Abstract
Purpose Organizational-level policies and practices that promote safety leadership and practices, disability management and ergonomic policies and practices are considered key contextual determinants of return to work. Our objective was to examine the role of worker-reported organizational policies and practices (OPPs) in return to work (RTW) and work role functioning (WRF) and the mediating role of pain self-efficacy and work accommodation. Methods A worker cohort (n = 577) in Ontario, Canada was followed at 1, 6 and 12 months post injury. Both RTW (yes/no) and WRF (WLQ-16) status (3 levels) were measured. OPPs were measured (high vs. low) at 1 month post-injury. Pain self-efficacy (PSE) and work accommodation (WA) were included in mediation analyses. Results OPPs predicted RTW at 6 months (adjusted OR 1.77; 95 % CI 1.07–2.93) and 12 months (adjusted OR 2.07; 95 % CI 1.18–3.62). OPPs predicted WRF at 6 months, but only the transition from working with limitations to working without limitations (adjusted OR 3.21; 95 % CI 1.92–5.39). At 12 months, OPPs predicted both the transition from not working to working with and without limitations and from not working or working with limitations to working without limitations (adjusted OR 2.13; 95 % CI 1.37–3.30). Offers of WA mediated the relationship between OPPs and both RTW and WRF at 6 months follow-up. PSE mediated the relationship between OPPs and RTW and WRF at 6 months. At 12 months neither mediated the relationship. Conclusions The findings support worker-reported OPPs as key determinants of both RTW and WRF. These results point to the importance of WA and PSE in both RTW and WRF at 6 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal disorders (MSDs) remain a significant global burden. Recent systematic reviews of injury prevention and disability programs found evidence supporting the effectiveness of disability management programs [1–3]. However, the majority of disability management programs target workers, health care providers and individual work accommodation and not the organization and the policies implemented and practiced [1–3]. Habeck and Hunt [4] proposed a model of how employer-reported organizational policies and practices (OPPs) can affect a range of occupational injury and illness outcomes. Amick [5], Ossmann [6], Williams [7, 8], Cullen [9], Tveito [10] and Tang [11], conducted measurement research building on the early work of Habeck and Hunt reducing the number of scales and items from the original employer OPP scale and developing a worker-reported version. Amick [12] and Katz [13], in a cohort of workers undergoing carpal tunnel surgery (CTS) in Maine, USA found OPPs were a strong predictor of both work absence and work role functioning (WRF). It was hypothesized OPPs affect return to work (RTW) through how they affect work accommodation and self-efficacy in managing pain. Franche [14] has shown how disability management policies and practices are strong predictors of a work accommodation offer, which is a well-established determinant of work absence duration [15–18]. Pain self-efficacy is one of several psychosocial factors that have been associated with pain and disability duration after onset of LBP [19]. There remains little research on the role of OPPs in RTW and the possible mediating role of self-efficacy in managing pain and work accommodation.
Theoretical research has highlighted the importance of considering an expanded range of work outcomes, beyond work absence duration [20, 21]. In this study, we differentiate between a RTW outcome (reporting being at work in some function at time of assessment) and a work role functioning outcome (factoring in the quality of WRF). In the Maine CTS II Cohort, Amick and Katz found clinical and economic factors were more important when predicting RTW while job and organizational factors were more important in predicting WRF [12, 13]. It may be that getting a person back to work is different from getting a person back to work and functioning well in their job [19]. With the growing emphasis on sustainable RTW and WRF following injury it is important to replicate this work in other injured worker populations.
We take advantage of data collected in a cohort of injured Ontario workers, the Readiness for Return to Work (R-RTW) Cohort Study, to answer the following questions:
-
1.
Do organizational policies and practices (OPPs) predict return to work (RTW) and work role functioning (WRF) work outcomes?
-
2.
Do OPPs differentially predict RTW and WRF work outcomes?
-
3.
If OPPs predict RTW and WRF, what roles do pain self-efficacy and work accommodations have in mediating the relationship?
