Abstract
A systematic review of the literature investigating the early traumatic stress responses in parents of children diagnosed with a serious illness/injury. A literature review was conducted (September 2013) using Medline, PsycINFO, and CINAHL databases. Twenty-four studies related to parents of children hospitalized due to diagnosis of cancer, type 1 diabetes, meningococcal disease, trauma or serious injury, preterm birth and other serious illnesses requiring admission to intensive care were included. Parents were assessed for early traumatic stress symptoms within 3 months of their child’s diagnosis/hospitalization. Prevalence rates of acute stress disorder in parents ranged from 12 to 63 %. Prevalence of posttraumatic stress disorder ranged from 8 to 68 %. Variability was related to methodological factors including differences in study design, timing of assessments, measurement tools, and scoring protocols. Psychosocial factors rather than medical factors predicted parent distress. This review integrates and compares early traumatic reactions in parents with children suffering a range of serious illnesses. Findings suggest a high prevalence of acute and posttraumatic stress symptoms in parents. Methodological inconsistencies made comparison of early traumatic stress prevalence rates difficult. Risk factors associated with traumatic stress symptoms were identified.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Serious childhood illnesses or injuries (SCII) that are life-threatening can have a significant impact on both child and parent psychological wellbeing (Landolt, Ystrom, Sennhauser, Gnehm, & Vollrath, 2012; Nugent, Ostrowski, Christopher, & Delahanty, 2007). Findings suggest that after a diagnosis of SCII, parents suffer increased psychological distress (Bruce, 2006; Hall et al., 2006; Pai et al., 2007), are at higher risk of developing symptoms of depression and anxiety (Doherty et al., 2009; van Oers et al., 2014), and may be at risk for persisting psychiatric morbidity (Bryant, Creamer, O’Donnell, Silove, & McFarlane, 2012).
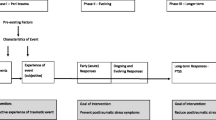
A diagnosis of SCII represents a potential psychological trauma for parents, as it involves the risk of death, serious injury, or threat to the child’s short and/or long-term health. While most parents adapt well over time to their child’s diagnosis (Kazak, 1994; Pai et al., 2007), a subset of parents will develop significant posttraumatic stress symptoms (Bronner et al., 2010; Kazak et al., 2006), including posttraumatic stress disorder (PTSD), which can significantly impair daily functioning (Best, Streisand, Catania, & Kazak, 2001; Young et al., 2003). Although acute traumatic stress reactions can be transient, a proportion of affected individuals will go on to experience debilitating and chronic posttraumatic stress symptoms (PTSS). Early detection of individuals at risk of suffering PTSS potentially allows for early intervention, and prevention of later mental health problems (Bryant, Sackville, Dang, Moulds, & Guthrie, 1999). Furthermore, given that early parental responses to illness are associated with later psychological adaptation of their children, and that chronic PTSS has been reported in parents of children across an array of illnesses/injuries (Landolt et al., 2012; Stuber & Shemesh, 2006), it is critical to characterize and better understand this response in this population.
Since the inclusion of a diagnosis of a life threatening illness in one’s child was recognized as a potentially traumatic event in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV: American Psychiatric Association, 1994), a significant body of literature has utilized a posttraumatic stress framework to examine the psychological responses of parents with ill or injured children (Balluffi et al., 2004; Winston et al., 2002). A smaller body of literature has examined acute or early traumatic stress responses of parents, which may be predictive of longer-term distress. According to the DSM-IV, for both Acute Stress Disorder (ASD) and PTSD, the individual must experience intense fear, horror, or helplessness in response to a traumatic event, as well as symptoms of re-experiencing, avoidance and physiological arousal associated with functional impairment. An ASD diagnosis also requires the presence of dissociative symptoms. ASD designates the presence of symptoms in the early post-trauma period (with onset and duration between 2 days and 4 weeks after the traumatic event), whereas PTSD is diagnosed when symptoms persist for at least 1 month (American Psychiatric Association, 1994). In addition, sub-clinical presentations of PTSD, commonly referred to as PTSS, can result in significant functional impairment for affected individuals (Stein, Walker, Hazen, & Forde, 1997).
Three previous reviews have examined parental posttraumatic stress in the context of childhood illness. Prevalence of parental PTSD following the diagnosis of childhood cancer ranged from 27 to 54 % (Bruce, 2006) and 10–30 % (Taïeb, Moro, Baubet, Revah-Lévy, & Flament, 2003), where PTSD was assessed 3 days to 33 years post-treatment and three to 6 years post-treatment, respectively. In a review of studies examining parents of children diagnosed with a chronic illness who were 3–6 years post treatment, the pooled prevalence of parental PTSD was reported to be 22.8 % (Cabizuca, Marques-Portella, Mendlowicz, Coutinho, & Figueira, 2009). The current review will extend previous work by focussing on parent reactions in the acute period post-diagnosis (within the first 3 months), rather than investigating chronic and longer term parent responses, as has been the case in all the previous reviews. Further, the current review includes 8 studies that were published after the most recent previous review.
