Abstract
Purpose To determine whether the delayed recovery often observed in simple musculoskeletal injuries occurring at work is related to poor workplace and home social support. Method A four question psychosocial screening tool called the “How are you coping gauge?” (HCG) was developed. This tool was implemented as part of the initial assessment for all new musculoskeletal workplace injuries. Participants were excluded if they did not meet the strict criteria used to classify a musculoskeletal injury as simple. The HCG score was then compared to the participant’s number of days until return to full capacity (DTFC). It was hypothesised that those workers indicating a poorer level of workplace and home support would take longer time to return to full capacity. Results A sample of 254 participants (316 excluded) were included in analysis. Significant correlation (p < 0.001) was observed between HCG scores for self-reported work and home support and DTFC thereby confirming the hypothesis. Path analysis found workplace support to be a significant moderate-to-strong predictor of DTFC (−0.46). Conclusion A correlation was observed between delayed workplace injury recovery and poor perceived workplace social support. The HCG may be an effective tool for identifying these factors in musculoskeletal workplace injuries of a minor pathophysiological nature. There may be merit in tailoring injury rehabilitation towards addressing psychosocial factors early in the injury recovery process to assist with a more expedient return to full work capacity following simple acute musculoskeletal injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Psychosocial factors can play an influential role in workplace injury causation and rehabilitation [1]. Those workers with poorer symptom self-coping and poorer perceived social supports often demonstrate prolonged workplace injury recovery time following simple acute musculoskeletal injuries [2]. Strong strength correlations have been observed between poor perceived workplace social support and work absenteeism due to injury [3]. Likewise, workers who have negative expectations about their return to work take a more prolonged actual time to recover, than those workers with positive expectations about return to work [4]. Promoting positive return to work expectations through education may be effective at reducing time off work due to workplace injury [5]. In regards to the home domain, poor home domain social support has also been postulated to be a potential factor in prolonging rehabilitation time following workplace injury [6]. Overall, there is a strong body of evidence supporting the correlation between poor work domain social support and prolonged return to work, but more research needs to be conducted regarding poor home domain social support and prolonged workplace injury recovery [7].
The normal pathophysiological healing timeframe for simple musculoskeletal injuries, such as muscle strains, ligament sprains or contusions, has been established. For a contusion, the normal healing timeframe has been measured to be an average of 24 days [8]. For a muscle strain, 90% of physical function has been measured to return by no later than 42 days [9]. Despite these consistent timeframes, simple musculoskeletal injuries when sustained at work will often demonstrate prolonged recovery timeframes possibly because of psychosocial factors influencing the worker’s recovery [1]. Given the link between psychosocial factors and delayed workplace injury recovery time, importance has been placed on the early detection of these psychosocial factors so that these injuries can be managed more effectively [10]. By alerting the treating medical team to the presence of these factors early in the rehabilitation process, treatment could be tailored to mitigate these factors, potentially resulting in a more expedient recovery and return to work [11]. By doing so, costs associated with workers’ compensation insurance claims could be reduced, potentially reducing the overall economic cost of workplace injuries [12, 13].
Screening tools are one such way of identifying factors that may be impacting normal injury recovery. There is no one screening tool that exists which can capture all factors that may be contributing to persistent pain in musculoskeletal injury in a time efficient manner with tools taking anywhere from a few minutes to 30 min to administer [14]. This prolonged time to administer was the largest barrier reported by physiotherapist to the more frequent implementation of screening tools in the clinic environment [15]. From a population of 1000 randomly selected physiotherapists across the United States, 73% of responders reported that the extended time required to administer these tools was the biggest barrier to consistent implementation. Of all responders, only 48% reported utilising screening tools as part of standard physiotherapy practice, further emphasising time as a barrier to implementation.