In answering these questions, we consider whether there are different predictors for two different work outcomes, RTW and WRF?
Methods
Study Design
The study was conducted using the R-RTW Cohort, a prospective study of Ontario workers filing a new Workplace Safety and Insurance Board (WSIB) lost-time claim for a work-related back or upper extremity (UE) MSK disorder in 2005 [16, 22]. Eligibility criteria included: self-reported work absence of at least 5 days within 14 days following injury, claim filing within 7 days of injury, and 15 years or older. Eligibility was based on claim filing not on whether entitlement was allowed. The participants were interviewed by phone at baseline (approximately 1 month post-injury), 6 and 12 months post-injury. Ethical approval for the study was granted by the University of Toronto’s Ethics Review Board. Participants were given the option to withdraw from the study at any point.
Sample
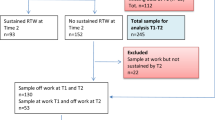
A total of 632 eligible claimants completed the baseline interview at 1 month (61 % participation). Of the baseline sample, 446 participants completed the 6 month follow-up (71 % retention) and 383 completed the 12-month follow-up (61 % retention). In the present study, 55 participants, who reported a change of employer at 6 or 12 months, were excluded, leaving a total of 577 participants at baseline (91.3 % of baseline sample). For the 55 excluded participants, RTW status and mean WRF scores at 6 month follow-up were similar to those of the included study participants. However, WRF scores at 12 month follow-up were significantly lower than those of the included participants.
At 6 and 12 months follow-up, data were available for 397 and 344 participants, respectively. A complete comparison of those lost to follow-up in the full cohort with those retained is presented elsewhere [22]. Attrition bias analysis at 12 months showed attriters were more likely to have a lower educational level, live alone, and work longer hours at the time of injury. Male attriters were more likely to be younger, whereas there were no differences in age for women. Attriters typically had poorer health and return to work status at baseline than continuing participants in terms of depressive symptoms, pain and functional disability and return to work status (further details available upon request).
Dependent Variables
Work role functioning (WRF) was assessed as one of two dependent work outcome variables. Based on information provided about return to work status (see below) and the 16-item version of the Work Limitations Questionnaire (WLQ-16), a 3-level outcome variable was created indicating whether a participant: (0) had not returned to work, (1) had returned to work and reported health-related work limitations for >10 % of the time (working with limitations), and (2) had returned to work and reported health-related work limitations for 10 % or less of the time (named “working without limitations”). The cut-point of 10 % follows Amick et al. [12] for comparability. If there was 25 % or more missing items, the overall scale score was set to missing.
The WLQ-16 covers four domains: output demands (4 items), psychosocial demands (6 items), physical demands (4 items), and time management demands (2 items). Items were scored on a 5-point scale, ranging from ‘0 % of the time’ to ‘100 % of the time’ with ‘50 % of the time’ in the middle [23, 24]. Individual item scores were averaged, and transformed to a standardized score of 0–100, with a higher score indicative of more limitations. Cronbach’s alphas, used to assess internal consistency, were 0.81 (output demands), 0.82 (psychosocial demands), 0.66 (physical demands), 0.76 (time management demands), and 0.84 (WLQ total) at baseline.
Return to work (RTW) status, reported at baseline, 6 and 12-month follow-up, was used to define RTW (1 = RTW; 0 = no RTW). The variable was constructed by combining the workers’ responses to: “Have you gone back to work at any point since your injury (includes part-time or modified work)?” and “Are you currently working at any job right now?”