To the best of our knowledge, there is no previous systematic review synthesizing the existing evidence for early parental traumatic stress following the diagnosis of a range of SCIIs. Such a review will contribute to current understanding of parents’ response to the diagnosis of SCII in their child, will inform hospital-wide clinical health service responses to parent distress, and potentially facilitate the development of preventative, evidence-based and generalizable parent interventions which are currently sparse. The majority of studies identified in this review are based on DSM-IV diagnostic criteria, and results remain relevant in the characterization of reactions in parents of children with SCII in a clinical context. Given the recent release of DSM-V (American Psychiatric Association, 2013), which involves some key changes to criteria for PTSD and ASD, a review of the literature to date is particularly timely and will potentially be useful in examining future directions of trauma-focused research in the pediatric medical context.
The aim of this systematic review was to provide a critique of studies investigating parental ASD, PTSD or PTSS in the acute period following the diagnosis of a SCII. Our primary research objective is to examine the prevalence of acute and/or posttraumatic stress symptoms in parents in the early period following the diagnosis of a SCII, and determine factors that may impact the variable parental responses to SCII.
Methods
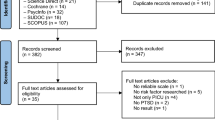
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (The PRISMA Statement; Moher, Liberati, Tetzlaff, & Altman, 2009). Three databases were searched in September 2013. There was no restriction on years in the search. The search yielded eligible papers published between 1998 and 2013. The search algorithms used for each database were: Medline: MeSH headings: (‘Parents’ OR ‘Caregivers’) AND (‘Neoplasms+’ OR ‘Burns+’ OR ‘Accidents, Traffic’ OR ‘Intensive Care, Neonatal’ OR ‘Intensive Care Units, Pediatric’ OR ‘Asthma+’ OR ‘Diabetes Mellitus+’ OR ‘Chronic Disease’ OR ‘Cerebral Palsy’ OR ‘Child Development Disorders, Pervasive+’ OR ‘Arthritis, Rheumatoid+’ OR ‘Cystic Fibrosis’ OR ‘Communicable Diseases+’ OR ‘Brain Injuries+’) AND (‘Stress Disorders, Traumatic+’); PsycINFO: Thesaurus terms: (‘Parents’ OR ‘Caregivers’) AND (‘Neoplasms’ OR ‘Burns’ OR ‘Organ Transplantation’ OR ‘Asthma’ OR ‘Diabetes’ OR ‘Intensive Care’ OR ‘Neonatal Intensive Care’ OR ‘Chronic Illness’ OR ‘Cerebral Palsy’ OR ‘Pervasive Developmental Disorders’ OR ‘Rheumatoid Arthritis’ OR ‘Cystic Fibrosis’ OR ‘Infectious Disorders’ OR ‘Traumatic Brain Injury’) AND (‘Posttraumatic Stress Disorder’ OR ‘Acute Stress Disorder’); CINAHL: Thesaurus terms: (‘Parents+’ OR ‘Caregivers’) AND (‘Neoplasms+’ OR ‘Burns+’ OR ‘Accidents, Traffic’ OR Intensive Care Units, Pediatric+’ OR ‘Chronic Disease’ OR ‘Asthma+’ OR ‘Diabetes Mellitus+’ OR ‘Cerebral Palsy’ OR ‘Child Development Disorders, Pervasive+’ OR ‘Arthritis, Rheumatoid+’ OR ‘Cystic Fibrosis’ OR ‘Communicable Diseases+’ OR ‘Brain Injuries+’) AND (‘Stress Disorders, Post-Traumatic+’).
Inclusion criteria were observational or interventional studies, published in English in a peer-reviewed journal, with a quantitative design, that assessed early posttraumatic stress symptoms in parents with a child: (1) 18 years or younger; (2) diagnosed with a SCII which involved threat of death or physical integrity of the child; and (3) diagnosed/hospitalized less than 3 months prior to assessment. A standardized measure of PTSS, ASD or PTSD was also a requirement. The search resulted in 209 abstracts after duplicates were removed, which were screened by the primary authors. Where abstracts were relevant or where review was not possible from the abstract alone, full text articles were retrieved (n = 70). Studies not meeting inclusion criteria were discarded (n = 185; see Fig. 1). Reference lists of the included studies were examined manually, yielding an additional six studies, resulting in a total of 30 included studies. Inter-rater agreement between the two reviewers regarding article eligibility for inclusion was 100 %.
Quality Assessment
A quality assessment approach previously described (Jackson, Cheater, & Reid, 2008) was undertaken, with each included study independently assessed by the primary authors. This particular quality assessment approach was chosen as it is utilizes validated tools (Jackson et al., 2008), offers a systematic approach to quality assessment, and has been used in previous systematic reviews involving similar samples (Green, Knight, McCarthy, & DeLuca, 2013; Wakefield, McLoone, Butow, Lenthen, & Cohn, 2011). This approach consists of 15 quality criteria (see Table 1). Inter-rater agreement was 97.7 % and Kappa corrected agreement was 93.6 %. The majority of studies described an explicit theoretical framework, study aims, data collection and analysis procedures, evidence of critical reflection, use of validated measures and study limitations (see Table 1). However, study samples were often poorly described (41.6 %), and a very limited number of articles included a control group (8.3 %). Overall, the quality of included studies was variable. Thirteen studies were considered ‘high quality’ (i.e., ≥13 criteria met) and six studies were considered ‘poor’ quality (i.e. ≤10 criteria met). In those studies considered to be of poor quality, the quality criteria most frequently not addressed were the inclusion of a control group, a clear description of the sample, a clear description of the data analysis procedure, the use of an appropriate sampling procedure, a description of the validity and reliability of the results, and the provision of information regarding attrition. Poor quality studies were removed from further analysis, leaving a total of 24 included articles.
