Abstract
Simple and accurate expressions describing the PaO2–FiO2 relationship in mechanically ventilated patients are lacking. The current study aims to validate a novel mathematical expression for accurate prediction of the fraction of inspired oxygen that will result in a targeted arterial oxygen tension in non-smoking and smoking patients receiving mechanical ventilation following open heart surgeries. One hundred PaO2–FiO2 data pairs were obtained from 25 non-smoking patients mechanically ventilated following open heart surgeries. One data pair was collected at each of FiO2 of 40, 60, 80, and 100% while maintaining same mechanical ventilation support settings. Similarly, another 100 hundred PaO2–FiO2 data pairs were obtained from 25 smoking patients mechanically ventilated following open heart surgeries. The utility of the new mathematical expression in accurately describing the PaO2–FiO2 relationship in these patients was assessed by the regression and Bland–Altman analyses. Significant correlations were seen between the true and estimated FiO2 values in non-smoking (r2 = 0.9424; p < 0.05) and smoking (r2 = 0.9466; p < 0.05) patients. Tight biases between the true and estimated FiO2 values for non-smoking (3.1%) and smoking (4.1%) patients were observed. Also, significant correlations were seen between the true and estimated PaO2/FiO2 ratios in non-smoking (r2 = 0.9530; p < 0.05) and smoking (r2 = 0.9675; p < 0.05) patients. Tight biases between the true and estimated PaO2/FiO2 ratios for non-smoking (−18 mmHg) and smoking (−16 mmHg) patients were also observed. The new mathematical expression for the description of the PaO2–FiO2 relationship is valid and accurate in non-smoking and smoking patients who are receiving mechanical ventilation for post cardiac surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The ability to accurately predict the arterial partial pressure of oxygen (PaO2) after changing the inspired oxygen fraction (FiO2) is an important clinical tool that can allow clinicians to decrease the need for arterial punctures and/or arterial blood gas (ABG) sampling. More importantly it allows trending the changes in the PaO2/FiO2 ratio, an essential indicator used for quantifying the degree of lung injury and subsequently optimize the management of patients receiving mechanical ventilation [1].
Several theoretical models have been proposed for predicting the response of PaO2 to changes in FiO2 [2–4]; however almost none of these predicting models have been widely accepted and implemented in clinical use. There are at least two reasons for this lack of utilization. First, the complex nature of the derived models as well as the technical difficulties involved (e.g., use of the virtual shunt lines) and the need to determine cumbersome variables such as alveolar gas tensions and respiratory quotients make them somewhat impractical at the bedside and second, the lack of reliability and accuracy of some of these models, particularly when underlying assumptions are not fulfilled [5].
Recently, Hardman and Al-Otaibi developed and validated a novel formula for prediction of PaO2 in mechanically ventilated patients [6, 7]. Their predictive equation for PaO2 has the advantage of including simple and straightforward variables such as old and new PaO2 and FiO2 values that are easily determined and readily available at the bedside. However, their new equation falls short of providing a more clinically relevant form of the relationship between PaO2 and FiO2. Their method predicts the new PaO2 following a step change in FiO2. In contrast, we believe that predicting the new FiO2 that will achieve a targeted or desired PaO2 is more relevant, appropriate, and useful for clinicians in managing oxygenation and FiO2 requirements in mechanically ventilated patients. Furthermore, Al-Otaibi and Hardman validated their formula in a group of ICU patients who were receiving different modes of ventilatory supports (e.g., volume controlled, pressure controlled and pressure support ventilation) that can have different and significant effects on ventilation/perfusion matching, cardiac output, and venous oxygen saturation (SvO2), and ultimately on the validity of their results. Also Al-Otaibi and Hardman used only a narrow range of FiO2 settings (i.e., 40–60%).
Therefore, we derived a new equation that will allow the clinician to predict the required FiO2 to achieve a desired or targeted PaO2 (El-Khatib-Chatburn equation) [8]. The new equation uses known values of FiO2 and PaO2 (i.e., oldFiO2 and oldPaO2) as well as the physician’s desired or target values for PaO2 (i.e., newPaO2) to predict the required value of FiO2 (i.e., newFiO2) to achieve the target PaO2:
where k = (2 − oldFiO2)2 + (8 × newPaO2 × oldFiO2)/(oldPaO2).