Independent Variable
Worker-reported organizational policies and practices (OPPs) were assessed at the baseline interview. Following Amick et al. [12] and Katz et al. [13] we combined 19 questions assessing people-oriented culture (4 items), safety practices (7 items), disability management policies and practices (6 items) and ergonomics policies and practices (2 items) into an overall measure of organizational support (see ESM Appendix). Employees endorsed how much they agreed or disagreed with statements on a 1–5 scale. As in the Maine CTS II cohort, the four types of OPPs are highly correlated and thus any organization can be described most precisely by a combination of all these dimensions. A highly supportive organization was identified by a summative combination of all four subscales above the median (3.2), which was the identical median split as in the Maine CTS II cohort. As one OPP item (item p) directly asks about work accommodations, a primary mediating variable in our study, it was removed for conceptual reasons and the disability management policies and practices scale was constructed using the other 5 items.
Mediating Variables
Pain self-efficacy was assessed as a mediator and measured at baseline and 6 months with a 4-item scale assessing ability to cope with pain [25, 26]. Three of the four items were from the return-to-work self-efficacy scale developed by Shaw and Huang [27]. One item is new. The four items assess whether a person can continue to work despite pain, can avoid injury, can manage pain effectively while at work and will be able to remain at work once back at work (new item). Each item was rated on a five-point scale (1 = not at all certain, 5 = completely certain) and a summative score was calculated, with linear transformation from 2 to 10 with higher score indicating better abilities to cope with pain. The internal consistency was 0.76 at both baseline and at 6-month follow-up [26]. The pain RTW self-efficacy scale was chosen over the full RTW self-efficacy scale based on its observed strong predictive validity and the weak predictive validity of the full RTW scale [26].
Work accommodation was assessed as a mediator at baseline and new accommodations at 6 and 12 months follow-up. Work accommodation was measured by asking “Have you been offered work accommodation?” (yes/no) and “Did you accept the work accommodation offer?” (yes/no). Participants were provided the following explanation of a work accommodation prior to being asked the questions: Work accommodation is when you go back to a job that is adapted to your physical abilities following your injury. For example, you can go back to lighter duties, shorter hours, a changed workstation, or a different job with the same employer. Other words commonly used are: “modified work” and “light duties”. For new accommodation at 6 and 12 months follow-up, respondents who answered “no” about acceptance earlier were asked “Did you end up accepting a work accommodation offer later on? (yes/no)”.
Covariates
Demographic covariates included gender, age (15–29, 30–39, 40–49, ≥50 years), education (some high school, high school completed, some university/college, university/college completed), living with partner (yes/no), children under the age of 18 (yes/no), and personal income (<20,000, 20,000–39,999, 40,000–59,999, >60,000 Canadian dollars).
Clinical covariates included co-morbidity (present/absent) measured with the Saskatchewan Comorbidity Scale [28]. Pain intensity was measured with one item from the Von Korff Pain Scale [29]. Pain site was derived from worker self reports on the Roland-Morris Back and Quick-Dash Upper Extremity (UE) baseline questionnaires [30, 31]. When participants reported pain in both the back and UE, they completed the Roland–Morris and the QuickDASH. Scores were converted into a z-score. Determination of the main pain site, i.e., back or UE, was based on the highest z-score on the Roland–Morris or the QuickDASH. The Short-Form-12 (SF-12) measured physical and mental health-related quality of life [32, 33]. Depressive symptoms were measured with the 20-item Center for Epidemiologic Studies Depression (CES-D) scale [34]. The score has a potential range from 0 to 60 with a higher score denoting more depressive symptoms. Cronbach’s alpha was 0.92 at baseline. For comparison with other studies, the CES-D was dichotomized at 16 and above to reflect individuals at risk for clinical depression [34].
Job/organizational covariates included unionization status (yes/no), the number of employees at the workplace (<20, 20–99, 100–300, >300), and physical demands assessed by “How physically demanding is your job on your body?” dichotomized into “low/high”.
Statistical Analysis
Descriptive statistics to characterize the bivariate relationship between potential predictors and both dependent variables were generated for outcomes at 6 and 12 months to identify potential predictors for multivariable models (P < 0.25). The Chi square statistic was used to test the association between categorized predictors and outcomes. For continuous predictors, t-tests were used for work absence and ANOVA tests were used for work role functioning.
