Abstract
Objectives
Objectives The objectives of this study are to (1) evaluate the ability of the immune system to synthesize specific antibodies that catalyze the degradation of amyloid β peptide (Aβ) and to (2) evaluate the prospect of developing a catalytic IVIG (CIVIG) formulation for therapy of Alzheimer’s disease (AD).
Conclusions
Polyclonal autoantibodies from humans without dementia hydrolyzed Aβ specifically. The catalytic activity improved as a function of age. Patients with AD produced catalytic antibodies at increased levels. IgM-class antibodies expressed the activity at levels superior to IgGs. Production of catalytic autoantibodies appears to be an innate immunity function with adaptive improvements occurring upon Aβ overexpression, which suggests a beneficial function of the catalytic activity. The catalytic autoantibodies impeded Aβ aggregation, dissolved preformed Aβ aggregates, and inhibited Aβ cytotoxicity in tissue culture. Recombinant catalytic antibodies from a human library have been identified, validating the phenomenon of antibody-catalyzed Aβ cleavage. As a single catalyst molecule inactivates multiple Aβ molecules, catalytic antibodies may clear Aβ efficiently. IVIG did not cleave Aβ, indicating the importance of purification procedures that maintain catalytic site integrity. Traditional Aβ-binding antibodies form immune complexes that can induce inflammatory reaction and vascular dysfunction. Catalysts do not form stable immune complexes, minimizing these risks. Criteria appropriate for developing a CIVIG formulation with potential therapeutic utility are discussed, including isolation of the Aβ-specific catalytic subsets present in IgM and IgG from human blood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The therapeutic power of natural IgG antibodies is evident from the use of intravenous immune globulin (IVIG) preparations (pooled IgG from the blood of healthy humans) for treating patients with immunodeficiency, autoimmune disease, bone marrow transplants, and several off-label diseases. The beneficial mechanisms underlying IVIG therapy have been highly debated [1]. The variable (V) domains of human antibodies are encoded by >100 V, D, and J heritable genes (germline genes). As B cells differentiate from their early IgM-secreting state to producing class-switched IgG/IgA antibodies, various immune mechanisms select for mutant V domains capable of recognizing individual antigens with increasing affinity and specificity. These include foreign antigens and autoantigens. The term natural antibodies is often used to distinguish comparatively low-affinity antibodies with polyreactive antigen reactivity profile from high-affinity antibodies that bind individual antigens with minimal or no cross-reactivity. A subset of antibodies that bind antigens noncovalently proceeds to catalyze chemical reactions. This has led to the consideration of novel physiological roles and therapeutic applications of antibodies. Naturally occurring peptide bond-cleaving antibodies use a serine protease-like mechanism that entails nucleophilic attack on the weakly electrophilic carbonyl groups of the peptide backbone. Catalysis was originally identified as a specific autoantigen-directed function of autoantibodies [2]. Examples of promiscuous catalytic antibodies, specific catalytic antibodies to foreign antigens, and specific catalytic antibodies to a B-cell superantigen have now been described [3, 4]. IgM-class antibodies from healthy humans express the catalytic activity preferentially [3, 4], and secretory IgAs can express catalytic activities directed to mucosal microbes [5]. The catalytic activity appears to be an innate immune function. This implies that the catalytic antibodies are phylogenetically ancient molecules that were developed prior to the evolution of modern adaptive immunity mediated by somatic selection of the high-affinity antigen-binding function.
Alzheimer’s disease (AD) is the most common age-induced dementia with an estimated worldwide prevalence of 26 million. Accumulation of amyloid β (Aβ) peptide aggregates is thought to play a central role in the disease’s pathogenesis. Even physiological aging may be associated with increased Aβ. Proteolytic processing of the amyloid precursor protein generates the 40/42 residue peptides Aβ40 and Aβ42, respectively, the dominant constituents of vascular and parenchymal Aβ deposits in the AD brain. The toxicity of soluble Aβ oligomers is suggested to cause neurodegenerative effects including impaired electrical conduction and memory-related receptor dysfunction [6]. Low Aβ concentrations can stimulate cell growth but there is no known physiological function of age-induced Aβ overproduction. Consequently, Aβ removal is a prospective treatment strategy for AD. Aβ-binding antibodies of the IgG class can clear Aβ from the brain by the following mechanisms [7] (Fig. 1a): (a) small amounts of peripherally administered IgG cross the blood-brain barrier (BBB) at ∼0.1% of injected IgG dose and bind Aβs in the brain. Microglial cells then ingest the immune complexes via an Fcγ-receptor–mediated process that results in Aβ clearance; (b) anti-Aβ IgG bound to the neonatal Fc receptor (FcRn) on the abluminal (brain) side of the BBB acts as a pump to enhance Aβ efflux into the periphery; (c) antibody binding constrains Aβ into a nonaggregable conformation; and (d) according to the “peripheral sink” hypothesis, Aβ binding by antibodies in peripheral blood perturbs the equilibrium between the diffusible peptide pools on the two sides of the BBB, thereby inducing compensatory Aβ release from the brain. In this hypothesis, there is no requirement for IgG entry into the brain.