Results
Characteristics of Study Samples
Sample size varied from 23 to 460 parents in the studies reviewed; Four studies had a sample less than 50 and nine studies had a sample size that exceeded 200. SCII diagnoses included children: admitted to the NICU or born preterm (n = 4), hospitalized due to road traffic accidents (RTAs; n = 6), with a new cancer diagnosis (n = 5), admitted to the Pediatric Intensive Care Unit (PICU; n = 2), with a new type 1 diabetes diagnosis (n = 2), and children with a meningococcal disease diagnosis (n = 1). Four additional studies included multiple medical conditions. Tables 2 and 3 summarize the articles included in the review.
Prevalence of Parental Traumatic Stress Symptoms
Eleven studies examined parental ASD or acute stress symptoms within a period of zero days to less than 4 weeks following diagnosis of a SCII. Nine specifically investigated parental ASD, and two investigated acute PTSS only. Of the nine studies investigating ASD, four also examined parental PTSS in the acute period or PTSD over time. A further 13 studies examined PTSD or PTSS alone across a period ranging from 4 weeks to 3 months. The prevalence of ASD ranged from 12 % in parents of children involved in RTAs to 63 % in mothers of children newly diagnosed with cancer. The majority of studies (n = 7), however, reported a prevalence of approximately 30 %, although two studies of parents of children newly diagnosed with cancer reported ASD rates of 50–60 %. The prevalence of PTSD in parents 30 days to three months post diagnosis ranged from 8 % in fathers of children admitted to the neonatal intensive care unit (NICU) to 68 % in parents of children who were involved in RTA, burn accidents or newly diagnosed with cancer. The majority of studies, however, reported prevalence rates of PTSD between 15 and 25 %.
Risk Factors Associated with Parental Traumatic Stress Symptoms
Demographic Factors
With respect to parent gender; four studies did not specify participant gender: two studies recruited only mothers, and one study only included fathers. Seven studies reported on approximately equal numbers of mothers and fathers, although in the majority of studies mothers were more highly represented. Overall, demographic factors were not found to consistently predict parent outcomes. Female gender was reported to be associated with the development of acute and posttraumatic parental stress symptoms in many studies investigating gender (n = 6). There were, however, four studies where gender was not associated with acute and/or posttraumatic stress responses. Three studies reported that parents of non-Caucasian ethnicity were at a greater risk for developing early traumatic stress responses, however this finding was not replicated in four other studies. Three studies reported that younger aged parents were more likely to develop acute and/or posttraumatic stress responses than older-aged parents, but three other studies reported no such association. Findings were also inconsistent for socioeconomic status (SES). Four studies reported parents with lower SES were more likely to develop ASD or PTSD, and six other studies described no such relationship. There was some limited evidence that parents with lower levels of education were more likely to develop significant acute and/or posttraumatic stress responses (n = 3). No studies found that child age and gender were associated with parent responses, with seven studies specifically finding no relationship between these factors.
Psychosocial Factors
Parents’ previous experience of stressful life events or trauma (n = 8), parent perception of life threat to their child (n = 4), and parent trait anxiety (n = 3) and levels of depressive symptoms (n = 3) were all identified as contributing to the development of acute and posttraumatic symptomatology. Inconsistent findings were reported regarding family structure; one study reported that single parent families were at a greater risk of acute and/or posttraumatic stress symptomatology than two-parent families, and two other studies reported no such association. Likewise, family cohesion (n = 2) and child ASD/PTSD symptoms (n = 3) were associated with parent psychological ASD and/or PTSD in some studies, but were not found to be related in other studies (n = 2 and n = 2, respectively).
Medical Factors
Illness severity or length of hospital admission were not associated with parental acute and posttraumatic stress symptomatology in the majority of studies (n = 10). In contrast, five studies found associations between illness severity, functional status, days in hospital and acute and/or posttraumatic stress responses.
Methodological Factors
Methodological factors identified as important and likely contributing to inconsistencies in findings included: study design, differences in the timing of assessments, variability in measurement tools, and differences in scoring methods. Study designs included cross-sectional, longitudinal, and intervention studies (see Table 2).
Assessment Timing
Four of the cross-sectional studies assessed parents within 1 month, and seven assessed parents greater than 1 month (and less than 3 months) after their child’s diagnosis. Eight of the longitudinal studies included an assessment time point within 1 month (from 0 days to less than 4 weeks), four had an assessment time point at 1 month, three at 2 months, and three at 3 months post-diagnosis. All longitudinal studies involved assessment time points that were greater than 3 months (beyond the scope of the current review). Three of the longitudinal studies had one assessment time point and eight had two time points within the three-month period post-diagnosis. With regard to the intervention studies, one had an assessment time point within 1 month, and one within 2 months post-diagnosis.
Measures and Scoring Methods
Six studies used the Acute Stress Disorder Scale (ASDS), and three studies used the Stanford Acute Stress Reaction Questionnaire to measure ASD. For PTSD, the Posttraumatic Diagnostic Scale (PDS) was the most frequently used measure (n = 6), followed by the PTSD Checklist (PCL; n = 4). Other studies used the Perinatal Posttraumatic Stress Disorder Questionnaire, Self-Rating Scale for PTSD, and PTSD Symptom Scale Interview to measure PTSD. Five studies used the Impact of Events Scale (IES). Different scoring methods for measures were also employed, including clinical cutoffs (n = 3), categorical scores (n = 4) and symptom severity scores (n = 9) while others failed to report on the scoring method used and how scores were classified or interpreted (n = 3).