Two approaches were used in multivariable analysis. For the two-level RTW outcome, logistic regression was used to identify predictors brought forward through bivariate analyses and to investigate mediation effects of pain self-efficacy and work accommodation. For the three level WRF outcome, preliminary analyses revealed the proportionality of odds assumption was violated and thus the three level ordinal logit model was inappropriate. Therefore, a partial proportional odds model was used [35]. In estimation, a variable by variable assessment (using a Score test; P > 0.05) of the proportionality of odds model was conducted. When odds were proportional across all levels of WRF then a single risk estimate is presented. When the odds were not proportional then two estimates are presented; one for transitioning from not working to working either with or without limitations and a second for transitioning from not working or working with limitations to working without limitations.
Mediation analysis followed accepted procedures [36]. First, adjusted models including OPPs but without either mediator, pain self-efficacy or work accommodation, were estimated. Then each mediator was introduced independently and then both together. If the OPP effect on either outcome was being mediated by pain self-efficacy or work accommodation, then the risk estimate should be reduced (we set a minimal standard of 10 %). The analysis for this study was generated using SAS software Version 9.3 (SAS, Copyright © 2002–2010 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC).
Sensitivity analyses were conducted by pain site and by including the OPP scale as a continuous variable (as opposed to the dichotomous version used above). The findings were generally similar to those with the dichotomous version in terms of direction and magnitude of the effects and how the magnitude of effect responded to adjustment by confounders and to the two mediating variables. Therefore, for comparability with previous research, dichotomized findings are reported.
Results
Sample
Tables 1 and 2 show the detailed sample population characteristics at 6 and 12 months respectively after injury. The sample was mostly male, with income 20–60,000 (Canadian dollars) and about one-third having a college education. Forty-four percent reported levels of depressive symptomatology at baseline reflecting a high risk of clinical depression. The injured workers worked in jobs with high physical demands in unionized workplaces, and in worksites with fewer than 100 employees. The workers had limited baseline pain self-efficacy in the return to work process. Over 40 % of the injured workers had still not been offered work accommodation at baseline and 80 % of these workers were not offered an accommodation by 6 months.
If workers worked in a highly supportive organization before injury, at 6 or 12 months post injury they were more likely to be back at work and back at work functioning well in the job (Tables 1, 2). As shown in Table 1, a people-oriented culture, strong disability management policies and practices, ergonomic policies and practices and safety practices were associated with returning to work and functioning well in the job after returning to work. The patterns persist when return to work yes or no was the outcome. Coefficients for people-oriented culture and ergonomic policies and practices were in the appropriate direction but not statistically significant.
Return to Work
Unadjusted results (Table 3) show OPPs predicted RTW at 6 months (OR = 2.08; 95 % CI 1.32–3.28) and 12 months (OR = 2.26; 95 % CI 1.36–3.75). After adjustment for demographic, clinical and job/organizational covariates, OPPs predicted RTW at 6 months (OR = 1.77; 95 % CI 1.07–2.93) and 12 months (OR = 2.07; 95 % CI 1.18–3.62) (see ESM Appendix 2 for the full models showing all predictors).
Mediating Effects of Work Accommodation and Pain Self-Efficacy
As shown in Table 3, the overall effect size for OPP drops, as predicted, indicating a mediating effect of both work accommodation (WA) and pain self-efficacy (PSE) at 6 month (OR drops from 1.77 to 1.64 for WA; 1.45 for PSE and 1.36 for both; the OPP effect becomes non significant). At 12 months the effects were less consistent (OR drops from 2.07 to 1.88 for WA; went up to 2.12 for PSE and drops to 1.88 for both; the OPP effect remained significant and the drop is <10 %). At 6 months, separate mediating effects for WA or PSE were found. At 12 months, no mediating effects were found, but injured workers who received a WA offer and accepted the offer prior to the end of the 1st injury month were significantly more likely to return to work compared to those who do not receive an offer (OR = 4.63; 95 % CI 2.04–10.5). Having a WA offer and the employee rejecting it also predicted RTW (OR = 5.0; 95 % CI 1.46–17.1). New WA offers at 6 months (2.66; 95 % CI 1.11–6.38) were also significant predictors of RTW while new WA offers at 12 months (OR = 3.61; 95 % CI 0.86–15.2) were not significant, but the direction was correct and the magnitude was significant to other effects. At 12 months, baseline PSE and improved PSE from baseline to 6 months did not increase the likelihood of RTW.
