Abstract
Background/purpose
Atrial fibrillation (AF) recurs post-ablation in 30–40% of patients. The approach to a repeat ablation, beyond isolation of reconnected pulmonary veins (PVs), is not well established. We sought to prospectively assess outcomes and predictors of recurrence among consecutive patients who underwent repeat AF ablation with a standardized approach.
Methods
This was a single-center prospective study of consecutive patients who underwent repeat AF ablation. Our protocol consisted of six steps: PV re-isolation, ablation of left atrial low-voltage areas (LVAs), ablation of isoproterenol-induced non-PV triggers, electrophysiology study (EPS) and ablation of induced AVNRT/AVRT, ablation of induced clinical atrial flutters, and lastly empiric ablation as per operator discretion if no other ablation was performed.
Results
Among 725 AF ablations performed during the study period, 74 were repeat ablations. Of those undergoing repeat ablation, 53 (72%) had PV reconnection, 30 (41%) had LVAs, seven (10%) had non-PV triggers, five (7%) had AVNRT, and 15 (20%) had typical atrial flutter. Following repeat ablation, arrhythmia-free survival was 65% at 1 year. The absence of PV reconnection was the only factor independently associated with recurrence after repeat ablation (recurrence rate 71%, adjusted OR 7.91, 95% CI 2.31–27.16, p = 0.001).
Conclusions
A comprehensive approach to repeat AF ablation including PV re-isolation, LVA ablation, non-PV trigger ablation, EPS, and flutter ablation was associated with a 65% 1-year arrhythmia-free survival. The absence of PV reconnection was the only independent predictor of arrhythmia recurrence. Further research is needed to identify therapies beyond PV isolation for patients undergoing repeat ablation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
After two decades of progress, catheter ablation has been established as a valuable means of reducing atrial fibrillation (AF) burden and improving quality of life [1]. However, 30–40% of patients still experience AF within the first year after ablation [2]. As such, repeat ablations are common [3, 4] and lead to an average of 1.3 procedures per patient [5]. While pulmonary vein (PV) reconnection is a frequent finding [6, 7], other potential causes of arrhythmia recurrence include non-PV triggers, pro-arrhythmic atrial scar, and re-entrant atrial flutters (some iatrogenic) [3]. Despite the frequency of recurrent arrhythmia after ablation, there is no consensus on the best technical approach to a repeat procedure beyond simply repeating PV isolation. The heterogeneity of approaches speaks to uncertainty in the field as investigators have proposed mapping and ablation of non-PV triggers [8, 9], isolation of the posterior wall via a box lesion set [10], targeting of complex fractionated electrograms [11], complex ablation lines [12], and superior vena cava (SVC) isolation [7]. The studies that critically examine a standardized repeat ablation strategy beyond re-isolation of PVs are limited to small cohorts [10, 13,14,15].
Given the lack of recommendations from professional societies, we designed a comprehensive standard approach for all patients undergoing repeat ablation that comprised re-isolation of any reconnected PVs, ablation of all low voltage areas (LVAs) within the left atria (LA), non-PV trigger mapping, a complete electrophysiology study (EPS) to rule out supraventricular tachycardia, cavo-tricuspid isthmus (CTI) ablation for induced or clinical typical atrial flutter, ablation lines for inducible clinical atypical atrial flutter, and additional lesions at the operator’s discretion in the absence of ablation at the prior steps. In this report, we prospectively assess outcomes and predictors of recurrence after implementing this approach.
2 Methods
This was a single-center prospective observational study. We included consecutive patients who underwent repeat AF ablation at the University of Ottawa Heart Institute. Patients with persistent and paroxysmal AF were included; patients who had more than one prior AF ablation were included once in the study cohort.
