obtained from Military Medical Academy, Belgrade, Serbia, were used for this study. The animals were housed in wire mesh cages under controlled temperatures at 22 ± 2 °C and controlled light/dark cycle (12/12 h). Food and water were provided ad libitum.
Preparation of isolated rat hearts
Perfusion of hearts with Krebs–Henseleit solution in a Langendorff apparatus (Experimetria Ltd, 1062 Budapest, Hungary) proceeded as described in previous work [16]. The animals were killed by cervical dislocation, after intraperitoneal injection of 100 µL of a 10:1 mixture of ketamine (100 mg/mL; Ketaset, Fort Dodge, Fort Dodge, IA) and xylazine (100 mg/mL; AnaSed, Lloyd Laboratories, Shenandoah, IA). After a ketamine/xylazine-induced narcosis, emergency thoracotomy was performed, the heart was isolated and rapidly excised into a basin of ice-cold isotonic saline. Thereafter heart was attached via an aortic cannula and retrogradely perfused on a Langendorff apparatus at constant perfusion pressure (CPP) of 70 cmH2O with Krebs–Henseleit solution (118 mM NaCl, 4.7 mM KCl, 2.5 mM CaCl2 × 2H2O, 1.7 mM MgSO4 × 7H2O, 25 mM NaHCO3, 1.2 mM KH2PO4, 5.5 mM glucose, equilibrated with 95% O2 mixed with 5% CO2, and warmed to 37 °C) at pH 7.4. Immediately after the restoration of normal rhythm, through the created entrance to the left atrium of the heart and damaged mitral valve, the sensor (transducer BS473-0184, Experimetria Ltd, Budapest, Hungary) was inserted into the left ventricle for continuous monitoring of cardiac function. The following parameters of myocardial function were continuously registered: maximum rate of pressure development in the left ventricle (dp/dt max), minimum rate of pressure development in the left ventricle (dp/dt min), systolic left ventricular pressure (SLVP), diastolic left ventricular pressure (DLVP), heart rate (HR). Coronary flow (CF) was measured flowmetrically.
Experimental protocol
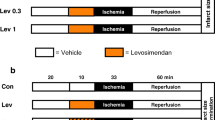
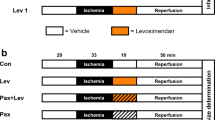
The hearts (n = 60 total, 12 per group) were divided into five groups, two controls and three experimental depending on acute administrated pharmacological agents.
-
1.
Sham group—without ischemia and reperfusion;
-
2.
I/R control group—preconditioning with Krebs–Henseleit solution;
-
3.
Verapamil group—preconditioning with verapamil in dose of 0,63 µmol/L [17];
-
4.
Amlodipine group—preconditioning with amlodipine in dose of 0,1 µmol/L [17];
-
5.
Nicorandil group—preconditioning with nicorandil in dose of 200 µmol/L [18].
After stabilization (average 30-min) and 5 min of preconditioning, all hearts except hearts from sham group underwent global ischemia and reperfusion. Ischemia was induced by turning off the tap on the tube leading to the heart, which stops the flow of the perfusion fluid to the heart. Reperfusion was established for 30 min by reopening the tap after 20 min of ischemia. On the other hand, hearts from sham group were continuously followed for 50 min.
All previously mentioned cardiodynamic parameters and coronary flow were recorded at the end of stabilization (S), 6, 21, 25, 30, 35, 40, 45, 50 min from the stabilization in case of sham group, or at the last minute of pharmacological preconditioning (P) and at intervals of 5 min (1, 5, 10, 15, 20, 25, 30) after global ischemia, during reperfusion (30 min) in case of other examined groups. In addition, at the same intervals, we collected coronary venous effluent from which we spectrophotometrically measured the parameters of oxidative stress: the index of lipid peroxidation measured as thiobarbituric acid reactive substances (TBARS), superoxide anion radical (O2−), hydrogen peroxide (H2O2), and nitrite (NO2−).
Index of lipid peroxidation
The lipid peroxidation level in the coronary venous effluent was estimated by measuring TBARS using 1% thiobarbituric acid in 0.05 NaOH incubated with coronary effluent at 100 °C for 15 min and read at 530 nm. As a blank, we used Krebs–Henseleit solution [19].
Nitrite determination
The NO2− level was measured as an index of NO production using the Griess reagent. A total of 0.5 mL of perfusate was precipitated with 200 μL of 30% sulfosalicylic acid, vortexed for 30 min, and centrifuged at 3000×g. The equal volumes of the supernatant and Griess reagent, containing 1% sulfanilamide in 5% phosphoric acid/0.1% naphthalene ethylenediamine dihydrochloride, were added, incubated for 10 min in the dark, and read at 543 nm. The nitrite levels are calculated using sodium nitrite as the standard [20].
