Abstract
Introduction
Systemic lupus erythematosus (SLE) and rheumatoid arthritis have complex genetic traits, but in both autoimmune diseases, dysfunctional apoptosis appears to play a part in disease pathology. This study examined the levels of in vitro apoptosis in lymphocytes from healthy, rheumatoid arthritis (RA) and SLE individuals and related observed differences to their lymphocyte apoptosis gene profiles.
Materials and Methods
Lymphocytes were assessed for cell death by nuclear pyknosis and DNA fragmentation. Control, SLE and RA apoptosis gene profiles were obtained by quantitative real-time polymerase chain reaction (QRT-PCR) analysis.
Results and Discussion
The mean levels of pyknosis in RA and SLE freshly isolated lymphocytes were significantly higher than in control lymphocytes. Ninety-three apoptosis genes were analysed by QRT-PCR of mRNA from RA, SLE and healthy lymphocytes. We identified significant differences (p < 0.05) in the expression of the same 11 of 93 and two of 93 apoptotic genes in individual SLE and RA patients tested as compared with controls.
Conclusion
We propose that similarly altered expression of specific apoptotic regulatory genes (e.g., the death effector domain-containing DNA-binding protein and apoptosis-associated speck-like protein containing a CARD) occurs in the lymphocytes of individual patients with SLE or RA that may influence the extent and rate of spontaneous apoptosis in these autoimmune conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been suggested that defective apoptosis (programmed cell death) may play a key role in human autoimmune diseases by causing an imbalance between the production and destruction of various cell types including lymphocytes [1–3]. It appears that the main mechanism by which “aged”/mature T cells are removed from the circulation involves apoptosis [4–6]. Identification of the molecular events leading to leukocyte apoptosis has been the subject of considerable attention [7, 8], and the persistence of these cells might be caused by dysregulation of apoptosis. Indeed, many laboratories have implicated several products of signalling pathways in defective apoptosis including FasL, NF-κB [9] and Bcl-2 [10]. This could ultimately lead to B and T cell hyperactivity resulting in excessive accumulation of autoantigens, polyclonal B cell activation and increases in autoantibody production [5, 11, 12]. Patients with autoimmune disease are treated with potent inducers of apoptosis (e.g. prednisolone and methotrexate), but the apoptotic genes that are influenced by these medications are not clearly established [13–15].
Lymphocytes are instrumental in regulating apoptosis of other cell types. For example, by cytotoxic T cells through the release of proteases such as perforin and granzyme B, and by T lymphocyte-derived Fas ligand (FasL/CD95L) which interacts with Fas (Apo-1/CD95) on epithelial cells. Moreover, an imbalance between the down-regulated apoptosis-inhibitor Bcl-2 and the up-regulated apoptosis-inducer Bax, or the autocrine and/or paracrine Fas/FasL interaction may influence the signals for survival or death of lymphocytes themselves or cells which they have identified for removal. Lymphocytes infiltrating the salivary glands of lupus-prone mice [16] and synovial fluid of RA patients [17] are blocked in their ability to commit to apoptosis. Alterations in the expression of the apoptosis-inducer Fas or expression of Bcl-2 may explain the resistance of these cells to apoptosis, resulting in a prolonged production of proinflammatory cytokines and autoantibodies. This could underlie the chronic inflammation at selected tissue sites in various autoimmune diseases. Furthermore, circulating lymphocytes from patients (systemic lupus erythematosus (SLE), rheumatoid arthritis and myositis) have increased levels of constitutive DNA damage, show reduced DNA repair capacity and increased susceptibility to killing by genotoxic agents [18]. We have previously shown increased levels of oxidative DNA damage in peripheral blood mononuclear cells from patients with RA and SLE suggesting an increased population of “pre-apoptotic” cells [19]. Moreover, post-translational modification of cell surface apoptotic recognition molecules may influence the sensing and removal of apoptotic cells in autoimmune conditions [20].
