Abstract
Duraplasty is necessary in nearly 30% of all neurological surgeries. Different tissues and materials have been evaluated in dura mater repair or as dural substitutes in neurosurgery. The aim was to evaluate the biocompatibility of the bacterial cellulose (BC) membranes, produced from sugarcane molasses, for dural defect repair in rats. Forty adults males Wistar rats divided into two groups: a control (ePTFE) and an experimental (BC). Bilateral frontoparietal craniectomy was performed, and a dural defect was created. The arachnoid underlying defect was disrupted with a narrow hook. The animals were observed for 120 days. There were no cases of infection, cerebrospinal fluid fistulae, delayed hemorrhages, behavior disturbances, seizures and palsies. The BC membrane showed to have suitable biocompatibility properties, was not induced immune reaction, nor chronic inflammatory response and absence of neurotoxicity signals.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Several conditions can promote damage to the dura mater, which can affect human beings at different stages of their existence. At a neurosurgical procedure, an inadequate dural closure exposes patients to cerebrospinal fluid fistula, infections, neural tissue herniation, hypertensive pneumocephalus, pseudomeningocele, and adhesions [1–3].
In everyday neurosurgical practice, numerous autogenic, allogenic, xenogenic, absorbable, and nonabsorbable synthetic materials have been used with varying degrees of success in the search for the perfect dural graft [3–7].
Different tissues and materials have been evaluated in dura mater repair or as dural substitutes in neurosurgery [8]. However, an entirely satisfactory solution still remains to be found, considering reports of side effects from the use of autologous, heterologous or synthetic substances [9–11].
The use of an autologous graft surgical procedure is an additional variable magnitude and the amount of tissue obtained may be insufficient, especially in children [8]. Furthermore, systemic treatment with synthetic materials increases the risk of wound infection when compared to the use of graft autólogo [10]. The need to employ substitutes for dura mater was identified before dawn neurosurgery as a medical specialty.
Important requirements for using biopolymers in the central nervous system are absence of toxicity of the material, suitable hydrophilic properties, ability to be absorbed by the host tissue and that they permit vascularization, especially due to the poor regenerative capabilities of the brain [12]. Bacteria-synthesized polysaccharides have attracted interest for biomedical applications as unique and promising materials to be used as implants and scaffolds, especially in bone, cartilage, and skin tissue engineering [13]. Some studies using bacterial cellulose have also indicated the compatibility of this type of biomaterial for duraplasty [14–17]. Either in the form of neurotubes, facilitating the process of nerve regeneration [18], or in combination with recombinant proteins or other molecules, bacterial cellulose has been used as substrate for neuronal cell lines or mesenchymal stem cells [19].
Recent evidence has shown that cellulose produced from sugarcane molasses by bacterial synthesis [20] is a non-toxic and low cost biomaterial, useful in a number of biomedical applications, as a support for trypsin immobilization [21], sutures [22], bone healing [23, 24], artery and vein prosthesis [25, 26], abdominal wall mesh repair [27, 28]. In these in vivo studies, satisfactory results were obtained, especially considering the ability of this bacterial cellulose to be successfully integration in the different tissues without causing side effects. Recent in vitro assays demonstrated its biocompatibility to support the adhesion and growth of human umbilical cord Wharton’s jelly´s mesenchymal stem cells [29].
Considering the evidence above described, the aims of the present study was to evaluate the biocompatibility of the bacterial cellulose (BC) membranes, produced from sugarcane molasses, for dural defect repair in rats.
2 Materials and methods
2.1 Properties of BC
BC was produced from sugarcane at the Experimental Station of Carpina, Federal Rural University of Pernambuco, Brazil. The sugar cane molasses is the only raw material used for the synthesis of BC. Molasses are adjusted for the ideal brix in order to facilitate the digestion process. Preparations of BC hydrogel acquire viscoelastic properties and remain stable at concentrations of 0.6 and 0.8% at the usual storage temperatures and in biological fluids (0–40 °C) [20].
The BC membranes have produced from the hydrogel to 0.8%. The compact BC membrane with a thickness of 0.2 mm, is manually pressed, during the process of dehydration and air dried. From the compact membrane, if it prepares multiperforated is stamping-holes 16 one millimeter diameter per cm2. BC membranes can be standardized in different thicknesses, widths and lengths. The membranes can be preserved in isopropyl alcohol 80% or dried, packed in surgical grade envelope and sterilized by gamma irradiation.