The aim of the current study was to confirm the clinical validation of the relationship between FiO2 and PaO2 in the context of using the El-Khatib-Chatburn equation for the accurate prediction of the fraction of inspired oxygen that will result in a targeted arterial oxygen tension in smoking and non-smoking patients receiving mechanical ventilation following open heart surgeries.
2 Methods
This study was approved by the Institutional Review Board at the American University of Beirut School of Medicine and Medical Center. All patients provided written informed consent prior to participation in the study.
Patients who were older than 18 years and scheduled to undergo open heart surgeries, who were not morbidly obese (Body Mass Index <35 kg/m2) and were not known to have interstitial lung diseases, pulmonary vascular diseases, hematologic malignancies, hemodynamic shocks, or pneumonia were included in the study. Exclusion criteria included patients who were hemodynamically and/or clinically unstable, significantly anemic (hemoglobin less than 8 g/dL1), or patients who required positive end expiratory pressure (PEEP) greater than 5 cmH2O during mechanical ventilatory support in the post-operative period. Patients were assigned to one of two groups based on whether they have smoking history (≥10 pack-year) or no smoking history (<10 pack-year).
Upon arrival to the Cardiac Surgery Unit (CSU), patients were started and maintained on standard monitoring with continuous electrocardiography, invasive and noninvasive blood pressure, and pulse oximetry throughout the study. All patients had an indwelling arterial line as per routine clinical management and monitoring. In the CSU, patients were allowed an initial 20 min period of stabilization on mechanical ventilation with a FiO2 of 100% prior to initiation of the study protocol and data collection.
After the initial stabilization period on FiO2 of 100%, an arterial blood sample was obtained for blood gas analysis and determination of PaO2. Subsequently the patient’s FiO2 was changed from 100 to 80, 60, and 40% in random order while all other mechanical respiratory support parameters were kept the same and while ensuring that the patient was well sedated with no spontaneous minute ventilation. The PaO2 values that resulted from the changes in FiO2 were considered the “new” PaO2 for purposes of using the prediction equation. The values of old FiO2, old PaO2, (that could be any previously determined FiO2 and PaO2 values) and new PaO2 were substituted into Eq. 1 and the equation was solved for new FiO2 (i.e., in clinical practice, the new FiO2 is what would have been predicted as the new therapeutic target if the new PaO2 had been the desired outcome target). Demographic and hemodynamic data as well as ventilatory support variables were obtained for all patients.
The medical team in charge of the patients had the option to terminate the study at any point in time if it was felt that a change in FiO2 was compromising the patient’s clinical condition. Arterial blood samples were collected after 20 min of stabilization on each FiO2 value. The arterial blood samples were collected via the indwelling arterial line following standard procedures using the same brand and model of arterial blood gas samplers (Marquest Quick A.B.G, GE Healthcare, USA). All arterial blood samples were immediately subjected to duplicate blood gas analysis measurements in two separate and calibrated blood gas machines (ABL-820 and ABL-720, Radiometer, Copenhagen) for the determination of PaO2 and for ensuring accuracy of PaO2 measurements. The average PaO2 values of the two samples from the two blood gas machines were used for data analysis.
2.1 Statistical analysis
A power analysis considering a type I error of 5%, a type II error of 20% (i.e., power is 80%) and an expected and significant correlation coefficient between true and estimated FiO2 of 0.55 indicates that at least 24 patients were needed [9]. Data was tested for normal distribution using the Chi squared goodness of fit test. The Bland–Altman analysis was used to determine the degree of bias and reliability between the true and estimated values of FiO2 and PaO2/FiO2 ratio for patients with and without smoking history [10]. Also standard techniques of linear regression and correlation by the least square method were used to assess the degree of correlation between new “estimated” FiO2 and true FiO2 values in the two patients’ groups. Paired t test was used to test the statistical significance of the differences between the estimated and true FiO2 values. Student t test and Chi square test were used for statistical analysis of the patients’ characteristics. Statistical significance was considered at the 5% level (i.e., p < 0.05).
