Abstract
Objective To estimate the associations between neighborhood disadvantage and neighborhood affluence with breastfeeding practices at the time of hospital discharge, by race-ethnicity. Methods We geocoded and linked birth certificate data for 111,596 live births in New Jersey in 2006 to census tracts. We constructed indices of neighborhood disadvantage and neighborhood affluence and examined their associations with exclusive (EBF) and any breastfeeding in multilevel models, controlling for individual-level confounders. Results The associations of neighborhood disadvantage and affluence with breastfeeding practices differed by race-ethnicity. The odds of EBF decreased as neighborhood disadvantage increased for all but White women [Asian: Adjusted odds ratio (AOR) 0.82 (95% confidence interval (CI) 0.69–0.97); Black: AOR 0.77 (95% CI 0.70–0.86); Hispanic: AOR 0.78 (95% CI 0.70–0.86); White: AOR 0.99 (95% CI 0.91–1.08)]. The odds of EBF increased as neighborhood affluence increased for Hispanic [AOR 1.19 (95% CI 1.08–1.31)] and White [AOR 1.12 (95% CI 1.06–1.18)] women only. The odds of any breastfeeding decreased with increasing neighborhood disadvantage only for Hispanic women [AOR 0.85 (95% CI 0.79–0.92)], and increased for White women [AOR 1.16 (95% CI 1.07–1.26)]. The odds of any breastfeeding increased as neighborhood affluence increased for all except Hispanic women [Asian: AOR 1.31 (95% CI 1.13–1.51); Black: AOR 1.19 (95% CI 1.07–1.32); Hispanic: AOR 1.08 (95% CI 0.99–1.18); White: AOR 1.30 (95% CI 1.24–1.38)]. Conclusions Race-ethnic differences in associations between neighborhood disadvantage and affluence and breastfeeding practices at the time of hospital discharge indicate the need for specialized support to improve access to services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
What is already known on this subject? Breastfeeding has numerous immediate and lifetime benefits for women, infants and society. Breastfeeding practices differ by race and ethnicity, and neighbors and neighborhoods may influence breastfeeding practices. Studies of neighborhood effects on breastfeeding have shown mixed results, did not account for a nested data structure, and did not specifically consider affluence as a neighborhood construct.
What this study adds? Both neighborhood disadvantage and affluence were associated with breastfeeding practices at the time of hospital discharge, with unique associations for exclusive and any breastfeeding by race-ethnicity. This study is the first application of multilevel modeling, which accounts for the complicated variance structure due to women being “nested” in neighborhoods, to estimate these associations. Considering the association between socioeconomic and resource-based characteristics of residential environments and breastfeeding practices has implications for the location of supportive services and media efforts to influence social norms.
Introduction
Despite World Health Organization (WHO) and American Academy of Pediatrics (AAP) recommendations for exclusive breastfeeding for the first 6 months of life with continued breastfeeding up to one (AAP 2012) or 2 years and beyond (WHO 2011), only 22% of U.S.-born infants in 2013 were exclusively breastfed for 6 months, and 31% were breastfed at 12 months (Centers for Disease Control and Prevention (CDC) 2016). In New Jersey in 2006, the percentage of live births that were exclusively breastfed was 34% and the percentage receiving any breastmilk was nearly 66% (New Jersey State Health Assessment Data 2017). These low rates stand in contrast to the numerous immediate and lifetime benefits of breastfeeding for maternal and child health (Grummer-Strawn and Rollins 2015) and society (U.S. Department of Health and Human Services (DHHS) 2011). Suboptimal breastfeeding practices are also both a cause and a consequence of intergenerational health and social disparities because low-income families have lower rates of breastfeeding than their wealthier counterparts (University of Sheffield 2016; Bolling et al. 2007).
