Abstract
Several dental implants are commercially available and new prototype design are constantly being fabricated. Nevertheless, it is still unclear what parameters of the design affect most the osseointegration of dental implants. The purpose of this study is to assess the effects of the microscopic and macroscopic design of dental implants in the osseointegration by comparing three macroscopic designs (Straumann tissue level (STD), essential cone (ECD) and prototype design (PD)) and six surface treatments. A total of 96 implants were placed in 12 minipigs. The implant stability quotient (ISQ), was assessed at the time of implantation, as well as at 2, 4 and 8 weeks. Histomorphometric and statistical analyses were conducted at the different sacrifice times, being 2, 4 and 8 weeks, to analyse the bone to implant contact (BIC), the bone area density (BAT) and the density of bone outside the thread region (ROI). The macroscopic design results showed higher ISQ values for the ECD, whereas the histomorphometric analysis showed higher ossoeintegration values for the STD. Regarding the microscopic design, both Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) and Shot-blasted or bombarded with alumina particles and posterior alkaline immersion and thermal treatment (ContacTi) showed superior results in terms of osseointegration and reduced the osseointegration times from 8 weeks to 4 weeks compared to the other analysed surfaces. In conclusion, each of the macroscopic and microscopic designs need to be taken into account when designing novel dental implants to enhance the osseointegration process.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
One of the most influential factors in implant osseointegration is the morphology and surface of the implant. Nowadays, research is striving to design dental implants that achieve the highest percentage of bone to implant contact (BIC) and an optimised distribution of stresses under applied loads [1]. On the one hand, the macrodesign of the dental implant is designed to transfer the applied load in a homogenous manner and hence reduce bone resorption, and is in charge as well of offering a high surface area in contact with the host bone. On the other hand, the microdesign of the implant, which refers to the surface morphology of the implant, is in charge of offering an increased specific surface area by presenting cavities and pits that allow bone to grow within these pores of tens of microns and hence enhance the osseointegration [2].
Regarding the macroscopic design, there are several features that define the threads and it has become of great importance controlling each of the features to design an optimised implant. For instance, the apical face angle, which is the angle formed between the most apical angle of the thread and the perpendicular plane to the axial axis of the implant itself has been vastly studied in previous works and has been shown to have greatest influence in dispersing the forces to the highest extent. Furthermore, as deduced from the structure, as the apical face angle becomes smaller, the placement of the dental implant is highly favoured. Along with the apical face angle, previous studies regarding the thread pitch, which refers to the distance between adjacent threads, previously showed that the dental implant presenting higher thread pitch increased the stability. The enhanced stability in the presence of bigger thread pitches allows decreasing the implant size. Other parameters, such as the shape of the thread or the apex width also play a pivotal role in ensuring an optimal integration with the host bone [3].
Besides the overall morphology of the implant, the surface of the implant plays a key role at the cellular level. Cellular interactions are mediated by the initial cell adhesion to the surface, which are regulated by the topographical and physicochemical features. In general, increased surface roughness have been shown to lead to higher protein adsorption and hence allow increased cellular interactions [4]. Surface properties of the implant hence play a decisive role in the short term and have a significant role in the final osseointegration, therefore it is considered as an important feature to take into account when designing dental implants [5]. Sandblasted implants are achieved by blasting surfaces with small particles (TiO2, SiO2,Al2O3, etc). The resulting surface topography is usually anisotropic consisting of craters and ridges. By developing moderately rough surfaces through sandblasting and acid etching, the surface results in uniform roughness with pits and craters of micrometric size, which increase the surface area. Previous works have shown a faster osseointegration of dental implants of high surface area, characterised by the formation of new bone, which results in more predictable immediate and early loading procedures [6, 7].
The first bioactive surface to be created was called SLActive (Institut Straumann AG, Basel, Switzerland). It is a modified version of the classic surface obtained by sandblasting and acid etching (SLA - Institut Straumann AG, Basel, Switzerland), which was introduced in a nitrogen atmosphere to avoid contamination of the passive elements in the air. It was then stored in an isotonic saline solution. By doing this, scientists were able to change the surface tension, obtaining more negatively surface energy and a higher wettability. This surface has shown excellent clinical results in both clinical and experimental studies compared to its predecessor [8, 9].
