Abstract
Purpose
To systematically review the accuracy of the variation in pulse oxymetry plethysmographic waveform amplitude (∆POP) and the Pleth Variability Index (PVI) as predictors of fluid responsiveness in mechanically ventilated adults.
Methods
MEDLINE, Scopus and the Cochrane Database of Systematic Reviews were screened for clinical studies in which the accuracy of ∆POP/PVI in predicting the hemodynamic response to a subsequent fluid bolus had been investigated. Random-effects meta-analysis was used to summarize the results. Data were stratified according to the amount of fluid bolus (large vs. small) and to the study index (∆POP vs. PVI).
Results
Ten studies in 233 patients were included in this meta-analysis. All patients were in normal sinus rhythm. The pooled area under the receiver operating characteristic curve (AUC) for identification of fluid responders was 0.85 [95 % confidence interval (CI) 0.79–0.92]. Pooled sensitivity and specificity were 0.80 (95 % CI 0.74–0.85) and 0.76 (0.68–0.82), respectively. No heterogeneity was found within studies with the same amount of fluid bolus, nor between studies on ∆POP and those on PVI. The AUC was significantly larger in studies with a large bolus amount than in those with a small bolus [0.92 (95 % CI 0.87–0.96) vs. 0.70 (0.62–0.79); p < 0.0001]. Sensitivity and specificity were also higher in studies with a large bolus [0.84 (95 % CI 0.77–0.90) vs. 0.72 (0.60–0.82) (small bolus), p = 0.08 and 0.86 (95 % CI 0.75–0.93) vs. 0.68 (0.56–0.77) (small bolus), p = 0.02], respectively.
Conclusions
Based on our meta-analysis, we conclude that ∆POP and PVI are equally effective for predicting fluid responsiveness in ventilated adult patients in sinus rhythm. Prediction is more accurate when a large fluid bolus is administered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Assessment of fluid responsiveness, i.e., the ability of patients to increase cardiac output in response to an infusion of fluids, is essential to guide fluid resuscitation and optimize preload. Dynamic indices, which measure the cardiovascular response to a controlled variation in preload [1], have been proven to predict fluid responsiveness far better than static measures of preload, such as central venous pressure (CVP) [2, 3].
Arterial waveform derived dynamic indices, such as pulse pressure variation (PPV) [4], systolic pressure variation (SPV) [5], and stroke volume variation (SVV) [6], have become increasingly popular as predictors of fluid responsiveness in patients undergoing mechanical ventilation. Those indices indirectly measure the beat-to-beat variations in either left ventricle stroke volume (SV) or its surrogates induced by positive pressure ventilation and are based on the analysis of the arterial blood pressure waveform, recorded invasively via an intra-arterial catheter.
The analysis of the pulse oximetry waveform was postulated more than 10 years ago as a non-invasive alternative to assess blood volume status in mechanically ventilated patients [7]. Recent advances in digital signal processing combined with improvements in pulse oximetry technology have led to the development of plethysmographic dynamic indices based on the analysis of the respiratory variations in the plethysmographic waveform recorded transcutaneously by the pulse oximeter [8]. The systematic review reported here was conducted to assess the accuracy of plethysmographic dynamic indices in predicting fluid responsiveness of mechanically ventilated adult patients in both the intensive care and perioperative settings.
Materials and methods
Data reported in this review are in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [9].
Description of investigated indices
Plethysmographic indices of fluid responsiveness include the respiratory variation in pulse oximetry plethysmographic waveform amplitude (∆POP) and the pleth variability index (PVI). Both ∆POP and PVI are obtained by continuous analysis of the raw pulse oximeter signal. ∆POP is calculated as (POPmax − POPmin)/[(POPmax + POPmin) × 0.5], where POPmax and POPmin represent the maximal and the minimal amplitude, respectively, of the plethysmographic waveform over one respiratory cycle [10]. PVI is calculated as [(PImax − PImin)/PImax] × 100, where PImax and PImin represent the maximal and the minimal value, respectively, of the plethysmographic perfusion index (PI) over one respiratory cycle [11, 12]. PI is the ratio between pulsatile and nonpulsatile infrared light absorption from the pulse oximeter, and it is physiologically equivalent to the amplitude of the plethysmographic waveform [13].