Return to Work SA (RTWSA), the body responsible for administering and regulating the workers compensation scheme within South Australia, require treating allied health therapists to use validated screening tools to measure their patient’s progress, and recommend the Orebro Musculoskeletal Pain Questionnaire (OMPQ) as an appropriate tool for monitoring psychosocial factors in workplace injury [16]. The OMPQ is a 21 item questionnaire taking approximately 10 min to administer, and was initially validated in a primary health care low back injury population [17]. The OMPQ was subsequently validated in a workers’ compensation environment for workplace injuries regardless of body area injured [18]. In this workplace injury population the OMPQ was able to identify those workers at risk of prolonged absence from work when the tool was administered between 4 and 12 weeks post initial injury. Given that addressing the psychosocial factors which are complicating a musculoskeletal injury can significantly reduce worker absence, and that having an allied health therapist visit a workplace can reduce the length of time a worker is absent from work, importance should be placed on identifying these psychosocial factors even earlier in the rehabilitation process, perhaps even as early as the initial assessment of the injured worker [19, 20]. However, in order to improve allied health therapists utilisation of screening tools, this early identification of psychosocial factors should be done using tools that are valid and time feasible.
In an effort to reduce the time constraints of administering the OMPQ, and improve therapist utilisation of the screening tool, a short form 10 question OMPQ was validated against the OMPQ in a combined occupational injury and primary health care setting [21]. This short form of the OMPQ was also shown to have good predictive validity when administered 4–12 weeks post initial injury. It is unknown whether the predicative validity of the short form OMPQ is equally valid when administered during the therapist’s initial assessment of the worker. Despite the improvement in time feasibility of the short form OMPQ over the original OMPQ, clinicians still regard those outcome measures currently available to take too much time to implement in the busy clinic environment [22]. Therefore there may be merit in identifying whether an even more time practical screening tool is effective at identifying psychosocial factors when administered during the initial assessment of an injured worker in a workers’ compensation environment.
We aim to determine whether a concise four-question psychosocial screening tool taking less than 1 min to administer is effective at predicting simple musculoskeletal injury recovery timeframe in a workers’ compensation environment. This tool developed by the authors is modelled on the common thematic components of the OMPQ given the large body of evidence validating this tool. Strict inclusion and exclusion criteria are defined to capture the sample of musculoskeletal injuries that are of an acute sprain, strain, or soft tissue nature with a generally quick pathophysiological repair timeframe [23]. By doing so, we hope to identify whether early identification of psychosocial factors can predict which workers are susceptible to a prolonged injury rehabilitation timeframe following simple musculoskeletal injury. From this, rehabilitation for at risk workers could be tailored towards improving injured worker’s perception of workplace and home domain social supports, in order to expedite the worker’s return to full capacity [24].
We hypothesise that the lower the workers’ self-reported workplace and home social support coping scores are, the longer their injury rehabilitation timeframe will be. Observing a relationship between these factors may then help to explain the prolonged recovery time often observed in workers who have a physiologically minor injury [25]. A summary of the hypotheses are as follows:
H1
The level of social support from the workplace will be a significant negative predictor of time taken to return to full capacity at work; and
H2
The level of support from the home domain will be a significant negative predictor of time taken to return to full capacity at work.
To summarise, it is expected that those workers reporting a poorer perceived level of workplace and home social support will take a longer period of time to return to full work capacity.
Method
An observational cohort study design was used with ethics approval being granted by the University of South Australia’s Human Research Ethics Committee prior to commencement of the study. Patients provided written consent before being treated by a physiotherapist at one of three Corporate Health Group (CHG) physiotherapy locations within South Australia. CHG primarily service referrals through the RTWSA workers’ compensation scheme. Patients came from a wide variety of occupational areas with varying degrees of physical job demands, ranging from customer service officers to manual labourers. The authors designed a tool called the ‘How are you Coping Gauge?’ (HCG). It was incorporated into the standard physiotherapy initial assessment protocol across CHG’s physiotherapy departments. The tool requires the therapist to read a brief paragraph explaining the use and purpose of the tool. Four questions are asked regarding how the patient is coping, in which the patient verbally responds with a score from “0” to “10”; “10” indicating a response of “very well” and “0” indicating “not at all”. The four questions of the HCG are:
(1) How well are you coping with your symptoms?
(2) How supported do you feel by your workplace, co-workers and managers?
(3) How safe and supported do you feel by your family, friends and finances?
(4) How confident are you that you will return to your normal work duties?
These four questions were developed from the common thematic components of the Orebro Musculoskeletal Pain Questionnaire (OMPQ) given that the OMPQ has good predictive validity [26]. The HCG attempts to identify major psychosocial factors in a time feasible manner, taking approximately 1 min to administer. Clear attention was paid in phrasing the questions to avoid reinforcing the theme of ‘pain’ in the tool as evidence has shown ‘painful words’ may have an inflammatory effect on a patient’s perception of their injury [27–29].