Hospital practices and social factors (such as lack of knowledge in the general population, discouraging social norms, poor social support, and maternal work practices and conditions) have been associated with suboptimal breastfeeding (Cohen et al. 1995; Declercq et al. 2009; DHHS 2011; U.S. Department of Health and Human Services, Health Services Research Association 2009; Ryan et al. 2006). Recognition of the importance of breastfeeding support for a woman upon returning to her community post-delivery is increasing; neighborhoods characterized by a lack of breastfeeding support, including professional support and services, have been called “first food deserts” (First Food Friendly 2012). Neighborhoods shape beliefs and behavior (Kawachi and Berkman 2003), and may influence prenatal intentions to breastfeed, which can predict breastfeeding initiation (DGirolamo et al. 2005). In addition, neighborhood economic deprivation is associated with poor infant outcomes (Sellström and Bremberg 2006) and suboptimal maternal health behaviors (Vinikoor-Imler et al. 2011), and could affect breastfeeding practices. Furthermore, socioeconomic and cultural challenges including a lack of privacy and crowded conditions at home may also negatively influence breastfeeding decisions (Kaufman et al. 2010).
Studies of neighborhood effects on breastfeeding showed mixed results: one indicated no relationship between neighborhood deprivation and breastfeeding initiation, but found associations with other perinatal outcomes (Cubbin et al. 2008). Another study found neighborhood deprivation was negatively associated with breastfeeding initiation for disadvantaged urban women, and that the concentration of college-educated individuals in a neighborhood was positively associated with breastfeeding practices (Burdette 2013). Neither study used multilevel modeling, nor analyzed results for different race-ethnicities. Because breastfeeding practices differ by race and ethnicity (McKinney et al. 2016), we stratified our analyses accordingly.
Furthermore, no study to date has investigated the role of neighborhood affluence, a sociological construct distinct from disadvantage that signals the presence of local institutions that stabilize and serve communities. Neighborhood affluence has been shown to be a better predictor of self-rated health (Browning and Cagney 2003) and perinatal health (Kane et al. 2017) than neighborhood disadvantage. Burdette’s study indicates a potential role for neighborhood affluence through college education (Burdette 2013). Thus, features of affluent neighborhoods (e.g., better access to supportive services and institutional supports for breastfeeding) may play a key role. Furthermore, these features may be particularly important for racial/ethnic minorities with low (average) rates of breastfeeding (e.g., Black women). Neighborhood affluence and disadvantage may also play an indirect role in reinforcing attitudes, beliefs and practices that influence breastfeeding. Discouraging social norms may be particularly influential in disadvantaged areas with fewer breastfeeding role models (Bentley et al. 2003).
The availability of and access to services that support breastfeeding in the hospital and community can differ according to the neighborhood racial-ethnic composition. Fewer breastfeeding support services were offered by facilities (hospitals and birth centers) and offices of the Women, Infants, and Children Supplemental Program (WIC) located in areas with larger Black populations compared to other groups (Evans et al. 2011; Lind et al. 2014). Additionally, Black women were more likely to receive advice about formula-feeding rather than breastfeeding from WIC counselors, compared to white women (Beal et al. 2003).
The purpose of this study is to estimate the associations of neighborhood disadvantage and neighborhood affluence with breastfeeding practices at the time of hospital discharge, by race-ethnicity. This study is the first to: apply multilevel modeling (which accounts for the complicated variance structure due to women being “nested” in neighborhoods), examine neighborhood effects on breastfeeding practices stratified by race-ethnicity; and estimate the effects of both neighborhood disadvantage and affluence on breastfeeding practices. We examined exclusive breastfeeding, the optimal feeding method for infants less than 6 months of age, and any breastfeeding, both of which are reported at state and national levels (CDC 2016). Results from our analyses can inform policy and programmatic decisions related to breastfeeding protection, promotion, and support. Considering the association between socioeconomic characteristics of residential environments and breastfeeding practices has implications for the location of supportive services and efforts to influence social norms.