Coating the implant surface with a layer of CaP (Carbonite-containing apatite) to achieve bioactivity has attracted much interest from researchers, who have demonstrated that it accelerates early bone healing and bone bonding due to its rapid protein absorption and the osteoconductivity of the implant. The technique described by Kokubo in 1996 led to the surface development called ContacTi (Klockner Implant System. SOADCO, Andorra). The technique consists of an alkaline immersion process, a thermal treatment followed by a biomimetic treatment consisting of an immersion in simulated body fluid. By doing this, the titanium surface is coated with a layer of apatite that interacts with the underlying bone accelerating the osseointegration process. The ContacTi surface was obtained from a two-step surface treatment. The surface was shot-blasted or bombarded with alumina particles (Al2O3), which provided an optimum microroughness for adhesion, proliferation and differentiation of human osteoblastic cells, and then given a subsequent treatment (alkaline immersion and thermal treatment). The metal surface changes with the thermochemical process, which transforms from bioinert to bioactive, provided by the formation of a dense and amorphous sodium titanate gel. The surface acquires bioactivity and demonstrates in vitro the formation of a layer of hydroxyapatite by crystallisation when introduced in a simulated body fluid [10].
Given the importance of the morphology of implants and their surfaces, we believe there is justification to test these different morphologies and surfaces given that they can have a positive effect on healing an analyse the predominant feature on the final osseointegration process. Hence, the purpose of the study is to assess the influence of microscopic and macroscopic implant design on osseointegration.
2 Material and methods
2.1 Implant description
The study was designed to assess the influence of different implant surfaces and morphologies on bone healing. Eight implants with different morphologies and surfaces were used as described in Table 1.
2.1.1 Macro design
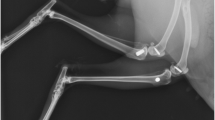
In order to assess the effect of the overall morphology on the bone healing ability, the studied morphologies were the Straumann tissue level, Klockner essential cone and implant prototype. The macrodesign of the Straumann tissue level implant—with its parallel-walls—features an 18° V-shaped thread with a 1.25 mm thread pitch and a 0.1 mm apex width. The morphology of the essential cone implant is characterised for being a conical implant with a 45° V-shaped thread, a 2.2 mm thread pitch with two inputs to increase the insertion speed and apex width of 0.21 mm. The morphology of the prototype implant is similar to the Klockner essential cone implant but differs in a 2-tenth reduction in the implant core, a sharper thread and the apex width is 0.12 mm (Fig. 1). The different implant morphologies were compared presenting the same surface treatment, which was the Shotblasting (Shot-blasted surface with alumina particles and acid attack with hydrochloric acid).
2.1.2 Microdesign
The different studied surfaces were the SLA, (Sandblasted surface plus acid etched) (Sa/roughness 0.96 ± 0.07), SLActive (Sandblasted surface plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere) (Sa/roughness 1.69 ± 0.03) [11], Shotblasting (Shot-blasted surface with alumina oxide plus acid passivation) (Sa/roughness 3.1 ± 0.4), ContacTi (shot-blasted or bombarded surface with alumina particles (Al2O3) and posterior alkaline immersion and thermal treatment) (Sa/roughness 3.5 ± 0.3) [12], Test surface 1 (sandblasted surface plus acid attack) (Sa/roughness 2.30 ± 0.18), Test surface 2 (sandblasted surface plus acid attack in a argon environment) (Sa/roughness 2.67 ± 0.39).
Roughness was evaluated for the test surfaces in the framework of the recommendations by Wennerberg and Albrektsson [13] on topographic evaluation for dental implants. A white light interferometer microscopy (Wyko NT1100, Veeco) was used. The surface analysis area was 459.9 × 604.4 µm2 for all the microrough surfaces. Data analysis was performed with Wyko Vision 232TM software (Veeco, USA). A Gaussian filter was used to separate waviness and form from the roughness of the surface. Cutoff values, λc = 0.8 mm, for microrough surfaces were applied. The measurements were made in three different surfaces of each type of surface treatment to characterise the Ra (the average roughness), which is the arithmetic average of the absolute values of the distance of all points of the profile to the mean line.
2.2 Animal surgery
The study was performed in a reduced number of animals [8,9,10,11,12,13,14]. Twelve 6-year-old female minipigs provided by the University of Córdoba, Centralised Experimental Animals Service, Rabanales Campus with cattle farms registration number ES14021000000933 authorised in favour of Mr Nahúm Ayala and Mr Ríos-Santos, project number 20-08-15-293 with the approval of the Ethics Committee of the Junta de Andalucía were used. All the requirements for animal testing were met, in compliance with the regulations in force in Spain and the European Union.
Animals were fed a diet of powdered and liquid food throughout the study, undergoing oral prophylaxis using an aseptic technique 3 weeks before the experimental surgeries. The feeding of the animals was suspended the night before the surgery. The animals were pre-anaesthetised with xylazine hydrochloride and ketamine, and maintained on gas anaesthesia (Isoflurane at 5%-oxygen). They were kept hydrated during surgery by administering Ringer Lactate’s solution intravenously. The animal’s heart and breathing rates were also monitored. Instructions recommended by the manufacturers were followed at all time for implant insertion.