The scores for each of the four questions were then compared to the number of days between the workers first contact with the treating physiotherapist (the initial assessment) and the day of certification to full work capacity deemed by the worker’s treating medical practitioner. This period of time was termed ‘days to full capacity’ (DTFC). The patients were unaware that their HCG score would be compared to their DTFC. This data were collected for all initial physiotherapy patients presenting for musculoskeletal work injury rehabilitation, over a one year period between July 2015 and July 2016. These patients underwent standard physiotherapy care [30].
This data was then assessed for eligibility by an independent physiotherapist to determine their inclusion as simple musculoskeletal injuries. Data were excluded if the initial consult with the physiotherapist was not within 7 days of the patients reported date of injury. By doing so we hoped to capture a population of injuries still within the acute stage of healing [31–34]. Considering the evidence for central sensitisation, data were also excluded where patients reported sustaining a previous injury to the same body area [35]. Additionally, a worker’s psychosocial coping state may be amplified by particularly traumatic injuries [36]. To avoid this confounding variable, data containing any radiographically confirmed fracture, ligament, or cartilage injury, including injuries that required surgical opinion were also excluded.
Data analysis was performed by an independent Research Associate. A total of 254 participants were included in the analysis, with 316 participants being excluded based on the exclusion criteria above. Given that the proportion of workers compensation injury claims in Australia is significantly higher in the male population (63%) compared to the female population (37%) it was anticipated that there would be more male (n = 172) than female participants (n = 82) [37]. Injured body area was generated by categorising the injury into one of three groups: (1) trunk (e.g., back, neck); (2) lower limb (e.g., ankle, knee, foot), and; (3) upper limb (e.g., shoulder, elbow, hand). Statistical analysis showed no significant difference (95% CI) between male and female participants for demographic characteristics of age, individual HCG question score, number of physiotherapy treatment sessions, DTFC, and overall HCG score per body area injured (Table 1). Thus data for both male and female populations were pooled for analysis.
Results
Correlations
Partial correlations were conducted to identify whether relationships existed between variables of interest, namely: work support (social support received from work colleagues and supervisors); home support (support received from family, friends, and financial situation); and days to return to full capacity (DTFC) as certified by the treating medical practitioner. Age, gender, and injured body area were all controlled for in the analysis.
Analysis showed a clear significant negative correlation between both self-reported work and home support, and the objective archival data on number of DTFC, such that the length of time required to return to work decreases as the level of social support increases from the work (−0.58***) and family domains (−0.25***). The relationships are significant despite controlling for the effects of demographic and injured body area variables, indicating that there may be an effect between social supports and return to full capacity that is worthy of further investigation.
Model Testing
Path analysis was conducted using Structural Equation Modelling in AMOS 21.0, in order to test the hypothesis that; H1: the level of social support from the workplace will be a significant negative predictor of time taken to return to full capacity, and likewise; H2: the level of support from the home domain will be a significant negative predictor of time taken to return to full capacity [38]. The decision was made to include all variables in a statistical model simultaneously, given that the two support variables and DTFC are correlated significantly. Further, the return to full capacity variable is likely to also be related to how well the patient is coping with their symptoms as well as their self-assessed confidence with returning to full duties. The advantage of including all of these variables in the same model is to see how all factors interact simultaneously, and avoid measuring shared variance (in separate analyses), giving us a more accurate picture of how factors come together to predict return to full capacity. Further, we can control for the influence of age, gender, and injured body area on the prediction of the outcome variables.
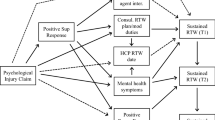
The statistical model is presented in Fig. 1, which shows support for H1, with DTFC being predicted significantly by work support (−0.46***) and also by home support (−0.11*) as per H2. According to Cohen’s gauge of relationship strength (0.10 = weak; 0.30 = moderate; 0.50 = strong), work support is a stronger predictor of time taken to return to return to full capacity (moderate-strong negative predictor), than home support (weak negative predictor) [39]. Both types of social support are robust predictors despite controlling for age, gender, and body area injured. There was no significant relationship between these controls and work support. Controlling for injury type in the model is important, as it appears that the area of the body that is injured affects the amount of social support received at home (0.13*), and of course is related to the speed of recovery in the form of time taken to return to full capacity (0.12*). It is interesting to note however that age in specific displayed a significant weak negative relationship with home support (−0.12**). It is intuitive to suggest that the older the participant, the less likely they are to have access to familial social support, especially given the mean age for the sample was 37.8 years, and clients older than this may start to experience children leaving home or otherwise begin to feel isolated.