The calculation of ∆POP is usually made offline, while PVI is automatically calculated by a commercial pulse oximeter (Masimo Radical 7®; Masimo Corp, Irvine, CA) so that it can be measured and continuously monitored at the bedside.
Study eligibility criteria
We considered for inclusion all clinical trials investigating the ability of ∆POP or PVI to predict the change in cardiac index, SV, or the SV index occurring after a fluid challenge in mechanically ventilated adult patients. Only studies that reported either the sensitivity, specificity, and area under the receiver operating characteristic curve (AUC) of ∆POP/PVI in identifying fluid responders, or the correlation coefficient (r) between baseline ∆POP/PVI values and subsequent changes in cardiac output after the fluid bolus were included.
Only full-text articles published in English in indexed journals were included. No publication date or publication status restrictions were imposed.
Data sources and search strategy
Two authors independently performed a search in MEDLINE, Scopus, and the Cochrane Database of Systematic Reviews using the following keywords: “fluid” OR “preload” OR “volume responsiveness”; “cardiovascular monitoring”; “fluid challenge”; “functional hemodynamic monitoring”; “dynamic indices OR indexes”; “delta POP”; “pleth index”; “plethysmographic waveform”. The search was iterated until 31 January 2012.
The automatic alert system of MEDLINE was used to identify additional studies published during the process of data extraction and analysis. References of included papers were reviewed to identify other studies of interest.
Data collection and data items
Data extraction was performed by two authors independently using a standardized form. Data were abstracted on study setting, type of ventilation, cardiac rhythm, open- versus closed-chest condition, type and amount of fluid infused, number of fluid boluses administered, definition of responders, percentage of responders, mean value of ∆POP/PVI in responders and in non-responders, correlation coefficient (Spearman or Pearson), AUC, best threshold, sensitivity, and specificity. When reported data were not sufficient to perform the planned statistical analysis, the first authors of the articles were contacted to acquire missing information.
Assessment of quality in individual studies
Quality assessment was made independently by two authors using the QUADAS scale [14], which is a tool developed specifically for assessing the quality of studies on diagnostic accuracy. Each study was scored from 0 to 14 on a 14-item evaluation sheet.
Summary measures and synthesis of results
Comprehensive Meta-Analysis® software ver. 2.2 (Biostat, Englewood, NJ: www.meta-analysis.com) was used to calculate the pooled values of AUC, the correlation coefficient r, and the difference between mean baseline values of ∆POP/PVI in responders and in non-responders. Using MetaDISC®, ver. 1.4, a dedicated software for the meta-analysis of test accuracy data [15], we calculated the pooled values of sensitivity and specificity of ∆POP/PVI in the included studies.
All values were reported as point estimate with 95 % confidence intervals (CI).
Heterogeneity and risk of bias across studies
A random-effects model was used to perform our meta-analysis. Heterogeneity was assessed using the Q and I 2 tests. The results were considered to be significant when p < 0.1 or I 2 > 50 %.
In order to investigate the potential causes of heterogeneity, the study sample was stratified according to the amount of fluid bolus administered [large (500 ml or 7–8 ml/kg) vs. small (250 ml)] and to the plethysmographic index used (∆POP vs. PVI). Differences between subgroups were analyzed using the interaction test [16].
Results
Study selection
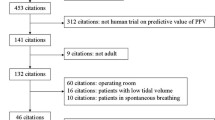
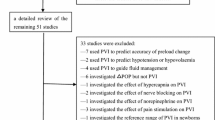
The initial dataset included 1,100 hits from MEDLINE and 1,604 hits from Scopus. No items were identified from the Cochrane Database of Systematic Reviews. After the removal of duplications and screening, 42 studies were considered for further analysis. Among these, 21 studies investigated plethysmographic indices but did not evaluate the prediction of fluid responsiveness, while 11 studies evaluated the prediction of fluid responsiveness but did not fulfil our inclusion criteria. The remaining ten studies [11, 12, 17–24] were ultimately included in our meta-analysis (Fig. 1). Excluded studies with details on the reasons for their exclusion are listed in Electronic Supplementary Material (ESM) 1.