Pyknosis is a valid indicator of lymphocyte death and is the key “gold standard” morphologic method of distinguishing apoptotic cells [21–23]. We therefore examined the possibility that dying lymphocytes accumulate in human autoimmune diseases by comparing the levels of in vitro apoptosis in lymphocytes from patients with RA, SLE and controls by morphological (light microscopy) examination of individual lymphocytes on slides (slide-death method) and by examining the cellular DNA for the characteristic 180 base-pair fragmentation. Apoptotic regulation has been the focus of attention in several autoimmune diseases: In SLE, there is accumulation of apoptotic debris, possibly resulting from excessive cell death at a rate greater than can be cleared [24, 25]. Similarly, proinflammatory T lymphocytes appear to be resistant to apoptosis in the RA synovium [17, 26, 27]. In this study, we used QRT-PCR to quantify apoptotic gene expression in cells from controls and patients with autoimmune disease. We demonstrate that distinct differences in cellular apoptosis are observed in SLE, RA and normal individuals within each subject group, revealing distinct apoptotic expression patterns in autoimmune patients at the cellular level and mRNA level.
Methods
Patients and Controls, Cell Isolation and Culture
For the pyknosis, DNA fragmentation and QRT-PCR assays, 14 patients with RA, 10 patients with SLE and 11 healthy volunteers were enrolled. For Q-PCR analysis, five RA patients (all on methotrexate), seven SLE patients (six on at least prednisolone; see Table I for other medication) and eight healthy age-matched control subjects were selected. All RA patients fulfilled the 1987 American College of Rheumatology (ACR) criteria for RA [28], and SLE patients fulfilled the 1982 ACR criteria for SLE [29]. Informed consent was obtained from all patients (MREC project number 06/Q2102/56). Due to the relatively large volumes of blood required for both pyknosis and QRT-PCR replicate analysis, it was not possible to perform both analyses on the same patients. In the genomic studies, disease activity in the patients with SLE was assessed using the British Isles Lupus Assessment Group (BILAG) index [30]. For the purposes of this study, the BILAG grades were converted into a global index where grade A = 9 points and grade D/E = 0 points. Arbitrary cut off values of 0–5 points for inactive disease and ≥6 points for active disease were used to distinguish the level of disease activity in the patients. Disease activity of RA patients was assessed by swollen joint counts, C-reactive protein (CRP) and 28 joint disease activity score (DAS28CRP).
Peripheral blood samples were obtained from all patients and healthy volunteers in parallel. Lymphocytes from subjects were isolated using standard lymphoprep™ [31]. Cells from each sample were examined immediately (0 h) for nuclear pyknosis (see below) or cultured at a concentration of 1 × 106 cells/ml in culture medium (RPMI-1640) with 20% autologous serum at 37°C in a 5% CO2 in air for 24 h.
Analysis of Apoptosis
Apoptotic cell death can be measured by numerous morphological and biochemical methods. The most common techniques employed are terminal deoxynucleotidyl-transferase-mediated dUTP-biotin nick end labelling (TUNEL) staining, Annexin V binding and DNA laddering, but are vulnerable to generating false positive results [32, 33]. This emphasises the importance of verifying results by at least two independent methods and preferably one method that looks at the cells directly. In our study, we employed a DNA fragmentation assay together with a pyknotic lymphocyte assay since the morphological changes ocuring in cells is what is actually observed in SLE patients.
Measurement of pyknotic cells by light microscopy: Slides of intact lymphocytes were prepared with Susa fixative and stained with Mayer's hemalum with subsequent dehydration in 2-ethoxy ethanol (Cellosolv), and 500 cells on each slide were examined. Cells exhibiting nuclear pyknosis and optically homogeneous nuclear chromatin were counted as histologically dead (Fig. 1b) and were readily distinguishable from surviving counterparts. Cells were analysed at 0 h and after 24 h in culture by blinded observers. For the DNA fragmentation assay, DNA was prepared by standard procedures from approximately 5 × 106 lymphocytes. Samples were treated with 100 μg/ml proteinase K and 20 μg/ml DNase-free RNase at 56°C for 30 min and run on a 1.5% w/v agarose gel. After agarose electrophoresis, gels were stained with ethidium bromide, exposed to ultraviolet (UV) light and photographed.
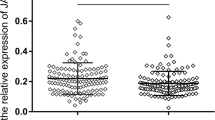
Slide deaths of lymphocytes. Immediately after lymphocyte isolation (0 h) and after 24 h in culture, cells were stained with Mayer’s hemalum, and the percentage of pyknotic cells was determined. Vertical scatter plots depict mean ± upper and lower 95% CI of the mean (as described in “Methods”)
RNA Isolation and cDNA Preparation for Apoptotic Gene QRT-PCR Analysis
For the QRT-PCR studies, 40–50 ml of blood was obtained per subject, from which fresh RNA was isolated from 5 × 106 purified lymphocytes from SLE, RA and sex-matched control subjects using the RNeasy mini kit and the RNA supplemented with 10 μl RNA stabilisation reagent (Quiagen® Ltd, West Sussex, UK). For the QRT-PCR Taqman apoptotic tiled low density (TLDA) gene array (Applied Biosystems, Warrington, UK, part no. 4378701) analysis, complementary DNA (cDNA) libraries were generated from up to 2 μg of total RNA from individual patients and healthy controls, employing a high-capacity reverse transcription kit and random primers (Applied Biosystems) in accordance to the manufacturer’s instructions.