Model predicting return to work via confidence in returning, individual coping, work and home support (controlling for demographics and injured body area). *p < 0.05; ***p < 0.001; as the exogenous predictor variables, correlation lines were drawn between confidence in returning, age, gender, injury type, and individual coping (not depicted for ease of interpretation)
Further, the model depicted in Fig. 1 also controls for individual coping. We would expect that the degree to which the client is individually coping with their symptoms would be related to DTFC, and could suppress the effect of social supports in return to work. However, there is no significant relationship between individual coping with symptoms and the time taken to return to full capacity, suggesting that social supports play a considerable role in return to full capacity over and above individual coping.
The model also includes the client’s confidence in returning to full capacity as a lead predictor of actual return to work. It is evident that individual confidence in returning to full capacity is a weak-moderate negative predictor of time taken to return to full capacity (−0.24***). A mediation process is also present, whereby the relationship between a client’s confidence in returning is mediated by the strength of their social supports (both work and home); so a client may be confident they will return to full capacity in appropriate time, however the better the work and home supports they have access to, the faster that client may actually return to full capacity at work. This is shown in the significant indirect effect of confidence in returning to full capacity on the actual DTFC variable via both work and home supports (−0.12); CI 95% at LL = −0.167, UL = −0.084, p < 0.01 (Bias-corrected percentile using the Monte Carlo parametric bootstrap method).
Discussion
To the authors knowledge, this is the first study conducted that has investigated a worker’s self-reported coping perceptions against the hard outcome variable of actual time taken to return to full capacity (DTFC; days to full capacity). Most importantly, the ‘moderate’ strength relationships found in this study aren’t commonly found in large model studies that link data from separate attainment sources (self-reported to archival in this study). As with any observational cohort study design in psychosocial health research, care must be taken when interpreting results as any identified relationship is correlational not causational [40]. Within this context, the relationships identified between social support and prolonged simple musculoskeletal workplace injury recovery appear worthy of notice.
Within a workers’ compensation environment, the results of our study suggests that those simple musculoskeletal injuries which take longer than the normal pathophysiological healing timeframe to recover could potentially be explained by poor workplace or home social support. Interestingly, social supports were more closely related to DTFC than an individuals perceived level of coping with their injury. Therefore, the treating health professionals, family, co-workers and managers may need to change the questions they use when inquiring about a worker’s simple musculoskeletal injury self-coping away from focusing on the injury symptoms and towards inquiring about their perceived workplace and home social support. Rather than asking “how are you going with your injury?” the more pertinent questions may be “how can I help support you more at work?” or “what can I do to help support you at home?” By doing so it may be possible to shift the responsibility away from the injured individual and that individual’s ability to build their own injury coping resilience. Instead the responsibility would be shared with those people who make up the surrounding society for that worker. Supportive social societies foster greater levels of health and well-being [41]. Therefore, this change in questioning and shift in responsibility is likely to create a more recovery conducive social network and improve the worker’s perceived level of workplace and home social support.
The workers’ compensation system within Australia already encourages a multidisciplinary approach to injury rehabilitation by facilitating the involvement of early physiotherapy treatment for musculoskeletal injuries. Within the South Australian scheme, recent changes in legislation have prompted the treating physiotherapist to become more engaged in the return to work process, through workplace visits where therapists can liaise with their patients in the work environment, and negotiate onsite with managers or recommend interventions to assist the injury recovery process [42, 43]. Early identification of poor perceived workplace social support could act as a prompt for the treating physiotherapist to perform a workplace visit within the first week of a simple musculoskeletal injury occurrence rather than waiting until a problem arises down the track. Likewise, identifying poor home support early could prompt the medical practitioner to arrange for an occupational therapist to do a thorough assessment of the worker’s home environment and home support system promptly rather than waiting until the need arises later on in the rehabilitation process. Engaging these services are generally an inevitable part of the workplace injury rehabilitation process, but organising these services more promptly during the injury claim may allow for reduced overall injury rehabilitation timeframes, with issues being addressed earlier, and workers needing less time to return to full capacity at work following simple musculoskeletal injury.