Methods
We constructed a retrospective cohort using electronic birth certificate data for 111,596 infants born to women residing in New Jersey at the time of delivery in 2006. We excluded infants resulting from multiple gestation pregnancies (n = 4970). We also excluded infants born to women who died before discharge (n = 7), did not reside in an urban census tract (n = 25,756), or reported a race-ethnicity other than White, Black, Hispanic, and Asian (n = 124), leaving 80,739 infants. Our multilevel models constituted a complete case analysis of 77,502 infants born to women residing in 1656 census tracts in the analytic sample [3237 (4%) observations were excluded because of missing data]. This study was reviewed and approved by the Institutional Review Board at the University of North Carolina, Chapel Hill.
Neighborhood Disadvantage and Neighborhood Affluence
We geocoded maternal addresses collected from the birth certificates and assigned values to variables from their tracts from two censuses—2000 and 2010. Using the assigned values, we applied a linear interpolation over the decade to create estimates for all variables in 2006. We standardized each variable before creating the indices; thus, index scores can be interpreted as the number of standard deviations away from the population mean.
We constructed indices of neighborhood disadvantage and neighborhood affluence following past research (Kane et al. 2017). This methodology produced and tested indices in urban settings. The neighborhood disadvantage index comprised an unweighted average of six variables: the proportion of households with incomes < $15,000, the proportion of households with incomes ≥ $50,000 (reverse coded), the proportion of families in poverty, the proportion of households receiving public assistance, the total unemployment rate, and the proportion of vacant housing units (Cronbach’s alpha = 0.93). The neighborhood affluence index comprised an unweighted average of three variables: the proportion of 16+ years old civilian workers in professional/managerial occupations, the proportion of 25+ years olds with 16+ years education, and median home values (Cronbach’s alpha = 0.92). The indices were moderately correlated (Pearson’s r = −0.69).
Breastfeeding Practice
Electronic birth certificates recorded the type of feedings given in the 24 h preceding hospital discharge: breastfeeding, formula feeding, combination, other, and unknown. We defined two outcomes: “exclusive breastfeeding” (EBF; 1 = infants fed only breast milk at the time of hospital discharge) and “any breastfeeding” (1 = infants fed a combination of formula and breastmilk).
Covariates
We identified these covariates as potential confounders of the association between neighborhood disadvantage and affluence with breastfeeding practices: maternal race-ethnicity [White, non-Hispanic (“White”); Black, non-Hispanic (“Black”); Hispanic; and Asian, non-Hispanic (“Asian”)], marital status (married or separated vs. not), maternal education (less than high school; high school completed; some college; college degree and higher), maternal age (continuous), parity (continuous), mother worked in previous year (yes/no), mother participated in Medicaid/Health Start during pregnancy (yes/no), father’s name was reported on birth certificate (yes/no), and nativity (U.S.- or foreign-born).
Statistical Analyses
We calculated descriptive statistics using Stata (v.14.1). We constructed multilevel, random-intercept logit models, stratified by race-ethnicity, to estimate odds ratios for both neighborhood disadvantage and neighborhood affluence, using the glmmPQL function in R (v.3.3), controlling for all confounders previously listed (and including a quadratic term for maternal age, given its non-linear distribution compared to the outcomes). We included both exposures in the model to control for one while estimating the other, given that neighborhoods experience degrees of both disadvantage and affluence (Kane et al. 2017). We also controlled for neighborhood race-ethnic composition (percent Asian/Pacific Islander, percent Black, percent Hispanic and percent White) in supplementary models.
Results
Descriptive Analyses
Figures 1 and 2 show the prevalence of exclusive and any breastfeeding at hospital discharge, respectively, for census tracts throughout New Jersey for births in 2006. Urban census tracts are stippled. Visual inspection of the spatial distribution of EBF at the time of hospital discharge shows a higher prevalence in the west and southwest parts of the state, with several contiguous areas of low prevalence in the northeast area of the state (Fig. 1). “Any breastfeeding” was prevalent throughout the state, due to its inclusion of both exclusive and mixed feeding, with the latter practice more prevalent in the northeast area where exclusive breastfeeding was less predominant (Fig. 2). An additional map shows the distribution of neighborhood disadvantage for women who gave birth in New Jersey in 2006 (Online Resource 1). Higher areas of disadvantage are concentrated in the main urban areas and visually correspond to areas with moderate breastfeeding and low exclusive breastfeeding prevalence. Plots of the two indices indicate the distinction between neighborhood disadvantage and neighborhood affluence among urban neighborhoods in New Jersey during the study period. In addition to neighborhoods with contrasting disadvantage and affluence index scores, some neighborhoods scored low on both the disadvantage and affluence scale, and others as high on both scales. These patterns were also observed within racial-ethnic groups (Online Resource 2).