Biomechanical tests with parameters analysis as traction speed, the maximum breaking strength and the specific deformation maximum strength, showed that multiperforated membrane of the BC was better than compact membrane, but with results similar to expanded polytetrafluoroethylene (ePTFE) [27, 28].
The mechanical properties including maximal loading (N), tensile strength (stress, MPa) and elongation (strain, %) of BC patches (previously moistened with isopropyl alcohol) were measured by conducting a standardized tensile test in a United Universal Mechanical Testing Machine (EMIC, model DL 500 MF) with a gap distance of 2.5 cm and a crosshead speed of 250 mm/min. Stress was calculated as F/A, where F is the loading force and A is the area of the cross section of materials. Strain was calculated considering DL/L, where L is the initial length and DL is the difference between the lengths at break and the initial length.
The samples (n = 10) were cut into test pieces each 2 × 7 cm. A digimatic point micrometer (Mitutoyo Series 342, Japan; Resolution: 0.001 mm; Graduation: 0.01 mm) was used to measure the thickness prior to loading the samples into the testing machine.
2.2 Animals
Male adult Wistar rats (40) with ages ranging from 4 to 6 months and weighing 300–440 g were used. All procedures related to the animal care were performed under veterinary supervision according to the institutional rules of Experimental Surgery Center of the Federal University of Pernambuco. The animals were fed a balanced commercial diet (Labina®), water was available ad libitum and a 12/12 h light/dark cycle (lights on at 6:00 h) was observed.
The animals were divided into two groups according to the material used as dura mater substitute: Group BC (n = 20) was treated with bacterial cellulose membranes and Group e-PTFE (n = 20) with membranes of expanded polytetrafluoroethylene (Preclude Membrane®) donated by W.L. Gore & Associates, Flagstaff, AZ, USA.
All experimental procedures adopted in this study were approved by the Ethics Committee for Animal Research of Federal University of Pernambuco (protocols #23076.000254/2013-72 and 60/05), in accordance with the Brazilian College for Animal Care guidelines which follows the “Principles of Laboratory Animal Care” (NIH, Bethesda, USA).
2.3 Anesthesia and neurosurgery
The rats were systemically anesthetized with Chloral hydrate 10%, (0.4 g/kg; i.p.). Local anesthesia in the region of trepanning was obtained with a subcutaneous injection of 1% lidocaine. Prophylactic antibiotic therapy was done with a single dose of cephalothin sodium (160 mg/kg, i.p.) during anesthesia induction. Before neurosurgery, a trichotomy and asepsis using Povidine-iodine® was performed in both groups, in the region along the incision of scalp and retraction of temporal muscle. Using a trephine of 10 mm diameter coupled to a dentistry drill with very low rotation, a fronto-parietal bilateral craniotomy was performed and subsequently the dura mater was displaced under the bone border. A 0.9 cm defect in dura mater was generated with preservation of the superior longitudinal sinus. In one of the cerebral hemispheres, the arachnoid membrane underlying defect was disrupted with a narrow hook to allow better adherence of the sutureless dural substitute [14].
For each group a circular patch of e-PTFE or BC (14 mm diameter) was placed over the exposed encephalic surface. The piece of bone was discarded, keeping the periosteum in contact with the dural substitutes and the scalp was sutured on two planes: the subcutaneous cellular with Vicryl® sutures and the skin with mononylon along continuous points. All the surgical procedure was performed using a D F Vasconcellos ® FC 250 surgery stereo microscope.
After the surgical procedure the animals were kept in individual cages and the two groups were compared in the postoperative period with respect to behavioral and motor changes, seizures, presence of liquoric fistula, cicatricial process, hematoma or signs of infection. After 120 days, each animal was weighed and re-anesthetized with 10% chloral hydrate. Through a transesternal thoracotomy, the catheterization of the ascending aorta was performed and the inferior vena cava was opened for perfusion of formaldehyde 10% in PBS, pH 7.4. Subsequently, the head was disarticulated and after removal of the skin, it was immersed in a similar solution of fixative for an additional 7 days.
