Abstract
To validate the Italian Perceived Maternal Parenting Self-Efficacy (PMP S-E), the first questionnaire specifically developed for mothers of preterm neonates hospitalized in the Neonatal Intensive Care Unit. Two hundred mothers filled the PMP S-E, the General Self-Efficacy Scale (GSES), the Edinburgh Postnatal Depression Scale (EPDS), the Parental Distress Index (PSI-SF/Pd). The Explanatory Factor Analysis outlined four factors: care-taking procedures, evoking behaviours, reading and managing bodily cues, reading and managing emotional cues. This factor-solution demonstrated adequate goodness of fit when the Confirmatory Factor Analysis was carried out. Internal consistency was high for the overall scale (α = 0.932), and the all the factors (all α > 0.80). There was a moderate correlation with GSES (r = .438; p < .001), while the associations with EPDS (r = .295; p < .001) and PSI-SF/Pd (r = .193; p = .006) were low. Good test–retest reliability was found over 2 weeks (r = .73; p < .001). These findings support the validity and reliability of the Italian PMP S-E.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Europe, preterm births (before 37th week of gestation) make up on average 7% of total annual births (Blencowe et al., 2012). The survival rates of preterm neonates have increased over recent decades, however, most of these neonates are at risk of morbidity and require long-term hospitalization in Neonatal Intensive Care Units (NICU) (Horbar et al., 2012). Parents of premature neonates experience a difficult start in parenting (Shaw, Bernard, Storfer-Isser, Rhine, & Horwitz, 2013) and parental role alteration was identified as the main source of stress in the immediate period after preterm delivery (Montirosso, Provenzi, Calciolari, & Borgatti, 2012b). The behavioural cues of a premature baby may be weaker than those of a healthy full-term baby, thus it can be difficult to interpret and adequately respond to them (Forcada-Guex, Borghini, Pierrehumbert, Ansermet, & Muller-Nix, 2011). Moreover, the hospitalization in NICU interferes with bonding because of the separation from the neonate and the rhythms imposed by medical or nursing procedures, which contribute to creating feelings of helplessness, alienation and low parenting self-efficacy (Montirosso et al., 2012b; Shaw et al., 2013; Woolf, Muscara, Anderson, & McCarthy, 2016).
Parenting self-efficacy is a crucial variable in the development of a child, as it directly influences parenting competence (Jones & Prinz, 2005; Teti & Gelfand, 1991; Teti, Hess, O’Connell, 2005). Parenting self-efficacy is a person’s belief in their ability to deal with parenting situations (Bandura, 1997; Hess, Teti, & Hussey-Gardner, 2004). It is particularly important when parents face difficult situations, such as preterm birth; indeed, cognitive processes (i.e. knowledge, beliefs, values, attitude) play a prominent role, both in the acquisition of new patterns of behaviour and in making changes to already existing behaviours (Bandura, 1977).
Low parenting self-efficacy had been reported by parents of preterm neonates (Özyurt, Özyurt, Ozturk, Yaman, & Berk, 2018; Montirosso et al., 2012b) and, in general, by parents of hospitalized children (Leyenaar, O’Brien, Leslie, Lindenauer, & Mangione-Smith, 2017; Warschburger & Kühne, 2014; Holditch-Davis, Miles, Burchinal, & Goldman, 2011; Holland et al., 2011). Parental self-efficacy and competence are moderated by a parent’s knowledge of the condition of the baby, as well as by their emotional state. Moreover, the experience of hospitalization is deeply influenced by culture (Heydarpour, Keshavarz & Bakhtiari, 2016). For example, Iranian parents often feel ashamed because of the related social stigma (Heidari, Hasanpour, & Fooladi, 2012). By contrast, in some countries, anger is the most common emotional response to the shock of preterm labour (Roman et al., 1995). These negative social reactions may prevent a healthy transition to motherhood and healthcare providers should consider these factors in order to establish effective communication with parents and a supportive relationship during this vulnerable phase (Heydarpour et al., 2016).
Parenting self-efficacy is improved through vicarious experiences (i.e. learning by observing others) and enactive learning (i.e. learning by doing) (Bandura, 1977). For this reason, parenting self-efficacy has been included as one of the target areas of intervention for mothers in the immediate postnatal period (Benzies, Magill-Evans, Hayden, & Ballantyne, 2013). The belief in maternal efficacy mediates the effects of depression, social support and infant temperament on parenting behaviours (Teti & Gelfand, 1991). Indeed, interventions implemented with the purpose of encouraging mother–baby interaction during NICU stay have a positive impact on mothers, mainly in terms of reduction of maternal stress (Melnyk et al., 2006; Kaaresen, Rønning, Ulvund, & Dahl, 2006) and improvement in their confidence in dealing with their babies (Ohgi, Fukuda, Akiyama, & Gima, 2004). At same time, positive effects have also been identified in the infants; indeed, studies with longer follow-up periods show that early interventions to enhance parent–baby interaction are associated with greater improvement in the children’s cognitive development (Teti et al., 2009) and a lower rate of behavioural problems at school age (Nordhov, Rønning, Ulvund, Dahl, & Kaaresen, 2012).