The study consisted of two surgical procedures, performed on maxillas of the minipigs. The 12 minipigs were randomly divided into three groups, placing eight implants in the maxillas of each pig, one of each type.
2.2.1 First surgical procedure
During the first surgery, the posterior teeth of the maxilla, bicuspids and molars were carefully extracted under general anaesthesia, by making an incision in the premolar and molar regions in both maxillary sides. At least 6-months healing was allowed in order to achieve a fully mature alveolar crest in this area of the maxilla and to ensure complete healing of the places from where the teeth had been extracted. The area was closed by primary intention with interrupted dermal sutures using synthetic polyamide (Supramid® 4-0). After the surgery was completed, buprenorphine hydrochloride was administered for pain control and amoxicillin to prevent infection. Animals were continuously monitored to prevent oedema formation, wound dehiscence and infection.
2.2.2 Second surgical procedure
After these 6 months of healing, eight implants (one of each group) were randomly placed in the maxilla of each pig, which had previously had all their teeth removed in the first surgical procedure. The implants were placed following the manufacturer’s recommendations, namely, the submerged technique, being completely covered by the skin. At the end of the preparations, the depth was checked to ensure that the polished neck was placed supracrestal and that the separation between them was at least 4 mm. Closing taps were placed on the implants and after irrigating them with sterile saline solution, the area was closed by primary intention with interrupted dermal sutures using synthetic polyamide (Supramid® 4-0). After the surgery was completed, buprenorphine hydrochloride and amoxicillin were administered, followed by a continuous monitoring as previously described.
2.3 Animal sacrifice
At the specified time points, animal sacrifice was performed by an overdose of sodium pentothal in perfusion through the carotid arteries. This solution also contained a mixture composed of glutaraldehyde at 5% and formaldehyde at 4% at a pH of 7.2. Each group was sacrificed at a different time point from the second surgery, being 2, 4, and 8 weeks, respectively.
2.4 Analysis of in vivo results
Once the implants were placed, the implant stability quotient (ISQ) was measured by means of resonance frequency analysis (RFA) using the Osstell ISQ® (Gothenburg, Sweden) according to the manufacturer’s indications. Similarly, RFA measurements of the implants were recorded at the time of sacrifice.
In order to carry out the analysis, block sections—including the implant, alveolar bone and mucous membrane—were obtained from each animal. The maxillae under study were cut using an Exakt 310® (Exact Vertriebs, Norderstedt, Germany) oscillating saw to delimit the implant and the surrounding bone with a thickness of no more than 4 mm to ensure a correct posterior fixation. Samples were then immersed in 10% buffered formalin solution for at least 2 weeks prior to processing.
Once the samples were fixed with formalin, samples were dehydrated in graded ethanol solutions (70%, 80%, 96% and 100%). The dehydrated samples were infiltrated and embedded in methyl methacrylate (MMA) resin (Technovit 7200 VLC, Kulzer-Heraus, Germany). Each polymerised block was cut in the axial direction of the implant with a diamond band saw to avoid overheating and deteriorating the tissues surrounding the implant. All sections were polished with the automatic polishing machine (Exakt 400 CS, Exakt, Germany).
The polished cuts were examined under scanning electron microscope (SEM, JSM-6400, Jeol, Japan) using scattered retro electrons to further differentiate the bone from the surface. Images at different magnifications were obtained. The histological study was carried out in such a way that the histopathologist in charge of the histomorphometric study was unaware of the sample type in each animal being assessed. Three main parameters were then analysed:
-
BIC: The percentage of direct contact between the mineralised bone and the titanium surface (Bone–implant contact).
-
BAT: The area of mineralised bone relative to the total tissue in the area between two threads.
-
ROI: Density of the bone in the outer area delimited by the beginning of the implant threads and one millimetre depth.
2.5 Statistical analysis
The statistical analysis was carried out by the Statistics Department of the Faculty of Dentistry, University of Seville, using the IBM SPSS 24.0 statistical package for Windows. Mean values and standard deviations were calculated globally and by groups (surface area, surface area of each moment, etc…)
A two-factor ANOVA was applied to compare numerical variables between the groups. When these tests were significant, multiple comparisons tests (Bonferroni) were used to detect the groups that differed and to obtain confidence intervals at 95% to quantify these differences. The significance of the differences was established for p < 0.05.
3 Results
A total of 96 implants were placed in the maxillae of 12 minipigs. The BIC, BAT, ROI and the ISQ evolution were analysed after 2, 4 and 8 weeks. The histological and histomorphometric analyses revealed that the samples showed a normal macroscopic anatomy for all time points and conditions studied. On the day of the necropsy, normal bone tissue was observed in contact with all implants, with no swelling, oedema, fibrosis or mobility around them or any other complication. No changes in tissue morphology were observed, as well as no signs of increased inflammatory cell count or necrosis. Clinically speaking, the implants appeared to have osseointegrated, which was then followed by the sample processing steps.