2.4 Histopathological analysis
After fixation, the region of the head where the surgery had been performed was dipped in paraffin wax and coronal sections of 5 μm were taken and stained in hematoxilin-eosin solution. The histopathological analysis was carried out independently by two individuals using a light Microscope (Nikon Eclipse 50i) coupled to a camera (Nikon DS-Fil) at magnifications of 100x and 400x using planachromatic objectives. A double blind approach was adopted where materials of BC or e-PTFE were not identified.
The systematic study was performed to evaluate the qualitative and quantitative responses of the nervous tissue and bone to the BC or e-PTFE grafts. Tissue cellularity in the external and internal surfaces adjacent to the prosthesis was analyzed according to the following criteria: 1, presence of macrophages only; 2, macrophages associated to giant cells; 3, presence of macrophages, giant cells and granuloma. It was also analyzed the ability of the tissue to biological integration the BC or e-PTFE films and the presence of fibrosis or ossification. A third parameter analyzed was related to the integrity of the prosthesis, taking into account the invasion of each membrane by mononuclear cells, the neovascularization and the presence of fibroblasts. The ability to be absorbed was classified as: absent, mild, moderate, strong or advanced, according to the intensity detected. All the data were transformed into quantitative variables by assigning indices and histological scores.
2.5 Parameters of biocompatibility
The clinical signs, inflammatory response and the capacity of adhesion of the membrane in dural defect (sutureless insertion of the BC), coupled with data from the literature, particularly involving the BC in vitro and in vivo tests that demonstrate toxicity [30, 31], mechanicals aspects [27, 28] and performance requirements [29, 32], list the parameters needed for substantiated analysis of the biocompatibility of the BC membrane.
2.6 Statistical analysis
The intergroup comparison was analyzed using Pearson Qui-square, Fisher test and the Mann-Whitney test. Statistical significance was accepted at 95% confidence level p < 0.05 for comparison between the groups.
3 Results
3.1 Clinical characteristics
Following the dural graft, at the 120 days no signs of toxicity including autonomic (salivation and piloerection) or neurological effects (tremors and convulsions), or even deficiency in the motor or feeding behavior were observed during this period. The healing of the post-operative wound was similar between the two groups. Presence of dehiscence, hematoma formation, leakage of liquor as well as signs of infection, was not observed. Before the surgery, the average body weight of the animals was 380 ± 50 g in Group BC and 395 ± 40 g in Group e-PTFE. On the day of sacrifice, the body weight did not differ between the groups.
3.2 Macroscopic aspect of the surgical wound at the 120th post-operative day
The visual evaluation performed during the removal of the head for histophatological analysis did not detect deformities in the surgical scar, fistulas, focal collections nor granulomas. After withdrawal of the scalp, no cicatricial adhesions in the conjunctive tissue between the scalp and the dura mater substitute were identified. Both the BC or e-PTFE membranes were covered with a thin layer of conjunctive tissue.
3.3 Histopathological analysis
The occurrence of variables between the groups with respect to tissue cellularity in the external and internal surfaces adjacent to the prosthesis of BC or e-PTFE is shown in the Table 1. The ability of the nervous tissue to biological integration the membranes was assessed by the presence of fibrosis or ossification (Table 1) as well as prosthesis integrity, which gave information on the absorption capability (Table 1).
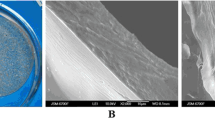
The presence of fibrosis in the outer surface of both membranes can be seen in these images where the absorption of BC was considered mild.
The capability of the BC membrane to be absorbable and invaded by vessels was distinct from the synthetic and non-porous e-PTFE film (Preclude®) as dural substitute. In most animals (~65%) the BC membrane absorption was considered moderate, in 25% it was mild, being registered in one case as strong and in another as advanced absorption reaction. e-PTFE absorption was not observed in the animals analyzed in the present study. Representative examples of moderate and strong absorption of BC membrane are shown in Figs. 1, 2.
Microscopic views of the BC or e-PTFE implants over the arachnoid membrane and cerebral cortex 120 days after dura mater excision surgery. The presence of fibrosis in the outer surface of both BC a and e-PTFE b membranes are seen in these representative images (arrows). Examples of ossification process (arrows) are seen in the adjacent outer surface of BC and e-PTFE membranes
4 Discussion
The main findings obtained in the present study corroborated the working hypothesis that bacterial cellulose membrane is a versatile biomaterial with potential biomedical and medical applications in neural tissue engineering. The use of e-PTFE as a positive control in this study was based on previous data in the literature showing the biocompatibility of this material as dural substitute without causing adhesion, rejection or absorption, and because of its ease in handling and durability [33–35].