Superoxide determination
The level of the O2− was measured by the reaction of Nitro Blue Tetrazolium in TRIS-buffer with coronary venous effluent and read at 530 nm. Krebs–Henseleit solution was used as a blank probe [21].
Hydrogen peroxide determination
The level of H2O2 was measured using oxidation of Phenol Red by H2O2 in a reaction catalyzed by horseradish peroxidase [22]. A volume of 200 μL of perfusate was precipitated with 800 μL of fresh Phenol Red solution, along with 10 μL of 1:20 horseradish peroxidase (made ex tempore). An adequate volume of Krebs–Henseleit solution was used for a blank probe (instead of coronary venous effluent). The level of H2O2 was read at 610 nm.
Ethical approval
The investigation complies with the European Directive for welfare of laboratory animals No: 2010/63/EU and principles of Good Laboratory Practice. The protocol of the current study was approved by the Faculty of Medical Sciences Ethics Committee for the welfare of experimental animals, University of Kragujevac, and by Ministry of Agriculture, Forestry and Water Management, Authority for Veterinary of Serbia. The investigators understand the ethical principles under which the journal operates and their work complies with animal ethics checklist.
Drugs
Verapamil, amlodipine, and nicorandil were purchased from Sigma–Aldrich Chemie GmbH, Germany.
Statistical analysis
All data are expressed as the mean ± SD. For statistical analysis, we used point of interest S, P, the first minute of reperfusion or 21st minute in sham group (marked as 1), and the last minute of reperfusion or 50th minute in sham group (marked as 30). For comparison within the group, we compared these points with each other, while for comparison between groups we compared the same interest point between groups.
After a normal distribution and homogeneity of variance were, respectively, confirmed using the Shapiro–Wilk test and Levene’s test, we performed a statistical analysis for all measured parameters. The effects of previously mentioned drugs on cardiodynamic and oxidative parameters between groups were analyzed by a one-way ANOVA (Scheffé’s F test) and non-parametric analogue test of ANOVA (Kruskal–Wallis test). Differences were considered significant at p < 0.05. Statistical analysis was performed using SPSS 20.0 software (SPSS Inc., Chicago, IL, USA).
Results
Effects of pharmacological preconditioning on cardiodynamic parameters of isolated rat heart
Maximum rate of left ventricular pressure development (dp/dt max)
In the I/R control group, the dp/dt max was significantly increased in the first minute of reperfusion compared with the S, P, and the last minute of reperfusion, while this parameter was significantly decreased in the last minute of reperfusion compared with the S and P. In the verapamil group, the dp/dt max was significantly decreased after acute administration of verapamil (P) in comparison with the S, the first and the last minute of reperfusion. While in the amlodipine and nicorandil groups this parameter was significantly increased in the last minute in comparison with the first minute of reperfusion.
The dp/dt max was significantly decreased in the first minute of reperfusion in amlodipine and nicorandil groups compared with sham group. In the last minute of reperfusion values, this parameter was almost similar in those groups but significantly increased compared with I/R control group. Also, acute preconditioning in the verapamil, amlodipine, and nicorandil groups significantly decreased the dp/dt max in the first minute of reperfusion, in comparison with I/R control group (Fig. 1; Table 1).
Minimum rate of left ventricular pressure development (dp/dt min)
The dp/dt min was significantly decreased in the last minute of reperfusion compared with the S, P, and the first minute of reperfusion in the I/R control group. Preconditioning with verapamil and amlodipine (P) significantly decreased the dp/dt min in comparison with the S and the last minute of reperfusion. This parameter was also decreased in the first minute of reperfusion compared with S in both groups (verapamil and amlodipine) and increased in the last minute compared with the first minute of reperfusion in the verapamil group.
Preconditioning with mentioned drugs in all examined groups significantly decreased the dp/dt min in the last minute of reperfusion compared to the I/R control group, but values of dp/dt max in experimental groups were almost similar to dp/dt max value of sham group (Fig. 1; Table 1).
Systolic pressure in the left ventricle (SLVP)
SLVP was significantly increased in the first minute of reperfusion compared with S, P, and the last minute of reperfusion in the I/R control group. This parameter was decreased after ex vivo administrated verapamil (P) compared with the S, the first and the last minute of reperfusion in the verapamil group. In the amlodipine group, SLVP was significantly decreased after administration of amlodipine (P) and in the last minute of reperfusion compared to the S.