3.1 Macro design
Initially, we assessed the macroscopic implant design on the osseointegration outcome. According to the ISQ values at 2, 4 and 8 weeks (Table 2), the different implants presented similar values at the time of surgery, not presenting significant differences among them. This trend continued in a similar way after 2 and 4 weeks time point, although at 8 weeks the ECD presented higher values than the STD. Nevertheless, there were no significant differences among the different groups. Regarding the histomorphometric analysis at the same time points, the results were slightly different. The BIC values, as shown in Table 3, were relatively low and not significantly different between them at 2 and 4 weeks time points, but became significantly different at 8 weeks, where the STD presented significant differences with PD and ECD (p < 0.05), although no significant differences were found between PD and ECD. Similar trend was observed for the BAT, where only the differences were significant at 8 weeks, having the STD presenting significantly higher values than the ECD (p < 0.05), whereas no significant differences were found between the PD and the other two groups. Finally, the ROI values followed as well a similar trend, presenting similar values at 2, 4 and 8 weeks for the different groups, not presenting significant differences among them at the different time points. Overall the results show that the implant morphology may present a significant effect on osseotintegration.
3.2 Micro design
We then assessed the effect of the surface morphology on the different variables. Initially, we assessed the differences between the shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) and the well-known surfaces used by Straumann, the Sandblasted plus acid etched surface (SLA) and the Sandblasted plus acid etching (hydrochloric/sulphuric acid)in a nitrogen atmosphere (SLActive). In terms of ISQ values (Table 4), both the Sandblasted plus acid etched surface (SLA) and the Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) performed in an ulterior manner, presenting higher values at all-time points. Both presented significantly higher values compared to the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shtoblasting) at 4 and 8 weeks (p < 0.05). Regarding the histomorphometric analysis, as shown in Table 5, the BIC values were shown to be similar at 2 weeks between the different groups, although these values became significantly higher at 4 weeks for the Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) compared to the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) (p < 0.05). At 8 weeks, Sandblasted plus acid etched surface (SLA) and Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) did not significantly increase their values, whereas the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid, (Shotblasting) surface significantly increased the values, not presenting significant differences among the three of them. The BAT values showed predominant values at all-time points for the Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive), although the values were not significantly higher at any time point. Finally, the ROI values presented similar trend in all cases not showing significant differences among them. The results therefore prove the higher performance of the Sandblasted plus acid etched surface (SLA) and Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere surface (SLActive), compared to the Shot-blasted surfaces with alumina particles and acid attack with hydrochloric acid (Shotblasting).
We then finally assessed the differences between the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) surfaces and the new ContacTi surface proposed by Klockner (Shot-blasted or bombarded with alumina particles and posterior alkaline immersion and thermal treatment), as well as two new prototype designed surfaces. The ISQ values (Table 6) generally showed similar values from the time of implantation to the values recorded at 8 weeks, being during all the time points in values between 70 and 75, not showing significant differences among the different groups. Regarding the histomorphometric analysis, as shown in Table 7, the BIC values at 2 weeks presented in general low values, presenting significantly lower values between the Sandblasted plus acid attack (test surface 1) and the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) (p < 0.05). At 4 weeks, the Shot-blasted or bombarded surface with alumina particles and posterior alkaline immersion and thermal treatment (ContacTi) values significantly increased up to 83.2, presenting significantly higher values compared to the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) and the Sandblasted plus acid attack (test surface 1) (p < 0.05). Finally, at 8 weeks the values generally increased, not presenting significant differences among the different surfaces. The BAT analysis revealed a similar pattern, showing in general a higher value for the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) and the Sandblasted surface with alumina oxide plus acid attack (hydrochloric/sulphuric acid) in argon environment (Test surface 2), without any significant differences among the groups. At 4 weeks, the Shot-blasted or bombarded surface with alumina particles and posterior alkaline immersion and thermal treatment (ContacTi) performed in an enhanced manner, although not showing significant differences with other surfaces. Finally, at 8 weeks, all values were in the range of 55% without presenting significant differences among them. Finally, the ROI values showed initially better results for the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) and the Sandblasted surface with alumina oxide plus acid attack (hydrochloric/sulphuric acid) in argon environment (Test surface 2), without significantly higher values. At 4 and 8 weeks, the values were similar among the different groups, not showing significant differences among the different groups.
4 Discussion
Several histomorphometric studies have been performed in animal models to assess the behaviour of new surfaces with regard to peri-implant bone healing. In order to improve and stimulate the bone surrounding the implant and achieve better osseointegration, we analysed implants with different macroscopic morphology as well as different surface morphology. We expected that the different overall morphology and the different surface morphology could contribute to a better interaction with the surrounding bone and hence enhance the osseointegration. By unravelling the effect of the surface morphology and the macroscopic design, we envisage better implant designs for future new dental implants.