Considering the aforementioned clinical implications of parenting self-efficacy, the availability of an instrument to monitor this psychological variable may be of value. More specifically, knowing whether or not the mother of a hospitalized premature neonate feels competent in areas of parenting would allow healthcare professionals to identify those mothers needing further individual support. Moreover, by tracking her own skills development, the mother is better able to formulate requests to healthcare staff, thus improving their understanding of the baby’s cues and overall the interaction with the baby (Melnyk et al., 2006).
There are a lot of instruments addressing parenting self-efficacy but they are unsuitable for parents of preterm neonates because of the specific conditions that they have to deal with. The Perceived Maternal Parenting Self-Efficacy (PMP S-E) is a self-report questionnaire specifically developed for mothers of hospitalized preterm babies (Barnes & Adamson-Macedo, 2007). The original validation study showed adequate psychometric properties of the questionnaire, mainly in terms of high internal consistency and adequate test–retest reliability (Barnes & Adamson-Macedo, 2007). The PMP S-E conforms to the widely accepted Bandurian self-efficacy theory; more specifically, it is a domain-specific instrument because it refers explicitly to concrete parenting tasks or activities, thus it is highly predictive of actual behaviour (Bandura, 1977). Moreover, the PMP S-E was formulated for the assessment of parenting self-efficacy in the early stages of neonatal development, therefore it is in line with the family-centred care approach (Westrup, 2015; Als et al., 2012; McAnulty et al., 2010; Bracht, OʼLeary, Lee, & OʼBrien, 2013; Melnyk et al., 2006; Ortenstrand et al., 2010; Montirosso, Del Prete, Bellù, Tronick, & Borgatti, 2012a).
The main objective of this study is to translate the Perceived Maternal Parenting Self-Efficacy (PMP S-E) into Italian and to assess its validity and reliability. There are no similar Italian instruments specifically formulated for mothers of preterm neonates, therefore, the results of this study could be relevant both for clinical and research purposes.
Methods
Setting and Procedure of Recruitment
The study was conducted at the NICU of Spedali Civili in Brescia, a tertiary referral hospital in Northern Italy. Mothers were recruited according to the following inclusion criteria: (i) they had given birth to a preterm baby (i.e. before 37 weeks of gestation); (ii) they were of Italian nationality; (iii) the neonates were in a medically stable condition; (iv) they gave written consent. Mothers of babies with genetic anomalies or congenital malformations were not recruited.
Informed consent was obtained from all individual participants included in the study. A clinical psychologist researcher met the mothers satisfying the inclusion criteria to inform them about the study and ask them to participate. Two mothers refused to participate at this stage. After written informed consent, the mothers received the PMP S-E with all the other questionnaires. Fifty mothers were chosen at random among the overall sample and they were asked to re-complete the PMP S-E 2 weeks later for the purpose of analysing test–retest reliability. Mothers of twins were asked to complete the questionnaire for the first neonate close to discharge from NICU. All the questionnaires were completed anonymously.
The Italian Adaptation of the PMP S-E
The adaptation of the PMP S-E (Barnes and Adamson-Macedo, 2007) to the Italian population was based on translation and the assessment of face validity. The questionnaire was translated and then back-translated. More specifically, a group of Italian neonatal nurses and neonatologists with lengthy professional experience translated the original English version of the PMP S-E from English into Italian. Then, a bilingual author, who was unfamiliar with the original questionnaire, re-translated this version back into English. Finally, the two English versions were compared in order to correct any inconsistencies. In order to analyse the face validity of the questionnaire, a further group of mothers of preterm, neonatal nurses, and neonatologists were asked to read the translated questionnaire and to comment on the applicability and comprehensibility of each item.
Measures
Perceived Maternal Parenting Self-Efficacy (PMP S-E) (Barnes & Adamson-Macedo, 2007)
The PMP S-E is a 20-item self-report questionnaire measuring parenting self-efficacy in the mothers of preterm neonates (Barnes & Adamson-Macedo, 2007). The PMP S-E was based on the self-efficacy theory (Bandura, 1977), and it was developed from a review of the literature and adaptation of the two most relevant similar scales: the Parenting Self-Efficacy Scale (Parker and Zahr, 1985), and the Maternal Efficacy Questionnaire (Teti & Gelfand, 1991).
The questionnaire asks the mother to rate her agreement with statements about parenting skills on a four-point Likert scale, from “strongly disagree” to “strongly agree”. All the item scores are added up to obtain a total score ranging from 20 to 80. Higher values indicate a greater perceived parenting self-efficacy.
The original validation study includes four subscales: (1) care-taking procedures (4 items), referring to a mother’s perception of her ability to perform the activities and tasks related to her baby’s basic needs, such as feeding; (2) evoking behaviour (7 items), referring to perceptions of her ability to elicit a change in her baby’s behaviour; (3) reading behaviour or signalling (6 items), referring to perceptions of her ability to understand and identify changes in her baby’s behaviour; (4) situational beliefs (3 items), referring to a mother’s belief in her ability to judge her overall interaction with her baby.