SLVP was significantly decreased in the first minute of reperfusion in all experimental groups and sham group in comparison with the I/R control group. On the other hand, SLVP was significantly lower after preconditioning with verapamil than after preconditioning with amlodipine or nicorandil (Fig. 1; Table 1).
Diastolic pressure in the left ventricle (DLVP)
In the I/R control group, there was a significant increase of DLVP in the first and in the last minute of reperfusion compared with the S and P. In the verapamil group DLVP was significantly decreased in the P point, the first, and in the last minute of reperfusion compared to the S. In nicorandil group, DLVP was significantly increased in the first minute of reperfusion compared with the S and P.
In all examined groups, DLVP was significantly lower than in the I/R control group in the last minute of reperfusion. DLVP was significantly lower after administration of verapamil compared to sham group and after administration of nicorandil. In the first minute of reperfusion, DLVP was significantly higher in the nicorandil group compared to the amlodipine and verapamil group, and also in the amlodipine and sham group compared to the verapamil group (Fig. 1; Table 1).
Heart rate (HR)
In I/R control group the HR was significantly decreased in the last minute of reperfusion compared with the S, P, and the first minute of reperfusion, while in the amlodipine group the HR was significantly decreased in the last minute of reperfusion compared with the S (Fig. 1; Table 1).
Coronary flow (CF)
Values of CF were significantly decreased in the last minute of reperfusion compared with the S, P, and the first minute of reperfusion in the I/R control and in the verapamil group.
CF was significantly increased after preconditioning with amlodipine or nicorandil than in the I/R control group. On the other hand, CF was significantly increased in verapamil group in the first minute of reperfusion and in amlodipine group in the last minute of reperfusion compared to the I/R control group (Fig. 1; Table 1).
Effects of pharmacological preconditioning on pro-oxidative parameters (O2 −, NO2 −, H2O2, TBARS) in the coronary venous effluent
Index of lipid peroxidation
The TBARS concentration was significantly increased in the first minute of reperfusion and after preconditioning with Krebs–Henseleit solution (P) compared with the first and the last minute of reperfusion in I/R control group.
The TBARS concentration was almost similar in sham and experimental groups during whole experimental protocol. In the first minute of reperfusion, the TBARS concentration was significantly lower in all experimental groups (verapamil, amlodipine, and nicorandil) compared to the I/R control group. The TBARS concentration was lower after preconditioning by verapamil than by amlodipine or nicorandil. However, in the last minute of reperfusion, TBARS concentration was significantly higher in the amlodipine than in the verapamil group (Fig. 2; Table 2).
Nitrite determination
All examined groups (controls and experimental) had a similar level of the NO2− during whole experimental protocol (Fig. 2; Table 2).
Superoxide determination
The O2− level was significantly increased in the first and the last minute of reperfusion compared with the S and P point in the I/R control group, while in the rest groups the level of this parameter was significantly increased in the first minute of reperfusion compared with the S, P, and the last minute of reperfusion.
In the first minute of reperfusion, the O2− level was significantly increased in I/R control and experimental groups compared to sham group and in the nicorandil group compared with the I/R control, verapamil, and amlodipine group, as well as in the verapamil group compared to the I/R control and amlodipine groups. However, in the last minute of reperfusion the O2− level was significantly increased in the sham group compared with the amlodipine group and also in the I/R control group compared with the sham, verapamil, amlodipine, and nicorandil groups (Fig. 2; Table 2).
Hydrogen peroxide determination
In the first minute of reperfusion, the H2O2 level was significantly increased compared with the S, P, and the last minute of reperfusion in the I/R control group.
The H2O2 level was significantly increased in the I/R control group than in sham and all experimental groups in the first minute of reperfusion. While at the last minute of reperfusion, the H2O2 level was significantly increased in the sham, I/R control, and nicorandil groups than in the verapamil group. Also, after preconditioning by nicorandil, the H2O2 level was significantly higher than in sham group and after preconditioning by amlodipine or verapamil (Fig. 2; Table 2).
Discussion
The aim of the present study was to examine and compare the effects of the acute administration of verapamil, amlodipine, or nicorandil to cardiac contractility, coronary flow, and oxidative stress markers on I/R injury in the isolated rat heart.
Due to different mechanisms of action, we thought it would be important to examine acute effects of both mentioned CCBs on I/R injury in the isolated rat heart. Actually, amlodipine (as a representative of dihydropyridine) induces peripheral vasodilatation and has a very little effect on myocardial contractility and sinus node automaticity, while on the other hand verapamil (as a representative of phenylalkylamine) has less influence on peripheral vascular smooth musculature and direct effects on cardiac inotropy and chronotropy [23, 24].