Regarding the macroscopic design, we compared three morphologies, mainly the Straumann tissue level, Klockner essential cone and a prototype design similar to the Klockner essential cone design having a common surface morphology in all cases. Overall, the thread pitch, the angle between the thread and the type of thread, were shown to influence the final outcome of the osseointegration process. The macrodesign of the Straumann tissue level implant—with its parallel-walls—features an 18° V-shaped thread with a 1.25 mm thread pitch and a 0.1 mm apex width. The morphology of the essential cone implant is characterised for being a conical implant with a 45° V-shaped thread, a 2.2 mm thread pitch with two inputs to increase the insertion speed and apex width of 0.21 mm. The morphology of the prototype implant is similar to the Klockner essential cone implant but differs in a 2-tenth reduction in the implant core, a sharper thread and the apex width is 0.12 mm (Fig. 1). Our hypothesis was that smaller angles allow better insertion of the implant hence reducing the tension concentration, which can negatively contribute to new bone formation [15].
In general, our results showed that the ISQ values tended to increase with the essential cone implant, especially at 8 weeks time point. The results showed a higher stability as the angle became higher, allowing a better fixation with the bone surface. Nevertheless, the histomorphometric results were shown to present an opposite trend, having the lowest values of BIC, BAT and ROI for the essential cone implant. This was probably due to a higher surface area in contact between the bone and the implant, which enhanced the formation of the new bone. Vivan Cardoso et al. [16]. carried out a study to assess the influence of implant morphology in relation to BIC along the surface, neck and body of the implant comparing AadvaTM implants (GC, Tokyo, Japan) and OsseoSpeedTM implants (Astra, Mölndal, Sweden), placed in the trabecular parietal bones of minipigs with a healing period of 1 and 3 months. The Aadva implant had a thread angle of approximately 100° at the top of the implant and 120° at the bottom, whereas the OsseoSpeed is characterised by a uniform thread and an angle of 83°. At one month of osseointegration, the OsseoSpeed implants yielded significant differences, as well as a higher degree of osseointegration after the 3-month healing period. These results, despite presenting significantly higher angles than in our study, were in accordance with our results, showing that smaller angles yielded higher osseointegration results.
Besides from the angle, an interesting aspect to be considered in the design is the shape of the threats. It has been previously demonstrated that the shape plays an important role in the stress transferred between the implant and the surrounding tissues, which determines the primary stability of the implant; hence the implant morphology that maximised the contact area between the implant and the bone is desired [17]. In the present study, the different morphologies were all V-shaped, although the Straumann implant presents smaller sized threats, which increases the contact area. An interesting aspect was the considerable difference between the essential cone implant and the prototype implant, showing higher histomorpometric values for the prototype design. This could be ascribed to the smaller threads, which again enhanced the contact area with bone and induced a higher bone formation on the surface. Previous studies developed by finite element showed that the V loops and reverse buttress present optimised morphologies [18, 19].
Another important aspect of the implant design is the thread pitch, which is the distance, measured parallel to the axis of the implant, between the adjacent threads. Implant designs that present small thread pitch allow incorporating more shapes for a unit of length and hence increase the surface area in contact between the surrounding tissue and the implant. In the present study, the thread pitch for the Straumman implants was 1.25 mm and for the Klockner implants the thread pitch was 2.2 mm. In general, the Straumman implants performed better in terms of amount of calcified bone formed, showing that smaller thread pitch obtained better results. Orsini et al. [20] conducted an animal study placing “narrow-pitch” (0.5 mm) and “wide-pitch” (1.7 mm implants in a sheep iliac crest model). The findings suggested that initial mechanical anchorage and subsequent early endosseous bone formation were improved in the lower thread pitch implants. The greater surface area gained by decreasing thread pitch increased bone–implant contact and primary stability from the time of implant placement. Another animal study performed by Chung et al. [21] also revealed that implants with a 0.6-mm pitch created more crestal bone resorption than those with a 0.5-mm pitch. Hence the macroscopic design has been shown to reveal important considerations in the overall implant design.
As far as the morphology is concerned, the Straumann morphology has attained better results, despite it is important to analyse each of the morphological parameters independently to understand and optimise the implant morphology. Furthermore, its combination with specific surface morphologies renders synergistic effects, which may enhance even more the osseointegration behaviour.
Regarding the surface morphology, in recent years attempts have been made to improve bone apposition by increasing surface micro-roughness or by improving its chemical interaction with the early stages of bone consolidation. Applying techniques such as acid etching, sandblasting, oxidation or coatings, among others, and their combinations, have shown an improvement in osseointegration compared to untreated smooth implants [22, 23].