Discussion
This review systematically examined the current literature exploring the prevalence of acute and/or posttraumatic stress symptoms and/or disorders in parents immediately (<3 months) following the diagnosis of a SCII, the risk factors associated with posttraumatic responses and methodological issues within this body of literature.
Prevalence
In general, there was a large range (12–63 %) of reported prevalence of ASD, with the majority of studies reporting a prevalence of approximately 24–40 %. Studies involving parents of children newly diagnosed with cancer tended to report higher rates of ASD symptoms. Similarly, there was a large range in the prevalence of PTSD reported (8–68 %), although the majority reported a prevalence of 15–25 %. Overall, the findings indicate that up to one quarter to one third of parents experience traumatic stress symptoms at a clinically significant level following the diagnosis of a SCII in their child.
Some psychosocial factors (prior trauma, history of mental health issues, trait anxiety, and parent perception of life threat to their child) were consistently found to be associated with parental acute and posttraumatic stress symptomatology. Dissociation was also found to be associated with later traumatic stress symptomatology in the one and only study to explore this relationship (Row 1 of Table 3, Allenou et al., 2003). Findings regarding demographic factors were mixed, and child factors such as child age and gender were not found to be associated with parent outcomes. Medical factors (illness severity, length of hospital stay) were either not predictive, or inconsistently predicted, parent outcomes. The finding that medical factors (e.g. illness severity, length of hospital admission) were generally not associated with parental acute and posttraumatic stress symptomatology is consistent with cognitive models of trauma which emphasize the role of dysfunctional, subjective appraisals that individuals make about the trauma (in this case, child illness), rather than the trauma itself as being critical to posttraumatic adjustment (Ehlers & Clark, 2000). It has therefore been suggested that treatment interventions targeting parental psychological variables, regardless of child’s medical diagnosis, may have the potential to prevent PTSS (Shaw, Bernard, Deblois, Ikuta, Ginzburg, & Koopman, 2009).
The variable rates of ASD and PTSD reported across the studies reviewed may be related to a range of factors. Firstly, the heterogeneity of the samples described in the field raises the possibility of different pathogenic pathways (Landolt, Vollrath, Ribi, Gnehm, & Sennhauser, 2003). For example, the immediate life threat associated with childhood cancer may play an important role for parents, as many of these children are likely to be in the early phases of intense, painful treatments, possibly making the threat of death more salient (Row 21 of Table 2, Landolt et al., 2003; also see Row 22, Landolt et al., 2012). In line with this, other studies reported that mothers who had been in or had witnessed an accident that involved their child were significantly more likely to have traumatic stress symptoms (Bryant, Mayou, Wiggs, Ehlers, & Stores, 2004; de Vries et al., 1999). Interestingly, although the threat or salience of death may appear critical in the development of traumatic stress disorders in parents, many studies reported no association between objective medical characteristics (such as length of hospital stay, severity of illness, length of ventilatory support, and risk of mortality) and traumatic stress symptomatology in parents (Row 1 of Table 3, Allenou et al., 2010; Row 16, Balluffi et al., 2004; Row 17, Bronner, Knoester, Bos, Last, & Grootenhuis, 2008; Row 23, Landolt, Boehler, Schwager, Schallberger, & Nuessli, 1998; Row 18, Landolt et al., 2002; Row 13, Lefkowitz, Baxt, & Evans, 2010; Row 14, Shaw et al., 2006). This finding is consistent with Kazak’s model of medical traumatic stress which contends that it is the subjective appraisal of threat not illness factors that will predict an individual’s response to a diagnosis (Kazak et al., 2006).
Methodological factors also likely contribute to variability in findings. Variations in study design, in particular timing of assessments, likely contributed to variable findings and rendered comparison across studies difficult. For this review, “early” traumatic responses were defined as parental ASD, PTSD or PTSS investigated within 3 months following the diagnosis of a SCII. There is currently limited understanding of the impact of timing of assessment on traumatic stress symptoms. This is especially the case for assessment within the “acute” period, when individuals experience transient stress reactions that will potentially abate in the following days (Bryant, Friedman, Spiegel, Ursano, & Strain, 2011). Determining the optimal time to assess for traumatic stress in the acute period is further complicated by the notion that stress reactions are largely influenced by contextual factors (Bryant et al., 2011). For example, it is possible that the higher rates of ASD symptoms reported in parents of children with cancer may be related to societal associations between cancer and death, or may be associated with the abrupt onset of invasive treatments such as chemotherapy that may be perceived as further threats to the child (Row 8 of Table 2, McCarthy, Ashley, Lee, & Anderson, 2012).
Across all included studies, nine different measures were used. Of these, two different instruments were administered to measure ASD, six to measure PTSD and one to measure symptom severity or risk for PTSD. One study (Row 10 of Table 2, Pöder, Ljungman, & von Essen, 2008) used the PCL-C (which does not measure dissociation) to index ASD. Further, different scoring protocols were employed to describe traumatic stress symptoms. Of the six studies that used the ASDS, three reported both categorical and continuous scores. The other studies did not describe their scoring protocol (Row 16 of Table 2, Balluffi et al., 2004), derived their own (Row 7 of Table 2, Kazak et al., 2005) or used the ASDS to measure PTSD (Row 11 of Table 2, Stehl et al., 2009). Similar ambiguities and variations in scoring protocols were identified in measures of PTSD. Of the six studies that used the PDS, none described their scoring protocol or reported clinical-cutoffs. Of the five studies using the PCL, two studies (Row 13 of Table 2, Lefkowitz et al., 2010; Row 10 of Table 2, Pöder et al., 2008) used a symptom cluster score and three used a symptom severity score (Row 1 of Table 2, Allenou et al., 2010; Row 16 of Table 2, Balluffi et al., 2004; Row 2 of Table 2, Kassam-Adams, Fleisher, & Winston, 2009).