QRT-PCR of Apoptotic Genes in SLE, RA and Healthy Individuals
Although this technique has not been previously used to analyse differences in mRNA of apoptosis genes in autoimmune patients, it has been used in several other clinical settings [34, 35]. Seven target apoptosis gene families and pathways consisting of 93 genes in total were screened (see Table II). cDNA was reverse transcribed from 500 ng of total RNA from seven SLE, five RA patients and seven controls, using the TaqMan Reverse Transcription kit (Applied Biosystems) in a total volume of 50 μl. Reaction mixtures for each sample contained 200 µl TaqMan Universal PCR master mix, 40 µl cDNA (corresponding to 400 ng RNA) in a total volume of 400 µl. Four times 100 µl of the reaction mix was added to each loading port on the array; two samples were analysed per plate. Amplification conditions were 2 min at 50°C to activate uracil-DNA glycosylase (UNG), 10 min at 94.5°C (activation), 40 cycles of denaturation at 97°C for 30 s and annealing and extension at 59.7°C for 1 min. Each sample was measured in duplicate on the same TLDA run. Data were analysed using relative quantification software (SDS2.2-Applied Biosystems) by the threshold cycle (Ct) ∆∆CT/comparative CT method, and samples were quantified relative to three housekeeping genes 18S, ACTB (β-actin), glyceraldehyde 3-phosphate dehydrogenase (GAPDH). Quality control was achieved by comparison of the duplicate crossing points for each gene per sample.
Statistical Analysis
Differences in pyknosis and apoptosis observed between SLE, RA and healthy controls were analysed by the non-parametric Mann–Whitney U test for independent samples. The statistical significance of differential TLDA gene expression among normal, RA and SLE subjects was determined by non-parametric Mann–Whitney U test by pair-wise comparison of individual Δct measurements (RA versus controls and SLE versus controls) for each group of samples. The threshold for significance was set at 0.05 (two-tailed) for all tests.
Results
Differences in Apoptotic Activity in Lymphocytes from SLE and RA Patients
The percentage of freshly isolated lymphocytes from each group showing evidence of apoptosis at 0 h was less than 10% (Fig. 1). However, the percentage of lymphocytes that were apoptotic at the beginning of culture (0 h) was moderately higher in patients with RA and SLE than in healthy controls. At 0 h, percentage (the mean ± 1 SD) of pyknotic lymphocytes (“slide-death”) in healthy controls was 1.7 ± 1.3% compared with patients with RA (3.9 ± 2.9%; p < 0.05) and SLE (3.6 ± 2.1%; p < 0.05 by Mann–Whitney U test).
The percentage of pyknotic lymphocytes after 24 h was significantly greater when compared with 0 h within each group, as expected (for healthy controls p < 0.01, for RA patients p < 0.01 and for SLE patients p < 0.0001 by Mann–Whitney U test). Patients with SLE showed significant increases in the percentage of pyknotic lymphocytes at 24 h (13.5 ± 5.2%) when compared with lymphocytes from healthy controls at 24 h (4.7 ± 1.6%; p < 0.0001), although percentage pyknosis in patients with RA at 24 h (6.3 ± 2.2%) was not significantly greater than controls at 24 h (see Fig. 1). Agarose electrophoresis of DNA isolated from both healthy and diseased lymphocytes showed the presence of a characteristic DNA “ladder”, reflecting the intranucleosomal fragmentation of DNA associated with apoptosis [24]. Typical examples of DNA fragmentation are shown in Fig. 2. The multiple bands of the ladder became progressively more intense as the culture period increased.