Potential for treatment of Alzheimer’s disease (AD): passive immunotherapy with Aβ binding and Aβ hydrolyzing Igs. a Aβ binding IgG. Reversibly binding IgG injected into peripheral blood can enter the brain in small amounts and help clear Aβ by mechanisms described in the text. Following binding of IgG to Aβ monomers (a) or aggregates (b), the immune complexes are ingested by an Fcγ receptor-dependent uptake process by microglia (c). The IgG bound by Fcn receptors at the blood-brain barrier (BBB) may help clear Aβ from the brain by facilitating efflux to the periphery through a transcytosis process (d). Microglial ingestion of the immune complexes is accompanied by release of inflammatory mediators, which could exacerbate the already inflamed state of the AD brain. In mouse AD models, clearance of amyloid plaques from the brain parenchyma induced by Aβ-binding IgGs is accompanied by Aβ deposition in the blood vessels and microhemorrhages. b Aβ hydrolyzing Ig. Sufficient amounts of a catalytic antibody administered into peripheral blood are predicted to gain entry into the brain and hydrolyze brain Aβ deposits and soluble oligomers, reducing the brain Aβ burden. Like the IgG in panel a, catalytic Ig containing the Fc domain may mediate an FcRn-mediated Aβ transcytosis. LRP1/RAGE transporters are known to help maintain the equilibrium between brain and peripheral Aβ. c Aβ hydrolyzing IgM. Hydrolysis of Aβ by peripheral IgM increases the Aβ brain-periphery concentration difference and thereby enhances Aβ efflux from the brain. Catalytic IgM bound to FcRμ/α on the luminal (blood) side of the BBB are hypothesized to enhance the local concentration difference at the BBB, thus inducing an overcompensatory depletion effect and facilitating sustained removal of brain Aβ into the periphery. FcRn neonatal Fc receptor; FcRμ/α Fc receptor for IgM; LRP-1 low-density lipoprotein receptor related protein 1, RAGE receptor for advanced glycation end products
We review here the ontogeny of catalytic antibodies to Aβ, adaptive immune mechanisms that may improve the catalytic function, potential physiological benefits of the catalytic antibodies, and the prospect of applying these molecules for passive immunotherapy of AD.
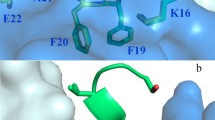
Aβ Autoantibodies
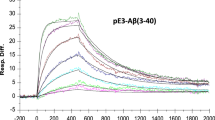
Aβ is an autoantigenic peptide. Small amounts of Aβ-binding IgG autoantibodies are present in the blood of healthy humans [8, 9]. IgM-class autoantibodies from healthy humans catalyze the specific breakdown of Aβ [10, 11]. Class-switched IgGs, which are produced in the terminal phase of adaptive B cell maturation, display lower catalytic activity (Fig. 2a). A single catalyst molecule cleaves multiple Aβ molecules, whereas the combining site of a reversibly binding antibody can only inactivate a single Aβ molecule. Consistent with the expectation of superior potency, Aβ cleavage is detected at substantially lower IgM concentrations than binding of the peptide by IgG-class autoantibodies. Aβ binding by the IgMs is not detected at all because their noncovalent binding affinity is insufficient and Aβ cleavage reduces the lifetime of the immune complexes. In addition, the catalysts and reversibly binding antibodies may express differing epitope specificities. IgG-class autoantibodies bind the central Aβ sequence and conformational epitopes generated by Aβ aggregation [8, 9]. Such binding reactions can impede further aggregation and sterically hinder the recognition of Aβ by other binding proteins. The functional effects of catalytic antibodies, on the other hand, are governed by the peptide bond cleavage event. Polyclonal catalytic IgMs hydrolyze the Lys16-Leu17 and Lys28-Gly29 bonds of Aβ. Fragments of Aβ are generally less aggregogenic than full-length Aβ. Nonetheless, the site of cleavage is important, because the fragments produced by cleavage at different bonds may form aggregates at varying rates and may also express other Aβ functional effects at variable levels. A recombinant catalytic Ig fragment hydrolyzed Aβ at a bond located in its central sequence but the initial noncovalent interaction occurred largely at the Aβ terminus. This illustrates the previously proposed split-site model of catalysis [3, 4] in which initial antigen binding at the noncovalent antibody site places a remote peptide bond in register with the catalytic site (Fig. 2b). Various aggregation states of Aβ contain constituent monomers with differing conformations. Therefore, noncovalent catalyst recognition of the same Aβ epitope in the monomer, oligomer, and higher-order aggregation states can result in cleavage of Aβ at different peptide bonds.