2.1 Ablation procedure
All repeat ablations were completed using a 3D electroanatomical mapping system (CARTO, Biosense Webster, Diamond Bar CA). High-density LA and PV voltage maps were created in sinus rhythm (or atrial pacing at cycle length ≥ 600 ms) using a 1-mm spacing multipolar catheter (Pentaray, Biosense Webster, Diamond Bar, CA; 2–6-2 mm inter-electrode spacing). In patients presenting with AF, electrical cardioversion to restore sinus rhythm was performed. A minimum of 750 LA points was acquired during this step. Bipolar voltage was acquired from septum, roof, anterior, posterior, and inferior LA with voltage settings as follows: < 0.25 mV for dense LVA and > 0.5 mV for normal atrial myocardium. Atrial LVA was collected using a standardized data collection software (Confidense®). The following settings were used for voltage data collection: (a) tissue proximity indicator enabled (TPI = ON) to ensure adequate catheter contact; (b) cycle length stability (baseline cycle length ± 5%) and catheter stability 2 mm; and (c) maximal point density 1 mm.
Contact force technology catheters were used for ablation (Thermocool SmartTouch, Biosense Webster) with a target contact force ≥ 8 g. Continuous monitoring of the surface electrocardiogram and intracardiac bipolar electrograms was done with a Pruka recording system (CardioLab Electrophysiology Recording System, GE Healthcare Systems, Chicago, IL). Endocardial bipolar electrograms were evaluated at 100 mm/s sweep speed and filtered at 30 to 500 Hz. All radiofrequency lesions were delivered point by point in power control mode using a SmartAblate generator (Biosense Webster). Linear lesions were evaluated with differential pacing to demonstrate bidirectional block across ablation lines and adenosine was administered at operator discretion. When cluster lesions were delivered, loss of local electrograms and loss of local capture were used as an ablation endpoint.
2.2 Ablation protocol
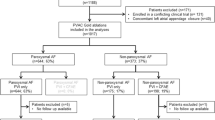
All patients underwent a standard repeat ablation protocol (Fig. 1).
Standardized repeat atrial fibrillation ablation protocol. The protocol was carried out in full for all patients in the study cohort. LA = left atrium, LVAs = low voltage areas, PV = pulmonary vein, EPS = electrophysiology study, AVNRT = AV-nodal re-entrant tachycardia, AVRT = atrio-ventricular re-entrant tachycardia, CTI = cavo-tricuspid isthmus
The subsequent ablation steps were as follows:
-
1.
Re-isolation of all reconnected PVs: Entrance and exit block was confirmed with pacing and use of adenosine to assess for dormant conduction (dose 12–18 mg targeting at least one blocked atrial beat).
-
2.
Ablation of all LA LVAs: This was defined as bipolar voltage of ≤ 0.5 mV on endocardial mapping. Areas of LVA ≤ 4 cm2 were treated with cluster ablation; areas larger than 4 cm2 were isolated by either encircling the scar or linear ablation to achieve exit and entrance block [16].
-
3.
Non-PV trigger mapping: Patients underwent targeting of non-PV triggers of AF that could be provoked by cardioversion of spontaneous AF, infusion of isoproterenol in incremental doses (3, 6, 12, and 20 μg/min), and/or burst pacing to provoke AF followed by cardioversion with low-dose isoproterenol infusion (2–8 μg/min). A non-PV trigger was defined as a source of repetitive and reproducible atrial premature depolarizations (APDs) that triggered AF [17, 18]. Trigger localization criteria have been previously described [19]. Trigger protocol was repeated after ablation to confirm trigger elimination.
-
4.
Electrophysiology study: Single extrastimulus pacing from a right-atrial catheter (or coronary sinus catheter) and the RV apex at two drive trains (600 ms/400 ms) down to refractoriness. All patients with inducible AV-nodal re-entrant tachycardia (AVNRT) or atrioventricular re-entrant tachycardia (AVRT) underwent slow pathway or accessory pathway ablation, respectively.
-
5.
Atrial flutter ablation: CTI ablation was performed if CTI-dependent atrial flutter was clinical or inducible. Non-CTI-dependent atrial flutters were ablated only if present clinically and inducible during EPS.