Gel electrophoresis of DNA. Intranucleosomal DNA samples from all groups were obtained as described in “Methods” and run on a 1.5% agarose gel using a 100-bp ladder as a molecular weight marker (denoted—STD). Samples from each group were isolated either immediately after cell isolation (0 h) or after 0, 24, 48 and 72 h in culture. Lanes 1–4, healthy control; lanes 5–8, SLE patient; and lanes 9–12, RA patient, each 0, 24, 48 and 72 h, respectively. Samples from control and RA samples over 48 h (lanes 1–3 and 9–11) show relatively little DNA fragmentation, but lanes 6, 7 and 8 from the SLE samples show the formation of “ladders” of intranucleosomal DNA fragments at ∼150–200-bp intervals (arrowheads). DNA fragmentation could be seen in control samples after 72 h (lane 4) and after 48 h in RA samples (lane 11)
QRT-PCR Analysis of Apoptotic Genes in RA and SLE Patients and Control Lymphocytes
Measurement of apoptotic gene expression in individual RA or SLE patients and age-matched controls was performed by QRT-PCR on 93 differentially expressed genes by TLDA. The results were consistent in that expression of apoptotic genes was more pronounced in lymphocytes obtained from individual SLE patients as compared with healthy controls. As shown in Fig. 3a, QRT-PCR revealed a significant increase in mRNA expression of 11 of the 93 genes screened. Comparing SLE patients with controls, BIRC2, RELB, HTRA2, BCL2L14, death effector domain-containing DNA-binding protein (DEDD2), BAD, IKBKB, TNFRSF10B, BBC3, IKBKE and BID were significantly up-regulated, and only one of 93 genes was down-regulated, namely apoptosis-associated speck-like protein containing a CARD (PYCARD) in six out of seven patients (Fig. 4). In contrast, only two of 93 genes were up-regulated significantly in RA patients, namely TNFRS21 (a member of the large TNF receptors superfamily that binds to TNF ligands) and DEDD2, the death effector domain-containing DNA-binding protein (Fig. 3b). Interestingly, (DEDD2) mRNA levels were present in control lymphocytes but significantly increased at the mRNA level from all seven SLE patients and five RA patients (by four- and five-fold, respectively). TNFRS21 was significantly up-regulated in all RA patients tested compared with controls. No significant increases or decreases were seen in the other 81 apoptotic genes screened (see Table II for genes included in study).
Genes differentially overexpressed in SLE and RA patients compared with healthy controls. Genes found to show statistically significant differences (p < 0.05) in gene expression levels in seven individual SLE patients (a) or and five RA patients (b) compared with seven control subjects are shown. The gene identity is given on the X-axis and the expression of each test gene (fold-change) relative to three house-keeping genes of each gene on the Y-axis. Levels of gene expression in pooled controls are shown in black and those in SLE or RA patients in white. Data are compiled from median fold increase and 75% interquartile ranges of individual Δct values from each individual subject analysed
PYCARD is differentially down-regulated in individual SLE patients compared with healthy controls. PYCARD mRNA expression found to be differentially expressed in seven individual control subjects and in seven individual SLE patients is shown on the graph. The gene identity is given on the X-axis and the relative expression level of each gene on the Y-axis. Levels of gene expression are relative to the average level of three endogenous control genes
Discussion
Our data confirm that freshly isolated lymphocytes show low levels of apoptosis immediately after isolation, and undergo further apoptosis in culture [36]. Immediately after isolation, the extent of pyknosis was significantly raised in both SLE and RA lymphocytes compared with healthy control cells. After 24 h in culture, the difference between SLE and control cells was accentuated, whilst there was no longer a statistically significant difference between RA and control cells, suggesting that lymphocytes from SLE patients may be more susceptible to apoptosis. This supports our previous work in which apoptotic leukocytes (measured by Annexin V binding and nuclear condensation) accumulated in the blood of SLE patients [37].
A few earlier studies have measured apoptosis in peripheral blood lymphocytes from patients with autoimmune diseases by direct morphological observation [24, 38] and demonstrated increased rates of in vitro apoptosis in cultured SLE lymphocytes but no difference of RA lymphocytes when compared with controls. However, the reliability of these methods is uncertain. Flow cytometry relies on the detection of very small percentage differences between cells, whilst the morphologic analysis [38] was restricted to small numbers of counted cells. We therefore suggest that for both methods, analysis of a greater number of lymphocytes is needed, particularly in RA where the majority of activated T cells migrate to the joints, as opposed to the vessels in SLE.