As we mentioned earlier, we used a Langendorff-isolated heart system to study the ex vivo effects of pharmacological preconditioning by verapamil, amlodipine, or nicorandil. This model allows a functional assessment of pharmacological treatments in real time and immediate delivery of the drug directly to the myocardium. Although in vivo ischemia models of reperfusion injury provide very useful results, they are not as effective for studying the functional effects of an I/R injury acutely in real time [16, 25].
During the first phase of our investigation, we focused on the effects of pharmacological preconditioning on the aforementioned cardiodynamic parameters, which served as indicators of myocardial function. Our results suggest that preconditioning with L-type CCBs (verapamil, amlodipine) or mitochondrial KATP opener (nicorandil) has improved recovery of contractile function (measured as dp/dt max and dp/dt min) during reperfusion. Comparing the values of the parameters of myocardial contractility, we note that there are no significant differences between experimental groups. Each of the acutely administered drugs significantly contributed to the improvement of myocardial contractility after global ischemia. Although preconditioning with verapamil led to an initial significant decrease of dp/dt max and dp/dt min, during reperfusion, these parameters were increased and reached values similar to the S. (Fig. 1; Table 1). A previous investigation from our laboratory on a different model of isolated rat heart showed that acute administrated verapamil in a dose of 3 µmol/L also significantly reduced contractile parameters [26]. Bearing in mind that verapamil blocks calcium influx and has direct negative inotropic effects, these effects are consistent with its mechanism of action [27]. Our results are in correlation with results obtained by Tang and coworkers. They reported that orally administrated verapamil at doses of 0, 3, 10, and 30 mg/kg decreases dp/dt max in the telemetered rat [28]. Similar results of contractile function were obtained in the group where the hearts were preconditioned with amlodipine, the second examined CCBs in this study. Hearts from amlodipine group took a little more time during reperfusion to return value of contractile parameters (primarily dp/dt max) to initial (Fig. 1; Table 1). Potential differences between preconditioning with amlodipine and verapamil are probably caused by a different mechanism of action of these drugs. Namely, amlodipine is long-acting, lipophilic, third-generation dihydropyridine CCBs and binds to both dihydropyridine and non-dihydropyridine binding sites. Dihydropyridines selectively inhibit calcium ion influx into vascular smooth muscle cells and myocardial cells, with a greater effect on vascular smooth muscle cells than on cardiac muscle cells [13, 29]. On the other hand, the least fluctuations in the contractile function are in the group where the hearts are preconditioned with nicorandil (Fig. 1; Table 1). Previous published papers have also provided that nicorandil, as a KATP channel opener and a NO donor, improves the recovery of the post-ischaemic contractile dysfunction of the heart [30, 31]. Preconditioning with nicorandil affects the mitochondrial membrane potential and does not allow mitochondrial dysfunction to occur which would contribute to the development and progression of cardiac remodeling and reduced contractility [32].
Application of examined drugs, before global ischemia, significantly improved SLVP and DLVP values during reperfusion. The values of SLVP were similar in all pharmacological preconditioned groups, except in the P point where verapamil caused a significant reduction of SLVP. In contrast to the SLVP, DLVP values were significantly different between groups during the first minutes of reperfusion. The highest values were in the group of hearts preconditioned with nicorandil, then amlodipine, and the lowest values were in the verapamil group. Preconditioning with verapamil significantly reduced values of DLVP and these reduced values were maintained during reperfusion (Fig. 1; Table 1). It is well known that CCBs are widely used for the treatment of hypertension. Regardless of groups, all CCBs bind to alpha-1c subunit of the L-type calcium channel and block the entrance of extracellular Ca2+, resulting in decrease of contractility, lowering of systolic and diastolic pressures, and vascular smooth muscle relaxation [33]. The results of this study correlate with the results of Davitt and coauthors, who also induced reduction of DLVP in rat heart after 5-min long administration of verapamil (300 nM/L) [34]. A clinical study by Okamura has shown that nicorandil, as a nitrite-like antianginal drug, improves coronary circulation without changing the systemic blood pressure [35].
Although there were no significantly differences between I/R control and experimental groups, it is clear that HR decreased over time in the I/R control group (Fig. 1; Table 1). Taking into account low doses as well as a short time of exposure to the investigated drugs, results obtained in our study were expected. In a previously mentioned study from our laboratory, administered in a higher dose, verapamil induces a significant decrease of HR [26]. CCBs are known to have the negative inotropic effect and that this action varies among agents [36]. In an experimental study, it has been shown that nicorandil prevents ventricular tachycardia during acute global ischemia in canine left ventricular wedges [37]. Furthermore, intravenously applied nicorandil reduces QT dispersion in humans after percutaneous transluminal coronary angioplasty of the right coronary artery or after acute myocardial infarction, respectively [38, 39].