The psychometric properties of the PMP S-E were analysed for a convenience sample of 165 mothers of relatively healthy preterm neonates during NICU stay. Results show high internal consistency for the overall scale (Cronbach’s alpha = 0.91) and for the subscale (Cronbach’s alpha ranging from 0.72 to 0.89). Over a 10-day interval, test–retest reliability was high for the total score (r = .96; p < .001) and for the subscale scores (care-taking procedures r = .92, p = .01; evoking behaviour r = .92, p = .01; reading behaviour or signalling r = .93, p = .01; situational beliefs r = .88, p = .01).
General Self-Efficacy Scale (GSES) (Schwarzer & Jerusalem, 1995)
The GSES includes 10 items (e.g. “I am confident that I could deal efficiently with unexpected events”) that describe both the ability to cope with daily demands and the level of adaptation to stressful events. Each item is rated on a four-point Likert scale, from 1 (= not at all true) to 4 (= completely true). The item scores are added up to obtain a total score ranging from 1 to 40, with higher values indicating greater perceived self-efficacy. The GSES showed adequate internal consistency and good validity in multicultural samples (Luszczynska, Scholz, & Schwarzer, 2005). In the sample of this study, the GSES showed good internal consistency (α = 0.887).
Edinburgh Postnatal Depression Scale (EPDS) (Cox, Holden, & Sagovsky, 1987; Benvenuti, Ferrara, Niccolai, & Valoriali, 1999)
The EPDS is a 10-item self-report questionnaire measuring the symptoms of perinatal depression (Cox et al., 1987; Benvenuti et al., 1999). For each item, the mother is asked to rate the statement best describing her feelings, by choosing one of four options describing different symptom severities. The item scores are added up to obtain a total score that ranges from 0 to 30, with higher values indicating more severe symptoms of depression. In the Italian validation study, the EPDS showed high internal consistency (α = 0.789), and the threshold score 8/9 was suggested for identifying mothers with depression with high sensitivity (94.4%) and good specificity (59%) (Benvenuti et al., 1999). In the sample of this study, the internal consistency of the EPDS was good (α = 0.876). Mothers were informed that they had the option of knowing their questionnaire score, upon request. Regardless of the study, all the parents undergo a consultation with a clinical psychologist during NICU admission.
Parenting Distress (PD) Subscale of the Parenting Stress Index, Short Form (PSI-SF/Pd) (Abidin, 2012; Guarino, Di Blasio, D’Alessio, Camicasca, & Serantoni, 2008)
The PSI-SF is a 36-item self-report questionnaire measuring parenting stress. Parents are asked to rate how much they agree with statements on a five-point Likert scale, from “strongly disagree” to “strongly agree”. All the item scores are added up to obtain the Total Stress Score (range 36–180) indicating the overall level of parenting stress. Moreover, there are three subscales: Parental Distress (PD) (range 12–60), which measures the level of distress due to personal factors; Parent–Child Dysfunctional Interaction (P-CDI) (range 12–60), which reflects how the child meets the expectations of the parent; Difficult Child (range 12–60), which measures the behavioural characteristics of the child that make him/her either easy or difficult to manage. Scores ≥ 85th percentiles are considered clinically significant. The Italian version of the PSI-SF showed high internal consistency (α = 0.93) and alpha values of the subscales ranged from 0.78 to 0.87 (Guarino et al., 2008). In the sample of this study, the internal consistency of the subscale PD was good (α = 0.894).
Statistical Analysis
The data were described as the mean (M) and standard deviation (SD) for continuous variables or frequencies and percentages for categorical variables. The Gaussianity assumption of continuous variables was assessed using Kolmogorov–Smirnov and Shapiro–Wilk tests, while any outliers were evaluated using the interquartile range method.
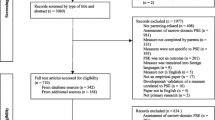
To test the validity of the factor structure shown in the original English validation study (Barnes & Adamson-Macedo, 2007), Confirmatory Factor Analysis (CFA) was conducted for the overall sample. Then, according to recommendations on scale development and validation studies (Cabrera-Nguyen, 2010; Worthington & Whittaker, 2006), we split the sample in order to conduct Exploratory Factor Analysis (EFA) and CFA on different samples. More specifically, we first performed EFA on one randomly selected half of the sample (calibration sample), and then, tested the factor structure derived from EFA on the other half of the sample (validation sample).
The following indices were used to determine the goodness of fit of the model: Root Mean Square Error of Approximation (RMSEA) smaller than 0.05, Comparative Fit Index (CFI) and Non-Normed Fit Index (NNFI) greater than 0.90 and ratio of the Chi-square value to its degrees of freedom (chi2/df) of less than 2.5.