In this study, we wished to quantify fold changes in apoptosis gene expression observed in individual autoimmune patients (prescribed the two most common treatments for SLE (prednisolone) and RA (methotrexate) in our hospitals). In this study, we screened a relatively small number of patients, and one might expect to see random variation in expression of four to five genes (with a p value set at 0.05) when screening 93 genes. However, we observed the same genes being over expressed in each patient of the patient groupings, which cannot be explained by chance.
A recurrent difference was the overexpression of DEDD2 in all the RA and SLE patients tested (Fig. 3a, b) irrespective of the different medications in all patients examined compared with healthy controls. DEDD2 is highly expressed in peripheral blood leukocytes. DEDD2 has been implicated in a diverse array of diseases including autoimmune lymphoproliferative disease, arthritis and Parkinson disease [39, 40]. The protein is of particular importance in T lymphocytes where it is involved in cell proliferation and activation. DEDD2 can activate apoptosis by direct interaction of caspases in various cellular locations and may mediate apoptosis induced by activation of cell surface death receptors. For example, DEDD2 is targeted to the nucleolus of cells by its nuclear localisation signal where DEDD2 can directly activate caspase 6. DEDD2 can also bind to caspases 8 and 10 and activate caspase 3 in the cytosol [40]. Caspase 8 translocates possibly via DEDD2 interaction to the nucleus during Fas (CD95) induced apoptosis. In RA, Fas/FasL-mediated apoptosis of T cells can be inhibited by a number of factors [41], which may explain the lower degree of cell death in cells isolated from RA lymphocytes compared with SLE patients. Moreover, death effector domain proteins may under certain conditions actually prevent lymphocyte cell death [42]. Although the protein induces only moderate apoptosis directly, it can substantially sensitise cells to undergo apoptosis by Fas (CD95/APO-1), Fas-associated death domain (FADD) or tumour necrosis-related apoptosis-inducing ligand (TRAIL) [43]. Here, we observed greater spontaneous apoptosis in the lymphocytes of SLE patients compared with RA patients despite DEDD2 being up-regulated in both patient groups. However, it is known that there are increased concentrations of soluble Fas/CD95-ligand present in RA patients that can act to prevent Fas/CD95-induced apoptosis [44]. Interestingly, we observed a five-fold up-regulation of TRAIL detected by cDNA array analysis in SLE pooled lymphocytes (data not shown).
Anti-TNF biological agents are highly effective in the treatment of RA [45], but some patients do not respond [46], and the use of anti-TNF therapy can exacerbate autoimmune disease in others [47]. Therefore, a greater understanding of TNF and TNF-related ligands, and their interaction with the 30 or so members of the TNFR superfamily is required. A single member of the TNFR family, TNFRSF21, was over expressed in all the RA patients in the present study, none of whom were receiving anti-TNF therapy. TNFRSF21 is particularly abundant in lymphoid tissue and is capable of inducing apoptosis and engaging in the NF-κB and JNK pathways [48]. TNFRSF21 utilises the adaptor protein TNFR-associated death domain (TRADD) to transmit the death signal. However, we observed no significant up-regulation of TRADD mRNA expression in our RA patients compared with controls lymphocytes.
The differential down-regulation of PYCARD in SLE patients compared with RA and controls was noteworthy. Autoantibodies to dsDNA are prevalent in SLE. The generation of anti-DNA antibodies may be due to oxidative or other damage to DNA during inflammation [49]. Cells have a distinct system to recognise aberrant DNA inside the cell; toll-like receptors (TLRs), especially TLR9 are adept at binding to aberrant DNA [50]. Several other factors modulate TLR9-mediated signalling, including PYCARD. Therefore, the production of PYCARD appears to play a crucial role in the recognition of DNA, acting as an adaptor molecule for activation of caspase 1. Defective recognition of self-DNA by TLR9 and other factors associated with the inflammasome, such as PYCARD, may contribute to that part of the pathogenesis of SLE associated with DNA damage. This is the first observation of reduced PYCARD mRNA levels in SLE, and given the recent findings that deficiencies in PYCARD are critical in T cell survival and the development of experimental autoimmune diseases, terminal deoxynucleotidyl-transferase-mediated dUTP-biotin nick end labelling warrants further investigation [51]. The recent work of Habib et al. [52] demonstrated that T lymphocytes in patients with SLE are more prone to apoptosis than T lymphocytes from healthy controls or RA patients in the presence of TNF-α via differences in the TNF-α signalling pathway. It is therefore of interest in this study that SLE lymphocytes are more susceptible to apoptosis, and a member of this signalling pathway TNFRSF10B is significantly up-regulated in SLE lymphocytes and not RA patients or healthy controls.