Cleavage of Aβ40 by human IgM and IgG. a Aβ40 (100 µM) was incubated for 3 days at 37°C with IgG (1.6 µM) or IgM (34 nM) pooled from six non-AD subjects each of age <35 years (young) or >72 years (old). Reactions were analyzed by reversed phase HPLC (gradient of 10% to 80% acetonitrile in trifluoroacetic acid, 45 min; detection at 220 nm). Hydrolysis rates were computed from the area of the Aβ1-28 product peak interpolated from a standard curve that was constructed using increasing amounts of synthetic Aβ1-28 (means ± SD; n = 4 assays). *P < 0.0044; **P < 0.035. Two-tailed unpaired t test. b Molecular basis for epitope specificity of proteolytic antibodies: split-site model. Two different antibody subsites are responsible for the initial noncovalent antigen binding and the subsequent peptide bond hydrolysis process. In the initial immune complex (left), the antigen region not involved in noncovalent antibody binding enjoys conformational flexibility. Consequently, peptide bonds remote from the noncovalent binding site that are in register with the antibody nucleophilic subsite can be hydrolyzed (right). Triangle nucleophile, circle neighboring general base that activates the nucleophile
Because Aβ is a self-antigen, findings of consistent autoantibody production by healthy humans raise novel questions concerning the mechanism of Aβ immunogenicity and evolutionary purpose of the anti-Aβ autoantibody response. Two seemingly contradictory views are reasonable. First, the autoantibody response may arise from dysfunctional autoimmune reactivity with an outcome that is coincidentally beneficial because excess Aβ is deleterious. Second, the autoantibody response may represent a physiological process that is expressed in a programmed manner to control the threat of Aβ-induced neurodegenerative effects. The first view is supported by the “horror autotoxicus” conception of autoimmunity. Production of Aβ autoantibodies may be explained by the appearance of aggregate-specific Aβ conformational epitopes and Aβ neoepitopes formed due to the reaction of Aβ with sugars and metabolites of lipid peroxidation [12, 13]. As these epitopes may not be present at sufficient concentrations until Aβ is overproduced at the later stages of life, induction of tolerance in the critical fetal stages of immune system development is likely to be inadequate. The second view is supported by the ability of the mostly conserved framework regions (FRs) of antibody V domains to participate in the recognition of certain polypeptides. A recent study reports binding of conformational epitopes expressed by amyloid proteins as an inherent property of antibody subunits that is evidently not dependent on classical mechanisms of antigen recognition [14]. Adaptive humoral immunity is generally mediated by the sequence-diversified complementarity determining regions (CDRs) of the V domain, the contact sites for traditional foreign antigens and self-antigens. In our initial studies, removal of the CDRs from a catalytic Ig fragment did not result in loss of Aβ cleaving activity (unpublished data), supporting a role for the FRs in Aβ recognition. This is functionally analogous to FR recognition of B-cell superantigens, an innate property developed over millions of years of immune system evolution, presumably to counter ancient microbes [15]. Perhaps an innate ability to recognize pathogenic amyloid structures represents a defense mechanism that is preprogrammed in the immune system.