The surface of dental implants can be modified by adapting several parameters, such as wettability, chemical composition, zeta potential, texture or topography, which have a direct effect on cell adhesion, proliferation and differentiation. In fact, these cellular processes are of crucial importance, where the characteristics of the surface are essential to obtain a determined cellular response at the bone–implant interface, directly affecting the growth and quality of the formed bone [7, 24]. In general, the presence of a rough surface is known to enhance the amount of new bone formed, since the rough surface is less prone to the remodelling activity during the initial stages after implant placement [25].
In the present study, we initially aimed at comparing the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) morphology with the well-known Sandblasted plus acid etched surface (SLA) and Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive). We then aimed at comparing the Shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) with novel surfaces such as the Shot-blasted or bombarded surface with alumina particles and posterior alkaline immersion and thermal treatment (ContacTi), and two different test surfaces (Sandblasted plus acid attack-test surface 1 and the sandblasted surface with alumina oxide plus acid attack (hydrochloric/sulphuric acid) in argon environment-test surface 2). Overall, the stability and the histomorphometric results showed a superior behaviour of the Sandblasted plus acid etched surface (SLA) and Sandblasted plus acid etching (hydrochloric/sulphuric acid)in a nitrogen atmosphere (SLActive) compared to the shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) implants. Both Sandblasted plus acid etched surface (SLA) and Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) exhibited a similar behaviour throughout the 8 weeks period. Previous results showed similar trend in which Sandblasted plus acid etched surface (SLA) and Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) attained similar results although authors claimed the overall superiority of the SLActive [26,27,28]. In fact, Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) has been considered to perform even better than implants that presented a nanometre sized calcium phosphate deposition [29]. The results of the Shot-blasted or bombarded surface with alumina particles and posterior alkaline immersion and thermal treatment (ContactTi) were similar to those of the Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive), presenting significantly higher values compared to the shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting). Therefore, in general terms the Shot-blasted or bombarded surface with alumina particles and posterior alkaline inmersion and thermal treatment (ContactTi), presented similar results to the Sandblasted plus acid etched surface (SLA) and Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere surface (SLActive). It is important to highlight, that Sandblasted plus acid etched surface (SLA), Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere surface (SLActive) and Shot-blasted or bombarded surface with alumina particles and posterior alkaline immersion and thermal treatment (ContactTi), obtained higher values of BIC at shorter times. Hence, the results demonstrated that these types of implants are able to enhance the osseointegration and new bone formation at early times of implantation (e.g., 4 weeks), whereas a longer time points (e.g., 8 weeks) these performed similarly to other tested surfaces [30,31,32]. The formation of an apatite layer on the surface of the implant has been shown to be the key aspect controlling the enhanced osseointegration. Despite Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) and Shot-blasted or bombarded surface with alumina particles and posterior alkaline inmersion and thermal treatment (ContactTi), induce the apatite formation in different manners, in both cases the deposited apatite layer has been shown to play the pivotal role in the final result [33, 34].
We then compared the Shot-blasted or bombarded surface with alumina particles and posterior alkaline inmersion and thermal treatment (ContacTi), with the new potential surfaces, surface test 1 (sandblasted with alumina oxide and HCl attack) and surface test 2 (sandblasted with alumina oxide and acid attack in argon environment). To some extent, these surfaces could resemble the Sandblasted plus acid etched surface (SLA) and Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive), presenting a more hydrophilic surface due to the presence of inert gas that would reduce the oxidation on the surface. The results were shown to be in general terms slightly better for the surface produced under the argon environment although differences were not significant. The main difference resides in the double acid etching performed on the test surface 2, which has been previously shown to enhance the bioactivity and hence the osseointegration [33]. Similarly to the Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive), the inert atmosphere rendered a better control on the formation of an oxide surface reducing the hydrocarbon contamination [4]. This could probably be ascribed to the formation of cavities in the range of tens of microns due to the sandblasting, followed by the double acid etching, which was able to create the smaller pits. Finally, the formation of a hydrophilic surface allowed the enhanced osseointegration compared to the sandblasted plus acid attack (test surface 1). Further experiments are needed to deeply characterise the new test surfaces and understand their interactions at the in vitro level.
Overall, the different surface morphologies have clearly showed the enhanced performance of the Sandblasted plus acid etching (hydrochloric/sulphuric acid) in a nitrogen atmosphere (SLActive) and the novel Shot-blasted or bombarded surface with alumina particles and posterior alkaline immersion and thermal treatment (ContacTi), surface compared with the shot-blasted surface with alumina particles and acid attack with hydrochloric acid (Shotblasting) and the newly designed surfaces, showing the importance of controlling, not only the surface roughness, but also the chemical functional groups exposed on the surface of the dental implant.
