Abstract
Respiratory variations in the photoplethysmographic waveform amplitude predict fluid responsiveness under certain conditions. Processing of the photoplethysmographic signal may vary between different devices, and may affect respiratory amplitude variations calculated by the standard formula. The aim of the present analysis was to explore agreement between respiratory amplitude variations calculated using photoplethysmographic waveforms available from two different pulse oximeters. Analysis of registrations before and after fluid loads performed before and after open-heart surgery (aortic valve replacement and/or coronary artery bypass grafting) with patients on controlled mechanical ventilation. Photoplethysmographic (Nellcor and Masimo pulse oximeters) and arterial pressure waveforms were recorded. Amplitude variations induced by ventilation were calculated and averaged over ten respiratory cycles. Agreements for absolute values are presented in scatterplots (with least median square regression through the origin, LMSO) and Bland–Altman plots. Agreement for trending presented in a four-quadrant plot. Agreement between respiratory photoplethysmographic amplitude variations from the two pulse oximeters was poor with LMSO ΔPOPNellc = 1.5 × ΔPOPMas and bias ± limits of agreement 7.4 ± 23 %. Concordance rate with a fluid load was 91 %. Agreement between respiratory variations in the photoplethysmographic waveform amplitude calculated from the available signals output by two different pulse oximeters was poor, both evaluated by LMSO and Bland–Altman plot. Respiratory amplitude variations from the available signals output by these two pulse oximeters are not interchangeable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Dynamic variables predict fluid responsiveness in mechanically ventilated patients [1]. Many patients are not equipped with arterial catheters necessary to calculate pulse pressure variations (ΔPP) [2]. Respiratory variations in the photoplethysmographic waveform amplitude have been explored as a non-invasive alternative [3] and recommended for clinical use [4].
The photoplethysmographic waveform represents variations in the amount of infrared light detected after being transmitted through tissue [5], predominantly due to variations of blood volume [6, 7]. Respiratory variations in the photoplethysmographic waveform amplitude (ΔPOP) are calculated as the difference between the maximal and minimal amplitudes (trough to peak) divided by their mean, expressed as a percentage. Both for ΔPP and ΔPOP, it is assumed that variations in the waveform amplitude through a respiratory cycle reflect variations in left ventricular stroke volume (SV). The photoplethysmographic waveform is however a complex signal which may, depending on the measurement site, also reflect other phenomena such as sympathetic nervous activity and venous blood volume [8–10].
Different groups using different pulse oximeters have studied ΔPOP. When calculating ΔPOP, one needs to have access to the photoplethysmographic waveform, and typically, auto-centering and auto-scaling functions (which otherwise makes it look tidy on the monitor) are disabled. However, signals are still processed by the devices before output from the pulse oximeter. It has not been thoroughly studied if this processing affects calculation of ΔPOP.
Pleth variability index (PVI) is a commercially available variable given by the Masimo Radical 7 pulse oximeter [11] and calculated as the difference between the maximal and minimal perfusion index (PI)-values within at least one respiratory cycle divided by the maximal PI-value. PI is the fraction of the pulsatile compared to the non-pulsatile infrared signal [11]. The calculation of PVI thus differs slightly from that of ΔPOP. In a systematic review and meta-analysis, Sandroni et al. [12] concluded that ΔPOP and PVI were equally effective to predict fluid responsiveness in ventilated adult patients in sinus rhythm. The authors suggested that the main limitation was the volume of the fluid bolus, although influence of different pulse oximetry technologies was discussed. A possible influence of different pulse oximeters on calculation of ΔPOP has not been extensively studied [13].
In a study on fluid responsiveness in cardiac surgery patients [14], photoplethysmographic waveforms were sampled from two different commercially available pulse oximeters (Nellcor and Masimo). The aim of the present analysis was to explore the agreement between ΔPOP from these two devices (ΔPOPNellc and ΔPOPMas, respectively) for absolute values and when trending a fluid load. PVI was also recorded. Furthermore, photoplethysmographic variables were compared to ΔPP.
2 Materials and methods
2.1 Patients
Data were collected in a study on fluid responsiveness in aortic stenosis (AS) patients [14]. Approval was given by the regional ethics committee (Regional Ethical Committee Sør-Øst C, Pb 1130 Blindern, 0318 Oslo, Norway; reference 2010/1629). After written informed consent, 43 patients were included; 32 scheduled for aortic valve replacement due to AS [with or without concomitant coronary artery bypass grafting (CABG)] and 11 patients scheduled for CABG only. Patients were >18 years, had sinus rhythm at inclusion, left ventricular ejection fraction >40 % and no suspected right heart failure.