Study characteristics
The characteristics of the ten included studies are summarized in Table 1. Six studies investigated ∆POP [17, 19, 20, 22–24], three studies investigated PVI [12, 18, 21], and one study investigated both ∆POP and PVI [11]. Since in this last study both indices were recorded in the same patient population at the same time, we included only data on PVI in the pooled analysis to avoid duplication of the sample size. The administered fluid bolus was large in seven studies and small in two studies. In one study [21], large and small fluid boluses were given to the same patient population at two different clinical times. The results from these two interventions were reported separately. In one study [18], different sites of measurements of PVI (finger, ear, forehead) were investigated. In order to maintain homogeneity with all other studies, only results obtained from the finger probe were included in the pooled analysis.
In four studies [20–23] multiple fluid boluses were administered to a single patient and the results reported using bolus—and not patient—as the statistical unit. We followed the same criteria in our meta-analysis.
Three studies [19, 22, 24] were carried out in general or post-surgical intensive care units (ICUs), while seven studies [11, 12, 17, 18, 20, 21, 23] were carried out in operating room during abdominal or cardiac surgery. All patients were in closed chest conditions, had normal sinus rhythm, and were ventilated in controlled mode with the tidal volume ranging from 7 to 10 ml/kg.
Results of included studies
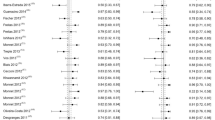
The results from the included studies are reported in Table 2. A total of 365 fluid boluses (214 large, 151 small) were administered to 233 patients (range 8–32 patients per study). The mean responder rate was 62.3 ± 14.0 %. The best threshold for the identification of responders ranged between 9.5 and 15 %.
Pooled values for AUC, sensitivity, and specificity in all studies were 0.85 (95 % CI 0.79–0.92), 0.80 (95 % CI 0.74–0.85), and 0.76 (95 % CI 0.68–0.82), respectively. The pooled r was 0.58 (95 % CI 0.43–0.70; p < 0.001), and the pooled difference between baseline values of ∆POP/PVI in responders and in non-responders was 9.1 % (95 % CI 6.3–11.9 %, p < 0.0001).
Heterogeneity and subgroup analysis
The median quality (QUADAS) score was 12 (range 12–13). Since study quality was uniformly good, a sensitivity analysis was not performed [25].
A significant heterogeneity within the ten studies was found for AUC and sensitivity (I 2 = 72.9 %, p < 0.0001 and I 2 = 46.8 %, p = 0.043, respectively; Table 3). Following stratification according to the amount of fluid bolus (large vs. small), no heterogeneity was found within each subgroup. Specificity was significantly higher in the subgroup receiving a large bolus than in that receiving the small bolus [0.86 (95 % CI 0.75–0.93) vs. 0.68 (95 % CI 0.56–0.77), respectively; p = 0.02]. Sensitivity was also higher—although not significantly—in the subgroup receiving the large bolus [0.84 (95 % CI 0.77–0.90) vs. 0.72 (95 % CI 0.60–0.82), respectively; p = 0.08).
Heterogeneity according to study index (∆POP vs. PVI) was also investigated. The analysis was restricted to the seven studies with large fluid bolus, for reasons of sample size. No heterogeneity was found between studies on ∆POP and those on PVI (Table 3).
Discussion
The results of our meta-analysis show that in adult patients with normal sinus rhythm receiving controlled mechanical ventilation, plethysmographic indices are an accurate tool for predicting the response to a subsequent fluid challenge of 500 ml or 7–8 ml/kg, while they are less accurate in predicting the response to a fluid challenge of 250 ml.
Plethysmographic indices and arterial waveform-derived indices of fluid responsiveness are physiologically related. The plethysmographic curve represents the pulsatile variation over the cardiac cycle in the amount of infrared light absorbed by hemoglobin in the capillaries of the explored tissue. The amount of absorbed light is proportional to the amount of blood in the capillary bed, which in turn is proportional to the amplitude of the arterial pulse [26, 27]. Variation in the amplitude of the arterial pulse—such as that induced by mechanical ventilation—therefore should result in a proportional variation in the amplitude of the plethysmographic curve [7, 28]. Cannesson et al. [29] found a strong correlation (r 2 = 0.83, p < 0.001) between PPV and the variations in POP in 22 sedated patients under mechanical ventilation. Similarly, a significant correlation between SPV and the variations in plethysmographic waveform peaks during controlled ventilation has been demonstrated in patients during general anaesthesia [7, 30].