Exploratory Factor Analysis (EFA), using varimax rotation, was used to determine the factor structure of the PMP S-E. The Kaiser–Meyer–Olkin (KMO) test verified the sampling adequacy for this analysis, and Barlett׳s Test of Sphericity assessed the degree of inter-correlation between variables. Factor extraction was determined through Kaiser’s criterion (eigenvalues ≥ 1). Factor loading greater than 0.54 was considered the threshold indicating that the item contributed sufficiently to the factor. Cronbach’s alpha coefficients were calculated to determine the internal consistency for both the whole scale and the factors, and values ≥ 0.70 were considered adequate. Any change in consistency was evaluated by removing one item at a time. Moreover, the Pearson’s correlation with the total score was evaluated for each item. Concurrent and divergent validity were evaluated using the Pearson’s correlation coefficient between PMP S-E, GSES, EPDS and PSI-SF/Pd.
All statistical analyses were carried out using the SPSS 21.0 and SPSS-AMOS programs. Statistical significance was set at p = .05.
Results
Sample Characteristics
A total of 200 mothers of preterm neonates admitted to the NICU were included. The assessment was conducted 39 (SD 33) days after delivery. Table 1 shows the clinical and sociodemographic characteristics of the sample. The mean age of the mothers was 34 (SD 5) years and most of them (N = 164; 82%) had completed high school or university. Participants delivered at 32 (SD 3) weeks’ gestation, and the mean neonatal weight at birth was 1549 (SD 505) g. One-third of the mothers (N = 65; 32%) showed clinically significant symptoms of postnatal depression, and N = 15 (7%) of the mothers showed clinically significant stress levels.
The clinical scales were Gaussian distributed (with p values of both Kolmogorov–Smirnov and Shapiro–Wilk tests greater than 0.05 for all scales) and no outliers were found. The mean PMP S-E total score was 62.4 (SD 6.6) and ranged from 44 to 80. The mean PMP S-E total score of this sample did not differ from the mean score reported in the original English validation study (t = 0.053; p = .957).
Construct Validity of the Italian PMP S-E
CFA was performed on the overall sample to evaluate the goodness of fit of the factor-solution originally proposed by Barnes and Adamson-Macedo (2007). As reported in Fig. 1, results indicated a poor fit: RMSEA = 0.534; CFI = 0.710; NNFI = 0.131; chi2/df = 59.468; p < .001.
Confirmatory factor analysis on the factors of the originally proposed by Barnes and Adamson-Macedo (2007)
After the splitting the sample into two halves, EFA was conducted on one-half of the sample (validation sample) in order to determine the optimal factor structure of the Italian version of the PMP S-E (Table 2). This analysis outlined four factors with eigenvalues exceeding 1, explaining 68% of the total variability. The factors appeared easily interpretable, and they were labelled according to the item content, as follows: evoking behaviours, explaining 46% of variance; reading and managing bodily cues, explaining 12% of variance; reading and managing emotional cues, explaining 5% of variance; and care-taking procedures, explaining 5% of variance. None of the items showed loading under the cut-off (0.5) and none loaded on more factors, thus suggesting that all the items were relevant for the measurement of the construct of parenting self-efficacy and that the factors were clearly distinct.
The model fit based on the above EFA-derived factor-solution was tested by performing CFA on a different sample (calibration sample). As showed in Fig. 2, the fit of the model to the data was excellent (chi2/df = 0.068, p = .794; RMSEA = 0.000; CFI = 1.000; NNFI = 1.000).
Internal Consistency of the Italian PMP S-E
The overall scale showed high internal consistency, as established by the Cronbach’s alpha value (α = 0.932). As reported in Table 2, no higher alpha values were found if any items were removed from the scale. Cronbach’s alpha values for the subscales were as follows: reading and managing bodily cues (α = 0.774); reading and managing emotional cues (α = 0.881); evoking behaviours (α = 0.874); care-taking procedures (α = 0.879). As reported in Table 2, item-total correlations were adequate, with values ranging from 0.449 to 0.711 (Table 2).
Concurrent and Divergent Validity of the Italian PMP S-E
Both the overall scale and the subscales of PMP S-E showed significant (although only moderate for some subscales) correlations with GSES (Table 3). Conversely, there were weak correlations between the PMP S-E, the EPDS, and the PSI-SF/Pd (Table 3), proving good divergent validity.
Test–Retest Reliability of the Italian PMP S-E
Over a 2-week period, the overall scale demonstrated good test–retest reliability (r = .73; p < .001). The correlation coefficients of the subscales were as follows: reading and managing bodily cues (r = .49; p = .006), reading and managing emotional cues (r = .61; p = .001); evoking behaviours (r = .75; p < .001); care -taking procedures (r = .60; p < .001).
Discussion
This study addresses the lack of tools for assessing parenting self-efficacy in the mothers of premature neonates in Italy; this is relevant because the assessment of this construct could be a valid strategy for implementing interventions for a more family-centred approach to care and to evaluate their outcome (Westrup, 2015).