2.2 Study protocol
Patients were premedicated with morphine/scopolamine. After induction of general anesthesia with diazepam, fentanyl and propofol, patients were mechanically ventilated in a volume-controlled mode, and anesthesia maintained with sevoflurane 1–1.5 %. Before surgery, patients were placed in the horizontal position, and a fluid load performed by rapid infusion of 750 ml acetated Ringer’s solution via a peripheral vein. Registrations were obtained before and after the fluid load, and completed before surgery was commenced.
After surgery, patients were taken to the intensive care unit (ICU) and mechanically ventilated in a pressure-controlled mode. Registrations were obtained before and after fluid loads, which were performed with a smaller volume than the preoperative load (500 ml acetated Ringer’s solution, 250 ml hydroxyl ethyl starch 130/0.4, 250 ml packed red blood cells or 250 ml plasma). Registrations were obtained if patients were on no or stable infusions of sedative and vasoactive drugs.
2.3 Signal acquisition and analysis
In the operating room (OR), a 5-lead ECG was attached and a 20G catheter placed in the left radial artery. Finger probes (DS-100A; Nellcor, Boulder, CO, USA) from a Nellcor pulse oximeter (Nellcor OxiMax/Tram451N; General Electric Healthcare, Milwaukee, WI, USA) and Masimo Radical 7, software 7.3.1.1 with a LNOP DC-I probe (Masimo Corp., Irvine, CA, USA) were placed on the right 2 and 3 fingers and covered from ambient light. Photoplethysmographic waveform from the Nellcor pulse oximeter and arterial pressure waveform were extracted from the analog output of a TramRac4A (General Electric Healthcare). Photoplethysmographic waveform from the Radical 7 was extracted by its analog output. Waveforms were sampled via a NIDAQPad-6015 analog–digital converter (National Instruments, Austin, TX, USA) at 400 Hz and stored on a laptop computer. ΔPOP and ΔPP were calculated in a custom made program in LabVIEW (National Instruments), where each respiratory cycle (determined by the thoracic impedance from the ECG-leads), was manually delimitated and the maximal and minimal amplitudes of the waveforms verified before calculating ΔPOP and ΔPP. ΔPOP and ΔPP were calculated as follows:
POPmax and PPmax are maximal and POPmin and PPmin minimal amplitudes of the photoplethysmographic and arterial pressure waveforms within one respiratory cycle, respectively.
SV was measured by an oesophageal Doppler (DP-12 probe; CardioQ; Deltex Medical, Chichester, UK). An increase in SV >15 % with the fluid load defined a responder. Data were downloaded beat-by-beat from the serial output of the oesophageal Doppler monitor. PVI was downloaded at 0.5 Hz by the TrendCom software (Masimo). Other hemodynamic data were downloaded at 1 Hz from a Solar 8500 or 9000 (General Electric Healthcare), using custom made software in LabVIEW (National Instuments).
ΔPOP and ΔPP-values were averaged over 10 respiratory cycles (≈1 min). Respiratory cycles with extrasystoles or obvious disturbances were omitted. SV, PVI and other hemodynamic data were averaged over 1 min. Registrations were made before and after the fluid loads, giving two observations per fluid load.
2.4 Statistics
Bland–Altman calculations were performed in MedCalc Statistical Software version 13.0.6 (MedCalc Software bvba, Ostend, Belgium) with multiple measurements per subject [15]. Bias values in Bland–Altman plots were compared by unpaired t tests, unequal variances assumed. Limits of agreement compared by F tests. Trending abilities are presented using a four-quadrant plot where the concordance rate represents the fraction of observations (outside a central exclusion zone) in the upper right and lower left quadrants. Cutoff for trending fluid responsiveness for ΔPP has been estimated to approximately 3 % [16]. We are not aware of corresponding data for ΔPOP, but arbitrarily set the central exclusion zone to 5 %. Abilities to predict fluid responsiveness are presented as areas under receiver operating characteristics curves (AUCROC) with 95 % exact binomial confidence intervals. Least median squares regressions through the origin (LMSO) [17] were performed in the MASS package in R 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria). As data were sampled in another study, separate sample size-calculations were not performed for the analyses in the present manuscript.