The quantification of the differences between individual patients by QRT-PCR pinpointed altered mRNA expression corresponding to a number of genes, which may help explain the differences in apoptosis observed in different disease states. Perhaps surprising was the select few apoptotic genes that were either up- or down-regulated observed in SLE and RA patients compared with healthy controls. There is no doubt that the therapeutic medications each patient was taking prior to cell isolation may influence the overall results. However, irrespective of treatment, all individual SLE and RA patients presented with up- or down-regulation of the same specific genes, indicating that their drug treatment alone (which differed for individual patients) was not the sole influence for differences in apoptotic gene expression at the mRNA level.
Finally, in this current study, the in vitro increase in pyknotic lymphocytes isolated from SLE patients at 24 h is very marked compared with lymphocytes isolated from healthy subjects and RA patients under identical culture conditions. This suggests that SLE lymphocytes may undergo more rapid apoptosis by intrinsic regulatory pathways. If this greater rate of apoptosis occurs in vivo, even if cells are efficiently removed at the same rate as in healthy subjects, the fact that more cells are undergoing apoptosis would lead to a greater accumulation of such cells in the circulation independently of specific defects in the ability to recognise and remove apoptotic cells in individual patients. The identification and up-regulation of a specific and limited number of apoptotic regulatory genes, particularly in the lymphocytes of SLE patients, would add support to this possibility. Further work is required to determine if the genes described here contribute to resistance or increased susceptibility of lymphocytes to apoptosis in these divergent diseases.
References
Mountz JD, Wu J, Cheng J, Zhou T. Autoimmune disease. A problem of defective apoptosis. Arthritis Rheum. 1994;37:1415–20.
Navratil JS, Liu CC, Ahearn JM. Apoptosis and autoimmunity. Immunol Res. 2006;36:3–12.
Lleo A, Selmi C, Invernizzi P, Podda M, Gershwin ME. The consequences of apoptosis in autoimmunity. J Autoimmun. 2008;31:257–62.
Brown S, Heinisch I, Ross E, Shaw K, Buckley CD, Savill J. Apoptosis disables CD31-mediated cell detachment from phagocytes promoting binding and engulfment. Nature. 2002;418:200–3.
Ren Y, Savill J. Apoptosis: the importance of being eaten. Cell Death Differ. 1998;5:563–8.
Savill J. Apoptosis in disease. Eur J Clin Invest. 1994;24:715–23.
Rose LM, Latchman DS, Isenberg DA. Apoptosis in peripheral lymphocytes in systemic lupus erythematosus: a review. Br J Rheumatol. 1997;36:158–63.
Nishioka K, Hasunuma T, Kato T, Sumida T, Kobata T. Apoptosis in rheumatoid arthritis: a novel pathway in the regulation of synovial tissue. Arthritis Rheum. 1998;41:1–9.
Kuhtreiber WM, Hayashi T, Dale EA, Faustman DL. Central role of defective apoptosis in autoimmunity. J Mol Endocrinol. 2003;31:373–99.
Tamura A, Katsumata M, Greene MI, Yui K. Inhibition of apoptosis and augmentation of lymphoproliferation in bcl-2 transgenic Fas/Fas ligand-defective mice. Cell Immunol. 1996;168:220–8.
Trebeden-Negre H, Weill B, Fournier C, Batteux F. B cell apoptosis accelerates the onset of murine lupus. Eur J Immunol. 2003;33:1603–12.
Ren Y, Savill J. Proinflammatory cytokines potentiate thrombospondin-mediated phagocytosis of neutrophils undergoing apoptosis. J Immunol. 1995;154:2366–74.
da Silva CP, de Oliveira CR, da Conceicao M, de Lima P. Apoptosis as a mechanism of cell death induced by different chemotherapeutic drugs in human leukemic T-lymphocytes. Biochem Pharmacol. 1996;51:1331–40.
Seki M, Ushiyama C, Seta N, Abe K, Fukazawa T, Asakawa J, et al. Apoptosis of lymphocytes induced by glucocorticoids and relationship to therapeutic efficacy in patients with systemic lupus erythematosus. Arthritis Rheum. 1998;41:823–30.
Nakazawa F, Matsuno H, Yudoh K, Katayama R, Sawai T, Uzuki M, et al. Methotrexate inhibits rheumatoid synovitis by inducing apoptosis. J Rheumatol. 2001;28:1800–8.