In our meta-analysis, the predictive value of plethysmographic indices in studies using a large fluid challenge was comparable to that of arterial waveform-derived indices. The pooled AUC of ∆POP/PVI in those studies was 0.92 (95 % CI 0.87–0.96). In comparison, in a meta-analysis from Marik et al. [2], in which almost all included studies had been made using a large fluid challenge, the pooled AUC for PPV, SVV and SPV were 0.94 (95 % CI 0.93–0.95), 0.84 (95 % CI 0.78–0.88), and 0.86 (95 % CI 0.82–0.90), respectively. However, the correlation coefficient of plethysmographic indices in our meta-analysis was lower than that of arterial waveform-derived indices. In fact, the pooled r between the baseline value of ∆POP/PVI and the following increase in cardiac output in studies with a large bolus was 0.66 (95 % CI 0.54–0.75), while in the above-mentioned meta-analysis from Marik et al. [2] the corresponding pooled r for PPV, SVV and SPV were 0.78 (95 % CI 0.74–0.82), 0.72 (95 % CI 0.66–0.78), and 0.72 ((95 % CI 0.65–0.77), respectively. A higher correlation coefficient r for PPV versus ∆POP was also demonstrated in a prospective study from Feissel et al. [19] which directly compared ∆POP with PPV in mechanically ventilated adults. These data suggest that while plethysmographic indices are as accurate as arterial waveform-derived indices in identifying fluid responders, they are less accurate in predicting the magnitude of cardiac output increase after the fluid challenge.
Arterial waveform-derived indices are not reliable in patients with spontaneous breathing or arrhythmias [31]. In these conditions, plethysmographic indices, which share the same physiological basis of arterial waveform-derived indices, are expected to lose their predictive ability as well. We are not aware of any study on plethysmographic indices made in arrhythmic patients. However, we identified two studies that enrolled a total of 51 spontaneously breathing healthy volunteers in sinus rhythm. One of those studies was made using ∆POP [32] and the other using PVI [33]. The pooled AUC and specificity in these two studies were only 0.70 ((95 % CI 0.56–0.84) and 0.60 (95 % CI 0.38–0.78), respectively. These data confirm that plethysmographic indices have probably a limited value in patients with spontaneously breathing activity in whom passive leg raising-induced changes in cardiac output [34] should rather be used to predict fluid responsiveness.
Being based on non-invasive pulse oximetry, plethysmographic indices do not require arterial catheterization, and this allows a safer and faster assessment of fluid responsiveness as compared to arterial waveform derived indices. However, the quality of the plethysmographic signal is critically dependent on peripheral perfusion [35], which may be significantly reduced by factors such as hypothermia [36], low cardiac output [37], and drug-induced vasoconstriction. In particular, norepinephrine, by increasing the peripheral vascular tone, may reduce the pulsatile component of plethysmographic wave and therefore the accuracy of plethysmographic indices. Recent observational studies [38, 39] have in fact shown that the correlation between ΔPOP/PVI and PPV is significantly reduced in patients who are given norepinephrine. Finally, a study carried out on critical patients using Laser Doppler Flowmetry [39] revealed the presence of spontaneous cyclic peripheral vasomotor tone changes which may cause wide periodical oscillations of the peripheral plethysmographic signal recorded from the index finger. These oscillations overlap the respiratory variations in the plethysmographic signal and may cause interferences whose removal requires appropriate signal processing [40, 41].
Another factor which could affect the accuracy of plethysmographic indices is their site of measurement. In a recent study from Desgranges et al. [18], the accuracy of PVI as a predictor of fluid responsiveness was higher when the probe was positioned on the forehead or earlobe, where the subcutaneous vasculature is relatively resistant to sympathetically mediated vasomotor tone changes [42]. This suggests that, contrary to the usual practice, the fingertip is not the preferred site of measurement for plethysmographic indices, especially in patients who are on vasoactive drugs.