-
6.
Additional ablation at physician discretion: Only in patients with no ablation targets in steps 1–5 (i.e., no evidence of PV reconnection, LVAs, non-PV triggers or inducible SVT, or CTI-dependent/clinical flutter), additional ablation was permitted at the operators’ discretion. This included empiric linear ablation (such as posterior wall isolation) and any additional right atrial ablation.
2.3 Study endpoints
The primary endpoint was freedom from atrial arrhythmia ≥ 30 s in duration at 1 year, excluding a 3-month blanking period immediately post procedure.
2.4 Follow-up
Patients were routinely followed at three, six, and 12 months post-ablation and at any time if symptomatic with 14-day ambulatory electrocardiogram (ECG) monitoring and outpatient clinical assessments. A 12-lead ECG was performed at each clinical assessment. Antiarrhythmic medications were typically stopped at three months post-ablation; however, this was left to physician discretion.
2.5 Statistical analysis
Continuous variables are reported as mean ± standard deviation; categorical variables are reported as number (percentage). Predictors of arrhythmia recurrence post-ablation were identified via multivariable logistic regression with covariate inclusion based on univariate analyses using a criterion of p < 0.10. Post hoc analyses including hypertension or using a more liberal criterion of p < 0.20 for covariate inclusion were also undertaken. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) using a two-tailed α level of 0.05 to define statistical significance.
2.6 Ethics
The study was approved by the Ottawa Health Science Network Research Ethics Board (OHSN-REB).
3 Results
3.1 Patients
Between February 2017 and January 2020, 725 AF ablations were performed at our center. Of these, 74 were repeat AF ablation procedures (of which 69/74 had the initial procedure performed at our center), with 11 (14.9%) presenting with atypical flutter and the rest with AF. The average age of the cohort was 63 ± 9 years old and comprised 18% females (Table 1). Fifty-one percent of patients had paroxysmal AF as their diagnosis at the time of initial ablation. All patients received PVI at the time of their initial ablation using radiofrequency energy, with 13 (18%) receiving concomitant CTI ablation and additional ablation (at the discretion of the operator) as follows:
-
Patients with persistent AF at initial ablation (n = 36): three had scar modification, three had linear ablation (two roof lines and one mitral annular line), and two had complex atrial fractionated electrogram-targeted ablation.
-
Patients with paroxysmal AF (n = 38): three had linear ablation (three roof lines), and one had complex fractionated atrial electrogram-based ablation.
3.2 Repeat procedure details
Results of the repeat ablation procedure are shown in Table 2. The mean number of LA voltage points collected was 1475.8 ± 798, range 495–3629.
-
1.
PV reconnection was found in 53 (72%) patients. Of these, 24 (32%) had right-sided PV reconnection, and 12 (16%) had left-sided reconnection, while 17 (23%) had all PVs reconnected. PV reconnection tended to be more frequent in patients that presented with paroxysmal AF as compared to persistent AF (82% vs 61%, p = 0.051).
-
2.
LVAs were found and ablated in 30 (41%) patients. As shown in Fig. 2, 16 (22%) patients had anterior LVAs, and 19 (26%) patients had posterior LVAs. Septal and roof LVAs were less common, found in three (4%) and five (7%) patients, respectively. Eleven (15%) had LVA in multiple areas. The ablation strategy was customized to the areas involved, as per protocol [16], with a cluster of lesions used in 20 (67%) patients, encircling lesions in three (10%) patients, and linear ablation in 14 (47%) patients.
-
3.
Non-PV triggers were identified and ablated in seven (10%) patients (Fig. 2). Six were found in the LA; two on the posterior wall; one on the roof, anterior wall, and septum; and the last was on the inferior wall, near the coronary sinus. One trigger was found at the Eustachian ridge in the right atrium. All were successfully ablated with no recurrence on re-attempts at induction.