Similarly for the IES, one study reported “high risk” to include individuals who scored above a cut-off of 26 (Row 5 of Table 2, Sturms et al., 2005; IES Dutch translation) and another reported “risk” to include individuals scoring above a cut-off of 35 (Row 20 of Table 2, Shears, Nadel, Gledhill, & Garralda, 2005).
A further issue with respect to measure methodology is the reliance on self-report measures to assess ASD and PTSD. Over 90 % of the studies examined used self-report measures, which do not allow for the assessment of Criterion F for ASD or PTSD in DSM-IV (that the traumatic stress symptoms cause “clinically significant distress or impairment in social, occupational, or other important areas of function”; American Psychiatric Association, 1994, p. 468). Further, evidence suggests that self-report measures often overestimate the rate of ASD and/or PTSD (Jones et al., 2006). Such measurement and methodological issues limit meaningful and useful conclusions regarding prevalence of parental traumatic stress responses. Stuber et al. (2011) noted that some studies focus on the number of stress symptoms present (yes/no for each symptom), while others focus on symptom severity or frequency, and yet others use the formal diagnostic criteria set by the DSM-IV. They argue that the variability in definitions has made it impossible to compare across studies and that, without common criteria defining PTSD, it is unlikely that consistent predictors of PTSD will be identified in clinical studies of childhood survivors of serious illness (Stuber et al., 2011).
Finally, a tendency to under-represent fathers and ethnic minorities in these studies is of concern. Whilst the majority of studies examined represented fathers well, three studies included mothers only (Row 1 of Table 2, Allenou et al., 2010; Row 12, Holditch-Davis et al., 2009; Row 15, Vanderbilt, Bushley, Young, & Frank, 2009) and in seven studies the sample comprised significantly more mothers than fathers. The exclusion of fathers is limiting considering recent evidence supporting the importance of fathers in healthcare contexts (Bronner et al., 2008). At least 10 studies excluded non-English (or relevant local language) speaking families, resulting in a predominately white, native speaking sample. This is pertinent as there is evidence to suggest that ethnicity, specifically, belonging to a minority ethnic group, may be a risk factor for posttraumatic stress (see Row 10 of Table 3, Pöder et al., 2008).
Limitations of this Study
Due to the limited data reported in the studies included in this review, the array of measures administered and scoring methods employed, only qualitative synthesis of findings was possible. In addition, our search was limited to studies published in English, and as such, results may not generalize to non-English speaking countries/cultures. Finally, only a very small number of studies used a control group, although these mostly included intervention studies, comparing the same cohort of families with ill children across different intervention arms. This limitation raises the challenges of incorporating a control group using healthy children in studies investigating posttraumatic stress responses in parents.
Future Research
For future research, consistency and consensus are needed regarding the operational definitions of traumatic stress responses and the measures used, in order to ensure a more standardized approach to data collection and to allow more meaningful comparison between studies. This is a particularly salient issue with the recent release of DSM-V (American Psychiatric Association, 2013) which includes some key changes in this field. In particular, the DSM-V Criterion A requires more explicit information on how the traumatic event was experienced and the subjective reaction of fear and helplessness (Criterion A2) is no longer required. Further, the emphasis on dissociation in an ASD diagnosis is reduced and the addition of a negative mood symptom cluster has been added to ASD and PTSD criteria.
With the release of DSM-V (American Psychiatric Association, 2013) and consistent with recommendations from Stuber et al. (2011), it is postulated that it may be more appropriate to conceptualize the ASD diagnosis as a means to identify individuals with clinically significant trauma reactions, such as marked fear or anxiety, in the initial month post-trauma. That is, acute stress reactions that are severe enough to warrant clinical attention (Bryant et al., 2011), but not prescribing that these symptoms need to be from specific clusters, such as dissociation (Bryant et al., 2011). Requiring a requisite number of symptoms may increase identification of acutely distressed individuals who may benefit from treatment by acknowledging the diversity of acute traumatic stress responses (Bryant et al., 2011). Given the changes to the DSM-V, the synthesis of findings contained in this review, and which have been based on DSM-IV criteria, are timely. Future research should be directed towards improved consensus on the application of traumatic stress responses to this population, and examination of the sensitivity of the altered DSM-V criteria in identifying distressed parents who would benefit from clinical care.
Clinical Implications
Findings from this review suggest that there is a high prevalence of traumatic stress symptoms in parents with children diagnosed with SCII. These findings contrast with estimates of lifetime prevalence of PTSD in the general adult population, which have been reported to range from 1 to 14 % (American Psychiatric Association, 1994). Importantly, early traumatic stress responses have been identified in parents with children with a range of illnesses and injuries suggesting that hospital-wide approaches for minimizing traumatic stress responses are warranted for children and families in the acute hospital setting. This extends the current literature, with previous reviews only focusing on a single illness group, or on more chronic and long-term outcomes. These findings will help to raise the awareness of medical and psychosocial clinicians about these difficulties and increase understanding of risk factors, which will allow for improved screening and detection of problems within the acute hospital setting. Given the impact that early traumatic responses have on parent and family functioning, and child recovery and outcome, earlier detection of maladaptive psychological responses in parents, combined with targeted intervention, will reduce the risk of chronic mental health problems developing in the longer term.