The multidimensional structure of the PMP S-E was confirmed; indeed, the EFA clearly outlined four factors referring to different parenting skills. More specifically, the factor care-taking procedures refers to the mother’s perception of her ability to perform activities and tasks related to basic needs (e.g. feeding). The factor evoking behaviours refers to the mother’s perception of her ability to elicit certain changes in her baby’s behaviour (e.g. soothing). The factor reading and managing bodily cues refers to the mother’s perception of her ability to identify and understand the body cues of the baby (e.g. tiredness). The factor reading and managing emotional cues refers to the mother’s perception of her ability to identify and manage changes in her baby’s behaviour based on emotional cues (e.g. when the baby is upset). The PMP S-E showed high internal consistency, and the removal of any item resulted in the increasing of the overall alpha coefficient, thus indicating that all the items significantly contribute to define the construct of parenting self-efficacy.
The four factors are clearly distinct; indeed, none of the items loaded on more than one factor, and the alpha coefficients revealed high internal consistency for each of the four factors. Overall, findings confirm the nature of the PMP S-E as a “domain-specific” measure of self-efficacy (Barnes & Adamson-Macedo, 2007). According to the well-accepted Bandurian theory of self-efficacy (Bandura, 1997), “domain-specific” measures refer directly to specific activities, and this makes them more predictive of parenting competence than general measures of self-efficacy (Bandura, 1997). In this sense, the PMP S-E is in line with the current approach to the care of preterm neonates that incorporates technological and pharmacological interventions with interventions addressing “relationship-based needs” (Westrup, 2015; Als et al., 2012; McAnulty et al., 2010). The assessment of mother–baby interaction requires specific procedures of observation and coding of behaviours (Jones & Prinz, 2005; Morsbach & Prinz, 2006). Indeed, attachment representations are the most important factors influencing mother–infant interaction (Fonseca, Nazaré, Canavarro et al., 2013). However, the assessment of perceived parenting self-efficacy may be informative; in fact, cognitive processes (i.e. knowledge, beliefs, values, attitude) influence the acquisition of new patterns of behaviour and the changing of already existing behaviours (Bandura, 1977). This may explain why parenting self-efficacy has been associated with parenting competence (Jones & Prinz, 2005; Teti & Gelfand, 1991; Teti et al., 2005).
The factor structure outlined in this study seems to provide a more detailed picture of parenting self-efficacy than that provided by the original factor-solution (Barnes & Adamson-Macedo, 2007). More specifically, the original study included the factor “reading behaviour or signalling” with six items; whereas, in this study, these six items are loaded on two distinct factors: the factor “reading and managing bodily cues” and the factor “reading and managing emotional cues”, respectively. In this way, it is possible to identify different components of perceived parenting self-efficacy: one related to the interpretation of emotional aspects and the other focused on somatic cues. In addition, the factor “situational beliefs” reported in the original study was not supported in this study; this seemed reasonable because this factor included only three items referring to overall interaction with the baby. Based on our data, these three items are loaded on different factors.
It would be interesting to elaborate the comparisons between the findings of this study with those derived from the initial English sample (Barnes & Adamson-Macedo, 2007). There were no differences in mean PMP S-E total score between the two samples, but the factors demonstrate different relevance in explaining the variability in perception of parenting self-efficacy. More specifically, the factor “care-taking procedures” was the main component in the English sample, as it explained about half of the total variability of parenting self-efficacy; by contrast, in the Italian sample, this factor contributes only marginally. In interpreting these results, the characteristics of the samples should be considered as possible source of differences. In particular, in the English study, the PMP S-E was completed 10 ± 6 days after delivery, whereas in this study, the assessment was performed 39 ± 33 days after delivery. Perception of parenting self-efficacy may change over time. In the early period after delivery, mothers may be focused on their performance in relation to the basic needs of care, while those relating to more complex tasks become salient only later. This is in line with a previous study showing that there is an association between the time interval between the delivery and the assessment of parenting self-efficacy and the perception reported by mothers (Pitetti, Smith, & Hsiao, 2016). Moreover, context-related factors (e.g. organization of the NICU, availability of early intervention for parents) should be considered. Specific interventions focused on mother–infant interaction were found to be effective in reducing stress related to parental role alteration (Kaaresen et al., 2006). Therefore, both the period in which the assessment is conducted and context-related factors may potentially explain the differences in the results obtained from the two studies. Based on the above considerations, future studies should clarify the association between personal factors, environmental variables and perceived parenting self-efficacy.