A suitable hydrophilicity, low toxicity, and capacity to adherence were identified in the present study as beneficial features of the BC membranes when they were implanted for 120 days, as observed in previous studies [30–32, 36]. Integration of the BC film to the tissue was biocompatible and induced the tissue remodeling.
Dural closure has been performed with different techniques, materials and protocols, and the optimal combination has yet to be elucidated [37]. It has been recommended that an ideal material for dural repair should be able to protect nerve tissue, inexpensive, easy to handle, without inducing infection or cortical inflammation [38]. Membranes of e-PTFE, chosen here as a control dural substitute, have been widely used in neurosurgery, either in experimental or clinical studies [33–35]. e-PTFE is easily sterilized, keeping its functional properties for long periods of time and is inert, promoting a mild inflammatory reaction characterized by macrophages and giant cells in the inner and outer surface of the implant. Usually they are not rejected by the host tissue and have not been related to malignancy in humans [39, 40].
Despite the different structure of BC and e-PTFE membranes with respect to chemical composition and ability to be absorbed by the tissue, the sutureless insertion of both membranes as a dural substitute did not induce CSF leakage, or local and systemic toxicity. There were no cases of infection, delayed hemorrhages, behavior disturbances, seizures and palsies. The occurrence of a mild inflammatory reaction characterized by the presence of few macrophages and giant cells in the inner and outer surface of the BC membrane was comparable to that found using e-PTFE. Similar reaction was also found when patches of BC and e-PTFE membranes were used in femoral artery [25] or vein [26] angioplasty in dogs for a period of 180 days. In these studies, both membranes were sutured and despite a mild reaction, none of the animals showed signs of degeneration, infection, rupture, pseudo aneurysm formation or thrombosis at clinical examination.
In the present study, microscopic analysis also demonstrated a satisfactory level of graft acceptance. Moderate extradural fibrosis in the external surface occurred in 15 and 5% of the animals treated with BC or e-PTFE membranes, respectively, enhancing adherence of the implants to the bone fragment. No case of adherence of these membranes to the nervous tissue surface was observed even considering the small incision in the arachnoid membrane performed in the surgical procedure adopted in our study and similar to that reported previously [14, 36].
Our results are comparable to those described using bacterial cellulose membranes synthesized as substitute dural in dogs [14] or in rabbits [17]. In these studies, moderate fibrosis occurred in contact with the bone fragment; but no adherence was seen in the cortical surface. In the dogs, cellulose fibers decreased in thickness until 270 days and were invaded by histiocytes and collagen fibers with low cellular reaction [14].
A recent study using bilayer chitosan scaffolding as a dural substitute allowed fibroblast infiltration and organized collagen fiber deposit in its porous layer [41]. Late favorable results of duroplasty in humans with Acetobacter xylinum synthesized cellulose were recently reported although a limitation of this material was the low elasticity of the membranes during suturing [15]. The thickness of BC (~85 µm) is comparatively lower and its elasticity was considered adequate for suturing vein or artery without tearing [25, 26].
In one study about with meshes manufactured from bacterial cellulose (BC), evaluate their organic tissue interaction and compare with an ePTFE’s prosthesis used to repair acute defect of muscle aponeurotic induced in rats, the authors observed that there was biological integration and biomechanical elasticity of BC membrane, and therefore, they considered as a new alternative biomaterial for use as a bio prosthesis [28].
Ossification in the external surface of BC or e-PTFE grafts was the most frequent data observed in the present study, regarding the host capacity in retaining the dural substitute (65% for BC vs. 50% for e-PTFE). These results seem to reinforce recent evidence related to biocompatibility of BC for interacting with the bone tissue in the treatment of critical defects in rat skulls [24]. According to this study, the association of collagen membrane of bovine origin (GenDerm® Baumer SA) and BC gel as carrier of bone morphogenetic protein (BMP) and lyophilized bovine bone grafts (Gen-ox inorg® Baumer SA) was able to induce new bone formation at the edge of the skull defect. The performance of BC graft was better than that using GenDerm® alone as BMP carrier for a period of 90 and 180 days after surgery [24].