Work Role Functioning
Unadjusted results (Table 4) showed that working in a highly supportive organization increased the likelihood an injured worker will return to work and function well in their job at 6 months (OR = 2.69; 95 % CI 1.82–3.95) and 12 months (OR = 2.49; 95 % CI 1.66–3.75). After adjusting for demographic, clinical and job/organizational covariates, the OPP effects remained significant at both 6 months for the transition from not working or working with limitation to working without limitation (OR = 3.21; 95 % CI 1.92–5.39) but were marginally non-significant for the transition from not working to returning to work with or without limitations (OR = 1.65; 95 % CI 0.99–2.75). At 12 months the odds for both transitions were proportional and the effect remained significant (OR = 2.13; 95 % CI 1.37–3.30) (see ESM Appendix 2 for full model, showing all predictors).
Mediating Effects of Work Accommodation and Pain Self-Efficacy
As shown in Table 4, the overall effect size for OPPs dropped >10 % for the marginally non-significant transition from not working to working with limitations for both WA (from 1.65 to 1.42) and PSE (from 1.65 to 1.34). While the effects for the transition from not at work or working with limitations to working without limitations dropped—the change did not result in a transition to non-significance for the OPP effect (for WA from 3.21 to 2.89 and for PSE to 2.65). Both WA and PSE were mediating the effects of OPPs on 6 month WRF. Baseline WA offers during the 1st month after injury predicted the transition from not working to working with or without limitations (WA offer rejected OR = 4.05; 95 % CI 1.45–11.3 and WA offer accepted OR = 2.90; 95 % CI 1.49–5.63) but not the transition from not working or working with limitations to working without limitations. A similar effect was observed with new WA offers at 6 months (OR = 4.98; 95 % CI 2.2–11.3). PSE at baseline and change in PSE were statistically significant predictors of all transitions (see ESM Appendix 2). At 12 months, the effects for WA and PSE on OPPs were nominal (for WA from 2.13 to 2.02 and for PSE to 2.10). Neither WA nor PSE appeared to mediate the effects of OPPs on 12 months WRF. At 12 months, WA effects at baseline and new WA offers at 6 and 12 months were significant for both getting back to work and for functioning well in the job (see ESM Appendix 2). At 12 months, baseline PSE (OR = 1.45; 95 % CI 1.17–1.79) and changes in PSE (OR = 1.70; 95 % CI 1.40–2.08) were significant only in the transition from not working to back at work.
Sensitivity Analyses
The OPP effects persisted when a continuous predictor was used instead of the median split suggesting this was not a function of how OPPs were operationalized. Whether results varied by pain site, upper extremity or back, was examined and the effects were more varied and inconclusive due to sample size limitations (results available from the first author upon request).
Discussion
In a prospective cohort of Canadian workers filing workers’ compensation claims, worker-reported organizational policies and practices (OPPs) predicted both return to work (RTW) and work role functioning (WRF). WA offers mediated the relationship between OPPs and both RTW and functioning without limitations in the job at 6 months follow-up. PSE mediated the relationship between OPPs and RTW and functioning without limitations in the job at 6 months. Neither WA nor PSE mediate the relationship between OPPs and RTW or functioning without limitations in the job at 12 months. Importantly, when examining the mediating effects of WA and PSE, only for 6 month RTW do the OPP effects become non-significant. Our results point to the important independent effects of OPPs on both RTW and WRF.