The majority of women who EBF and who provided some breast milk (“any breastfeeding”) were married or separated, born in the U.S., working in the previous year, not enrolled in Medicaid/Health Start during pregnancy, not caring for infants in the NICU, and reported the father’s name on the birth certificate (Table 1). Women who exclusively breastfed at the time of hospital discharge had an average age of 30 and were mostly White and college graduates, with an average neighborhood affluence value of 0.22 (one-fifth of a standard deviation above the mean for New Jersey urban areas) and an average neighborhood disadvantage value of − 0.07 (slightly below the New Jersey urban mean). Women providing some breast milk (“any breastfeeding”) had an average age of 29 and were mostly Hispanic or White and college-educated, with an average neighborhood affluence value of 0.04 and an average neighborhood disadvantage value of − 0.23. The prevalence of both EBF and any breastfeeding decreased with higher parity.
Multi-level Analyses
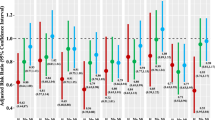
We reported odds ratios (OR) for crude, adjusted, and race-ethnic-specific models with both exposures (neighborhood affluence and neighborhood disadvantage; Table 2).
The crude models showed associations in the expected directions, with negative associations for neighborhood disadvantage with both exclusive and any breastfeeding, and positive associations for neighborhood affluence with both exclusive and any breastfeeding. Adjusting for confounders attenuated these associations, but they remained significant and in the expected direction for exclusive breastfeeding. With adjustment, the association between neighborhood disadvantage and any breastfeeding for all women was not statistically significant. The association between neighborhood affluence and any breastfeeding remained significant and positive.
In race/ethnicity-stratified models, the odds of exclusive breastfeeding decreased as neighborhood disadvantage increased for all but White women [Asian: Adjusted odds ratio (AOR) 0.82 (95% Confidence Interval (CI) 0.69–0.97); Black: AOR 0.77 (95% CI 0.70–0.86); Hispanic: AOR 0.78 (95% CI 0.70–0.86); White: AOR 0.99 (95% CI 0.91–1.08)]. The odds of exclusive breastfeeding increased as neighborhood affluence increased for Hispanic [AOR 1.19 (95% CI 1.08–1.31)] and White [AOR 1.12 (95% CI 1.06–1.18)] women only.
The odds of any breastfeeding decreased as neighborhood disadvantage increased only for Hispanic women [AOR 0.85 (95% CI 0.79–0.92)], and increased for White women [AOR 1.16 (95% CI 1.07–1.26)]. The odds of any breastfeeding increased as neighborhood affluence increased for all except Hispanic women [Asian: AOR 1.31 (95% CI 1.13–1.51); Black: AOR 1.19 (95% CI 1.07–1.32); Hispanic: AOR 1.08 (95% CI 0.99–1.18); White: AOR 1.30 (95% CI 1.24–1.38)].
Supplementary analyses controlling for neighborhood race-ethnic composition did not indicate substantive differences (see Online Resource 3).
Discussion
The purpose of this study was to estimate the associations of neighborhood disadvantage and neighborhood affluence with breastfeeding practices at the time of hospital discharge, by race-ethnicity. This study was the first to use multilevel modeling to estimate these associations, and the first to do so while employing race-ethnic-stratified models. This study was also the first to consider the role of neighborhood affluence in contributing to breastfeeding practices—which past studies have shown to be a better predictor of health outcomes and prenatal health behaviors than neighborhood disadvantage (Browning and Cagney 2003; Kane et al. 2017). Our findings provide information that enhances understanding of race-ethnic disparities in breastfeeding practices, and have implications for policy and programmatic considerations related to the locations of supportive services and efforts to change social norms that discourage optimal infant feeding.