According to the correlations observed in our study, poor workplace support appears to be more significantly correlated with delayed return to full capacity following simple musculoskeletal injury over that of poor home domain support. Assisting with home support may fall outside the bounds of the capabilities of a worker’s manager and co-workers. However, the results of our study suggest that managers and co-workers are in the best position possible to aid an injured worker’s recovery via workplace social support. Previous evidence has shown that a workplace that promotes a supportive workplace environment and safety culture, as reported by the workers, have lower injury rates than those workplaces whose workers do not feel their workplace environment is supportive [44]. This study supports previous speculation that a workplace which maintains a supportive environment, may benefit from fewer injuries being sustained as well as reduced injury recovery timeframes, resulting in improved individual wellbeing as well as reduced financial impact to the organisation [45–47]. It is therefore important that workplaces take note of this expanding body of research and actively engage in creating and maintaining a supportive workplace environment.
It is interesting to note that our study identified a correlation between older injured workers and poorer levels of home domain social support in simple acute musculoskeletal injury. To maintain a holistic approach to workplace injury management, it may be important for governing bodies and society as a whole to recognise that those older injured workers could potentially need more assistance when it comes to social support in the home domain. Past evidence has portrayed a possible link between older patients and longer workplace injury recovery timeframes from a pathophysiological level [48]. Other research suggests social isolation delays the musculoskeletal injury healing timeframe [49, 50]. The results from our study appear to support these conjectures, highlighting that home domain social support may be an important factor in simple musculoskeletal injury recovery and should be promptly addressed particularly in the older working population. If future research identifies a causal relationship between older workers and poor home domain social support, as a governing body, it may be worth placing importance on the provision of medical services and home support services to the older working population. This could involve a case by case consideration of Home and Activities of Daily Living Assessments for those workers who live in isolation, and the subsequent organisation and provision of active home assistance programs.
Although our methodology was purely quantitative rather than qualitative or a mixed methods approach, consulting already established qualitative findings may assist us in determining the value of the relationships identified in our quantitative data [51, 52]. As such we can draw on the current body of qualitative literature to speculate on the potential meaning of the correlational relationships identified in our study.
Workplace injury has been shown to have a negative impact on interpersonal relationships within both the workplace and home domain [53]. This qualitative research lends support for our rationale behind the creation and implementation of our HCG screening tool, as a method of identifying the presence of poor social supports in the individual. As such improving workplace and home domain social supports by way of the strategies recommended in our study may be an effective way to assist with the return to work process of an individual.
Similarly, qualitative investigation has identified the feeling of powerlessness felt by the injured worker due to not being involved and consulted in the rehabilitation process [54]. Workers have reported feeling like victims not only to the injury but to the workers’ compensation system, highlighting that there is undue pressure isolated on the individual to get well and to get back to work quickly. This data adds support to our recommendations of sharing the responsibility of injury recovery between all parties involved in the rehabilitation process, including the worker’s managers, co-workers, family, friends, treating allied health therapists, medical practitioners, insurance claim managers and return to work co-ordinators. Furthermore, some workers felt more impeded than aided by their treating allied health therapists, medical practitioners, claim managers and return to work co-ordinators in returning to work [54]. This was expressed to be due to the worker not feeling adequately supported by these parties, and not feeling like they were adequately consulted or involved in the decisions made during their rehabilitation. Another study has highlighted that the psychosocial factors present in an injured worker may also be due to organisational and systemic issues, which could be reduced if the worker were more involved at every stage of their rehabilitation, and consulted for their opinion in regards to appropriateness of workplace light duties and graduated return to work programs [55]. This qualitative literature highlights the importance of involving the injured work in every step of the rehabilitation process and decision making. By doing so the worker may be empowered to take control of their rehabilitation whilst also potentially improving the worker’s perception of the extent of social support being provided by those involved in their care.