The foregoing views can be reconciled by positing that Aβ recognition is an innate antibody function that improves adaptively when needed most, that is, under nonhomeostatic conditions of Aβ overproduction. Adaptive improvements of both the catalytic rate constant and noncovalent binding functions are possible. The former improvement mechanism is supported by observations of an age-dependent increase of catalytic IgMs in humans without dementia and a further increase of the catalytic antibodies in AD patients [11]. Nucleophilic catalytic sites mediate Aβ cleavage [11]. Others and we have demonstrated improved nucleophilic catalysis by antibodies raised to synthetic electrophilic antigens [16, 17]. The Aβ adducts with metabolites of lipid peroxidation and dicarbonyl glycation intermediates can be anticipated to react covalently with nucleophilic groups [3, 4]. Electrophilic stimulation of B cells by the Aβ reaction products may be conceived, therefore, as a process that drives selection of antibodies with adaptively increased nucleophilic reactivity and favors improved expression of the innate catalytic function.
Inefficient IgM→IgG class switching of the Aβ-cleaving antibodies reveals a limitation on adaptive improvement of the catalytic function. The limitation may derive from accumulation of CDR mutations in the IgG compartment of the response that disrupt the fine structure of the catalytic site; reduced structural integrity of the catalytic site when expressed within the constant domain scaffold of IgG; or insufficiency of T-cell help, an important requirement for IgM→IgG class switching.
Adaptive improvement of the traditional function of antibodies, noncovalent binding, is supported by the appearance of Aβ-binding autoantibodies in transgenic mice that overexpress Aβ [18] and in AD patients [19]. However, opposing observations of decreased Aβ-binding antibodies in AD patients have also been reported [20]. It is difficult to detect antibodies that are tightly bound by endogenous Aβ [18]. An interpretation that diminished Aβ-binding autoantibodies contribute to the pathogenesis of AD cannot be sustained until the conflicting observations are resolved. This caveat does not apply to the observed increase of catalytic antibodies in AD patients because catalysts do not form stable immune complexes. Consequently, we prefer to view catalytic antibody production in elderly and AD patients as beneficial events that might protect against the neurodegenerative effects of Aβ only partially.
IVIG and Catalytic IVIG Formulations
After enrichment by immobilized Aβ chromatography, Aβ-binding IgG autoantibodies from healthy humans impeded formation of Aβ aggregates and dissolved preformed Aβ fibrils [21]. Administration of IVIG to AD patients at a cumulative dose of hundreds of grams over several months has provided preliminary evidence of reduced cognitive decline accompanied by transiently increased blood Aβ and decreased cerebrospinal Aβ levels [22].
A firm mechanistic basis for the potential benefit of reversibly binding Aβ antibodies present in IVIG is not available. Information gleaned from Aβ-binding humanized monoclonal antibodies is relevant to interpreting the IVIG effects. Studies in Aβ-overexpressing transgenic mice have provided unambiguous evidence for the ability of the monoclonal antibodies to clear brain Aβ deposits and improve cognition [7]. Like the monoclonal antibodies, small amounts of Aβ-binding IgGs purified from human blood appear to cross the BBB [23], permitting conception of local antibody-facilitated Aβ clearance. The phase 2 trial of intravenously infused bapineuzumab, a monoclonal IgG to the Aβ N terminus, revealed a modest, reduced risk of cognitive decline in AD patients who were negative for the ApoE4 allele, a genetic trait associated with delayed AD onset [7]. In another phase 2 trial of an intravenously administered monoclonal IgG directed to an epitope in the middle region of Aβ (Eli Lilly and Co., Indianapolis, IN, USA), increased Aβ levels in cerebrospinal fluid and decreased Aβ levels in peripheral blood of AD patients were noted [7]. To the extent that the increase of peripheral Aβ is attributable to a release from the brain peptide stores, the antibody may exert a favorable effect.
Safety concerns have been raised about Aβ-binding antibodies [7]. Mouse studies indicate that clearance of antibody-Aβ immune complexes through the microglial uptake pathway holds the risk of inflammatory mediator release. Immune complex deposition in the vascular walls may cause microbleeds. There was no evidence for an unacceptable inflammatory reaction in the monoclonal IgG human trials, but a dose-limiting incidence of vasogenic edema was evident in magnetic resonance imaging (MRI) tests after bapineuzumab administration, an effect that suggests vascular dysfunction (Fig. 1a). Antibodies that do not permeate into the brain should be free of this side effect. The safety profile of IVIG in AD patients remains to be examined by predictive methods such as MRI, but no untoward effects were reported in a recently published trial on eight patients [22]. From these results, there is cautious support for passive AD immunotherapy using Aβ-binding antibodies. However, there is also concern that their therapeutic efficacy may not be sufficiently robust and that side effects are possible.