Our results present a nuanced picture of the associations between neighborhood disadvantage and affluence with breastfeeding practices at the time of hospital discharge. Neither exposure was associated with either outcome for all groups, but interesting patterns emerged. The construct of neighborhood affluence signals local access to resources—health-promoting or otherwise—that are (a) available in the neighborhood as a direct result of the efforts of influential, highly-educated, prestigious individuals in that community who worked to attract such resources to the neighborhood, and (b) can benefit all residents, regardless of individual-level socioeconomic status (Browning and Cagney 2003). Thus, we anticipated that local resources could potentially play an important role for EBF in particular, as it is the optimal but more intensive feeding practice. Indeed, our findings showed that higher levels of neighborhood affluence increased the odds of EBF for Hispanic and White women. Neighborhood disadvantage, on the other hand, posed an additional burden for EBF practice among Black and Hispanic women. In terms of any breastfeeding, neighborhood disadvantage hindered the odds for Hispanic women, which was consistent with the findings for EBF. For Black women, neighborhood disadvantage did not pose an additional burden, although breastfeeding rates were low in this group (see Table 1). However, residing in a resource-rich area (in terms of higher levels of neighborhood affluence) seemed to benefit groups with comparatively low rates of breastfeeding (Black and Asian women), and also gave an additional boost to White women, a group with a comparatively higher rate of breastfeeding.
These results indicate that the increased resources associated with more affluent neighborhoods can benefit groups with low (average) rates of any breastfeeding. However, given the structural barriers that non-white women face (Kulka et al. 2011; Lind 2014), we speculate that access to such resources may be insufficient to counteract other difficulties (such as group-specific social norms guiding breastfeeding practices). In terms of neighborhood disadvantage, these results suggest that this factor can be a powerful determinant particularly for exclusive breastfeeding practices, likely given its constructs related to low income, which can affect breastfeeding practices (DHHS 2011). In addition, low-income minority women have reported a lack of support in social, work and cultural environments in addition to barriers related to language, literacy, and access to information (Jones et al. 2015).
This study demonstrates the complex interplay between neighborhood affluence and disadvantage, race-ethnicity, and breastfeeding practices. Separating the optimal breastfeeding practice (exclusive) from any breastfeeding provides important information for breastfeeding promotion and support through the different associations with neighborhood disadvantage and affluence for each race-ethnic group, although women who exclusively breastfed comprised nearly half of the group that did any breastfeeding. Regardless of neighborhood affluence, each additional increment of neighborhood disadvantage may have associated effects that discourage Hispanic women who want to breastfeed, and all non-White women who want to exclusively breastfeed. The positive association between neighborhood disadvantage and any breastfeeding among White women is puzzling on the surface, until one considers the persistent structural racism in service provision (Evans et al. 2011; Lind et al. 2014). Controlling for neighborhood disadvantage, neighborhood affluence may benefit only White women’s breastfeeding practices overall, in addition to Hispanic women who want to exclusively breastfeed, and to Black and Asian women who want to do some (but not exclusive) breastfeeding.
Other factors related to lack of supportive services likely affect breastfeeding practices for women living in disadvantaged neighborhoods. While nearly half of U.S. infants participate in the WIC program, breastfeeding rates have been found to be substantially lower for WIC infants (U.S. Government Accountability Office (GAO) 2006). Some infant formula marketing uses the trademarked WIC acronym, and, although states are required to restrict this practice, most do not (GAO 2006). This practice is particularly egregious in light of the fact that suboptimal breastfeeding practices have been cited as both an outcome and cause of intergenerational health and social disparities (University of Sheffield 2016; Bolling et al. 2007). However, given its widespread use, the WIC program presents an opportunity for community-based breastfeeding support and should be reviewed at national, state, and local levels to ensure that optimal support is provided to all women. In addition, as more hospitals seek “Baby-Friendly” designation, they may need to liaise with community-based breastfeeding support services in order to have referral options for women at the time of discharge (Baby-Friendly USA 2012).