The development and evaluation of evidence based interventions, which are aimed at ameliorating distress or preventing longer term adjustment issues, and which can be applied within the hospital or community setting in a feasible and effective manner, is an important future goal (Kazak et al., 2005). To date there have been few studies examining the efficacy of psychological interventions of parents of seriously ill children. However, a small number of studies conducted with parents of children with cancer and cardiac disease in the early period following diagnosis have reported promising results for reducing parental distress (Burke et al., 2014; Sahler et al., 2002, 2005) and enhancing child adjustment (Fedele et al., 2013). Given the impact of early traumatic responses on parent and family functioning and child recovery and outcome, the findings of this review indicate that families affected by SCII need psychosocial intervention in the acute phase post the child’s diagnosis to reduce the risk of potential long term mental health problems.
References
References marked with an asterisk indicate studies included in the review
* Allenou, C., Olliac, B., Bourdet-Loubère, S., Brunet, A., David, A. C., Claudet, I., … Birmes, P. (2010). Symptoms of traumatic stress in mothers of children victims of a motor vehicle accident. Depression & Anxiety (1091–4269), 27, 652–657.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association.
American Psychiatric Association. (2013). Diagnostic and Statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
* Balluffi, A., Kassam-Adams, N. L., Kazak, A. E., Tucker, M., Dominguez, T., & Helfaer, M. (2004). Traumatic stress in parents of children admitted to the pediatric intensive care unit. Pediatric Critical Care Medicine: A Journal Of The Society Of Critical Care Medicine And The World Federation Of Pediatric Intensive And Critical Care Societies, 5, 547–553.
Best, M., Streisand, R., Catania, L., & Kazak, A. E. (2001). Parental distress during pediatric leukemia and posttraumatic stress symptoms (PTSS) after treatment ends. Journal of Pediatric Psychology, 26, 299–307.
* Bronner, M. B., Knoester, H., Bos, A. P., Last, B. F., & Grootenhuis, M. A. (2008). Follow-up after paediatric intensive care treatment: Parental posttraumatic stress. Acta Paediatrica, 97, 181–186.
Bronner, M. B., Peek, N., Knoester, H., Bos, A. P., Last, B. F., & Grootenhuis, M. A. (2010). Course and predictors of posttraumatic stress disorder in parents after pediatric intensive care treatment of their child. Journal of Pediatric Psychology, 35, 966–974.
Bruce, M. (2006). A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clinical Psychology Review, 26, 233–256.
Bryant, R. A., Creamer, M., O’Donnell, M., Silove, D., & McFarlane, A. C. (2012). The capacity of acute stress disorder to predict posttraumatic psychiatric disorders. Journal of Psychiatric Research, 46, 168–173.
Bryant, R. A., Friedman, M. J., Spiegel, D., Ursano, R., & Strain, J. (2011). A review of acute stress disorder in DSM-5. Depression and Anxiety, 28, 802–817.
Bryant, B., Mayou, R., Wiggs, L., Ehlers, A., & Stores, G. (2004). Psychological consequences of road traffic accidents for children and their mothers. Psychological Medicine, 34, 335–346.
Bryant, R. A., Sackville, T., Dang, S. T., Moulds, M., & Guthrie, R. (1999). Treating acute stress disorder: An evaluation of cognitive behavior therapy and supporting counselling techniques. American Journal of Psychiatry, 156, 1780–1786.
Burke, K., Muscara, F., McCarthy, M. C., Dimovski, A., Hearps, S. J., Anderson, V., & Walser, R. (2014). Adapting acceptance and commitment therapy for parents of children with life-threatening illness: Pilot study. Families, Systems, & Health, 32, 122–127. doi:10.1037/fsh0000012.
Cabizuca, M., Marques-Portella, C., Mendlowicz, M. V., Coutinho, E. S. F., & Figueira, I. (2009). Posttraumatic stress disorder in parents of children with chronic illnesses: A meta-analysis. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 28(3), 379–388.
de Vries, A. P. J., Kassam-Adams, N., Cnaan, A., Sherman-Slate, E., Gallagher, P. R., & Winston, F. K. (1999). Looking beyond the physical injury: Posttraumatic stress disorder in children and parents after pediatric traffic injury. Pediatrics, 104, 1293–1299.
Doherty, N., McCusker, C. G., Molloy, B., Mulholland, C., Rooney, N., Craig, B., … Casey, F. (2009). Predictors of psychological functioning in mothers and fathers of infants born with severe congenital heart disease. Journal of Reproductive and Infant Psychology, 27, 390–400.
Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345.
Fedele, D. A., Hullmann, S. E., Chaffin, M., Kenner, C., Fisher, M. J., Kirk, K., … Mullins, L. L. (2013). Impact of a parent-based interdisciplinary intervention for mothers on adjustment in children newly diagnosed with cancer. Journal of Pediatric Psychology, 38, 531–540.
Green, J. L., Knight, S., McCarthy, M. C., & DeLuca, C. D. (2013). Motor functioning during and following chemotherapy treatment for pediatric acute lymphoblastic leukemia. Pediatric Blood & Cancer, 60, 1261–1266.