The results replicate and expand on findings from the Maine Carpal Tunnel II cohort study [12, 13] and earlier R-RTW Cohort work [14]. We considered whether using different work outcomes resulted in different predictors. Hypothetically, getting a worker back to work is easier to manage because an injured worker can return to work with or without work limitations. Simply returning to work is not a good indicator of whether the person has returned to work and is functioning well in his or her job, [5, 22] which has direct implications for RTW sustainability. Being injured in a highly supportive organization has consistent effects across all models as do the effects of high levels of depressive symptoms and of high physical demands. PSE was important across outcomes (except 12 month RTW), but more important in helping the worker return to work and function well in the job. WA matters across all outcomes except for 6 month WRF where the effect becomes non-significant when PSE is in the model. These findings differ from the Maine CTS II findings where no significant WA effect was found. Supporting healthy working lives following a work-related injury may be different than just getting the injured worker back to work. More research is needed on this important topic. The findings clearly indicate that work disability can only be solved in collaboration with the workplace [37–39].
The mediating effects of WA are new. While there is a large literature on self-efficacy as a predictor of behavior change in the management of chronic diseases and a growing literature in RTW and work disability, these findings are the first to suggest this important mechanism is at least partially driven by organizational support. A small number of published studies examining the role of self-efficacy in mediating the job stress health relationship have produced mixed results [40–42]. Theoretically, the findings support one key causal pathway in the socio-cognitive theory; the role of the perceived environment on self-efficacy in behavior change [43]. Importantly, we measured pain self-efficacy in the RTW context. Measuring context-specific self-efficacy helps to avoid measurement bias associated with misattribution of perceived competencies associated with other more general contexts [44]. We chose to use the pain self-efficacy subscale of the RTW self-efficacy scale based on construct and predictive validity [25, 26]. With respect to the Readiness for Change Model, [45] this research supports the importance of considering OPPs in relation to the three vectors of readiness-self-efficacy, decisional balance, and change processes. We believe that our findings emphasize the determinant role of OPPs in predicting RTW and WRF.
The research has several strengths. It used a large sample and strong statistical analyses including many potential covariates in a multidimensional model of RTW and WRF. There is temporal ordering, not only for OPPs predicting outcomes, but also for OPPs predicting change in PSE and new WA offers. While we had significant variability in the size of the organizations, it could be hypothesized that organizations of different sizes may have more resources to be successful in WA. Further research should examine the impacts of organizational size on the mediating effects. Still all data are based on self-reports. Hence, some unmeasured variables may explain the relationship between OPPs and RTW and WRF and the mediating effects of PSE and WA. In other research, Habeck and colleagues have shown that OPPs are represented in observed organizational policies and practices supporting the validity of self-reports [4]. Amick and colleagues have found strong correspondence between manager and worker reports of OPPs especially in unionized organizations [7]. Finally, predictors were assessed one-month post injury so that some effects may have already played out by 1 month post-injury.
There are some important lessons from this work. Choose your outcome carefully: different outcomes lead to different predictors. Future work will examine whether one specific OPP, like disability management or ergonomics policies and practices, is driving the observed effects. Furthermore, other pathways through which OPPs can affect RTW and WRF should be considered.
References
Brewer S, King E, Amick B, Delclos G, Spear J, Irvin E, Mahood Q, Lee L, Lewis C, Tetrick L, Gimeno D, Williams R. A systematic review of injury/illness prevention and loss control programs (IPC). Toronto: Institute for Work & Health; 2007.
Van Oostrom SH, Driessen MT, de Vet HCW, Franche, R-L, Schonstein E, Loisel P, et al. Workplace interventions for preventing work disability. Cochrane Database Syst Rev 2009.
Gensby U, Labriola M, Irvin E, Amick BC, Lund T. A classification of components of workplace disability management programs: results from a systematic review. J Occup Rehabil. 2014;24:220–41.
Habeck RV, Hunt HA, VanTol B. Work-place factors associated with preventing and managing work disability. Rehabil Counsel Bull. 1998;42:98–143.