-
4.
EPS revealed inducible AVNRT in five (7%) patients, and all five underwent slow pathway ablation. None of the patients had an accessory pathway.
-
5.
CTI-dependent atrial flutter was clinical or induced in 15 (20%) patients who underwent CTI ablation. Clinical atypical flutter was inducible and ablated in eight patients (five mitral annular flutters and three roof flutters); 2/8 patients had presented in atypical flutter that was terminated with ablation. Seven patients had brief flutter that either spontaneously terminated or degenerated into AF. None had re-inducible flutter post ablation.
-
6.
Additional ablation: eight (11%) patients received additional ablation. Of these, one was in the right atrium for area of LVA. Seven had empiric LA linear ablation (five had posterior wall isolation; two had roof lines).
Graphical representation of approximate location of low voltage areas (*), defined as bipolar voltage ≤ 0.5 mV, and non-pulmonary vein triggers (X). SVC = superior vena cava, IVC = inferior vena cava, ER = Eustachian ridge, CS Os = coronary sinus ostium, CS = coronary sinus, RSPV = right superior pulmonary vein, RIPV = right inferior pulmonary vein, LSPV = left superior pulmonary vein, LIPV = left inferior pulmonary vein, LAA = left atrial appendage
3.3 Patient outcomes and predictors of arrhythmia recurrence
One year after repeat ablation, 65% (48/74) of patients were free from atrial arrhythmia. Of the 26 patients with recurrence, 2 had atypical flutter or atrial tachycardia. Multivariable analysis identified isolated PVs at the repeat study as associated with arrhythmia recurrence (OR 7.91, 95% CI 2.31–27.16, p = 0.001; Table 3). This finding persisted in more inclusive multivariable models that included hypertension (OR 8.0, 95% CI 2.2–29.8, p = 0.001) and after adjusting for age and gender (OR 6.84, 95% CI 1.93–24.22, p = 0.003). The number of PVs found to be reconnected at the repeat study correlated with AF recurrence, as arrhythmia-free survival was 75% (27/36) in patients with one set of PVs reconnected, and increased to 88% (15/17) in patients with all PVs reconnected (Fig. 3). The average time to recurrence in those with isolated PVs at repeat ablation was 215 ± 156 days vs 340 ± 235 days in those with at least one reconnected PV; this difference was not significant (p = 0.064).
Among the 48 patients who did not have recurrence at one year, seven were still on antiarrhythmic drugs. Two of these patients had symptomatic palpitations but no documented arrhythmia (one remained on propafenone and one on flecainide); the remaining five stayed on amiodarone due to patient preference.
Table 4 shows difference in characteristics between those who had PV reconnection and those who did not; those with absence of reconnection had more LVA (67% vs 30%, p = 0.004) and hypertension (67% vs 30%, p = 0.004).
We did not find any differences between patients with paroxysmal versus persistent AF.
3.4 Outcomes in patients with durable PVI at repeat procedure
Among the 21 patients with no PV reconnection at the repeat EP study, six patients (29%) had no recurrence, and 15 (71%) had recurrence. Among the patients with no recurrence, three had LVAs that were ablated (two with cluster ablation and one with posterior wall isolation), two had CTI ablation for inducible atrial flutter, and one had empiric posterior wall isolation. LA arrhythmia was not inducible with isoproterenol or rapid atrial pacing in these six patients, and none had evidence of non-PV triggers or inducible SVT.
In comparison, among the 15 patients who had recurrence, two (13%) had non-PV triggers, three (20%) had inducible AVNRT, and six (40%) had inducible LA arrhythmia (two with isoproterenol, four with atrial pacing). The difference in rate of inducible LA arrhythmia (40% vs 0%) was not statistically significant (p = 0.067).
4 Discussion
In this prospective single-center study of 74 patients undergoing repeat AF ablation using a standardized comprehensive protocol, we found a subsequent 1-year arrhythmia-free survival rate of 65%. Twenty-eight percent of patients had durable PV isolation, which was a strong predictor of subsequent arrhythmia recurrence (adjusted OR 7.9, 95% CI 2.3–27.2).