After administration of amlodipine or nicorandil, the CF was significantly increased in comparison with the I/R control group (Fig. 1; Table 1). The underlying mechanisms could be the increase of coronary flow mediated by the increased amount of nitric oxide and the attenuation of Ca2+ inflow in vascular smooth muscle cells [40, 41]. Serizawa and coworkers have reported that nicorandil could prevent endothelial dysfunction by upregulating NO and downregulating the level of endothelin-1 [42, 43].
Considering that values of all measured cardiodynamic parameters of experimental groups were mostly similar to values of the sham group in contrast to I/R control group, examined drugs preserved the isolated heart of rats and improve ex vivo I/R injury.
During the next phase of our investigation, we focused on the effects of pharmacological preconditioning on the previously mentioned markers of oxidative stress.
Our results suggested that preconditioning with amlodipine and nicorandil results in a significant increase of TBARS, while on the end of preconditioning the highest values of TBARS were in amlodipine group. Based on our results, we notice that verapamil kept the initial values throughout the experimental protocol, while nicorandil and amlodipine led to a pick of TBARS concentration after their administration. During reperfusion, concentration of TBARS has returned to the stabilization in nicorandil group, while amlodipine groups remained at elevated concentration. None of the examined drugs led to an increase of TBARS concentration in the first minute of reperfusion, as it was in I/R control group (Fig. 2; Table 2). Allah and coauthors reported that concomitant treatment of verapamil and ferrous sulfate induced increase in serum total antioxidant capacity and decline of serum total peroxide, in contrast to the group treated only with ferrous sulfate [44]. In previous work from our laboratory, verapamil did not induce significant changes in values of TBARS [26]. Alam and coworkers in their study on Swiss albino mice showed that amlodipine decreased TBARS levels in a dose-dependent manner [45]. Literature data suggest that CCBs can inhibit lipid peroxidation if they accumulate in cardiac membranes in sufficiently higher concentrations than in serum in vivo [24]. Given that dihydropyridines are highly vascular selective, while verapamil is relatively selective for the myocardium, it could be a reason for higher concentration of TBARS after preconditioning by amlodipine than by verapamil [23]. Abdel-Raheem and coworkers investigated the cardioprotective effect of the nicorandil, on cardiotoxicity induced by doxorubicin in rats. They showed that nicorandil prevented the doxorubicin-induced elevation in TBARS levels and decreased its elevated levels [46].
In all examined groups there were no changes in NO2− level during the whole experimental protocol, while O2− level was significantly different between groups during early minutes of reperfusion. The highest values were in the group of hearts preconditioned with nicorandil, then verapamil, and the lowest values were in the amlodipine group. However, in all experimental group, level of O2− has returned to the stabilization level during reperfusion. The most significant effect of pharmacological preconditioning in our model is the reduction in H2O2 values relative to the I/R control group (Fig. 2; Table 2). The improved cardiac functions could be due to the availability of CCBs and nicorandil to scavenging free radicals generated during early minutes of reperfusion. Some previous studies have shown that pretreatment with verapamil reduces cell death induced by H2O2 by decreasing caspase-3 expression [47]. Da Hyun Lee and other authors showed that verapamil activates nuclear factor erythroid 2-related factor 2 and protect cells from oxidative damage in human and rodent tissues [48]. Several previously published papers support our findings that amlodipine, a highly lipophilic CCBs, reduce oxidative stress. The antioxidative activity of amlodipine is attributed to its high lipophilicity and chemical structure that facilitates proton donation and stabilize the free radical reaction [49]. Nicorandil has been shown to be cardioprotective through inhibition of cardiomyocyte apoptosis induced by oxidative stress and hypoxia. It is considered that nicorandil inhibits oxidative stress-induced apoptosis in cardiac myocytes through a nitric oxide/cGMP-dependent mechanism as well as by activating mitochondrial KATP channels [50].
CCBs exert their beneficial effects on myocardium probably by inhibiting the action of slow Ca2+ inward current through the L-type Ca2+ channels in the cardiac cells. Verapamil reduces oxygen demand by reducing afterload, preload, and contractility; improves oxygen supply to the ischemic zone; preserves the mitochondrial structure and function; and reduces the availability of calcium to stimulate ATPase, protease, and lipase [51, 52]. On the other hand, a mitochondrial KATP channel opener mimics the effect of an ischemic precondition and achieving a protective role in the heart reduces the size of myocardial infarction thereby depolarizing the mitochondrial membrane and preventing mitochondrial Ca2+ overload [18, 30].