3 Results
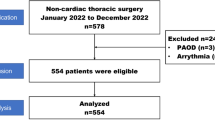
Overall, 50 patients were included in the study. Twenty five patients had a smoking history and 25 patients had no significant smoking history. Patients’ characteristics are presented in Table 1. There were no statistically significant differences in hemodynamic parameters throughout the study in both non-smoking and smoking patients (Table 2). The comparison of arterial blood gas values at different levels of FiO2s revealed significant differences only in PaO2 as a result of changing the FiO2 levels for both non-smoking (Table 3) and smoking patients (Table 4).
A total of one hundred PaO2–FiO2 data pairs corresponding to four levels of FiO2 per patient were obtained from the 25 patients with no smoking history. Similarly, another set of 100 PaO2–FiO2 data pairs were obtained from the 25 patients with smoking history. There were strong and significant correlations between the true and estimated FiO2 values in non-smokers (r2 = 0.9424; p < 0.05) (Fig. 1) with a 95% confidence interval for the estimated FiO2 of 7.94% as well as in smokers (r2 = 0.9466; p < 0.05) (Fig. 2) (95% CI for the estimated FiO2 = 7.79%). Furthermore, the 95% confidence intervals for the differences between the estimated and true FiO2 (i.e., estimated-true FiO2) were 1.92% and 1.81% in non-smokers and smokers respectively. Similarly strong and significant correlations were observed between the true and estimated PaO2/FiO2 ratios in non-smokers (r2 = 0.9530; p < 0.05) as well as in smokers (r2 = 0.9675; p < 0.05).
The Bland–Altman analyses revealed strong agreements with tight biases between the true and estimated FiO2 values in non-smoking patients (bias: 3.1%; limit of agreement range: −4.7%–10.9%) (Fig. 3) as well as in smoking patients (bias of 4.1%; limit of agreement range: −4.6%–12.8%) (Fig. 4). The differences between the estimated and true FiO2 values in both non-smoking and smoking patients were not statistically significant. Moreover, strong agreements and tight biases were observed between the true and estimated PaO2/FiO2 ratios in non-smokers (bias: −18 mmHg; limit of agreement range: −57 mmHg–21 mmHg) (Fig. 5) as well as in smokers (bias: −16 mmHg; limit of agreement range: −51 mmHg–20 mmHg) (Fig. 6).
4 Discussion
The findings of the current study indicate that El-Khatib-Chatburn formula possesses sufficient accuracy and consistency to predict the fraction of inspired oxygen that will result in a targeted arterial oxygen tension as well as the PaO2/FiO2 ratios in non-smoking and smoking patients receiving mechanical ventilation following open heart surgeries.
As early as 1973, Benatar et al. [11] developed the iso-shunt diagrams based on a series of 44 arterial blood gas measurements obtained from 4 patients in an attempt to understand and quantify the relationship between FiO2 and PaO2. Despite being cumbersome and complicated, the iso-shunts have been considered to date the gold standard for the understanding and quantification of the PaO2–FiO2 relationship. However, several studies have attempted to express PaO2–FiO2 relationship in a more simplified and easy to use mathematical expression [2, 3, 12]. Most of the derived relationships are complicated, cumbersome and even limited in accuracy [5]. It was not until recently that Al-Otaibi and Hardman developed a simple, easy, and straightforward mathematical expression for predicting the new PaO2 following a step change in FiO2 [6, 7]. With Al-Otaibi and Hardman mathematical expression, all what is needed for the accurate prediction of PaO2 is the applied change in FiO2 and one previous and known combination of PaO2–FiO2 values. The mathematical expression for the PaO2–FiO2 relationship validated in the current study differs from Al-Otaibi and Hardman mathematical expression in the sense that ours is presented to predict the required FiO2 to achieve or target a desired PaO2 value. So rather than predicting what the new PaO2 would be following a step change in FiO2, predicting the new FiO2 that will achieve a targeted or desired PaO2 and PaO2/FiO2 ratio is more appropriate and more useful for clinicians in managing oxygenation and FiO2 requirements in critically ill and mechanically ventilated patients. As such, our mathematical expression can provide a clinically more relevant form of the relationship between PaO2 and FiO2.