An important technical limitation of plethysmographic indices is represented by filtering. Pulse oximeters have been primarily developed to detect the oxygen saturation signal rather than to detect ventilation-induced changes in pulsatile plethysmogram. In particular, adaptive digital filters, which dynamically change their filtering characteristics in response to a change in band noise, have been adopted to remove noise occurring within the pulse oximeter signal bandwidth. However, this continuous adjustment in filtering may result in changes in the pulse amplitude that interfere with those induced by mechanical ventilation [43]. We cannot exclude the possibility that the accuracy of the plethysmographic indices of fluid responsiveness as reported in our review could have been affected by filtering techniques. Moreover, the use of different filtering techniques in different devices may have represented an undetected source of heterogeneity in our meta-analysis.
No difference in accuracy between PVI and ∆POP was identified in our meta-analysis. Similarly, the only study conducted to date which has directly compared PVI with ∆POP [11] did not find any significant difference between those two indices, whose reciprocal correlation coefficient r was high (0.92). In practical terms, however, PVI is more appropriate for monitoring purposes than ∆POP since it is automatically and continuously displayed by a dedicated pulse oximeter with no need for off-line analysis.
Study limitations
Our study has a series of limitations. Firstly, only three of the ten studies included in our meta-analysis were conducted in ICUs, and one of these three studies included only postoperative patients. This scarcity of studies in this clinical setting reflects the limited evidence that is currently available on the use of plethysmographic indices in the ICU, which is not entirely surprising considering that many possible sources of interference, such as spontaneous breathing, arrhythmias, and peripheral hypoperfusion, are common in intensive care patients.
Secondly, in almost all studies included in our systematic review patients were ventilated using a tidal volume of ≥8 ml/kg; therefore, our results cannot be extrapolated to patients ventilated using lower tidal volumes. Both plethysmographic and arterial waveform-derived indices are based on the hemodynamic effects on preload caused by positive pressure ventilation. These heart–lung interactions are more likely to occur when higher rather than lower tidal volumes are used. According to a paper from de Backer et al. [44], a tidal volume of at least 8 ml/kg is required for a reliable prediction using arterial waveform-derived indices. We suppose the same applies to plethysmographic indices, but this hypothesis will require further studies to be confirmed.
Thirdly, we could not specifically assess whether plethysmographic indices are less reliable predictors of fluid responsiveness in patients who are given norepinephrine, since the use of norepinephrine was reported in only three studies [19, 20, 22] included in our meta-analysis. These studies were heterogeneous as regards the amount of fluid challenge, and in two of them norepinephrine was used in combination with other vasoactive drugs (dobutamine, dopamine, or epinephrine). Specifically designed studies will be needed to investigate the effects of norepinephrine or other vasopressors on the accuracy of plethysmographic indices.
Fourthly, our meta-analysis included only studies carried out on adults, so that its results cannot be directly extrapolated to the pediatric population. Although some studies on plethysmographic indices in children have been carried out (see ESM 1), evidence regarding their use at present is still insufficient to allow for a meta-analysis.
Conclusions
The results of our meta-analysis show that in mechanically ventilated adult patients in normal sinus rhythm, both ΔPOP and PVI are reliable predictors of responsiveness to a fluid infusion of at least 500 ml or 7–8 ml/kg, while they are less capable of predicting the response to smaller boluses. The applicability of plethysmographic indices in the ICU may be limited by potential interference from several factors, such as the use of low tidal volume ventilation, spontaneous breathing activity, arrhythmias, and the use of vasopressors.