We found that arrhythmia-free survival in those with reconnected PVs was high (42/53 = 79.2%), especially in those with all PVs reconnected (88% at 1 year). This confirms that at time of repeat ablation, PV reconnection remains the most significant treatable cause of recurrence [20, 21]. We found a pattern of more right-sided PV reconnections, as has been previously described [22, 23].
The PV reconnection rate was 72% among patients undergoing repeat AF ablation. In the past, rates as high as 95% have been reported with more recent studies reporting rates around 70% [24, 25], likely representing advancement of catheter technology and techniques. The question of what to do beyond PV re-isolation, however, is still unclear. Despite systematically ablating non-PV targets such as LVAs, non-PV triggers, and SVT, those without PV reconnection still had a high recurrence rate (71%) in our study. As rates of PV reconnection decrease, more attention will have to be directed towards understanding the mechanism of AF recurrence in patients with isolated PVs.
Patients without PV reconnection were more likely to have hypertension and LVAs. It is possible that in these patients, progressive atrial myopathy had a larger role in arrhythmia recurrence, and routinely targeting the LVAs with ablation was not sufficient to prevent recurrence of atrial arrhythmia. We also found that those without PV reconnection and inducible atrial arrhythmia at time of repeat ablation had numerically higher recurrence; an observation seen previously [9]. Lastly, we found that patients without PV reconnection had a numerically lower time to recurrence after redo ablation. Further ablation beyond PV isolation may not be effective in reducing recurrences without concurrently preventing and treating atrial myopathy. Possible treatment approaches have been evaluated. A prior randomized control trial of aggressive blood pressure control with medications before ablation in an effort to treat myopathy did not reduce recurrence [26]. A randomized trial of renal denervation with PV isolation, however, did reduce recurrence [27]. Non-randomized studies have shown benefit with treatment of obstructive sleep apnea and weight loss as well [28, 29].
With the use of high-density voltage mapping, 41% of patients had evidence of LVAs. We did not find the presence of LVA to be a predictor of recurrence. This is in contrast to prior studies investigating recurrence after first ablation [30, 31]. Although routine LVA-targeted ablation has not been adopted into widespread practice, a non-randomized cohort study found recurrence was decreased with a LVA-modification strategy [32], and subsequent recurrence rates were similar to patients without LVA. Thus, it is possible that in our protocol, the routine targeting of LVA reduced the impact of the LVA on recurrence. However, without a comparator group, it is difficult to conclusively determine this.
We found that seven (10%) patients had inducible non-PV triggers. Among the six patients with left atrial triggers, the most common location was the posterior wall (50%). We did not find that non-PV trigger ablation was associated with reduced recurrence; this may have been due to a relatively low number of patients with triggers. The prevalence of non-PV triggers at repeat ablation has been described previously [6, 24], with one study of patients undergoing repeat ablation finding a 29% rate of ablatable non-PV triggers; the rate of recurrence was twice that of those without ablatable triggers [9]. Studies have also described multiple non-PV triggers, as well as new triggers at subsequent repeat ablations [6, 24], suggesting that triggers may be the result of underlying atrial myopathy or probabilistic during induction.
Our overall recurrence rate of 35% after repeat ablation was higher than previously reports, including one study with a recurrent rate of 21% at 12 months4 and one with a 36% rate at a mean of 17 months [14]. This is possibly explained by our intensive follow-up monitoring strategy with 2-week Holter monitors at three, six, and 12 months, compared to 24-hour Holter monitors in the first study and symptomatic transtelephonic ECGs in the second.