In summary, our findings clearly indicate that the blocking of the calcium channel or the activation of KATP may mediate the protective effect of myocardial preconditioning. The ex vivo results showed that all examined drugs have beneficial cardioprotective properties after ischemia and reperfusion. Obtained effects seem to be the most convincible in case of nicorandil. Administration of all agents was associated with lower values of major pro-oxidative molecules indicating that accomplished effects could at least in part be consequential in their antioxidative properties.
Taking into account that the investigated ion modulators proved to be excellent agents in the preconditioning model future research should consider their combined application that could provide even better results.
References
Yang Q, He GW, Underwood MJ, Yu CM (2016) Cellular and molecular mechanisms of endothelial ischemia/reperfusion injury: perspectives and implications for postischemic myocardial protection. Am J Transl Res 8:765
Cadenas S (2018) ROS and redox signaling in myocardial ischemia-reperfusion injury and cardioprotection. Free Radic Biol Med 117:76–89
Kiselyov K, Muallem S (2016) ROS and intracellular ion channels. Cell Calcium 60:108–114
Cao CM, Xia Q, Gao Q, Chen M, Wong TM (2005) Calcium-activated potassium channel triggers cardioprotection of ischemic preconditioning. J Pharmacol Exp Ther 312:644–650
Kwong JQ, Molkentin JD (2015) Physiological and pathological roles of the mitochondrial permeability transition pore in the heart. Cell Metab 21:206–214
Morciano G, Giorgi C, Bonora M, Punzetti S, Pavasini R, Wieckowski MR, Campo G, Pinton P (2015) Molecular identity of the mitochondrial permeability transition pore and its role in ischemia-reperfusion injury. J Mol Cell Cardiol 78:142–153
Altamirano F, Wang ZV, Hill JA (2015) Cardioprotection in ischaemia-reperfusion injury: novel mechanisms and clinical translation. J Physiol 593:3773–3788
Kojima A, Fukushima Y, Ito Y, Ding WG, Kitagawa H, Matsuura H (2018) TRPC channel blockers improve ventricular contractile functions after ischemia/reperfusion in a Langendorff-perfused mouse heart model. J Cardiovasc Pharmacol. https://doi.org/10.1097/FJC.0000000000000566
Piper HM, Meuter K, Schafer C (2003) Cellular mechanisms of ischemia-reperfusion injury. Ann Thorac Surg 75:S644–S648
Hausenloy DJ, Yellon DM (2013) Myocardial ischemia-reperfusion injury: a neglected therapeutic target. J Clin Investig 123:92–100
Venkatesh N, Lamp ST, Weiss J-N (1991) Sulfonylureas, ATP-sensitive K1 channels, and cellular K1 loss during hypoxia, ischemia, and metabolic inhibition in mammalian ventricle. Circ Res 69:623–637
Nichols CG (2016) Adenosine triphosphate-sensitive potassium currents in heart disease and cardioprotection. Card Electrophysiol Clin 8:323–335
Simonovic N, Jeremic J (2017) Role of calcium channel blockers in myocardial preconditioning. Ser J Exp Clin Res 18:281–287
Gross GJ, Auchampach JA, Maruyama M, Warltier DC, Pieper GM (1992) Cardioprotective effects of nicorandil. J Cardiovasc Pharmacol 20:S22-8
Ahmed LA, Salem HA, Attia AS, Agha AM (2011) Pharmacological preconditioning with nicorandil and pioglitazone attenuates myocardial ischemia/reperfusion injury in rats. Eur J Pharmacol 663:51–58
Herr DJ, Aune SE, Menick DR (2015) Induction and assessment of Ischemia-reperfusion injury in Langendorff-perfused rat hearts. J Vis Exp 101:e52908
Miyawaki H, Ashraf M (1997) Ca2+ as a mediator of ischemic preconditioning. Circ Res 80:790–799
Mitani A, Kinoshita K, Fukamachi K, Sakamoto M, Kurisu K, Tsuruhara Y, Fukumura F, Nakashima A, Tokunaga K (1991) Effects of glibenclamide and nicorandil on cardiac function during ischemia and reperfusion in isolated perfused rat hearts. Am J Physiol 261:H1864-71
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 351:8–16