3 Results
One patient in the AS group was excluded due to arterial waveform dampening and in four patients, analog data were lost, giving 38 patients for analysis (27 in the AS group and 11 in the CABG-group). In one CABG-patient, analog data before the preoperative fluid load were lost. In one AS patient, the Masimo pulse oximeter (ΔPOPMas and PVI) did not function during a postoperative fluid load. One AS-patient had frequent extrasystoles before surgery, and was only studied postoperatively. One preoperative fluid load was performed in each patient (26 in AS-patients and 11 in CABG-patients). Postoperatively, 27 fluid loads were performed in 19 AS patients, and three fluid loads were performed in three CABG-patients. Patient characteristics are presented in Table 1, hemodynamic data in Table 2.
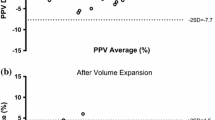
Scatterplots with LMSO are presented in Fig. 1. Results from Bland–Altman plots are presented in Fig. 2 and Table 3. There were wide limits of agreement between ΔPOPNellc and ΔPOPMas with bias ± LOA 7.4 ± 23 % and a percentage error of 164 %. Results from AS-patients and CABG-patients are also presented separately (Table 3).
Scatterplots with lines of identity (y = x) dashed, and least mean squares regression lines through the origin (LMSO) solid. Regression coefficient is for LMSO slope. Black dots are from coronary artery bypass grafting patients, circles are from aortic stenosis patients. ΔPOP Nellc respiratory photoplethysmographic waveform amplitude variations by Nellcor pulse oximeter, ΔPOP Mas respiratory photoplethysmographic waveform amplitude variations by Masimo pulse oximeter, PVI pleth variability index, ΔPP pulse pressure variation
Bland–Altman plots. Solid lines are bias and dashed lines are limits of agreement. Black dots are from coronary artery bypass grafting patients, circles are from aortic stenosis patients. ΔPOP Nellc respiratory photoplethysmographic waveform amplitude variations by Nellcor pulse oximeter, ΔPOP Mas respiratory photoplethysmographic waveform amplitude variations by Masimo pulse oximeter, PVI pleth variability index, ΔPP pulse pressure variation
The agreement between ΔPP and the photoplethysmographic variables (ΔPOPNellc, ΔPOPMas and PVI) was calculated and compared. The bias was higher (unpaired t tests, unequal variances assumed, both p < 0.001) and limits of agreement were wider (F tests, both p < 0.001) for ΔPP versus ΔPOPNellc than for both ΔPP versus PVI and ΔPP versus ΔPOPMas.
Assessment of trending with fluid loads is presented in Fig. 3. Concordance rate was 91 %. The abilities to predict fluid responsiveness are presented in Table 4.
Four quadrant scatterplot displaying the agreement between ΔPOPMas and ΔPOPNellc when trending a fluid load. A 5 % exclusion zone has been used in the calculations. Observations within the exclusion zone (marked as grey circles) are not used for calculations of concordance rate. ΔPOP Mas respiratory photoplethysmographic waveform amplitude variations by Masimo pulse oximeter, ΔPOP Nellc respiratory photoplethysmographic waveform amplitude variations by Nellcor pulse oximeter
4 Discussion
The main finding of this analysis was the poor agreement between ΔPOP calculated from two different commercially available pulse oximeters both judged by LMSO and Bland–Altman plots. ΔPOPMas agreed better than ΔPOPNellc with ΔPP. The results indicate that the photoplethysmographic waveform from the two pulse oximeters cannot be used interchangeably to calculate ΔPOP.
ΔPOP has been explored as a non-invasive alternative to ΔPP or SV variation [3, 13]. The photoplethysmographic waveform is however influenced by other phenomena than respiratory variations in SV [6, 10, 18, 19]. The photoplethysmographic signal presented on the monitor screen as well as the signals extracted from analog outputs are highly processed, e.g. by bandpass filtering, auto-centering and amplitude adjustment [20]. As stated by Feldman [21], signal processing in commercial, proprietary algorithms complicates the use of these devices in research. From a clinical point of view, all the devices (and software versions) may need to be validated for relevant end points before clinical implementation. From a research point of view, the proprietary signal processing complicates physiological interpretation.