Hall, E., Saxe, G., Stoddard, F. J., Kaplow, J., Koenen, K., Chawla, N., … King, D. (2006). Posttraumatic Stress Symptoms in Parents of Children with Acute Burns. Journal of Pediatric Psychology, 31, 403–412.
* Holditch-Davis, D., Miles, M. S., Weaver, M. A., Black, B., Beeber, L., Thoyre, S., & Engelke, S. (2009). Patterns of distress in African-American mothers of preterm infants. Journal of Developmental and Behavioral Pediatrics, 30, 193–205. doi:10.1097/DBP.0b013e3181a7ee53.
Jackson, C., Cheater, F. M., & Reid, I. (2008). A systematic review of decision support needs of parents making child health decisions. Health Expectations, 11, 232–251.
Jones, S., Rantell, K., Stevens, K., Colwell, B., Ratcliffe, J. R., Holland, P., … Parry, G. J. (2006). Outcome at 6 months after admission for pediatric intensive care: A report of a national study of pediatric intensive care units in the United kingdom. Pediatrics, 118, 2101–2108.
* Kassam-Adams, N., Fleisher, C. L., & Winston, F. K. (2009). Acute stress disorder and posttraumatic stress disorder in parents of injured children. Journal of Traumatic Stress, 22, 294–302.
Kazak, A. E. (1994). Implications of survival: Pediatric oncology parents and their families. New York: Oxford University.
Kazak, A. E., Kassam-Adams, N., Schneider, S., Zelikovsky, N., Alderfer, M. A., & Rourke, M. (2006). An integrative model of pediatric medical traumatic stress. Journal of Pediatric Psychology, 31, 343–355.
* Kazak, A. E., Simms, S., Alderfer, M. A., Rourke, M. T., Crump, T. A., McClure, K. S., … Reilly, A. (2005). Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. Journal of Pediatric Psychology, 30, 644–655.
* Landolt, M. A., Boehler, U., Schwager, C., Schallberger, U., & Nuessli, R. (1998). Post-traumatic stress disorder in paediatric patients and their parents: An exploratory study. Journal of Paediatrics and Child Health, 34, 539–543.
* Landolt, M. A., Ribi, K., Laimbacher, J., Vollrath, M. E., Gnehm, H. E., & Sennhauser, F. H. (2002). Posttraumatic Stress Disorder in parents of children with newly diagnosed Type 1 diabetes. Journal of Pediatric Psychology, 27, 647–652.
* Landolt, M. A., Vollrath, M. E., Laimbacher, J., Gnehm, H. E., & Sennhauser, F. H. (2005a). Prospective study of posttraumatic stress disorder in parents of children with newly diagnosed type 1 diabetes. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 682–689.
* Landolt, M. A., Vollrath, M. E., Ribi, K., Gnehm, H. E., & Sennhauser, F. H. (2003). Incidence and associations of parental and child posttraumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry and Allied Disciplines, 44, 1199–1207.
* Landolt, M. A., Vollrath, M. E., Timm, K., Gnehm, H. E., & Sennhauser, F. H. (2005b). Predicting posttraumatic stress symptoms in children after road traffic accidents. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 1276–1283.
* Landolt, M. A., Ystrom, E., Sennhauser, F. H., Gnehm, H. E., & Vollrath, M. E. (2012). The mutual prospective influence of child and parental post-traumatic stress symptoms in pediatric patients. Journal of Child Psychology and Psychiatry, 53, 767–774.
* Lefkowitz, D. S., Baxt, C., & Evans, J. R. (2010). Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU). Journal of Clinical Psychology in Medical Settings, 17(3), 230–237.
* McCarthy, M. C., Ashley, D. M., Lee, K. J., & Anderson, V. (2012). Predictors of acute and posttraumatic stress symptoms in parents following their child’s cancer diagnosis. Journal of Traumatic Stress, 25, 558–566. doi:10.1002/jts.21745.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Medicine, 3, e123–e130.
* Nugent, N. R., Ostrowski, S., Christopher, N. C., & Delahanty, D. L. (2007). Parental posttraumatic stress symptoms as a moderator of child’s acute biological response and subsequent posttraumatic stress symptoms in pediatric injury patients. Journal of Pediatric Psychology, 32, 309–318.
Pai, A. L., Greenley, R. N., Lewandowski, A., Drotar, D., Youngstrom, E., & Peterson, C. C. (2007). A meta-analytic review of the influence of pediatric cancer on parent and family functioning. Journal of Family Psychology, 21, 407–415.
* Patino-Fernández, A. M., Pai, A. L., Alderfer, M., Hwang, W., Reilly, A., & Kazak, A. E. (2008). Acute stress in parents in children newly diagnosed with cancer. Pediatric Blood & Cancer, 50, 289–292.
* Pöder, U., Ljungman, G., & von Essen, L. (2008). Posttraumatic stress disorder among parents of children on cancer treatment: A longitudinal study. Psycho-Oncology, 17, 430–437.
* Ribi, K., Vollrath, M. E., Sennhauser, F. H., Gnehm, H. E., & Landolt, M. A. (2007). Prediction of posttraumatic stress in fathers of children with chronic diseases or unintentional injuries: A six-months follow-up study. Child and Adolescent Psychiatry and Mental Health, 1, 16–25.