Skarstein K, Nerland AH, Eidsheim M, Mountz JD, Jonsson R. Lymphoid cell accumulation in salivary glands of autoimmune MRL mice can be due to impaired apoptosis. Scand J Immunol. 1997;46:373–8.
Salmon M, Scheel-Toellner D, Huissoon AP, Pilling D, Shamsadeen N, Hyde H, et al. Inhibition of T cell apoptosis in the rheumatoid synovium. J Clin Invest. 1997;99:439–46.
Lawley PD, Topper R, Denman AM, Hylton W, Hill ID, Harris G. Increased sensitivity of lymphocytes from patients with systemic autoimmune diseases to DNA alkylation by the methylating carcinogen N-methyl-N-nitrosourea. Ann Rheum Dis. 1988;47:445–51.
Bashir S, Harris G, Denman MA, Blake DR, Winyard PG. Oxidative DNA damage and cellular sensitivity to oxidative stress in human autoimmune diseases. Ann Rheum Dis. 1993;52:659–66.
Eggleton P, Haigh R, Winyard PG. Consequence of neo-antigenicity of the ‘altered self’. Rheumatology (Oxford). 2008;47:567–71.
Thomson AE, O'Connor TW, Wetherley-Mein G. Killing and characterizing action of colchicine in vitro on lymphocytes of chronic lymphocytic leukaemia. Scand J Haematol. 1972;9:231–47.
Ru YX, Zhu XF, Gao JT, Wang HJ, Zhao SX, Feng M, et al. Ultrastructural characteristics of nucleated cells in bone marrow of patients with acquired aplastic anemia. Ultrastruct Pathol. 2008;32:81–8.
Ishimaru MJ, Ikonomidou C, Tenkova TI, Der TC, Dikranian K, Sesma MA, et al. Distinguishing excitotoxic from apoptotic neurodegeneration in the developing rat brain. J Comp Neurol. 1999;408:461–76.
Emlen W, Niebur J, Kadera R. Accelerated in vitro apoptosis of lymphocytes from patients with systemic lupus erythematosus. J Immunol. 1994;152:3685–92.
Ren Y, Xiong L, Wu JR. Induction of mitochondrion-mediated apoptosis of CHO cells by tripchlorolide. Cell Res. 2003;13:295–300.
Raza K, Scheel-Toellner D, Lee CY, Pilling D, Curnow SJ, Falciani F, et al. Synovial fluid leukocyte apoptosis is inhibited in patients with very early rheumatoid arthritis. Arthritis Res Ther. 2006;8:R120.
Filer A, Parsonage G, Smith E, Osborne C, Thomas AM, Curnow SJ, et al. Differential survival of leukocyte subsets mediated by synovial, bone marrow, and skin fibroblasts: site-specific versus activation-dependent survival of T cells and neutrophils. Arthritis Rheum. 2006;54:2096–108.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24.
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–7.
Hay EM, Bacon PA, Gordon C, Isenberg DA, Maddison P, Snaith ML, et al. The BILAG index: a reliable and valid instrument for measuring clinical disease activity in systemic lupus erythematosus. Q J Med. 1993;86:447–58.
Boyum A. Separation of leukocytes from blood and bone marrow. Introduction. Scand J Clin Lab Invest Suppl. 1968;97:7.
Walker JA, Quirke P. Viewing apoptosis through a ‘TUNEL’. J Pathol. 2001;195:275–6.
Rieger AM, Hall BE, Luong LT, Schang LM, Barreda DR. Conventional apoptosis assays using propidium iodide generate a significant number of false positives that prevent accurate assessment of cell death. J Immunol Methods. 2010 (in press).
Lu B, Xu J, Chen J, Yu J, Xu E, Lai M. TaqMan low density array is roughly right for gene expression quantification in colorectal cancer. Clin Chim Acta. 2008;389:146–51.
Jiang Z, Hu J, Li X, Jiang Y, Zhou W, Lu D. Expression analyses of 27 DNA repair genes in astrocytoma by TaqMan low-density array. Neurosci Lett. 2006;409:112–7.
Bell DA, Morrison B, VandenBygaart P. Immunogenic DNA-related factors. Nucleosomes spontaneously released from normal murine lymphoid cells stimulate proliferation and immunoglobulin synthesis of normal mouse lymphocytes. J Clin Invest. 1990;85:1487–96.