The patients’ disease mix in Al-Otaibi and Hardman’s study is different than the patients mix in the current study [5, 6]. Eighty-one (68%) patients in Al-Otaibi and Hardman were post-cardiac surgery and the remaining 32% were patients with active lung diseases (e.g., acute respiratory failure, ARDS, pneumonia) as opposed to the patients in the current study who were all (100%) post-cardiac surgery patients. As such, mixing patients with active and non-active lung diseases might not be optimal for validation of PaO2–FiO2 relationship due the potential effects of existing V/Q mismatches and hemodynamic status and subsequently the existence of such physiological conditions on the response to changes in FiO2. Also, Al-Otaibi and Hardman did not stratify their patients by smoking history. Our data shows that smoking history might not be a significant factor in the relationship between PaO2 and FiO2 particularly when patients are not in any active lung disease. In the current study, significant levels of correlation and agreements were observed between true and estimated FiO2 as well as between true and estimated PaO2/FiO2 ratios in both non-smoking and smoking patients clinically cleared to undergo open heart surgeries.
Al-Otaibi and Hardman did not consider the effects of multiple changes in FiO2 values in the same patient [6, 7]. Furthermore, the range of changes in FiO2 value in their study was a very narrow range from 48 to 60% [7]. In their validation, they did not include values of PaO2 from the same patient but different PaO2 values corresponding to multiple and different FiO2 values from different patients. Two patients could have very different V/Q distribution, cardiac output, and shunt yet have the same PaO2 at the same FiO2. But when FiO2 is changed by the same amount in the two patients, their PaO2 would not necessarily change by the same amount. The more shunt and the less V/Q inequality there is, the less will PaO2 increase for a given increase in FiO2. This concern was considered and avoided in the current study during which several changes in FiO2 that cover the whole clinical range of FiO2 were applied in the same patient (40, 60, 80, and 100%).
Patients in the Al-Otaibi and Hardman’s study were receiving a variety of ventilatory support modes including volume-controlled, pressure-controlled, and pressure-support ventilation with some of their patients exhibiting spontaneous breathing activities during their mechanical ventilatory support [7]. This could have significantly affected the V/Q mismatch and cardiac output and subsequently the response of PaO2 to changes in FiO2. In contrast, in the current study patients were fully sedated with no spontaneous breathing activity and were receiving the same mode and settings for mechanical ventilation throughout the experimental protocol. Such experimental design where only FiO2 is changed will allow for more accurate estimation of the PaO2–FiO2 relationship and allows for better validation of the mathematical expression. Also, it is unlikely that our patients had clinically significant V/Q mismatches; otherwise, sudden and significant drops in oxygenation would have occurred below a certain FiO2 level. In such events, an exponential interpolation of the PaO2–FiO2 relation would have been more appropriate.
Our data show that our modified equation resulted in 95% confidence intervals for the differences between estimated and true FiO2 values that are less than 2% for both patients who are non-smokers and smokers. From a clinical perspective, this is clearly a narrow 95% confidence interval for the differences between estimated and true FiO2. Also, our results show that there is a non-statistically significant tendency for overestimating rather than underestimating FiO2. Clinically speaking, this can provide some level of safety margin as it is almost always better to overestimate FiO2 rather than underestimate FiO2 and expose the patients to risks of hypoxia.
In our study, periods of 20 min of stabilization were allowed following each step change in FiO2 before any data collection. This was essential to allow for adequate equilibration of PaO2 to occur after FiO2 changes [13].
Several issues should be considered prior to generalization the findings of the current study. First, the modified formula for the prediction of FiO2 was tested in two cohort groups of patients with no active lung diseases and receiving mechanical ventilation for post cardiac surgery management. Also all our patients were clinically and hemodynamically stable. As such, patients with significant lung diseases and/or patients with unstable pathophysiological states may not reproduce similar findings. As such, other patient populations (e.g. asthmatics) might need to be treated using an equation with different parameter values than those used in the current equation. Patients who are receiving PEEP levels greater than 5cmH2O and/or are actively breathing during the mechanical ventilatory support might also be treated using an equation with different parameters than those used in the current equation.