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR (1982) Analysis of nitrate, nitrite and [15N] nitrate in biological fluids. Anal Biochem 131:8–17
Auclair C, Voisin E (1985) Nitroblue tetrazolium reduction. In: Greenvvald RA (ed) Hadnbook of methods for oxygen radical research. CRC Press Une, Boca Raton 123:32–48
Pick E, Keisari Y (1980) A simple colorimetric method for the measurement of hydrogen peroxide produced by cells in culture. J Immunol Methods 38:161–170
Lefrandt JD, Heitmann J, Sevre K, Castellano M, Hausberg M, Fallon M, Urbigkeit A, Rostrup M, Agabiti-Rosei E, Rahn KH, Murphy M, Zannad F, de Kam PJ, Smit AJ (2001) Contrasting effects of verapamil and amlodipine on cardiovascular stress responses in hypertension. Br J Clin Pharmacol 52:687–692
Sugawara H, Tobise K, Kikuchi K (1996) Antioxidant effects of calcium antagonists on rat myocardial membrane lipid peroxidation. Hypertens Res 19:223–228
Skrzypiec-Spring M, Grotthus B, Szeląg A, Schulz R (2007) Isolated heart perfusion according to Langendorff—still viable in the new millennium. J Pharmacol Toxicol Methods 55:113–126
Stojic I, Srejovic I, Zivkovic V, Jeremic N, Djuric M, Stevanovic A, Milanovic T, Djuric D, Jakovljevic V (2017) The effects of verapamil and its combinations with glutamate and glycine on cardiodynamics, coronary flow and oxidative stress in isolated rat heart. J Physiol Biochem 73:141–153
Tang L, El-Din TMG, Swanson TM, Pryde DC, Scheuer T, Zheng N, Catterall WA (2016) Structural basis for inhibition of a voltage-gated Ca2+ channel by Ca2+ antagonist drugs. Nature 537:117
Tang HM, Ju H, Zhao S, LaDuke C, Hahn S, Glick J, Carey C, Friedrichs GS (2016) Translational assessment of cardiac contractility by echocardiography in the telemetered rat. J Pharmacol Toxicol Methods 77:24–32
Fares H, DiNicolantonio JJ, O’Keefe JH, Lavie CJ (2016) Amlodipine in hypertension: a first-line agent with efficacy for improving blood pressure and patient outcomes. Open Heart 3:e000473
Kitakaze M, Asakura M, Kim J, Shintani Y, Asanuma H, Hamasaki T, Seguchi O, Myoishi M, Minamino T, Ohara T, Nagai Y, Nanto S, Watanabe K, Fukuzawa S, Hirayama A, Nakamura N, Kimura K, Fujii K, Ishihara M, Saito Y, Tomoike H, Kitamura S, investigators JW (2007) Human atrial natriuretic peptide and nicorandil as adjuncts to reperfusion treatment for acute myocardial infarction (j-wind): two randomised trials. Lancet 370:1483–1493
Ishii H, Ichimiya S, Kanashiro M, Amano T, Imai K, Murohara T, Matsubara T (2005) Impact of a single intravenous administration of nicorandil before reperfusion in patients with st-segment-elevation myocardial infarction. Circulation 112:1284–1288
Wang S, Fan Y, Feng X, Sun C, Shi Z, Li T, Lv J, Yang Z, Sun D (2018) Nicorandil alleviates myocardial injury and post-infarction cardiac remodeling by inhibiting Mst1. Biochem Biophys Res Commun 495:292–299
Cleophas TJ, van Marun R (2001) Meta-analysis of efficacy and safety of second-generation dihydropyridine calcium channel blockers in heart failure. Am J Cardiol 87:487–490
Davitt K, Hensley L, Clements-Jewery H (2016) Verapamil but not lidocaine suppresses ischemia-induced ventricular fibrillation in the isolated female rat heart. FASEB J 30:1274–1278
Okamura A, Rakugi H, Ohishi M, Yanagitani Y, Shimizu M, Nishii T, Taniyam Y, Asai T, Takiuchi S, Moriguchi K, Ohkuro M, Komai N, Yamada K, Inamoto N, Otsuka A, Higaki J, Ogihara (2001) Additive effects of nicorandil on coronary blood flow during continuous administration of nitroglycerin. J Am Coll Cardiol 37:719–725
Curt FD, Psaty MB, Meyer VJ (1995) Nifedipine dose-related increase in mortality in patients with coronary heart disease. Circulation 92:1326–1331
Hirose M, Tsujino N, Nakada T, Yano S, Imamura H, Yamada M (2008) Mechanisms of preventive effect of nicorandil on ischaemia-induced ventricular tachyarrhythmia in isolated arterially perfused canine left ventricular wedges. Basic Clin Pharmacol Toxicol 102:504–514