Provided that the cleavage of Aβ is sufficiently specific, clearance of Aβ by catalytic antibodies should occur with many of the advantages and none of the disadvantages of Aβ-binding antibodies. Because catalysts that enter the brain will not form long-lived immune complexes, the risk of vascular immune complex deposition and microglial release of inflammatory mediators occurring as a result of Fc-receptor mediated immune complex uptake is minimized (Fig. 1b). If the rate of Aβ cleavage is sufficiently rapid, any reduction in Aβ clearance due to loss of the immune complex uptake pathway is inconsequential. Similarly, antibodies bound via the Fc receptor on the brain side of the BBB will cleave Aβ, and the process of antibody-facilitated Aβ efflux from the brain will be rendered redundant (Fig. 1b). Catalytic IgM preparations from healthy humans inhibited Aβ aggregation, dissolved preformed Aβ aggregates, and inhibited the toxic effect of Aβ oligomers on cultured neuronal cells [10, 11]. Other than microbial B cell superantigens [3, 4], the Aβ-cleaving human IgM preparations did not degrade various self-proteins or foreign proteins. Pooled IgM from human blood, therefore, deserves consideration as a potentially therapeutic catalytic IVIG (CIVIG) formulation. In light of the large mass of IgM molecules (900 kDa), ingress of peripherally injected IgM into the brain is predicted to be more restricted than the smaller IgG molecules (150 kDa). The potential benefit of an IgM CIVIG preparation, therefore, will depend largely on compensatory release of brain Aβ stores following peripheral Aβ clearance by the catalytic IgM (Fig. 1c).
IgG purified from the plasma of old humans by an affinity fractionation procedure involving acid treatment also hydrolyzed Aβ detectably (Fig. 2a), albeit at levels smaller than the IgM fractions from the same humans. No Aβ hydrolysis was detected by an IVIG preparation (Fig. 3a; Carimune, CSL Behring, 2.2 mg/mL; a concentration >100-fold of polyclonal human IgM yielding detectable Aβ hydrolysis in Fig. 2a). Similarly, there was no detectable hydrolysis of 125I-Aβ by another IVIG preparation (Fig. 3b; Intratect, Biotest Pharma GmbH, 0.15 mg/mL). In a previous study [24], we tested as substrates small peptide microantigens that are recognized by catalytic antibodies largely with minimal contributions from noncovalent epitope recognition. The small peptides were also cleaved poorly by IVIG preparations compared with IgG purified by the acid-affinity purification procedure. Evidently, the IgG catalytic activity does not survive the purification procedures used to prepare IVIG. Recent studies on a recombinant catalytic antibody fragment also suggest the sensitivity of the catalytic site to conformational perturbations [25]. The antibody fragment displayed profoundly altered levels of Aβ-cleaving activity following structural perturbations remote from the catalytic site [25]. The catalytic activity of antibodies depends on maintenance of intramolecular activation interactions within precisely positioned amino acid dyads and triads, e.g., the activation of the Ser hydroxyl side chain enabled by hydrogen bonding with properly positioned imidazole nitrogen. Even small, sub-angstrom side-chain movements can weaken the activation reaction and compromise the catalytic activity. In order to purify catalytic antibodies, therefore, procedures that minimize their structural perturbations must be used.
The distinction between the catalytic and binding function of antibodies is also illustrated by the recent report that that even mild denaturing steps used for industrial preparation of IVIG expose cryptic autoantibody-binding activities, including an increased ability to bind Aβ [26]. The activating effect was ascribed to subtle changes in the IgG structure. Removal of physiological autoantibody inhibitors is another possibility. In contrast, the IVIG fractionation technology compromises the catalytic function of antibodies.
Homogeneous vs. Heterogeneous Antibody Formulations
Blood-borne antibodies are a mixture of varying proportions of a large number of individual antibodies with diverse antigenic specificities. They represent a snapshot of ongoing immune responses and immune memory developed as a result of prior stimulation with foreign antigens and self-antigens. Pooling the antibodies from thousands of individuals for IVIG preparation presumably amplifies the range of beneficial antigenic specificities. It can be argued that the presence of antibodies with multiple antigenic specificities is an essential aspect of IVIG therapy. For example, autoantibodies to tau, the protein responsible for forming tau tangles in the AD brain, have been described [27]. It is conceivable that the combination of antibodies to Aβ and tau is more beneficial than the individual antibodies to these antigens. On the other hand, the use of antibody mixtures might reduce therapeutic efficacy because of the presence of inhibitory antibodies or tightly bound antigens, e.g., homeostatic anti-idiotypic antibodies to the combining site of Aβ autoantibodies or Aβ bound to the autoantibodies.