5 Conclusions
All the surfaces studied were biocompatible, and a natural healing pathway was observed, regardless of the implant surface in all histological sections. Regarding the macrodesign of the implant, the essential cone implant attained a better stability although the amount of newly bone formed was higher for the Straumann tissue level implant, demonstrating the need to still find optimum implant macrodesign. Furthermore, each of the components of the dental implant need to be taken into account to design the optimised design. Regarding the surface treatments, both SLActive and ContacTi, demonstrated similar stages in bone healing and remodelling, with dense and mature bone. To date, very encouraging results have been achieved with the ContacTi surface, but randomised clinical trials are needed in order to validate them in humans under functional loads. The seek and understanding of biological responses and the development of surface treatments, as well as implant morphology in order to achieve dental implants with the best and fastest osseointegration possible still needs further research.
References
Huang HL, Chang CH, Hsu JT, Fallgatter AM, Ko CC. Comparison of implant designs and threaded designs of dental implants: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2007;22:551–62.
Steigenga JT, Al- Shamamari KF, Nociti FH, Mish CE, Wang HL. Dental implant design and it’s relationship to long term implant success. Implant Dent. 2003;12:306–17.
Strong JT, Misch CE, Bidez MW, Nalluri P. Functional surface area: thread- form parameter optimization for implant body design. Compend Contin Clin Educ Dent. 1998;19:4–9.
Buser D, Broggini N, Wieland M, Schenk RK, Denzer AJ, Cochran DL, Hoffmann B, Lussi A, Steinemann SG. Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res. 2004;83:529–33.
Pazos L, Corengia P, Svoboda H. Effect of surface treatments on the fatigue life of titanium for biomedical applications. J Mech Behav Biomed Mater. 2010;3:416–24.
Lincks J, Boyan BD, Blanchard CR, Lohmann CH, Liu Y, Cochran DL, Dean DD, Schwartz Z. Response of MG63 osteoblast-like cells to titanium and titanium alloy is dependent on surface roughness and composition. Biomaterials. 1998;19:2219–32.
Aparicio C, Gil FJ, Fonseca C, Barbosa M, Planell JA. Corrosion behaviour of commercially pure titanium shot blasted with different materials and sizes of shot blasted with different materials and sizes of shot particles for dental implant applications. Biomaterials. 2003;24:263–73.
Buser D, Nydegger T, Oxland T, Cochran DL, Schenk RK, Hirt HP, Snetivy D, Nolte LP. Interface shear strength of titanium implants with a sand-blasting and acid-etched surface. A biomechanical study in the maxilla of miniature pigs. J Biomed Mater Res. 1999;45:75–83.
Gottlow J, Barkarmo S, Sennerby L. An experimental comparison of two different clinically used implant designs and surfaces. Clin Implant Dent Relat Res. 2012;14(Suppl 1):e204–12.
Manero JM, Salsench J, Noqueras J, Aparicio C, Padrós A, Balcells M, Gil FJ, Planell JA. Growth of bioactive surfaces on dental implants. Implant Dent. 2002;11:170–5.
Kournetas N, Spintzyk S, Schweizer E, Sawada T, Said F, Schmid P, Geis-Gerstorfer J, Eliades G, Rupp F. Comparative evaluation of topographical data of dental implant surfaces applying optical interferometry and scanning electron microscopy. Dent Mater. 2017;33:e317–27.
Herrero-Climent M, Romero Ruiz MM, Calvo PL, Santos JVR, Perez RA, Gil Mur FJ. Effectiveness of a new dental implant bioactive surface: histological and histomorphometric comparative study in minipigs. Clin Oral Invest. 2017;22:1423–32. https://doi.org/10.1007/s00784-017-2223-y. [epub ahead of print]
Wenneberg A, Albrektsson T. Suggested guidelines for the topographic evaluation of implant surfaces. Int J Oral Maxillofac Implants. 2000;15:331–44.
Germanier Y, Tosatti S, Broggini N, Textor M, Buser D. Enhanced bone apposition around biofunctionalized sandblasted and acid-etched titanium implant surfaces. A histomorphometric study in miniature pigs. Clin Oral Implants Res. 2006;17:251–7.
Ryu HS, Namgung C, Lee JH, Lim YJ. The influence of thread geometry on implant osseointegration under immediate loading: a literature review. J Adv Prosthodont. 2014;6:547–54.
Vivan Cardoso M, Vandamme K, Chaudhari A, De Rycker J, Van Meerbeek B, Naert I, Duyck J. Dental implant macro-design features can impact the dynamics of osseointegration. Clin Implant Dent Relat Res. 2015;17:639–45.
Ivanoff CJ, Gröndahl K, Sennerby L, Bergström C, Lekholm U. Influence of variations in implant diameters: a 3- to 5-year retrospective clinical report. Int J Oral Maxillofac Implants. 1999;14:173–80.