Amick BC III, Habeck RV, Hunt A, Fossel AH, Chapin A, Keller RB, Katz JN. Measuring the impact of organizational behaviors on work disability prevention and management. J Occup Rehabil. 2000;10:21–38.
Ossmann J, Amick BC III, Habeck RV, Hunt A, Ramamurthhy G, Soucie V, Katz JN. Management and employee agreement on reports of organizational policies and practices important in return to work following carpal tunnel surgery. J Occup Rehabil. 2005;15:17–26.
Williams RM, Westmorland MG, Shannon H, Rasheed F, Amick BC III. Disability management practices in education, hotel/motel and health care workplaces. Am J Ind Med. 2005;47:217–26.
Williams RM, Westmorland MG, Shannon HS, Amick BC III. Disability management practices in Ontario health care workplaces. J Occup Rehabil. 2007;17:153–65.
Cullen KL, Williams RM, Shannon HS, Wessel J, Amick BC III, Westmoreland MG. Workplace disability management practices in Ontario educational facilities. J Occup Rehabil. 2005;15:417–33.
Tveito TH, Sembajwe G, Boden LI, Dennerlein JT, Wagner GR, Kenwood C, Stoddard AM, Reme SE, Hopcia K, Hashimoto D, Shaw WS, Sorensen G. Impact of organizational policies and practices on workplace injuries in a hospital setting. J Occup Environ Med. 2014;56:802–8.
Tang K, MacDermid JC, Amick BC, Beaton DE. The 11-item workplace organizational policies and practices questionnaire (OPP-11): examination of its construct validity, factor structure, and predictive validity in injured workers with upper-limb disorders. Am J Ind Med. 2011;54:834–46.
Amick BC III, Habeck RV, Ossmann J, Fossel AH, Keller R, Katz JN. Predictors of successful work role functioning after carpal tunnel release surgery. J Occup Environ Med. 2004;46:490–500.
Katz JN, Amick BC III, Keller R, Fossel AH, Ossmann J, Soucie V, Losina E. Determinants of work absence following surgery for carpal tunnel syndrome. Am J Ind Med. 2005;47:120–30.
Franche R-L, Severin C, Hogg-Johnson S, Lee H, Côté P, Krause N. A multivariate analysis of factors associated with offer and acceptance of a work accommodation following an occupational musculoskeletal injury. J Occup Environ Med. 2009;51:969–83.
Franche R-L, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J, et al. Workplace-based return-to-work interventions: a systematic review of the quantitative literature. J Occup Rehabil. 2005;15:607–31.
Franche R-L, Severin C, Hogg-Johnson S, Côté P, Vidmar M, Lee H. The impact of early workplace-based return-to-work strategies on work absence duration: a 6-month longitudinal study following an occupational musculoskeletal injury. J Occup Environ Med. 2007;49:960–74.
Krause N, Dasinger LK, et al. Modified work and return to work: a review of the literature. J Occup Rehabil. 1998;8:113–39.
Brooker A-S, Cole DC, Hogg-Johnson S, Smith J, Frank JW. Modified work: prevalence and characteristics in a sample of workers with soft-tissue injuries. J Occup Eviron Med. 2001;43:276–84.
Busch H, Göransson S, Melin B. Self-efficacy beliefs predict sustained long-term sick absenteeism in individuals with chronic musculoskeletal pain. Pain Pract. 2007;7:234–40.
Amick BC III, Lerner DJ, Rogers WH, Rooney T, Katz Jeffrey N. A review of health-related work outcome measures and their uses, and recommended measures. Spine. 2000;25:3152–60.
Wasiak R, Young AE, et al. Measuring return to work. J Occup Rehabil. 2007;17:766–81.
Bültmann U, Franche RL, Hogg-Johnson S, Côté P, Lee H, Severin C, Vidmar M, Carnide N. Health status, work limitations, and return-to-work trajectories in injured workers with musculoskeletal disorders. Qual Life Res. 2007;16:1167–78.