As concerns test–retest reliability, the coefficient of correlation of the total score was high over a 2-week period, and the coefficients of the factors ranged from moderate to good, thus supporting the test–retest reliability of the questionnaire. The PMP S-E showed moderate correlations with the GSES, which is the gold-standard measure of general self-efficacy (Schwarzer & Jerusalem, 1995). There were also significant associations between PMP S-E, EPDS and PSI-SF/Pd, but the correlation coefficients were lower than those with GSES: this confirms that the PMP S-E measures a related, but distinct, construct. Notably, the associations followed the expected trend, with higher parenting self-efficacy associated with lower depression and stress. These findings suggest the existence of reciprocal influence between these psychological variables and this may also explain why interventions targeting parenting self-efficacy have a positive effect on maternal mental health (Kaaresen et al., 2006; Melnyk et al., 2006). Finally, despite the fact that it goes beyond the primary scope of the study, it is interesting to note that one-third of the mothers showed EPDS scores over the cut-off recommended for the identification of clinical cases of perinatal depression. This is relevant because the assessment was conducted close to discharge from the NICU, thus confirming the need for careful monitoring of mothers in this vulnerable phase to ensure functional interaction with neonates (Shaw et al., 2013; Woolf et al., 2016).
Strengths and Limitations
The findings can be considered robust because the sample size exceeds the minimal requirements for factor analysis (i.e. five to seven subjects for each item) (Tabachnick & Fidell, 2007; Bryant & Yarnold, 1995). Secondly, no strict inclusion criteria were set, and few mothers refused to participate. The age and the educational level of the sample are similar to those reported in previous studies conducted in Northern Italy; however, our findings cannot be considered representative of the full population of mothers of preterm neonates. Indeed, in Italy, a considerable proportion of preterm neonates (13.6%) are born to recently arrived immigrant mothers. Moreover, immigrant women have a higher risk of premature birth (Sosta et al., 2008; Zanconato, Iacovella, Parazzini, Bergamini, & Franchi, 2011). Thirdly, confirmation of these findings through multicentre studies would be appropriate. Finally, a rigorous approach to test the concurrent validity of the PMP S-E would require the measurement of the same construct (i.e. parenting self-efficacy) but this was not possible given the unavailability of the relevant instruments in Italy.
Conclusion
The study was conducted on a large sample of Italian mothers of preterm neonates and it supported the validity and the reliability of the Italian version of the PMP S-E. Considering that parenting self-efficacy is potentially associated with the quality of parent–baby interaction, the use of this questionnaire could have strong clinical and research implications. Indeed, the early enhancement of parent–baby interaction is of long-term benefit to the neurodevelopment process of preterm neonates. This study also helps improve knowledge about the construct of parenting self-efficacy and provides evidence of its manifestation in Italy.
References
Abidin, R. R. (2012). Parenting stress index. Odessa: Psychological Assessment Resources.
Als, H., Duffy, F. H., McAnulty, G., Butler, S. C., Lightbody, L., Kosta, S., … Warfield, S. K. (2012). NIDCAP improves brain function and structure in preterm infants with severe intrauterine growth restriction. Journal of Perinatology, 32, 797–803. https://doi.org/10.1038/jp.2011.201.
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioural change. Psychological Review, 84, 191–215.
Barnes, C. R., & Adamson-Macedo, E. N. (2007). Perceived Maternal Parenting Self-Efficacy (PMP S-E) tool: Development and validation with mothers of hospitalized preterm neonates. Journal of Advanced Nursing, 60, 550–560. https://doi.org/10.1111/j.1365-2648.2007.04445.x.
Benvenuti, P., Ferrara, M., Niccolai, C., Valoriani, V., & Cox, J. L. (1999). The Edinburgh Postnatal Depression Scale: Validation for an Italian sample. Journal of Affective Disorders, 53, 137–141.
Benzies, K. M., Magill-Evans, J. E., Hayden, K. A., & Ballantyne, M. (2013). Key components of early intervention programs for preterm infants and their parents: A systematic review and meta-analysis. BMC Pregnancy Childbirth, 13, S10. https://doi.org/10.1186/1471-2393-13-S1-S10.
Blencowe, H., Cousens, S., Oestergaard, M. Z., Chou, D., Moller, A. B., Narwal, R., … Lawn, J. E. (2012). National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. The Lancet, 379, 2162–2172. https://doi.org/10.1016/S0140-6736(12)60820-4.
Bracht, M., OʼLeary, L., Lee, S. K., & OʼBrien, K. (2013). Implementing family-integrated care in the NICU: A parent education and support program. Advance in Neonatal Care, 13, 115–126. https://doi.org/10.1097/ANC.0b013e318285fb5b.
Bryant, F. B., & Yarnold, P. R. (1995). Principal-components analysis and exploratory and confirmatory factor analysis. In L. G. Grimm & P. R. Yarnold (Eds.), Reading and understanding multivariate statistics (pp. 99–136). Washington, DC: American Psychological Association.
Cabrera-Nguyen, P. (2010). Author Guidelines for reporting scale development and validation results. Journal of the Society for Social Work and Research, 1, 99–103.
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786.
Fonseca, A., Nazaré, B., & Canavarro, M. C. (2013). Parental psychological distress and confidence after an infant’s birth: The role of attachment representations in parents of infants with congenital anomalies and parents of healthy infants. Journal of Clinical Psychology in Medical Settings, 20, 143–155. https://doi.org/10.1007/s10880-012-9329-9.