Critiques of studies of neighborhood effects on health have been discussed (e.g., Oakes 2004). We controlled for factors related to selection into neighborhoods including individual-level socioeconomic status, but undoubtedly some confounding remains, possibly related to social network and support functions independent of individual-level socioeconomic status. We considered individual attributes to confound the association between neighborhood disadvantage and affluence with breastfeeding practices, and controlling for those variables was consistent with extant literature (Burdette 2013; Cubbin et al. 2008). However, some suggest that individual attributes may mediate, rather than confound, neighborhood effects on health (Glass and Bilal 2016). If that is true, then we may have underestimated these associations.
Study limitations include the possibility that the census tract in which one resides does not reflect one’s perceived neighborhood, although census units have been found to be reasonable proxies for neighborhoods (O’Campo and O’Brien Caughy 2006). Birth certificates are subject to limitations related to record keeping, including mis-specification of variables like race and ethnicity, and some misclassification of our outcome variables is likely. These data are from 2006; however, breastfeeding practices at the time of hospital discharge have not increased substantially in New Jersey (EBF: 37.6% and any breastfeeding: 76.7% in 2015; New Jersey State Health Assessment Data 2017), thus we believe that our conclusions remain valid. By design, our study does not permit examination of breastfeeding practices when women return to their homes and neighborhoods, but the timing of our outcome measures (at hospital discharge) means that the outcomes likely represent prenatal influences on breastfeeding intention (including neighborhood influences) in addition to individual, familial, and hospital attitudes and practices in the immediate postpartum period. Potential effect modifiers or mediators—including prenatal care (frequency, quality), place of delivery (home, birth center or hospital), WIC status and infant health conditions that affect breastfeeding—deserve further research in terms of their associations with neighborhood socioeconomic environment and breastfeeding practices.
In conclusion, both neighborhood disadvantage and affluence were associated with breastfeeding practices, and there were unique associations for each practice by race-ethnicity. Given that increasing levels of neighborhood disadvantage decrease the odds of EBF for nonwhite women, further research and targeted support is needed for those women living in economically depressed neighborhoods. This could take the form of visibility and social marketing events in communities, and home visits, which may encourage exclusive breastfeeding (Yonemoto et al. 2013). Other interventions could include increasing access to the supportive services that may exist in wealthier neighborhoods, and removing incentives to use infant formula (Kent 2006). Neighborhood affluence had a positive association with any breastfeeding for Asian, Black and White women, as well as a positive association with exclusive breastfeeding for Hispanic and White women. Thus, if the supportive resources that likely exist in more affluent neighborhoods could be replicated in all neighborhoods, greater gains in breastfeeding may be observed. Furthermore, future work should seek to ensure that these resources are accessible to all women. Supportive services should be reviewed and expanded to ensure universal access.
Conclusions for Practice
This study underscores the importance of considering neighborhood socioeconomic conditions in efforts to increase optimal breastfeeding practices among all women, while acknowledging that challenges may differ by race-ethnicity. Health disparities across the life course may be perpetuated by modifiable neighborhood attributes, such as access to supportive services, that disproportionately affect women living in poor neighborhoods where the environment discourages optimal breastfeeding practices. More research is needed about specific mechanisms operating in poor, and affluent, neighborhoods for the different race-ethnic groups living within. Those mechanisms likely include access to supportive services and social norms, and interventions to address those factors should be tested.
References
American Academy of Pediatrics Section on Breastfeeding Medicine. (2012). Breastfeeding and the use of human milk. Pediatrics, 129, e827–e841.
Baby-Friendly USA (2012). The ten steps to successful breastfeeding. Accessed October 5, 2017 from https://www.babyfriendlyusa.org/about-us/baby-friendly-hospital-initiative/the-ten-steps.