Lerner DJ, Amick BC III, Rogers WH, Malspeis S, Bungay K, Cynn D. The work limitations questionnaire. Med Care. 2001;39:72–85.
Lerner DJ, Amick BC III, Lee J, Rooney T, Rogers WH, Chang H, Berndt ER. The relationship of employee-reported work limitations to work productivity. Med Care. 2003;41:649–59.
Brouwer S, Franche RL, Hogg-Johnson S, Lee H, Krause N, Shaw WS. Return-to-work self-efficacy: development and validation of a scale in claimants with musculoskeletal disorders. J Occup Rehabil. 2011;2:244–58.
Brouwer S, Amick BC III, Lee H, Franche RL, Hogg-Johnson S. The predictive validity of the return-to-work self-efficacy scale for return-to-work outcomes in claimants with musculoskeletal disorders. J Occup Rehabil. 2015;25:725–32.
Shaw WS, Huang YH. Concerns and expectations about returning to work with low back pain: identifying themes from focus groups and semi-structured interviews. Disabil Rehabil. 2005;27:1269–81.
Jaroszynski G, Cassidy JD, Côté P, Carroll L, Yong-Hing H. Development, reliability, and concurrent validity of a new self-assessed comorbidity scale. Unpublished manuscript, University of Saskatchewan (1998).
Von Korff M, Jensen MP, Karoly P. Assessing global pain severity by self-report in clinical and health services research. Spine. 2000;25:3140–51.
Beaton DE, Wright JG, Katz JN, The Upper Extremity Collaborative Group. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87:1038–46.
Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–4.
Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33.
Ware J, Kosinski M, Keller SD. SF-12: how to score the SF-12 physical and mental health summary scales. Lincoln: Quality Metric Incorporated; 2002.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS system. 2nd ed. Cary: SAS Institute Inc.; 2000.
MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008.
Anema JR, Steenstra IA, Bongers PM, de Vet HC, Knol DL, Loisel P, van Mechelen W. Multidisciplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both?: a randomized controlled trial. Spine. 2007;32:291–8.
Lambeek LC, van Mechelen W, Knol DL, Loisel P, Anema JR. Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ. 2010;340:c1035.
Loisel P, Abenhaim L, Durand P, Esdaile JM, Suissa S, Gosselin L, Simard R, Turcotte J, Lemaire J. A population-based, randomized clinical trial on back pain management. Spine. 1997;22:2911–8.
Schreurs B, van Emmerik H, Notelaers G, De Witte H. Job insecurity and employee health: the buffering potential of job control and job self-efficacy. Work Stress. 2010;24:56–72.
Schaubroeck J, Lam SSK, Xie JL. Collective efficacy versus self-efficacy in coping responses to stressors and control: a cross-cultural study. J Appl Psychol. 2000;85:512–25.
Xanthopoulou D, Bakker A, Demerouti E, Schaufeli WB. The role of personal resources in the job demands-resources model. Int J Stress Manag. 2007;14:121–41.
Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13:623–49.
Bandura A. Self-efficacy: the exercise of control. New York: W. H. Freeman; 1997.
Franche R-L, Krause N. Readiness for return to work following injury or illness: conceptualizing the interpersonal impact of healthcare, workplace, and insurance factors. J Occup Rehabil. 2002;12:233–56.
Acknowledgments
The development of the Readiness for Return to Work Cohort was supported by Grants (#6021, #4010) from the Workplace Safety and Insurance Board. All authors were involved in either the conception and design or the analysis and interpretation of data, in the drafting of the article, and in the final approval.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Amick, B.C., Lee, H., Hogg-Johnson, S. et al. How Do Organizational Policies and Practices Affect Return to Work and Work Role Functioning Following a Musculoskeletal Injury?. J Occup Rehabil 27, 393–404 (2017). https://doi.org/10.1007/s10926-016-9668-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-016-9668-8