Integration of biomaterials or implants with surrounding native tissue is determinative for both functionality and long-term performance of the tissue. Capability to be absorbed and integrated into different living tissues has been reported as one of BC’s properties, which motivated the present study. The findings revealed that as dural substitute for 120 days, this biopolymer was slowly integrated into the surrounding tissue and a moderate level of absorption was detected in 65% of the animals. In two animals, a higher level of absorption was seen, characterized by the presence of intense cells infiltration and vascularization.
5 Conclusion
These results show that bacterial cellulose membrane is an adequate biomaterial for dural repair. The biocompatible BC was, retained the properties of local tissues and provides adequate mechanical properties, without the need for sutures when implanted for 120 days. The BC membrane not induced immune reaction, nor chronic inflammatory response and absence of neurotoxicity signals.
Furthermore the BC membrane can be easily produced, it has simple sterilization, is easy to handle and application and affordable.
Future studies should be carried out in order to assess the viability of BC as a dural substitute over longer periods of time.
References
Becker SS, Jackler RK, Pitts LH. Cerebrospinal fluid leak after acoustic neuroma surgery: a comparison of the translabyrinthine, middle fossa, and retrosigmoid approaches. Otol Neurotol. 2003;24:107–12.
Kuhn J, Hofmann B, Knitelius H, Coenen H, Bewermeyer H. Bilateral subdural haematoma and lumbar pseudomeningocele due to a chronic leakage of liquor cerebrospinalis after a lumbar discectomy with the application of ADCON-L gel. J Neurol Neurosurg Psychiatry. 2005;76:1031–33.
Sabatino G, Della Pepa GM, Bianchi F, Capone G, Rigante L, Albanese A, Maira G, Marchese E. Autologous dural substitutes: a prospective study. Clin Neurol Neurosurg. 2014;116:20–23.
Ostendorf AP, Connolly AM. Medical management of eosinophilic meningitis following bovine graft duraplasty for Chiari malformation type I repair. J Neurosurg Pediatr. 2013;12:357–9.
Sandoval-Sanchez JH, Ramos-Zuniga R, de Anda SL, Lopez-Dellamary F, Gonzalez-Castaneda R, Ramírez-Jaimes de L, Jorge-Espinoza G. A new bilayer chitosan scaffolding as a dural substitute: experimental evaluation. World Neurosurg. 2012;77:577–82.
Lam FC, Kasper E. Augmented autologous pericranium duraplasty in 100 posterior fossa surgeries-a retrospective case series. Neurosurgery. 2012;71(2 Suppl Operative):ons302–7. doi:10.1227/NEU.0b013e31826a8ab0.
Gazzeri R, Galarza M, Alfieri A, Neroni M, Roperto R. Simple intraoperative technique for minor dural gap repair using fibrin glue and oxidized cellulose. World Neurosurg. 2011;76:173–5.
Messing-Jünger AM, Ibanez J, Calbucci F, Choux M, Lena G, Mohsenipour I, Van Calenbergh F. Effectiveness and handling characteristics of a three-layer polymer dura substitute: a prospective multicenter clinical study. J Neurosurg. 2006;105:853–8.
Yamada K, Miyamoto S, Nagata I, Kikuchi H, Ikada Y, Iwata H, Yamamoto K. Development of a dural substitute from synthetic bioabsorbable polymers. J Neurosurg. 1997;86:1012–7.
Malliti M, Page P, Gury C, Chomette E, Nataf F, Roux FX. Comparison of deep wound infection rates using a synthetic dural substitute (Neuropatch) or pericranium graft for dural closure: a clinical review of 1 year. Neurosurgery. 2004;54:599–604.
Knopp U, Christmann F, Reusche E, Sepehrnia A. A new collagen biomatrix of equine origin versus a cadaveric dura graft for the repair of dural defects - a comparative animal experimental study. Acta Neurochir (Wien). 2005;147:877–87.
Clausen F, Lindh T, Salimi S, Erlandsson A. Combination of growth factor treatment and scaffold deposition following experimental traumatic brain injury show a temporary effect on cellular regeneration. Brain Res. 2014;1588:37–46.
Khan F, Ahmad SR. Polysaccharides and Their derivatives for versatile tissue engineering application. Macromol Biosci. 2013;13:395–421.
Mello LR, Feltrin LT, Fontes Neto PT, Ferraz FA. Duraplasty with biosynthetic cellulose: an experimental study. J Neurosurg. 1997;86:143–50.