Ueda H, Hayashi T, Tsumura K, Yoshimaru K, Nakayama Y, Yoshikawa J (2004) Intravenous nicorandil can reduce QT dispersion and prevent bradyarrhythmia during percutaneous transluminal coronary angioplasty of the right coronary artery. J Cardiovasc Pharmacol Ther 9:179–184
Ueda H, Nakayama Y, Tsumura K, Yoshimaru K, Hayashi T, Yoshikawa J (2004) Intravenous nicorandil can reduce the occurrence of ventricular fibrillation and QT dispersion in patients with successful coronary angioplasty in acute myocardial infarction. Can J Cardiol 20:625–629
Ok SH, Kwon SC, Kang S, Choi MJ, Sohn JT (2014) Mepivacaine-induced intracellular calcium increase appears to be mediated primarily by calcium influx in rat aorta without endothelium. Korean J Anesthesiol 67:404–411
Sahara M, Sata M, Morita T, Hirata Y, Nagai R (2012) Nicorandil attenuates monocrotaline-induced vascular endothelial damage and pulmonary arterial hypertension. PLoS ONE 7:e33367
Serizawa K, Yogo K, Aizawa K, Tashiro Y, Ishizuka N (2011) Nicorandil prevents endothelial dysfunction due to antioxidative effects via normalisation of NADPH oxidase and nitric oxide synthase in streptozotocin diabetic rats. Cardiovasc Diabetol 10:105
Chen Z, Chen X, Li S, Huo X, Fu X, Dong X (2015) Nicorandil improves myocardial function by regulating plasma nitric oxide and endothelin-1 in coronary slow flow. Coron Artery Dis 26:114
Abd Allah ES, Ahmed MA, Abdel Mola AF (2014) Comparative study of the effect of verapamil and vitamin D on iron overload-induced oxidative stress and cardiac structural changes in adult male rats. Pathophysiology 21:293–300
Alam M, Singh BK, Kumar V (2015) Amlodipine potentiates the protective effect of zonisamide on pentylenetetrazol-induced kindling in mice. Drug Dev Ther 6:88
Abdel-Raheem IT, Taye A, Abouzied MM (2013) Cardioprotective effects of nicorandil, a mitochondrial potassium channel opener against doxorubicin-induced cardiotoxicity in rats. Basic Clin Pharmacol Toxicol 113:158–166
Wang Z, Wang D, Li Y, Zhang X (2014) Protective effects of verapamil against H2O2-induced apoptosis in human lens epithelial cells. Biomol Ther 22:553–557
Da Hyun Lee JSP, Lee YS, Sung SH, Lee YH, Bae SH (2017) The hypertension drug, verapamil, activates Nrf2 by promoting p62-dependent autophagic Keap1 degradation and prevents acetaminophen-induced cytotoxicity. BMB Rep 50:91
Tanaka M, Nishimura R, Nishimura T, Kawai T, Meguro S, Irie J, Saisho Y, Itoh H (2014) Effect of single tablet of fixed-dose amlodipine and atorvastatin on blood pressure/lipid control, oxidative stress, and medication adherence in type 2 diabetic patients. Diabetol Metab Syndr 6:56
Nagata K, Obata K, Odashima M, Yamada A, Somura F, Nishizawa T, Ichihara S, Izawa H, Iwase M, Hayakawa A, Murohara T, Yokota M (2003) Nicorandil inhibits oxidative stress-induced apoptosis in cardiac myocytes through activation of mitochondrial ATP-sensitive potassium channels and a nitrate-like effect. J Mol Cell Cardiol 35:1505–1512
Yui H, Imaizumi U, Beppu H, Ito M, Furuya M, Arisaka H, Yoshida KI (2011) Comparative effects of verapamil, nicardipine, and nitroglycerin on myocardial ischemia/reperfusion injury. Anesthesiol Res Pract. https://doi.org/10.1155/2011/521084
Yu W, Wang JJ, Gan WY, Lin GS, Huang CX (2010) Effects of verapamil preconditioning on cardiac function in vitro and intracellular free Ca2+ and L-type calcium current in rat cardiomyocytes post ischemia-reperfusion injury. Zhonghua Xin Xue Guan Bing Za Zhi 38:225–229
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simonovic, N., Jakovljevic, V., Jeremic, J. et al. Comparative effects of calcium and potassium channel modulators on ischemia/reperfusion injury in the isolated rat heart. Mol Cell Biochem 450, 175–185 (2019). https://doi.org/10.1007/s11010-018-3384-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-018-3384-y