Beal, A. C., Kuhlthau, K., & Perrin, J. M. Breastfeeding advice given to African American and white women by physicians and WIC counselors. (2003). Public Health Reports 118, 368–376.
Bentley, M. E., Dee, D. L., & Jensen, J. L. (2003). Breastfeeding among low income, African-American women: Power, beliefs and decision making. Journal of Nutrition, 133(1), 305S–309S.
Bolling, K., Grant, C., & Hamlyn, B. (2007). Infant feeding survey 2005. London: The Information Centre for Health and Social Care.
Browning, C. R., & Cagney, K. A. (2003). Moving beyond poverty: Neighborhood structure, social processes, and health. Journal of Health and Social Behavior, 44(4), 552–571.
Burdette, A. (2013). Neighborhood context and breastfeeding behaviors among urban mothers. Journal of Human Lactation, 29(4), 597–604.
Centers for Disease Control and Prevention. (2016). Breastfeeding Data. Accessed November 16, 2016 from http://www.cdc.gov/breastfeeding/data/nis_data/.
Cohen, R., Mrtek, M. B., & Mrtek, R. G. (1995). Comparison of maternal absenteeism and infant illness rates among breast-feeding and formula-feeding women in two corporations. American Journal of Health Promotion, 10, 148–153.
Cubbin, C., Marchi, K., Lin, M., Bell, T., Marshall, H., Miller, C., et al. (2008). Is neighborhood deprivation independently associated with maternal and infant health? Evidence from Florida and Washington. Maternal and Child Health Journal, 12, 61–74.
Declercq, E., Labbok, M. H., Sakala, C., & O’Hara, M. (2009). Hospital practices and women’s likelihood of fulfilling their intention to exclusively breastfeed. American Journal of Public Health, 99(5), 929–935.
DGirolamo, A., Thompson, N., Martorell, R., Fein, S., & Grummer-Strawn, L. (2005). Intention or experience? Predictors of continued breastfeeding. Health Education and Behavior, 32(2), 208–226.
Evans, K., Labbok, M., & Abrahams, S. (2011). WIC and breastfeeding support services: Does the mix of services offered vary with race and ethnicity? Breastfeeding Medicine, 6(6), 401–408.
First Food Friendly. (2012). First food desert infographic. Accessed November 16, 2016 from http://befirstfoodfriendly.org/what-is-a-first-food-desert/.
Glass, T. A., & Bilal, U. (2016). Are neighborhoods causal? Complications arising from the ‘stickiness’ of ZNA. Social Science and Medicine, 166, 244–253.
Grummer-Strawn, L., & Rollins, N. (2015). Summarising the health effects of breastfeeding. Acta Pediatrica, 104(S467), 1–2.
Jones, K. M., Power, M. L., Wueenan, J. T., & Schulkin, J. Racial and ethnic disparities in breastfeeding. (2015). Breastfeeding Medicine, 10(4), 186–196.
Kane, J. B., Miles, G., Yourkavitch, J., & King, K. (2017). Neighborhood context and birth outcomes: Going beyond neighborhood disadvantage, incorporating affluence. Social Science and Medicine Population Health, 3, 699–712.
Kaufman, L., Deenadayalan, S., & Karpati, A. (2010). Breastfeeding ambivalence among low-income African American and Puerto Rican women in north and central Brooklyn. Maternal and Child Health Journal, 14, 696–704.
Kawachi, I., & Berkman, L. (2003). Neighborhoods and health. New York: Oxford University Press Inc.
Kent, G. (2006). WIC’s promotion of infant formula in the United States. International Breastfeeding Journal, 1, 8–10.
Kulka, T. R., Jensen, E., McLaurin, S., et al. (2011). Community based participatory research of breastfeeding disparities in African American women. Infant Child and Adolescent Nutrition, 3, 233–239.
Lind, J. N., Perrine, C. G., Li, R., Scanlon, K. S., & Grummer-Strawn, L. M. (2014). Racial disparities in access to maternity care practices that support breastfeeding—United States, 2011. Morbidity and Mortality Weekly Report, 63(33), 725–728.