References
Cavallaro F, Sandroni C, Antonelli M (2008) Functional hemodynamic monitoring and dynamic indices of fluid responsiveness. Minerva Anestesiol 74:123–135
Marik PE, Cavallazzi R, Vasu T, Hirani A (2009) Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med 37:2642–2647
Marik PE, Baram M, Vahid B (2008) Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest 134:172–178
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P (1998) Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 89:1313–1321
Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, Perel A (2001) Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg 92:984–989
Shamir M, Eidelman LA, Floman Y, Kaplan L, Pizov R (1999) Pulse oximetry plethysmographic waveform during changes in blood volume. Br J Anaesth 82:178–181
Shelley KH (2007) Photoplethysmography: beyond the calculation of arterial oxygen saturation and heart rate. Anesth Analg 105:S31–S36, tables of contents
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Desebbe O, Cannesson M (2008) Using ventilation-induced plethysmographic variations to optimize patient fluid status. Curr Opin Anaesthesiol 21:772–778
Cannesson M, Desebbe O, Rosamel P, Delannoy B, Robin J, Bastien O, Lehot JJ (2008) Pleth variability index to monitor the respiratory variations in the pulse oximeter plethysmographic waveform amplitude and predict fluid responsiveness in the operating theatre. Br J Anaesth 101:200–206
Zimmermann M, Feibicke T, Keyl C, Prasser C, Moritz S, Graf BM, Wiesenack C (2010) Accuracy of stroke volume variation compared with pleth variability index to predict fluid responsiveness in mechanically ventilated patients undergoing major surgery. Eur J Anaesthesiol 27:555–561
Cannesson M, Delannoy B, Morand A, Rosamel P, Attof Y, Bastien O, Lehot JJ (2008) Does the Pleth variability index indicate the respiratory-induced variation in the plethysmogram and arterial pressure waveforms? Anesth Analg 106:1189–1194, table of contents
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J (2003) The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 3:25
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. Br Med J 326:219
Cannesson M, Attof Y, Rosamel P, Desebbe O, Joseph P, Metton O, Bastien O, Lehot JJ (2007) Respiratory variations in pulse oximetry plethysmographic waveform amplitude to predict fluid responsiveness in the operating room. Anesthesiology 106:1105–1111
Desgranges FP, Desebbe O, Ghazouani A, Gilbert K, Keller G, Chiari P, Robin J, Bastien O, Lehot JJ, Cannesson M (2011) Influence of the site of measurement on the ability of plethysmographic variability index to predict fluid responsiveness. Br J Anaesth 107:329–335
Feissel M, Teboul JL, Merlani P, Badie J, Faller JP, Bendjelid K (2007) Plethysmographic dynamic indices predict fluid responsiveness in septic ventilated patients. Intensive Care Med 33:993–999
Hoiseth LO, Hoff IE, Skare O, Kirkeboen KA, Landsverk SA (2011) Photoplethysmographic and pulse pressure variations during abdominal surgery. Acta Anaesthesiol Scand 55:1221–1230
Hood JA, Wilson RJ (2011) Pleth variability index to predict fluid responsiveness in colorectal surgery. Anesth Analg 113:1058–1063
Natalini G, Rosano A, Taranto M, Faggian B, Vittorielli E, Bernardini A (2006) Arterial versus plethysmographic dynamic indices to test responsiveness for testing fluid administration in hypotensive patients: a clinical trial. Anesth Analg 103:1478–1484
Solus-Biguenet H, Fleyfel M, Tavernier B, Kipnis E, Onimus J, Robin E, Lebuffe G, Decoene C, Pruvot FR, Vallet B (2006) Non-invasive prediction of fluid responsiveness during major hepatic surgery. Br J Anaesth 97:808–816
Wyffels PA, Durnez PJ, Helderweirt J, Stockman WM, De Kegel D (2007) Ventilation-induced plethysmographic variations predict fluid responsiveness in ventilated postoperative cardiac surgery patients. Anesth Analg 105:448–452
La Torre G, Chiaradia G, Gianfagna F (2006) Quality assessment in meta-analysis. Ital J Public Health 3:69–76
Awad AA, Stout RG, Ghobashy MA, Rezkanna HA, Silverman DG, Shelley KH (2006) Analysis of the ear pulse oximeter waveform. J Clin Monit Comput 20:175–184