4.1 Limitations
Limitations of our study include the single center and observational nature of the cohort study. Without a comparator group, it is difficult to make definitive conclusions from our observations. In particular, we do not have data on patients who had recurrent AF after initial ablation but did not undergo repeat ablation; this could lead to selection bias. Additionally, we do not have data on non-arrhythmic outcomes such as number of cardioversions or hospitalizations. Given the relatively intense monitoring, recurrence may overestimate the clinical impact on patients. The small number of patients who had absence of reconnected PVs at repeat ablation did not allow us to statistically examine predictors of recurrence in this population.
5 Conclusions
We describe a comprehensive approach to repeat AF ablation using a standardized protocol that includes isolation of reconnected PVs, targeting all LVAs and ablating all non-PV triggers, as well as ablation of inducible SVTs, CTI-dependent atrial flutter, and clinical non-CTI dependent flutters. Reconnected PVs at repeat procedure was a strong predictor of arrhythmia-free survival with high recurrence rates among patients without evidence of PV reconnection. Our findings demonstrate that PV re-isolation remains the most important treatable cause of atrial arrhythmia recurrence after AF ablation; however, further research is needed to investigate therapies beyond PV re-isolation.
Change history
14 June 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10840-022-01269-y
Abbreviations
- AF:
-
Atrial fibrillation
- PV:
-
Pulmonary vein
- SVC:
-
Superior vena cava
- LVA:
-
Low voltage areas
- LA:
-
Left atrium
- EPS:
-
Electrophysiology study
- CTI:
-
Cavo-tricuspid isthmus
- APDs:
-
Atrial premature depolarizations
- AVNRT:
-
AV-nodal re-entrant tachycardia
- AVRT:
-
Atrioventricular re-entrant tachycardia
- ECG:
-
Electrocardiogram
- PVI:
-
Pulmonary vein isolation
References
Wokhlu A, Monahan KH, Hodge DO, Asirvatham SJ, Friedman PA, Munger TM, … Packer DL. Long-term quality of life after ablation of atrial fibrillation the impact of recurrence, symptom relief, and placebo effect. J Am Coll Cardiol. 2010;55(21):2308–2316. https://doi.org/10.1016/j.jacc.2010.01.040
Wokhlu A, Hodge DO, Monahan KH, Asirvatham SJ, Friedman PA, Munger TM, … Packer DL. Long-term outcome of atrial fibrillation ablation: impact and predictors of very late recurrence. J Cardiovasc Electrophysiol. 2010;21(10):1071–1078. https://doi.org/10.1111/j.1540-8167.2010.01786.x
Hussein AA, Saliba WI, Martin DO, Bhargava M, Sherman M, Magnelli-Reyes C, … Wazni O. Natural history and long-term outcomes of ablated atrial fibrillation. Circ Arrhythm Electrophysiol. 2011;4(3):271–278. https://doi.org/10.1161/CIRCEP.111.962100
Bhargava M, Di Biase L, Mohanty P, Prasad S, Martin DO, Williams-Andrews M, … Natale A. Impact of type of atrial fibrillation and repeat catheter ablation on long-term freedom from atrial fibrillation: results from a multicenter study. Heart Rhythm. 2009;6(10):1403–1412. https://doi.org/10.1016/j.hrthm.2009.06.014
Cappato R, Calkins H, Chen S-A, Davies W, Iesaka Y, Kalman J, … Biganzoli E. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3(1):32–38. https://doi.org/10.1161/CIRCEP.109.859116
Lin D, Santangeli P, Zado ES, Bala R, Hutchinson MD, Riley MP, … Marchlinski FE. Electrophysiologic findings and long-term outcomes in patients undergoing third or more catheter ablation procedures for atrial fibrillation. J Cardiovasc Electrophysiol. 2015;26(4):371–377. https://doi.org/10.1111/jce.12603
Cappato R, Negroni S, Pecora D, Bentivegna S, Lupo PP, Carolei A, … De Ambroggi L. Prospective assessment of late conduction recurrence across radiofrequency lesions producing electrical disconnection at the pulmonary vein ostium in patients with atrial fibrillation. Circulation. 2003;108(13):1599–1604. https://doi.org/10.1161/01.CIR.0000091081.19465.F1
Callans DJ, Gerstenfeld EP, Dixit S, Zado E, Vanderhoff M, Ren J-F, Marchlinski FE. Efficacy of repeat pulmonary vein isolation procedures in patients with recurrent atrial fibrillation. J Cardiovasc Electrophysiol. 2004;15(9):1050–5. https://doi.org/10.1046/j.1540-8167.2004.04052.x.