McKinney, C. O., Hahn-Holbrook, J., Chase-Lansdale, P. L., Ramey, S. L., Krohn, J., Reed-Vance, M., et al. (2016). Racial and ethnic differences in breastfeeding. Pediatrics, 138(2), e20152388.
New Jersey State Health Assessment Data. (2017). Health Indicator Report of Feeding at Discharge. Accessed October 9, 2017 from https://www26.state.nj.us/doh-shad/indicator/view/Feeding.Trend.html.
O’Campo, P., & O’Brien Caughy, M. (2006). Measures of residential community contexts. In J. M. Oakes & J. S. Kaufman (Eds.), Methods in social epidemiology (pp. 193–208). San Francisco: Wiley.
Oakes, J. M. (2004). The (mis)estimation of neighborhood effects: casual inference for a practicable social epidemiology. Social Science and Medicine, 58, 1929–1952.
Ryan, A. S., Zhou, W., & Arensberg, M. B. (2006). The effect of employment status on breastfeeding in the United States. Women’s Health Issues, 16(5), 243–251.
Sellström, E., & Bremberg, S. (2006). The significance of neighbourhood context to child and adolescent health and well-being: a systematic review of multilevel studies. Scandinavian Journal of Public Health, 34(5), 544–554.
U.S. Department of Health and Human Services. (2011). The surgeon general’s call to action to support breastfeeding. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General.
U.S. Department of Health and Human Services, Health Services Research Association. (2009). Business case for breastfeeding. Washington, DC: U.S. Department of Health and Human Services, Health Services Research Association.
U.S. Government Accountability Office. (2006). Breastfeeding: some strategies used to market infant formula may discourage breastfeeding; state contracts should better protect against misuse of WIC name. GAO-06-282. Accessed November 20, 2016, from http://www.gao.gov/new.items/d06282.pdf.
University of Sheffield. (2016). Benefits of Breastfeeding. Public Health website. Accessed November 16, 2016, from http://www.shef.ac.uk/scharr/sections/ph/research/breastmilk/benefitsofbreastfeeding.
Vinikoor-Imler, L. C., Messer, L. C., Evenson, K. R., & Laraia, B. A. (2011). Neighborhood conditions are associated with maternal health behaviors and pregnancy outcomes. Social Science and Medicine, 73(9), 1302–1311.
WHO. (2011). Exclusive breastfeeding for six months best for babies everywhere. Media Centre website. Accessed November 20, 2016, from http://www.who.int/mediacentre/news/statements/2011/breastfeeding_20110115/en/.
Yonemoto, N., Dowswell, T., Nagai, S., & Mori, R. (2013). Schedules for home visits in the early postpartum period. Cochrane Database of Systematic Reviews, 7, CD009326.
Acknowledgements
Brian Frizzelle performed the geocoding, linked the data, and created the maps. UNC’s Breastfeeding Umbrella Support Team provided suggestions. Julien Teitler and Nancy Reichman obtained the data. Yourkavitch and Miles were supported in part by the Training Program in Reproductive, Perinatal and Pediatric Epidemiology, (T32-HD52468; Anna Maria Siega-Riz, PI) and by NICHD K99/R00 HD075860 (PI: Kane). Kane was supported by NICHD K99/R00 HD075860.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic Supplementary material
Below is the link to the electronic supplementary material.
10995_2017_2423_MOESM2_ESM.docx
Online Resource 2—Plots of neighborhood disadvantage and affluence indices for urban neighborhoods in New Jersey, by race-ethnicity (DOCX 234 KB)
Rights and permissions
About this article
Cite this article
Yourkavitch, J., Kane, J.B. & Miles, G. Neighborhood Disadvantage and Neighborhood Affluence: Associations with Breastfeeding Practices in Urban Areas. Matern Child Health J 22, 546–555 (2018). https://doi.org/10.1007/s10995-017-2423-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-017-2423-8