Forcada-Guex, M., Borghini, A., Pierrehumbert, B., Ansermet, F., & Muller-Nix, C. (2011). Prematurity, maternal posttraumatic stress and consequences on the mother-infant relationship. Early Human Develepment, 87, 21–26. https://doi.org/10.1016/j.earlhumdev.2010.09.006.
Guarino, A., Di Blasio, P., D’Alessio, M., Camicasca, E., & Serantoni, G. (2012). Parenting stress index: manuale. Florence: Giunti O.S.
Heidari, H., Hasanpour, M., & Fooladi, M. (2012). The Iranian parents of premature infants in NICU experience stigma of shame. Medicinski Archives, 66, 35–40.
Hess, C. R., Teti, D. M., & Hussey-Gardner, B. (2004). Self-efficacy and parenting of high-risk infants: The moderating role of parent knowledge of infant development. Applied Developmental Psychology, 25, 423–437.
Heydarpour, S., Keshavarz, Z., & Bakhtiari, M. (2016). Factors affecting adaptation to the role of motherhood in mothers of preterm infants admitted to the neonatal intensive care unit: A qualitative study. Journal of Advanced Nursing, 73, 138–148.
Holditch-Davis, D., Miles, M. S., Burchinal, M. R., & Goldman, B. D. (2011). Maternal role attainment with medically fragile infants: Part 2. relationship to the quality of parenting. Research in Nursing and Health, 34, 35–48. https://doi.org/10.1002/nur.20418.
Holland, M. L., Yoo, B. K., Kitzman, H., Chaudron, L., Szilagyi, P. G., & Temkin-Greener, H. (2011). Self-efficacy as a mediator between maternal depression and child hospitalizations in low-income urban families. Maternal and Child Health Journal, 15, 1011–1019. https://doi.org/10.1007/s10995-010-0662-z.
Horbar, J. D., Carpenter, J. H., Badger, G. J., Kenny, M. J., Soll, R. F., Morrow, K. A., & Buzas, J. S. (2012). Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics, 129, 1019–1026. https://doi.org/10.1542/peds.2011-3028.
Jones, T. L., & Prinz, R. J. (2005). Potential roles of parental self-efficacy in parent and child adjustment: A review. Clinical Psychology Review, 25(3), 341–363.
Kaaresen, P. I., Rønning, J. A., Ulvund, S. E., & Dahl, L. B. A. (2006). Randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics, 118, e9–e19.
Leyenaar, J. K., O’Brien, E. R., Leslie, L. K., Lindenauer, P. K., & Mangione-Smith, R. M. (2017). Families’ priorities regarding hospital-to-home transitions for children with medical complexity. Pediatrics. https://doi.org/10.1542/peds.2016-1581.
Luszczynska, A., Scholz, U., & Schwarzer, R. (2005). The general self-efficacy scale: Multicultural validation studies. The Journal of Psychology, 139, 439–457.
McAnulty, G. B., Duffy, F. H., Butler, S. C., Bernstein, J. H., Zurakowski, D., & Als, H. (2010). Effects of the Newborn Individualized Developmental Care and Assessment Program (NIDCAP) at age 8 years: Preliminary data. Clinical Pediatrics, 49, 258–270. https://doi.org/10.1177/0009922809335668.
Melnyk, B. M., Feinstein, N. F., Alpert-Gillis, L., Fairbanks, E., Crean, H. F., Sinkin, R. A., … Gross, S. J. (2006). Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: A randomized, controlled trial. Pediatrics, 118, e1414–e1427. https://doi.org/10.1542/peds.2005-2580.
Montirosso, R., Del Prete, A., Bellù, R., Tronick, E., Borgatti, R., & Neonatal Adequate Care for Quality of Life (NEO-ACQUA) Study Group (2012a). Level of NICU quality of developmental care and neurobehavioral performance in very preterm infants. Pediatrics, 129, e1129–e1137. https://doi.org/10.1542/peds.2011-0813.
Montirosso, R., Provenzi, L., Calciolari, G., Borgatti, R., & NEO-ACQUA Study Group (2012b). Measuring maternal stress and perceived support in 25 Italian NICUs. Acta Paediatrica, 101, 136–142. https://doi.org/10.1111/j.1651-2227.2011.02440.x.
Morsbach, S. K., & Prinz, R. J. (2006). Understanding and improving the validity of self-report of parenting. Clinical Child and Family Psychological Review, 9, 1–21.
Nordhov, S. M., Rønning, J. A., Ulvund, S. E., Dahl, L. B., & Kaaresen, P. I. (2012). Early intervention improves behavioral outcomes for preterm infants: Randomized controlled trial. Pediatrics, 129, e9–e16. https://doi.org/10.1542/peds.2011-0248.
Ohgi, S., Fukuda, M., Akiyama, T., & Gima, H. (2004). Effect of an early intervention programme on low birthweight infants with cerebral injuries. Journal of Paediatric and Child Health, 40, 689–695. https://doi.org/10.1111/j.1440-1754.2004.00512.x.