Dorlas JC, Nijboer JA (1985) Photo-electric plethysmography as a monitoring device in anaesthesia: application and interpretation. Br J Anaesth 57:524–530
Monnet X, Lamia B, Teboul JL (2005) Pulse oximeter as a sensor of fluid responsiveness: do we have our finger on the best solution? Crit Care 9:429–430
Cannesson M, Besnard C, Durand PG, Bohe J, Jacques D (2005) Relation between respiratory variations in pulse oximetry plethysmographic waveform amplitude and arterial pulse pressure in ventilated patients. Crit Care 9:R562–R568
Partridge BL (1987) Use of pulse oximetry as a noninvasive indicator of intravascular volume status. J Clin Monit 3:263–268
Heenen S, De Backer D, Vincent JL (2006) How can the response to volume expansion in patients with spontaneous respiratory movements be predicted? Crit Care 10:R102
Delerme S, Castro S, Freund Y, Nazeyrollas P, Josse MO, Madonna-Py B, Rouff E, Riou B, Ray P (2010) Relation between pulse oximetry plethysmographic waveform amplitude induced by passive leg raising and cardiac index in spontaneously breathing subjects. Am J Emerg Med 28:505–510
Keller G, Cassar E, Desebbe O, Lehot JJ, Cannesson M (2008) Ability of pleth variability index to detect hemodynamic changes induced by passive leg raising in spontaneously breathing volunteers. Crit Care 12:R37
Cavallaro F, Sandroni C, Marano C, La Torre G, Mannocci A, De Waure C, Bello G, Maviglia R, Antonelli M (2010) Diagnostic accuracy of passive leg raising for prediction of fluid responsiveness in adults: systematic review and meta-analysis of clinical studies. Intensive Care Med 36:1475–1483
Broch O, Bein B, Gruenewald M, Hocker J, Schottler J, Meybohm P, Steinfath M, Renner J (2011) Accuracy of the pleth variability index to predict fluid responsiveness depends on the perfusion index. Acta Anaesthesiol Scand 55:686–693
Yamaura K, Irita K, Kandabashi T, Tohyama K, Takahashi S (2007) Evaluation of finger and forehead pulse oximeters during mild hypothermic cardiopulmonary bypass. J Clin Monit Comput 21:249–252
Antonelli M, Levy M, Andrews PJ, Chastre J, Hudson LD, Manthous C, Meduri GU, Moreno RP, Putensen C, Stewart T, Torres A (2007) Hemodynamic monitoring in shock and implications for management. International Consensus Conference, Paris, France, 27–28 April 2006. Intensive Care Med 33:575–590
Biais M, Cottenceau V, Petit L, Masson F, Cochard JF, Sztark F (2011) Impact of norepinephrine on the relationship between pleth variability index and pulse pressure variations in ICU adult patients. Crit Care 15:R168
Landsverk SA, Hoiseth LO, Kvandal P, Hisdal J, Skare O, Kirkeboen KA (2008) Poor agreement between respiratory variations in pulse oximetry photoplethysmographic waveform amplitude and pulse pressure in intensive care unit patients. Anesthesiology 109:849–855
Cannesson M, Awad AA, Shelley K (2009) Oscillations in the plethysmographic waveform amplitude: phenomenon hides behind artifacts. Anesthesiology 111:206–207, author reply 207–208
Shelley KH, Awad AA, Stout RG, Silverman DG (2006) The use of joint time frequency analysis to quantify the effect of ventilation on the pulse oximeter waveform. J Clin Monit Comput 20:81–87
Awad AA, Ghobashy MA, Ouda W, Stout RG, Silverman DG, Shelley KH (2001) Different responses of ear and finger pulse oximeter wave form to cold pressor test. Anesth Analg 92:1483–1486
Bendjelid K (2008) The pulse oximetry plethysmographic curve revisited. Curr Opin Crit Care 14:348–353
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL (2005) Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med 31:517–523
Acknowledgments
We gratefully thank Dr. Giuseppe Natalini, MD (Chief of Intensive Care Unit, Fondazione Poliambulanza–Istituto Ospedaliero, Via Bissolati 57, 25124 Brescia, Italy) for having provided the raw data from his study for our meta-analysis.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sandroni, C., Cavallaro, F., Marano, C. et al. Accuracy of plethysmographic indices as predictors of fluid responsiveness in mechanically ventilated adults: a systematic review and meta-analysis. Intensive Care Med 38, 1429–1437 (2012). https://doi.org/10.1007/s00134-012-2621-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2621-1