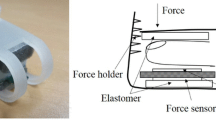
Processing of photoplethysmographic signals probably vary between the two measuring devices (an example presented in Fig. 4). Baseline variations with the respiration seem to be more pronounced in the signal from the Nellcor device, compared to the Masimo device, affecting calculation of ΔPOP. The Masimo Radical 7 pulse oximeter also calculates PVI, specifically intended to reflect respiratory SV variations. The photoplethysmographic signal may have been processed to reduce the influence of other phenomena, making this particular device especially prone to give different results compared to other pulse oximeters. As baseline modulations synchronous with respiration seemed to be more pronounced in the Nellcor photoplethysmographic signal, this signal was also analyzed after filtering with a 3rd order Butterworth highpass filter with 0.4 Hz cutoff. This did however not substantially improve the agreement with ΔPP (LMSO slope 1.4, Bland–Altman bias ± LOA 9.2 ± 19 %). Which signal processing is the best when using the photoplethysmographic signal to predict fluid responsiveness is beyond the scope of this article, but both amplitude modulations with each heartbeat as well as baseline modulations with respiration might be related to volume status [22]. Whether the complexity of the photoplethysmographic signal represents a limitation or an opportunity is discussed [7, 23]. The signal can be decomposed into frequencies representing the cardiac and respiratory cycles, respectively [7]. A respiratory-synchronous component can represent variations of blood volume in the venous compartment [10, 24]. If variations in SV are represented by variations in the cardiac-synchronous component, the venous component may pose a problem when using the ordinary formula to calculate ΔPOP. As some time passes from the trough to the peak in each cardiac cycle, variations in the respiratory component will cause the calculated amplitude to change, even though there is no variation in the cardiac component. This possible effect has been illustrated in a simple simulation using sine waves in Fig. 5.
Example of synchronously recorded waveforms with maximal and minimal amplitudes within one respiratory cycle marked. ΔPP pulse pressure variation, ΔPOP Nellc respiratory photoplethysmographic waveform amplitude variations by Nellcor pulse oximeter, ΔPOP Mas respiratory photoplethysmographic waveform amplitude variations by Masimo pulse oximeter
Simulations illustrating the potential effect of the respiratory oscillation on ΔPOP. Sin(x) represents cardiac oscillations, sin(0.2x) represents respiratory oscillations, whereas sin(x) + sin(0.2x) represents the photoplethysmographic signal. Although there are no variations in the cardiac component, the respiratory component will influence the calculations of ΔPOP due to the lag between the trough and the peak. A smaller respiratory component [0.5sin(0.2x)] attenuates this effect, giving smaller calculated ΔPOP-values
ΔPOP and PVI have been recommended to predict fluid responsiveness [4]. The meta-analysis by Sandroni et al. [12] indicated that ΔPOP and PVI accurately predict fluid responsiveness when the fluid load is 500 ml, but less accurate for 250 ml. Of note, the studies using 250 ml in the meta-analysis [12] were performed during ongoing surgery, whereas the studies using 500 ml were performed in the ICU or in the operating room immediately after the induction of anesthesia or after surgery. Study heterogeneity was not significant after stratifying the studies according to fluid load volume. However, variations in filtering techniques in different devices could have influenced the results [12]. The present analysis shows that different devices may produce different values of ΔPOP and that ΔPOPMas and PVI agreed better than ΔPOPNellc with ΔPP.
In previous studies, our group has used both Nellcor [19, 25] and Masimo [26] pulse oximeters to calculate ΔPOP. A Nellcor pulse oximeter was used when we found larger values and larger variability for ΔPOP than for ΔPP in a study on ICU patients [19]. However, both by using Nellcor and Masimo pulse oximeters, we have found moderate or poor abilities to predict fluid responsiveness during ongoing abdominal surgery [25, 26]. Although the agreement between the ΔPOP-values was poor, their abilities to predict fluid responsiveness as judged by the AUCROC-values were quite similar.
4.1 Methodological considerations
The agreement between the waveforms could potentially be different in the two patient groups (AS and CABG-patients), influencing the results. The bias and limits of agreement were therefore also calculated separately and compared for AS and CABG patients (Table 3). The only statistically significant difference was between the LOAs of ΔPOPMas and ΔPP, influenced by outliers (Fig. 2). The overall results do therefore not seem to be specific for one patient group.