Sahler, O. J. Z., Fairclough, D. L., Phipps, S., Mulhern, R. K., Dolgin, M. J., Noll, R. B., … Butler, R. W. (2005). Using problem-solving skills training to reduce negative affectivity in mothers of children with newly diagnosed cancer: report of a multisite randomized trial. Journal of Consulting And Clinical Psychology, 73, 272–283.
Sahler, O. J. Z., Varni, J. W., Fairclough, D. L., Butler, R. W., Noll, R. B., Dolgin, M. J., … Mulhern, R. K. (2002). Problem-solving skills training for mothers of children with newly diagnosed cancer: A randomized trial. Journal of Developmental & Behavioral Pediatrics, 23, 77–86.
Shaw, R. J., Bernard, R. S., Deblois, T., Ikuta, L. M., Ginzburg, K., & Koopman, C. (2009). The relationship between acute stress disorder and posttraumatic stress disorder in the neonatal intensive care unit. Psychosomatics, 50(2), 131–137.
* Shaw, R. J., Deblois, T., Ikuta, L., Ginzburg, K., Fleisher, B., & Koopman, C. (2006). Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics, 47, 206–212.
* Shears, D., Nadel, S., Gledhill, J., & Garralda, M. E. (2005). Short-term psychiatric adjustment of children and their parents following meningococcal disease. Pediatric Critical Care Medicine: A Journal Of The Society Of Critical Care Medicine And The World Federation Of Pediatric Intensive And Critical Care Societies, 6, 39–43.
* Stehl, M. L., Kazak, A. E., Alderfer, M. A., Rodriguez, A., Hwang, W., Pai, A. L., … Reilly, A. (2009). Conducting a randomized clinical trial of an psychological intervention for parents/caregivers of children with cancer shortly after diagnosis. Journal of Pediatric Psychology, 34, 803–816.
Stein, M., Walker, J., Hazen, A., & Forde, D. (1997). Full and partial posttraumatic stress disorder: Findings from a community survey. American Journal of Psychiatry, 154, 1114–1119.
Stuber, M. L., Meeske, K. A., Leisenring, W., Stratton, K., Zeltzer, L. K., Dawson, K., … Krull, K. R. (2011). Defining medical posttraumatic stress among young adult survivors in the Childhood Cancer Survivor Study. General Hospital Psychiatry, 33, 347–353.
Stuber, M. L., & Shemesh, E. (2006). Post-traumatic stress response to life-threatening illnesses in children and their parents. Child and Adolescent Psychiatric Clinics of North America, 15, 597–609.
* Sturms, L. M., van der Sluis, C. K., Stewart, R. E., Groothoff, J. W., ten Duis, J. H., & Eisma, W. H. (2005). A prospective study on paediatric traffic injuries: Health-related quality of life and post-traumatic stress. Clinical Rehabilitation, 19, 312–322.
Taïeb, O., Moro, M. R., Baubet, T., Revah-Lévy, A., & Flament, M. F. (2003). Posttraumatic stress symptoms after childhood cancer. European Child & Adolescent Psychiatry, 12(6), 255–264.
van Oers, H. A., Haverman, L., Limperg, P. F., van Dijk-Lokkart, E. M., Maurice-Stam, H., & Grootenhuis, M. A. (2014). Anxiety and depression in mothers and fathers of a chronically ill child. Maternal and Child Health Journal. doi:10.1007/s10995-014-1445-8.
* Vanderbilt, D., Bushley, T., Young, R., & Frank, D. A. (2009). Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: A preliminary study. Journal of Developmental and Behavioral Pediatrics, 30, 50–56.
Wakefield, C. E., McLoone, J. K., Butow, P., Lenthen, K., & Cohn, R. J. (2011). Parental adjustment to the completion of their child’s cancer treatment. Pediatric Blood & Cancer, 56, 524–531. doi:10.1002/pbc.22725.
* Winston, F. K., Kassam-Adams, N., Vivarelli-O’Neill, C., Ford, J., Newman, E., Baxt, C., … Cnaan, A. (2002). Acute stress disorder symptoms in children and their parents after pediatric traffic injury. Pediatrics, 109, e90.
Young, G. S., Mintzer, L. L., Seacord, D., Castañeda, M., Mesrkhani, V., & Stuber, M. L. (2003). Symptoms of posttraumatic stress disorder in parents of transplant recipients: incidence, severity, and related factors. Pediatrics, 111, e725–e731.
Acknowledgement
The research project reported in this published work was conducted by the authors as part of their Masters in Psychology at the University of Melbourne, or employment with the Murdoch Childrens Research Institute, or The Royal Children’s Hospital, Melbourne, Australia. We acknowledge the funding support for this project from the Pratt Foundation and the Victorian Government’s Operational Infrastructure Support Program. None of these funders had any involvement in the planning, design or execution of this research, and neither played a role in drafting the manuscript. The authors have full control of all primary data and agree to allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Claudia Woolf, Frank Muscara, Vicki Anderson and Maria McCarthy all declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation of (Royal Children’s Hospital, HREC 30044) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study. No animal or human studies were carried out by the authors for this article.
Rights and permissions
About this article
Cite this article
Woolf, C., Muscara, F., Anderson, V.A. et al. Early Traumatic Stress Responses in Parents Following a Serious Illness in Their Child: A Systematic Review. J Clin Psychol Med Settings 23, 53–66 (2016). https://doi.org/10.1007/s10880-015-9430-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-015-9430-y