It can be hypothesized that improved therapeutic efficacy may be possible by the use of the Aβ-specific catalytic antibody subset isolated from polyclonal human antibodies or a homogenous preparation consisting of a single catalytic antibody. This subset within the polyclonal IgM and IgG preparations can be isolated by a covalent affinity chromatography procedure analogous to the selection method used to identify recombinant phage antibodies with specific Aβ-cleaving activity [25]. The procedure relies on covalent binding of an electrophilic Aβ analog to the nucleophilic antibody sites responsible for catalysis. Irrelevant and noncovalently binding antibodies are removed by dissociation at acid pH prior to catalyst elution. Homogeneous human antibody fragments isolated by this procedure display Aβ-cleaving activities several orders of magnitude superior to polyclonal IgM and IgG fractions purified from human blood [25]. Because Aβ-specific catalysts represent a small minority of the polyclonal antibody mixtures, the purification procedure is predicted to yield a CIVIG formulation with catalytic rate constant rivaling that of homogenous antibodies. In principle, small amounts of an Aβ-specific CIVIG formulations are predicted to clear Aβ with minimal side effects.
Lacroix-Desmazes et al [28] observed that high levels of catalytic antibodies that cleaved a small peptide microantigen described earlier correlate with reduced mortality in patients with sepsis. This provides additional impetus for the notion that supplementing endogenous catalytic antibodies by CIVIG infusion will be a useful therapeutic principle. Further studies of the medical utility of CIVIG are warranted.
References
Vani J, Elluru S, Negi VS, Lacroix-Desmazes S, Kazatchkine MD, Bayary J, et al. Role of natural antibodies in immune homeostasis: IVIg perspective. Autoimmun Rev. 2008;7:440–4.
Paul S, Volle DJ, Beach CM, Johnson DR, Powell MJ, Massey RJ. Catalytic hydrolysis of vasoactive intestinal peptide by human autoantibody. Science. 1989;244:1158–62.
Paul S, Nishiyama Y, Planque S, Taguchi H. Theory of proteolytic antibody occurrence. Immunol Lett. 2006;103:8–16.
Paul S, Nishiyama Y, Planque S, Karle S, Taguchi H, Hanson C, et al. Antibodies as defensive enzymes. Springer Semin Immunopathol. 2005;26:485–503.
Planque S, Mitsuda Y, Taguchi H, Salas M, Morris MK, Nishiyama Y, et al. Characterization of gp120 hydrolysis by IgA antibodies from humans without HIV infection. AIDS Res Hum Retroviruses. 2007;23:1541–54.
Walsh DM, Selkoe DJ. Aβ oligomers—a decade of discovery. J Neurochem. 2007;101:1172–84.
Brody DL, Holtzman DM. Active and passive immunotherapy for neurodegenerative disorders. Annu Rev Neurosci. 2008;31:175–93.
Szabo P, Relkin N, Weksler ME. Natural human antibodies to amyloid β peptide. Autoimmun Rev. 2008;7:415–20.
O'Nuallain B, Acero L, Williams AD, Koeppen HP, Weber A, Schwarz HP, et al. Human plasma contains cross-reactive Aβ conformer-specific IgG antibodies. Biochemistry. 2008;47:12254–6.
Taguchi H, Planque S, Nishiyama Y, Szabo P, Weksler ME, Friedland RP, et al. Catalytic antibodies to amyloid β peptide in defense against Alzheimer’s disease. Autoimmun Rev. 2008;7:391–7.
Taguchi H, Planque S, Nishiyama Y, Symersky J, Boivin S, Szabo P, et al. Autoantibody-catalyzed hydrolysis of amyloid β peptide. J Biol Chem. 2008;283:4714–22.
Qahwash IM, Boire A, Lanning J, Krausz T, Pytel P, Meredith SC. Site-specific effects of peptide lipidation on β-amyloid aggregation and cytotoxicity. J Biol Chem. 2007;282:36987–97.
Munch G, Mayer S, Michaelis J, Hipkiss AR, Riederer P, Muller R, et al. Influence of advanced glycation end-products and AGE-inhibitors on nucleation-dependent polymerization of β-amyloid peptide. Biochim Biophys Acta. 1997;1360:17–29.