Our method is equally good at predicting new FiO2 values for large and smaller magnitudes of FiO2 changes. The Box and Whisker plot for the differences between the estimated and true FiO2 values for the three possible magnitude of changes in FiO2 (i.e., 20%, 40%, and 60%) shows comparable medians and interquartiles (Fig. 7). Furthermore, the modified equation for the prediction of FiO2 validated in this study is simple and straightforward and can be solved using widely available hand held calculators and applications for calculators on smart phones. By using this equation in daily practice at the bedside, clinicians may be able to minimize their dependence on arterial blood gas samplings for the management of oxygenation and oxygen requirements of open heart patients receiving mechanical ventilation in the post-operative period. Valuable resources and time spent on arterial punctures, arterial cannulations, as well as collecting, transporting, and analyzing arterial blood samples might be saved with the use of such formula that can ultimately lead to more clinical efficiency and reduction of health care costs. Future studies will be needed to confirm these postulations.
In conclusion, our results confirm the utility of a new and simple predictive formula for management of oxygenation in mechanically ventilated patients following open heart surgeries.
References
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Hess D. Predicition of the change in PaO2. Crit Care Med. 1979;7:568–9.
Abizanda R, Lopez J. The Possibility of predicting PaO2 following changes in FiO2. Intensive Care Med. 1981;7:247.
Ogawa S, Kusunoki M, Shirai J, Takeda K, Takezawa J, Taenaka N, Matsumoto M, Kamada T. Prediction of arterial oxygen partial pressure from intrapulmonary venous admixture. Crit Care Med. 1989;17:1191–3.
Bigeleisen PE. Models of venous admixture. Adv Physiol Educ. 2001;25:159–66.
Hardman G, Al-Otaibi M. Prediction of arterial oxygen tension: validation of a novel formula. AJRCCM. 2010;182:435–6.
Al-Otaibi H, Hardman G. Prediction of arterial oxygen partial pressure after changes in FIO2: validation and clinical application of a novel formula. Br J Anaesth. 2011;107:806–12.
El-Khatib MF, Chatburn RL. Prediction of fraction of inspired oxygen to achieve a desired arterial partial pressure of oxygen. AJRCCM. 2012;185:685–6.
Hulley SB, Cummings SR, Browner WS, Grady D, Newman TB (2013) Designing clinical research: an epidemiologic approach. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013. Appendix 6C, p. 79.
Bland J, Altman D. Measuring agreement in method comparison studies. Stat Methods Med. 1999;8(2):135–60.
Benatar SR, Hewlett AM, Nunn JF. The use of iso-shunt lines for control of oxygen therapy. Br J Anaesth. 1973;45:711–8.
Maxwell C, Hess D, Shefet D. Use of the arterial/alveolar oxygen tension ratio to predict the inspired oxygen concentration needed for a desired arterial oxygen tension. Respir Care. 1984;29:1135–9.
Fildissis G, Katostaras T, Moles A, Katsaros A, Myrianthefs P, Brokalaki H, Tsoumakas K, Baltopoulos G. Oxygenation equilibration time after alteration of inspired oxygen in critically ill patients. Heart Lung. 2010;39:147–52.
Acknowledgments
The authors thank Dr. Rani Abou-Khouzam, Dr. Sana Chalhoub, and Dr. Hicham Bou-Fakhreddine for their help in this study.
Funding
Only departmental funds were used for this study. No external funds were obtained.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no competing interests.
Human and animal participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Pierre Bou-Khalil and Salah Zeineldine have equally contributed to this manuscript.
Rights and permissions
About this article
Cite this article
Bou-Khalil, P., Zeineldine, S., Chatburn, R. et al. Prediction of inspired oxygen fraction for targeted arterial oxygen tension following open heart surgery in non-smoking and smoking patients. J Clin Monit Comput 31, 999–1008 (2017). https://doi.org/10.1007/s10877-016-9941-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9941-6