A mixed-methods study identified a superior overall well-being reported in workers who perceived their workplace to be attending to their individual needs, and when they were perceived to have good social support from the interpersonal relationships with their co-workers and managers [56]. This evidence lends support to the correlation observed in our study between good perceived work support and more expedient return to work. As such our recommendation on the importance of employers improving their workplace social supports may have merit.
Limitations
The findings of this study should only be considered within the bounds of those limitations innate to observational cohort study designs [40]. Thus, despite the ‘moderate’ strength relationships identified in our study, and given that our methodology was purely quantitative it is important to take note that any connection is still correlational not causational and any direction of association is only speculation. Nevertheless the relationships identified in our study are consistent with current qualitative literature in this research field and attention may still be warranted.
The directive of this study was to identify whether psychosocial factors play a role in the prolonged injury recovery timeframe observed in those workplace injuries of a relative pathophysiological minor or simple nature. Due to this, strict and substantiative exclusion criteria were instated to ascertain only a population of simple acute musculoskeletal injuries. All non-physical workplace injury compensation claims were also excluded. The findings of our study can only be considered within this subset population of simple acute musculoskeletal injuries. Any correlations identified will not apply to injuries that are non-workplace, complex musculoskeletal, highly traumatic, solely psychological, mental stress related, chronic, or aggravations of previous injuries. The speculated relationship between psychosocial factors and workplace injuries in these populations of injuries still needs to be investigated. Therefore further study should be conducted to explore the relationship between perceived social supports and workplace injury regardless of the history or nature of the injury.
This study could also not control for workers requesting an early medical clearance, possibly due to potential psychosocial or economic factors, prior to their injury fully resolving. Although this is only estimated to be a very small subset of injured workers, and therefore only a small effect on DTFC, it should still be highlighted as a potential confounding variable. Therefore, the recommendations made in our study should only be considered within this overall context.
Conclusion
This study looked to identify a correlation between psychosocial factors and prolonged injury recovery time in simple acute musculoskeletal injuries. The correlations found in our study highlight the potential relationship between poor perceived workplace and home domain social support and prolonged injury recovery timeframe, a notion that is commonly discussed in both quantitative and qualitative literature in this field. The screening tool developed for this study appears to be an effective means of identifying these social support factors in simple acute musculoskeletal injuries. Given the correlations found in our study and their consistency with past qualitative findings, addressing these psychosocial factors early may potentially improve the speed of return to full capacity at work following a simple musculoskeletal injury. However it has yet to be determined whether these correlations are also present in workplace injuries that are chronic, complex, or non-physical in nature. It is important that further study is conducted in this area in order to advance our understanding of the role that social supports play in their relationship to an injured worker’s return to full capacity within the workers’ compensation environment.
References
Bailey TS, Dollard MF, McLinton SS, Richards, PAM. Psychosocial safety climate, psychosocial and physical factors in the aetiology of musculoskeletal disorder symptoms and workplace injury compensation claims. Work Stress. 2015;29(2):190–211.
Heymans MW, de Vet HCW, Knol DL, Bongers PM, Koes BW, Mechelen WV. Workers’ beliefs and expectations affect return to work over 12 months. J Occup Rehabil. 2006;16(4):685–695.
Dunstan DA, Covic T, Tyson GA. What leads to the expectation to return to work? insights from a theory of planned behavior (TPB) model of future work outcomes. Work. 2013;46(1):25–37.
Cole DC, Mondloch MV, Hogg-Johnson S. Listening to injured workers: how recovery expectations predict outcomes—a prospective study. Can Med Assoc J. 2002;166(6):749–754.
Godges JJ, Anger MA, Zimmerman G, Delitto A. Effects of education on return-to-work status for people with fear-avoidance beliefs and acute low back pain. Phys Ther. 2008;88(2):231–239.
Lysaght RM, Larmour-Trode S. An exploration of social support as a factor in the return-to-work process. Work. 2008;30(3):255–266.
Hoogendoorn WE, van Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine. 2000;25(16):2114–2125.
Crisco JJ, Jokl P, Heinen GT, Connell MD, Panjabi MM. A muscle contusion injury model: biomechanics, physiology, and histology. Am J Sport Med. 1994;22(5):702–710.
Askling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. Brit J Sport Med. 2006;40(1):40–44.
Sullivan M, Feuerstein M, Gatchel R, Linton S, Pransky G. Integrating psychosocial and behavioral interventions to achieve optimal rehabilitation outcomes. J Occup Rehabil. 2005;15(4):475–489.