Adekar SP, Klyubin I, Macy S, Rowan MJ, Solomon A, Dessain SK, et al. Inherent anti-amyloidogenic activity of human Ig γ heavy chains. J Biol Chem. 2009. doi:10.1074/jbc.M109.044321.
Silverman GJ, Goodyear CS. Confounding B-cell defenses: lessons from a staphylococcal superantigen. Nat Rev Immunol. 2006;6:465–75.
Paul S, Planque S, Zhou YX, Taguchi H, Bhatia G, Karle S, et al. Specific HIV gp120-cleaving antibodies induced by covalently reactive analog of gp120. J Biol Chem. 2003;278:20429–35.
Durova OM, Vorobiev II, Smirnov IV, Reshetnyak AV, Telegin GB, Shamborant OG, et al. Strategies for induction of catalytic antibodies toward HIV-1 glycoprotein gp120 in autoimmune prone mice. Mol Immunol. 2009;47:87–95.
Li Q, Gordon M, Cao C, Ugen K, Morgan D. Improvement of a low pH antigen-antibody dissociation procedure for ELISA measurement of circulating anti-Aβ antibodies. BMC Neurosci. 2007;8:22.
Mruthinti S, Buccafusco JJ, Hill WD, Waller JL, Jackson TW, Zamrini EY, et al. Autoimmunity in Alzheimer’s disease: increased levels of circulating IgGs binding Aβ and RAGE peptides. Neurobiol Aging. 2004;25:1023–32.
Weksler ME, Relkin N, Turkenich R, LaRusse S, Zhou L, Szabo P. Patients with Alzheimer’s disease have lower levels of serum anti-amyloid peptide antibodies than healthy elderly individuals. Exp Gerontol. 2002;37:943–8.
Istrin G, Bosis E, Solomon B. Intravenous immunoglobulin enhances the clearance of fibrillar amyloid-beta peptide. J Neurosci Res. 2006;84:434–43.
Relkin NR, Szabo P, Adamiak B, Burgut T, Monthe C, Lent RW, et al. 18-Month study of intravenous immunoglobulin for treatment of mild Alzheimer’s disease. Neurobiol Aging. 2009;30:1728–36.
Bacher M, Depboylu C, Du Y, Noelker C, Oertel WH, Behr T, et al. Peripheral and central biodistribution of (111)In-labeled anti-β-amyloid autoantibodies in a transgenic mouse model of Alzheimer’s disease. Neurosci Lett. 2009;449:240–5.
Mitsuda Y, Planque S, Hara M, Kyle R, Taguchi H, Nishiyama Y, et al. Naturally occurring catalytic antibodies: evidence for preferred development of the catalytic function in IgA class antibodies. Mol Biotechnol. 2007;36:113–22.
Taguchi H, Planque S, Sapparapu G, Boivin S, Hara M, Nishiyama Y, et al. Exceptional amyloid β peptide hydrolyzing activity of nonphysiological immunoglobulin variable domain scaffolds. J Biol Chem. 2008;283:36724–33.
St-Amour I, Laroche A, Bazin R, Lemieux R. Activation of cryptic IgG reactive with BAFF, amyloid β peptide and GM-CSF during the industrial fractionation of human plasma into therapeutic intravenous immunoglobulins. Clin Immunol. 2009;133:52–60.
Asuni AA, Boutajangout A, Quartermain D, Sigurdsson EM. Immunotherapy targeting pathological tau conformers in a tangle mouse model reduces brain pathology with associated functional improvements. J Neurosci. 2007;27:9115–29.
Lacroix-Desmazes S, Bayry J, Kaveri SV, Hayon-Sonsino D, Thorenoor N, Charpentier J, et al. High levels of catalytic antibodies correlate with favorable outcome in sepsis. Proc Natl Acad Sci USA. 2005;102:4109–13.
Acknowledgments
This work was supported by the US National Institutes of Health (1R01AG025304). We thank the co-authors listed in our previous publications for their collaborations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Paul, S., Planque, S. & Nishiyama, Y. Immunological Origin and Functional Properties of Catalytic Autoantibodies to Amyloid β Peptide. J Clin Immunol 30 (Suppl 1), 43–49 (2010). https://doi.org/10.1007/s10875-010-9414-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-010-9414-5