Mello LR, Alcantara BB, Bernardes CI, Boer VH. Late favorable results of duraplasty with biocellulose: clinical retrospective study of 20 cases. Arq Bras Neurocir. 2012;31:128–34. http://files.bvs.br/upload/S/0103-5355/2012/v31n3/a3396.pdf.
Rosen CL, Steinberg GK, Demonte F, Delashaw JB, Lewis SB, Shaffrey ME, Aziz K, Hantel J, Marciano FF. Results of the prospective, randomized, multicenter clinical trial evaluating a biosynthesized cellulose graft for repair of dural defects. Neurosurgery. 2011;69:1093–103.
Xu C, Ma X, Chen S, Tao M, Yuan L, Jing Y. Bacterial Cellulose Membranes Used as Artificial Substitutes for Dural Defection in Rabbits. Int J Mol Sci. 2014;15:10855–67.
Kowalska-Ludwicka K, Cala J, Grobelski B, Sygut D, Jesionek-Kupnicka D, Kolodziejczyk M, Bielecki S, Pasieka Z. Modified bacterial cellulose tubes for regeneration of damaged peripheral nerves. Arch Med Sci. 2011;9(3):527–34. doi:10.5114/aoms.2013.33433. 20.
Pértile RAN, Moreira S, Andrade FK, Domingues L, Gama M. Bacterial cellulose modified using recombinant proteins to improve neuronal and mesenchymal cell adhesion. Biotechnol Prog. 2012;28:526–32.
Paterson-Beedle M, Kennedy JF, Melo FAD, Lloyd LL, Medeiros V. Cellulosic exopolysaccharide produced from sugarcane molasses by a Zoogloea sp. Carbohydr Polym. 2000;42:375–83.
Cavalcante AHM, Carvalho LB, Carneiro-da-Cunha MG. Cellulosic exopolysaccharide produced by Zoogloea sp. as a film support for trypsin immobilization. Biochem Eng J. 2006;29:258–61.
Carvalho Junior AM, Santos MM, Barkokébas BB, de Andrade Aguiar JL, Lima SVC, Dambros M. Characterization of the deposition of collagen fibers and lithogenic potential in bladder of rats submitted to a sugar cane biopolymer graft. Int Braz J Urol. 2012;38:544–51.
Albuquerque PCVC, Aguiar JLA, Santos SM, Pontes Filho N, Mello RJV, Costa MLCR. Comparative study of the areas of osteochondral defects produced in the femoral condyles of rabbits treated with gel of sugarcane biopolymer. Acta Cir Bras. 2011;26:383–6.
Medeiros Junior MD, Carvalho EJDA, Catunda IS, Bernardino-Araujo S, Aguiar JLA. Hydrogel of polysaccharide of sugarcane molasses as carrier of bone morphogenetic protein in the reconstruction of critical bone defects in rats. Acta Cir Bras. 2013;28:233–8.
Aguiar JLA, Lins EM, Barros Marques SR, Barros Coelho AR, Rossiter RO, Melo RJV. Surgarcane biopolymer patch in femoral artery angioplasty on dogs. Acta Cir Bras. 2007;22:77–81.
De Barros-Marques SR, Marques-Lins E, De Albuquerque MCS, Aguiar JLA. Sugarcane biopolymer patch in femoral vein angioplasty on dogs. J Vasc Surg. 2012;55:517–21.
Falcão SC, Coelho ARDB, Evêncio Neto J. Biomechanical evaluation of microbial cellulose (Zoogloea sp.) and expanded polytetrafluoroethylene membranes as implants in repair of produced abdominal wall defects in rats. Acta Cir Bras. 2008;23:184–91.
Silveira RK, Coelho AR, Pinto FC, de Albuquerque AV, de Melo Filho DA, de Andrade Aguiar JL. Bioprosthetic mesh of bacterial cellulose for treatment of abdominal muscle aponeurotic defect in rat model. J Mater Sci Mater Med. 2016;27(8):129. doi:10.1007/s10856-016-5744-z.
Fragoso AS, Silva MB, De Melo CP, Aguiar JLA, Rodrigues CG. Dielectric study of the adhesion of mesenchymal stem cells from human umbilical cord on a sugarcane biopolymer. J Mater Sci Mater Med. 2014;25:229–37.