Schultz IZ, Crook J, Berkowitz J, Milner R, Meloche GR. Predicting return to work after low back injury using the psychosocial risk for occupational disability instrument: a validation study. J Occup Rehabil. 2005;15(11):365–376.
Nicholas MK, Linton SJ, Watson PJ, Main CJ. Early identification and management of psychological risk factors (“yellow flags”) in patients with low back pain: a reappraisal. Phys Ther. 2011;91(5):1–17.
Wall C, Ogloff JP, Morrissey S. The psychology of injured workers: health and cost of vocational rehabilitation. J Occup Rehabil. 2006;16(4):513–528.
Grimmer-Somers K, Vipond N, Kumar S, Hall G. A review and critique of assessment instruments for patients with persistent pain. Journal of pain research. 2009;2(2):21–47.
Jette DU, Halbert J, Iverson C, Micheli E, Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009;89(2):125–135.
WorkSafe Victoria. Clinical framework for the delivery of health services. Melbourne: WorkSafe Victoria; 2012. p. 24.
Linton SJ, Halldén K. Can we screen for problematic back pain? A screening questionnaire for predicting outcome in acute and subacute back pain. Clin J Pain. 1998;14(3):209–215.
Dunstan DA, Covic T, Tyson GA, Lennie IG. Does the Örebro Musculoskeletal Pain Questionnaire predict outcomes following a work-related compensable injury? Int J Rehabil Res. 2005;28(4):369–370.
Arnetz BB, Sjögren B, Rydéhn B, Meisel R. Early workplace intervention for employees with musculoskeletal-related absenteeism: a prospective controlled intervention study. J Occup Environ Med. 2003;45(5):499–506.
Franche RL, Severin CN, Hogg-Johnson S, Côté P, Vidmar M, Lee H. The impact of early workplace-based return-to-work strategies on work absence duration: a 6-month longitudinal study following an occupational musculoskeletal injury. J Occup Environ Med. 2007;49(9):960–974.
Linton SJ, Nicholas M, MacDonald S. Development of a short form of the Örebro Musculoskeletal Pain Screening Questionnaire. SPINE. 2011;36(22):1891–1895.
Duncan EA, Murray J. The barriers and facilitators to routine outcome measurement by allied health professionals in practice: a systematic review. BMC Health Serv Res. 2012;12(1):96.
Järvinen TAH, Järvinen TLN, Kääriäinen M, Kalimo H, Järvinen M. Muscle injuries: biology and treatment. Am J Sport Med. 2005;33(5):745–764.
Shain M, Kramer DM. Health promotion in the workplace: framing the concept; reviewing the evidence. Occup Environ Med. 2004;61(7):643–648.
MacEachen E, Kosny A, Ferrier S, Chambers L. The “toxic dose” of system problems: why some injured workers don’t return to work as expected. J Occup Rehabil. 2010;20(3):349–366.
Hockings RL, McAuley JH, Maher CG. A systematic review of the predictive ability of the Orebro Musculoskeletal Pain Questionnaire. SPINE. 2008;33(15):E494–E500.
Minden P. The importance of words: suggesting comfort rather than pain. Holist Nurs Pract. 2005;19(6):267–271.
Eck J, Richter M, Straube T, Miltner WHR, Weiss T. Affective brain regions are activated during the processing of pain-related words in migraine patients. PAIN. 2011;152(5):1104–1113.
Richter M, Eck J, Straube T, Litner WHR, Weiss T. Do words hurt? Brain activation during the processing of pain-related words. PAIN. 2010;148(2):198–205.
Hertling D, Kessler RM. Management of common musculoskeletal disorders: physical therapy principles and methods. 4th ed. Maryland: Lippincott Williams & Wilkins; 2006.
Dahlgren LA, Mohammed HO, Nixon AJ. Temporal expression of growth factors and matrix molecules in healing tendon lesions. J Orthopaed Res. 2005;23(1):84–92.
Sharma P, Maffulli N. Basic biology of tendon injury and healing. Surg. 2005;3(5):309–316.
Schultz G, Mozingo D, Romanelli M, Claxton K. Wound healing and TIME; new concepts and scientific applications. Wound Repair Regen. 2005;13(s4):S1–S11.
Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37(5):1528–1542.
Woolf CJ. Central sensitization: Implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl):S2–S15.
Zatzick D, Jurkovich GJ, Rivara FP, Wang J, Fan MY, Joesch J, Mackenzie E. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–423.
Safe Work Australia. Australian workers’ compensation statistics 2012-13. Canberra: Safe Work Australia; 2013.
Arbuckle JL. IBM SPSS AMOS 21 user’s guide. Armonk: IBM Corporation; 2012.
Cohen J. Statistical power for the behavioral sciences. 2nd ed. Hillsdale: Erlbaum; 1998.
Taris TW, Kompier M. Challenges in longitudinal designs in occupational health psychology. Scand J Work Environ Health 2003;29(1):1–4.
Karademas EC. Self-efficacy, social support and well-being: the mediating role of optimism. Pers Indiv Differ. 2006;40(6):1281–1290.
Return to Work Act 2014 (SA).
ReturnToWorkSA. Physiotherapy fee schedule and policy. Adelaide (AU): ReturnToWorkSA; 2016. p. 26.
Smith GS, Huang YH, Ho M, Chen PY. The relationship between safety climate and injury rates across industries: the need to adjust for injury hazards. Accid Anal Prev. 2006;38(3):556–562.
Gillen M, Yen IH, Trupin L, Swig L, Rugulies R, Mullen K, Font A, Burian D, Ryan G, Janowitz I. The association of socioeconomic status and psychosocial and physical workplace factors with musculoskeletal injury in hospital workers. Am J Ind Med. 2007;50(4):245–260.
Franche R-L, Krause N. Readiness for return to work following injury or illness: conceptualizing the interpersonal impact of health care, workplace, and insurance factors. J Occup Rehabil. 2002;12(4):233–256.
Shamian J, O’Brien-Pallas L, Thomson D, Alksnis C, Steven Kerr M. Nurse absenteeism, stress and workplace injury: what are the contributing factors and what can/should be done about it? Int J Sociol Soc Policy. 2003;23(8/9):81–103.
Rogers E, Wiatrowksi WJ. Injuries, illnesses, and fatalities among older workers. Mon Labor Rev. 2005;128(10):24–30.
Hermes GL, Rosenthal L, Montag A, McClintock MK. Social isolation and the inflammatory response: sex differences in the enduring effects of a prior stressor. Am J Physiol Regul Integr Comp Physiol. 2006;290(2):R273–R82.
Detillion CE, Craft TKS, Glasper ER, Prendergast BJ, DeVries AC. Social facilitation of wound healing. Psychoneuroendocrino. 2004;29(8):1004–1011.
Onwuegbuzie AJ, Leech NL. Enhancing the interpretation of significant findings: the role of mixed methods research. The Qualitative Report. 2004;9(4):770–792.
Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educational researcher. 2004;33(7):14–26.
Kirsh B, Slack T, King CA. The nature and impact of stigma towards injured workers. J Occup Rehabil. 2012;22(2):143–154.
Beardwood BA, Kirsh B, Clark NJ. Victims twice over: perceptions and experiences of injured workers. Qual Health Res. 2005;15(1):30–48.
Soklaridis S, Ammendolia C, Cassidy D. Looking upstream to understand low back pain and return to work: psychosocial factors as the product of system issues. Soc Sci Med. 2010;71(9):1557–1566.
Chan ANW. Social support for improved work integration: perspectives from Canadian social purpose enterprises. Soc Enterp J. 2015;11(1):47–68.
Funding
All authors declare that no funding was obtained in formation of this body of work.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Conflict of interest
Author Sareen McLinton, Sarven Savia McLinton and Martin van der Linden declare that they have no conflict of interest.
Ethical Approval
This study was submitted to the University of South Australia for ethics review prior to commencement. Our application was reviewed and was considered exempt based on its study design. Therefore approval was given to undertake data collection.
Rights and permissions
About this article
Cite this article
McLinton, S., McLinton, S.S. & van der Linden, M. Psychosocial Factors Impacting Workplace Injury Rehabilitation: Evaluation of a Concise Screening Tool. J Occup Rehabil 28, 121–129 (2018). https://doi.org/10.1007/s10926-017-9701-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-017-9701-6