Ortenstrand, A., Westrup, B., Brostrom, E. B., Sarman, I., Akerström, S., Brune, T., … Waldenström, U. (2010). The Stockholm Neonatal Family-Centered Care Study: Effects on length of stay and infant morbidity. Pediatrics, 125, e278–e285. https://doi.org/10.1542/peds.2009-1511.
Özyurt, G., Özyurt, A., Ozturk, T., Yaman, A., & Berk, A. T. (2018). Evaluation of maternal attachment, self-efficacy, levels of depression, and anxiety in mothers who have babies diagnosed with retinopathy of prematurity. Ophthalmic Epidemiology, 25, 140–146. https://doi.org/10.1080/09286586.2017.1372487.
Parker, S., & Zahr, L. K. (1985). The maternal confidence questionnaire. Boston: Boston City Hospital.
Pitetti, K., Smith, B., & Hsiao, R. (2016). Application of Perceived Maternal Parenting Self-Efficacy (PMP S-E) questionnaire in a Mid-West Community Medical Center NICU in the United States. Neonatal Pediatric Medicine, 1, 106. https://doi.org/10.4172/2572-4983.1000106.
Roman, L. A., Lindsay, J. K., Boger, R. P., De Wys, M., Beaumont, E. J., Jones, A. S., & Haas, B. (1995). Parent-to-parent support initiated in the neonatal intensive care unit. Research in Nursing and Health, 18, 385–394.
Schwarzer, R., & Jerusalem, M. (1995). Generalized self-efficacy scale. In J. Weinman, S. Wright & M. Johnston (Eds.), Measures in health psychology: A user’s portfolio (pp. 35–37). Windsor: NFER-Nelson.
Shaw, R. J., Bernard, R. S., Storfer-Isser, A., Rhine, W., & Horwitz, S. M. (2013). Parental coping in the neonatal intensive care unit. Journal of Clinical Psychology in Medical Settings, 20, 135–142. https://doi.org/10.1007/s10880-012-9328-x.
Sosta, E., Tomasoni, L. R., Frusca, T., Triglia, M., Pirali, F., El Hamad, I., & Castelli, F. (2008). Preterm delivery risk in migrants in Italy: An observational prospective study. Journal of Travel Medicine, 15, 243–247. https://doi.org/10.1111/j.1708-8305.2008.00215.x.
Tabachnick, B. G., & Fidell, L. S. (2007). Using multivariate statistics (5th ed.) Boston: Allyn and Bacon.
Teti, D. M., Black, M. M., Viscardi, R., Glass, P., O’Connell, M. A., Baker, L., … Hess, C. R. (2009). Intervention with African American premature infants: Four-month results of an early intervention program. Journal of Early Intervention, 31, 146–166.
Teti, D. M., & Gelfand, D. M. (1991). Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development, 62, 918–929.
Teti, D. M., Hess, C. R., & O’Connell, M. (2005). Parental perceptions of infant vulnerability in a preterm sample: Pre diction from maternal adaptation to parenthood during the neonatal period. Journal of Developmental and Behavioral Pediatrics, 26, 283–292.
Warschburger, P., & Kühne, D. (2014). Psychosocial determinants of quality of life in parents of obese children seeking inpatient treatment. Quality of Life Research, 23, 1985–1995.
Westrup, B. (2015). Family-centered developmentally supportive care: The Swedish example. Archives of Pediatrics, 22, 1086–1091. https://doi.org/10.1016/j.arcped.2015.07.005.
Woolf, C., Muscara, F., Anderson, V. A., & McCarthy, M. C. (2016). Early traumatic stress responses in parents following a serious illness in their child: A systematic review. Journal of Clinical Psychology in Medical Settings, 23, 53–66.
Worthington, R. L., & Whittaker, T. A. (2006). Scale development research: A content analysis and recommendations for best practices. The Counseling Psychologist, 34, 806–838.
Zanconato, G., Iacovella, C., Parazzini, F., Bergamini, V., & Franchi, M. (2011). Pregnancy outcome of migrant women delivering in a public institution in northern Italy. Gynecology and Obstetrical Investigation, 72, 157–162.
Acknowledgements
The Authors would like to thank all the mothers who participated to the study and Professor Gaetano Chirico as representative of all the clinicians of the Neonatal Intensive Care Unit of Spedali Civili in Brescia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Laura Pedrini, Clarissa Ferrari and Alberto Ghilardi declare that they have no conflict of interest.
Human and Animal Rights
All procedures performed in studies involving human participants were complied with the ethical standards of the Italian National Research Council and with the 1964 Declaration of Helsinki and subsequent amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants who participated in the study.
Rights and permissions
About this article
Cite this article
Pedrini, L., Ferrari, C. & Ghilardi, A. Psychometric Properties of the Italian Perceived Maternal Parenting Self-Efficacy (PMP S-E). J Clin Psychol Med Settings 26, 173–182 (2019). https://doi.org/10.1007/s10880-018-9578-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-018-9578-3