The present study was not powered to demonstrate a clinically relevant difference in the ability to predict fluid responsiveness. Fluid loads pre- and postoperatively were aggregated for CABG-patients, as there were few postoperative fluid loads and dynamic variables have been demonstrated to predict fluid responsiveness well both pre-and postoperatively in this patient group [1]. For AS-patients, we calculated separate AUCROC for pre- and postoperative fluid loads, as ΔPP only demonstrated a moderate predictive ability preoperatively [14]. ΔPP had a higher AUCROC than PVI for AS patients after surgery. Otherwise, we did not demonstrate statistically significant differences in the abilities to predict fluid responsiveness for any of the variables.
For observations symmetrically distributed about the line y = x, the slope of ordinary least squares regression lines tends to deviate from 1 (y = x, line of identity) towards 0 as correlation between x and y decreases from 1 towards 0. This severely limits its use in method comparison. We are not aware of data describing the degree to which the LMSO also has this propensity.
The Bland–Altman plots were adjusted for dependence between repeated measurements within patients. T tests and F tests used when comparing bias and limits of agreement between subgroups of patients assume independent data, which repeated data (e.g. before and after a fluid load) are not. However, analyzing only measurements made before fluid loads (one observation per fluid load) gave similar results (data not shown). Postoperatively in AS-patients, some patients had repeated fluid loads, violating the assumption of independent observations in the AUCROC-calculations. However, analyzing only the first fluid load in each patient gave similar results (data not shown).
ΔPP, ΔPOPNellc and ΔPOPMas were calculated over ten respiratory cycles, starting synchronized with the 1 min averaging period of SV. PVI as calculated and displayed by the Masimo Radical 7 pulse oximeter was also averaged over this 1 min period. This PVI-value displayed by the device is however processed and averaged over some min, implying that the PVI-values to some extent lag behind the other variables. This could especially affect the registrations made after the fluid loads, as they were performed shortly (1–2 min) after finishing the infusion.
In summary, ΔPOP calculated from the Nellcor and Masimo pulse oximeters do not seem to be interchangeable. The device used should be taken into consideration when interpreting data based on the photoplethysmographic waveform.
References
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37(9):2642–7. doi:10.1097/CCM.0b013e3181a590da.
Maguire S, Rinehart J, Vakharia S, Cannesson M. Technical communication: respiratory variation in pulse pressure and plethysmographic waveforms: intraoperative applicability in a North American academic center. Anesth Analg. 2011;112(1):94–6. doi:10.1213/ANE.0b013e318200366b.
Antonsen LP, Kirkeboen KA. Evaluation of fluid responsiveness: Is photoplethysmography a noninvasive alternative? Anesthesiol Res Pract. 2012;2012:617380. doi:10.1155/2012/617380.
Guerin L, Monnet X, Teboul JL. Monitoring volume and fluid responsiveness: from static to dynamic indicators. Best Pract Res Clin Anaesthesiol. 2013;27(2):177–85. doi:10.1016/j.bpa.2013.06.002.
Mannheimer PD. The light-tissue interaction of pulse oximetry. Anesth Analg. 2007;105(6 Suppl):S10–7. doi:10.1213/01.ane.0000269522.84942.54.
Shelley KH. Photoplethysmography: beyond the calculation of arterial oxygen saturation and heart rate. Anesth Analg. 2007;105(6 Suppl):S31–6. doi:10.1213/01.ane.0000269512.82836.c9.
Shelley KH, Alian AA, Shelley AJ. Role of the photoplethysmographic waveform in the care of high-risk surgical patients. Anesthesiology. 2013;118(6):1479–80. doi:10.1097/ALN.0b013e31829101fa.
Awad AA, Ghobashy MA, Ouda W, Stout RG, Silverman DG, Shelley KH. Different responses of ear and finger pulse oximeter wave form to cold pressor test. Anesth Analg. 2001;92(6):1483–6.
Jablonka DH, Awad AA, Stout RG, Silverman DG, Shelley KH. Comparing the effect of arginine vasopressin on ear and finger photoplethysmography. J Clin Anesth. 2008;20(2):90–3. doi:10.1016/j.jclinane.2007.09.008.
Phillips JP, Belhaj A, Shafqat K, Langford RM, Shelley KH, Kyriacou PA. Modulation of finger photoplethysmographic traces during forced respiration: venous blood in motion? Conf Proc IEEE Eng Med Biol Soc. 2012;2012:3644–7. doi:10.1109/EMBC.2012.6346756.
Pleth variability index: a dynamic measurement to help assess physiology and fluid responsiveness. http://www.masimo.com/pdf/pvi/LAB4583B_Technical_Bulletin_Pleth_Variability_Index.pdf. Accessed 27 March 2015.