Geng JP, Ma QS, Xu W, Tan KB, Liu GR. Finite element analysis of four thread-form configurations in a stepped screw implant. J Oral Rehabil. 2004;31:233–9.
Abuhussein H, Pagni G, Rebaudi A, Wang HL. The effect of thread patter upon implant osseointegration. Clin Oral Implants Res. 2010;21:129–36.
Orsini E, Giavaresi G, Trirè A, Ottani V, Salgarello S. Dental implant thread pitch and its influence on the osseointegration process: an in vivo comparison study. Int J Oral Maxillofac Implants. 2012;27:383–92.
Chun HJ, Cheong SY, Han JH, Heo SJ, Chung JP, Rhyu IC, Choi YC, Baik HK, Ku Y, Kim MH. Evaluation of design parameters of osseointegrated dental implants using finite element analysis. J Oral Rehabil. 2002;29:565–74.
Donath K, Breuner G. A method for the study of undecalcified bones and teeth with attached soft tissues. The Säge-Schliff (sawing and grinding) technique. J Oral Pathol Med. 1982;11:318–26.
Albrektsson T, Wennerberg A. Oral implant surfaces: Part 2-review focusing on clinical knowledge of different surfaces. Int J Prosthodont. 2004;17:544–64.
Deligianni DD, Katsala ND, Koutsoukos PG, Missirlis YF. Effect of surface roughness of hydroxyapatite on human bone marrow cell adhesion, proliferation, differentiation and detachment strength. Biomaterials. 2001;22:87–96.
Suzuki K, Aoki K, Ohya K. Effects of surface roughness of titanium implants on bone remodeling activity of femur in rabbits. Bone Int J Oral Maxillofac Implants. 1997;21:507–14.
Lai H-C, Zhuang L-F, Zhang Z-Y, Wieland M, Liu X. Bone apposition around two different sandblasted, large-grit and acid-etched implant surfaces at sites with coronal circumferential defects: an experimental study in dogs. Clin Oral Implants Res. 2009;20:247–53.
Philipp A, Duncan W, Roos M, Hämmerle CH, Attin T, Schmidlin PR. Comparison of SLA ® or SLActive ® implants placed in the maxillary sinus with or without synthetic bone graft materials-an animal study in sheep. Clin Oral Implants Res. 2014;25:1142–8.
Stafford GL. Review found little difference between sandblasted and acid-etched (SLA) dental implants and modified surface (SLActive) implants. Evid Based Dent. 2014;15:87–8.
Schwarz F, Sager M, Kadelka I, Ferrari D, Becker J. Influence of titanium implant surface characteristics on bone regeneration in dehiscence-type defects: an experimental study in dogs. J Clin Periodontol. 2010;37:466–73.
Lang NP, Salvi GE, Huynh-Ba G, Ivanovski S, Donos N, Bosshardt DD. Early osseointegration to hydrophilic and hydrophobic implant surfaces in humans. Clin Oral Implants Res. 2011;22:349–56.
Bosshardt DD, Salvi GE, Huynh-Ba G, Ivanovski S, Donos N, Lang NP. The role of bone debris in early healing adjacent to hydrophilic and hydrophobic implant surfaces in man. Clin Oral Implants Res. 2011;22:357–64.
Favero V, Lang NP, Favero R, Antunes AA, Salata LA, Botticelli D. Sequential morphometric evaluation at UnicCa(®) and DCD(®) implant surfaces. An experimental study in the dog. Clin Oral Implants Res. 2017;28:833–9.
He FM, Yang GL, Li YN, Wang XX, Zhao SF. Early bone response to sandblasted, dual acid-etched and H2O2/HCl treated titanium implants: an experimental study in the rabbit. Int J Oral Maxillofac Surg. 2009;38:677–81.
Aparicio C, Padrós A, Gil F-J. In vivo evaluation of micro-rough and bioactive titanium dental implants using histometry and pull-out tests. J Mech Behav Biomed Mater. 2011;4:1672–82.
Acknowledgements
This project has been financially supported by two research contracts with SOADCO SL, Project Code 1162 of the Research Foundation of the University of Seville and Straumann, Project Code: 1183 with Working Group Code 0480.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article contains no studies with human participants, and as regards animal testing, the study was sanctioned by the Experimentation Committee of the Junta de Andalucía.
Rights and permissions
About this article
Cite this article
Ríos-Santos, J.V., Menjívar-Galán, A.M., Herrero-Climent, M. et al. Unravelling the effect of macro and microscopic design of dental implants on osseointegration: a randomised clinical study in minipigs. J Mater Sci: Mater Med 29, 99 (2018). https://doi.org/10.1007/s10856-018-6101-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-018-6101-1