Donnelly S, Roake W, Brown S, Young P, Naik H, Wordsworth P, et al. Impaired recognition of apoptotic neutrophils by the C1q/calreticulin and CD91 pathway in systemic lupus erythematosus. Arthritis Rheum. 2006;54:1543–56.
Lorenz HM, Grunke M, Hieronymus T, Herrmann M, Kuhnel A, Manger B, et al. In vitro apoptosis and expression of apoptosis-related molecules in lymphocytes from patients with systemic lupus erythematosus and other autoimmune diseases. Arthritis Rheum. 1997;40:306–17.
Ryu EJ, Angelastro JM, Greene LA. Analysis of gene expression changes in a cellular model of Parkinson disease. Neurobiol Dis. 2005;18:54–74.
Valmiki MG, Ramos JW. Death effector domain-containing proteins. Cell Mol Life Sci. 2009;66:814–30.
Alcivar A, Hu S, Tang J, Yang X. DEDD and DEDD2 associate with caspase-8/10 and signal cell death. Oncogene. 2003;22:291–7.
Yu JW, Shi Y. FLIP and the death effector domain family. Oncogene. 2008;27:6216–27.
Roth W, Stenner-Liewen F, Pawlowski K, Godzik A, Reed JC. Identification and characterization of DEDD2, a death effector domain-containing protein. J Biol Chem. 2002;277:7501–8.
Korb A, Pavenstadt H, Pap T. Cell death in rheumatoid arthritis. Apoptosis. 2009;14:447–54.
Coenen MJ, Toonen EJ, Scheffer H, Radstake TR, Barrera P, Franke B. Pharmacogenetics of anti-TNF treatment in patients with rheumatoid arthritis. Pharmacogenomics. 2007;8:761–73.
Erickson AR, Mikuls TR. Switching anti-TNF-alpha agents: what is the evidence? Curr Rheumatol Rep. 2007;9:416–20.
Ramos-Casals M, Brito-Zeron P, Munoz S, Soria N, Galiana D, Bertolaccini L, et al. Autoimmune diseases induced by TNF-targeted therapies: analysis of 233 cases. Medicine (Baltimore). 2007;86:242–51.
Pan G, Bauer JH, Haridas V, Wang S, Liu D, Yu G, et al. Identification and functional characterization of DR6, a novel death domain-containing TNF receptor. FEBS Lett. 1998;431:351–6.
Lunec J, Herbert K, Blount S, Griffiths HR, Emery P. 8-Hydroxydeoxyguanosine. A marker of oxidative DNA damage in systemic lupus erythematosus. FEBS Lett. 1994;348:131–8.
Lande R, Gregorio J, Facchinetti V, Chatterjee B, Wang YH, Homey B, et al. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature. 2007;449:564–9.
Shaw PJ, Lukens JR, Burns S, Chi H, McGargill MA, Kanneganti TD. Cutting Edge: critical role for PYCARD/ASC in the development of experimental autoimmune encephalomyelitis. J Immunol. 2010;184:4610–4.
Habib HM, Taher TE, Isenberg DA, Mageed RA. Enhanced propensity of T lymphocytes in patients with systemic lupus erythematosus to apoptosis in the presence of tumour necrosis factor alpha. Scand J Rheumatol. 2009;38:112–20.
Acknowledgements
We thank Dr Alicja M Gruska for help with the slide assays, Dr Claire Bennett (Exeter University, UK) for help in optimising the TLDA-QRT-PCR method and Dr Vanessa Gilston for technical assistance. We also thank Mrs Susan Westoby for secretarial assistance and Dr Marc Williams (University of Rochester School of Medicine and Dentistry) for critical review of the manuscript. This work was supported by research grants from the Arthritis Research Campaign numbers, E0521, E0543, 17231, and 16537 and Lupus UK. Support was also received from the Peninsula NIHR Clinical Research facility. We dedicate this paper to the memory of our colleague Dr Gilmour Harris, a provocative and admired immunologist, who played a central role in initiating the study reported here.
Disclosure statement
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eggleton, P., Harries, L.W., Alberigo, G. et al. Changes in Apoptotic Gene Expression in Lymphocytes from Rheumatoid Arthritis and Systemic Lupus Erythematosus Patients Compared with Healthy Lymphocytes. J Clin Immunol 30, 649–658 (2010). https://doi.org/10.1007/s10875-010-9429-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-010-9429-y