Sandroni C, Cavallaro F, Marano C, Falcone C, De Santis P, Antonelli M. Accuracy of plethysmographic indices as predictors of fluid responsiveness in mechanically ventilated adults: a systematic review and meta-analysis. Intensive Care Med. 2012;38(9):1429–37. doi:10.1007/s00134-012-2621-1.
Addison PS. A review of signal processing used in the implementation of the pulse oximetry photoplethysmographic fluid responsiveness parameter. Anesth Analg. 2014;119(6):1293–306. doi:10.1213/ANE.0000000000000392.
Hoiseth LO, Hoff IE, Hagen OA, Landsverk SA, Kirkeboen KA. Dynamic variables and fluid responsiveness in patients for aortic stenosis surgery. Acta Anaesthesiol Scand. 2014;58(7):826–34. doi:10.1111/aas.12328.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17(4):571–82. doi:10.1080/10543400701329422.
Le Manach Y, Hofer CK, Lehot JJ, Vallet B, Goarin JP, Tavernier B, Cannesson M. Can changes in arterial pressure be used to detect changes in cardiac output during volume expansion in the perioperative period? Anesthesiology. 2012;117(6):1165–74. doi:10.1097/ALN.0b013e318275561d.
Addison PS, Wang R, Uribe AA, Bergese SD. On better estimating and normalizing the relationship between clinical parameters: comparing respiratory modulations in the photoplethysmogram and blood pressure signal (DPOP versus PPV). Comput Math Methods Med. 2015;2015:576340. doi:10.1155/2015/576340.
Nilsson LM. Respiration signals from photoplethysmography. Anesth Analg. 2013;117(4):859–65. doi:10.1213/ANE.0b013e31828098b2.
Landsverk SA, Hoiseth LO, Kvandal P, Hisdal J, Skare O, Kirkeboen KA. Poor agreement between respiratory variations in pulse oximetry photoplethysmographic waveform amplitude and pulse pressure in intensive care unit patients. Anesthesiology. 2008;109(5):849–55. doi:10.1097/ALN.0b013e3181895f9f.
Alian AA, Shelley KH. Photoplethysmography. Best Pract Res Clin Anaesthesiol. 2014;28(4):395–406. doi:10.1016/j.bpa.2014.08.006.
Feldman JM. Can clinical monitors be used as scientific instruments? Anesth Analg. 2006;103(5):1071–2. doi:10.1213/01.ane.0000247882.20257.b6.
Alian AA, Galante NJ, Stachenfeld NS, Silverman DG, Shelley KH. Impact of central hypovolemia on photoplethysmographic waveform parameters in healthy volunteers part 2: frequency domain analysis. J Clin Monit Comput. 2011;25(6):387–96. doi:10.1007/s10877-011-9317-x.
Cannesson M, Le MY. Noninvasive hemodynamic monitoring: no high heels on the farm; no clogs to the opera. Anesthesiology. 2012;. doi:10.1097/ALN.0b013e3182700ad6.
Nilsson L, Johansson A, Kalman S. Respiratory variations in the reflection mode photoplethysmographic signal. Relationships to peripheral venous pressure. Med Biol Eng Comput. 2003;41(3):249–54.
Hoiseth LO, Hoff IE, Skare O, Kirkeboen KA, Landsverk SA. Photoplethysmographic and pulse pressure variations during abdominal surgery. Acta Anaesthesiol Scand. 2011;55(10):1221–30. doi:10.1111/j.1399-6576.2011.02527.x.
Hoiseth LO, Hoff IE, Myre K, Landsverk SA, Kirkeboen KA. Dynamic variables of fluid responsiveness during pneumoperitoneum and laparoscopic surgery. Acta Anaesthesiol Scand. 2012;56(6):777–86. doi:10.1111/j.1399-6576.2011.02641.x.
Acknowledgments
The study was funded by departmental resources only.
Conflict of interest
Pulse oximeter Masimo Radical 7 provided by Masimo Corp., which had no influence on the planning or conduction of the study. Otherwise, the authors declare no conflicts of interest. The authors declare no financial disclosures.
Ethical standard
All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Written informed consent was given by all the patients participating in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Høiseth, L.Ø., Hoff, I.E., Hagen, O.A. et al. Respiratory variations in the photoplethysmographic waveform amplitude depend on type of pulse oximetry device. J Clin Monit Comput 30, 317–325 (2016). https://doi.org/10.1007/s10877-015-9720-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9720-9