Castro CMMB, Aguiar JLA, Melo FAD, Silva WTF, Marques E, Silva DB. Sugarcane biopolymer cytotoxicity. An Fac Med Univ Fed Pernamb. 2004;49:119–23. http://www.anaisdemedicina.revistaonline.org/_Secao/3289/_Pagina/Revista/ArtigoVisualizar.aspx?artigoId=85&ass=64816093.
Pinto FCM, De-Oliveira ACAX, De-Carvalho RR, Gomes-Carneiro MR, Coelho DR, Lima SVC, Paumgartten FJR, Aguiar JLA. Acute toxicity, cytotoxicity, genotoxicity and antigenotoxic effects of a cellulosic exopolysaccharide obtained from sugarcane molasses. Carbohydr Polym. 2016;137:556–60.
Lucena MT, Melo Júnior MR, Lira MMM, Castro CM, Cavalcanti LA, Menezes MA, Pinto FCM, Aguiar JLA. Biocompatibility and cutaneous reactivity of cellulosic polysaccharide film in induced skin wounds in rats. J Mater Sci Mater Med. 2015;26:5410
Gortler M, Braun M, Becker I, Roggendorf W, Heiss E, Grote E. Animal experiments with a new dura graft (polytetraflurethylene). Results. Neurochirurgia (Stuttg). 1991;34:103–6.
Yamagata S, Goto K, Oda Y, Kikuchi H. Clinical experience with expanded polytetrafluoroethylene sheet used as an artificial dura mater. Neurol Med Chir (Tokyo). 1993;33:582–5.
Matsumoto Y, Aikawa H, Tsutsumi M, Narita S, Yoshida H, Etou H. Histological examination of expanded polytetrafluoroethylene artificial dura mater at 14 years after craniotomy. Neurol Med Chir (Tokyo). 2013;53:43–6.
Viñas FC, Ferris D, Kupsky WJ, Dujovny M. Evaluation of expanded polytetrafluoroethylene (ePTFE) versus polydioxanone (PDS) for the repair of dura mater defects. Neurol Res. 1999;21:262–8.
Walcott BP, Neal JB, Sheth SA, Kahle KT, Eskandar EN, Coumans JV. The incidence of complications in elective cranial neurosurgery associated with dural closure material. J Neurosurg. 2014;120:278–84.
Vakis A, Koutentakis D, Karabetsos D, Kalostos G. Use of polytetrafluoroethylene dural substitute as adhesion preventive material during craniectomies. Clin Neurol Neurosurg. 2006;108:798–802.
Nazzaro JM, Craven DE. Successful treatment of postoperative meningitis due to Haemophilus influenzae without removal of an expanded polytetrafluoroethylene dural graft. Clin Infect Dis. 1998;26:516–8.
Nakagawa S, Hayashi T, Anegawa S, Nakashima S, Shimokawa S, Furukawa Y. Postoperative infection after duraplasty with expanded polytetrafluoroethylene sheet. Neurol Med Chir (Tokyo). 2003;43:120–4.
Sandoval-Sánchez JH, Ramos-Zúñiga R, Luquín De Anda S, López-Dellamary F, Gonzalez-Castañeda R, Ramírez-Jaimes JDLC. A new bilayer chitosan scaffolding as a dural substitute: Experimental evaluation. World Neurosurg. 2012;77:577–82.
Acknowledgements
Research Performed at Center for Experimental Surgery of the Federal University of Pernambuco UFPE, Recife-PE, Brazil. Research Performed at collaboration with the Laboratory of Human Reproduction of the University of São Paulo (UNIFESP), Laboratory of Immunopathology Keizo Asami (LIKA), and the Department of Nuclear Energy (DEN) of the Federal University of Pernambuco, Recife/PE, Brazil. The English version of this text has been revised by a native speaker, Sidney Pratt, Canadian, BA, MAT (The Johns Hopkins University), RSA diploma (TEFL) University of Cambridge.
Funding
National Council for Scientific and Technological Development (CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Lima, F.d.M.T., Pinto, F.C.M., Andrade-da-Costa, B.L.d.S. et al. Biocompatible bacterial cellulose membrane in dural defect repair of rat. J Mater Sci: Mater Med 28, 37 (2017). https://doi.org/10.1007/s10856-016-5828-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5828-9