Takigawa M, Takahashi A, Kuwahara T, Okubo K, Takahashi Y, Nakashima E, … Isobe M. Impact of non-pulmonary vein foci on the outcome of the second session of catheter ablation for paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 2015;26(7):739–746. https://doi.org/10.1111/jce.12681
Bisignani A, Overeinder I, Kazawa S, Iacopino S, Cecchini F, Miraglia V, … Chierchia GB. Posterior box isolation as an adjunctive ablation strategy with the second-generation cryoballoon for paroxysmal atrial fibrillation: a comparison with standard cryoballoon pulmonary vein isolation. J Interv Card Electrophysiol. 2021;61(2):313–319. https://doi.org/10.1007/s10840-020-00812-z
Winkle RA, Mead RH, Engel G, Patrawala RA. Long-term results of atrial fibrillation ablation: the importance of all initial ablation failures undergoing a repeat ablation. Am Heart J. 2011;162(1):193–200. https://doi.org/10.1016/j.ahj.2011.04.013.
Chang T-Y, Lo L-W, Te ALD, Lin Y-J, Chang S-L, Hu Y-F, … Chen S-A. The importance of extrapulmonary vein triggers and atypical atrial flutter in atrial fibrillation recurrence after cryoablation: Insights from repeat ablation procedures. J Cardiovasc Electrophysiol. 2019;30(1):16–24. https://doi.org/10.1111/jce.13741
Tang R-B, Yan X-L, Dong J-Z, Kalifa J, Long D-Y, Yu R-H, … Ma C-S. Predictors of recurrence after a repeat ablation procedure for paroxysmal atrial fibrillation: role of left atrial enlargement. Europace. 2014;16(11):1569–1574. https://doi.org/10.1093/europace/euu013
Shah S, Barakat AF, Saliba WI, Abdur Rehman K, Tarakji KG, Rickard J, … Hussein AA. Recurrent atrial fibrillation after initial long-term ablation success: electrophysiological findings and outcomes of repeat ablation procedures. Circ Arrhythm Electrophysiol. 2018;11(4):e005785. https://doi.org/10.1161/CIRCEP.117.005785
Liang JJ, Elafros MA, Muser D, Pathak RK, Santangeli P, Supple GE, … Dixit S. Comparison of left atrial bipolar voltage and scar using multielectrode fast automated mapping versus point-by-point contact electroanatomic mapping in patients with atrial fibrillation undergoing repeat ablation. J Cardiovasc Electrophysiol. 2017;28(3):280–288. https://doi.org/10.1111/jce.13151
Nery PB, Al Dawood W, Nair GM, Redpath CJ, Sadek MM, Chen L, … Birnie DH. Characterization of low-voltage areas in patients with atrial fibrillation: insights from high-density intracardiac mapping. Can J Cardiol. 2018;34(8):1033–1040. https://doi.org/10.1016/j.cjca.2018.04.008
Dixit S, Lin D, Frankel DS, Marchlinski FE. Catheter ablation for persistent atrial fibrillation: antral pulmonary vein isolation and elimination of nonpulmonary vein triggers are sufficient. Circ Arrhythm Electrophysiol. 2012;5(6):1216–23; discussion 1223. https://doi.org/10.1161/CIRCEP.111.970343.
Dixit S, Marchlinski FE, Lin D, Callans DJ, Bala R, Riley MP, … Gerstenfeld EP. Randomized ablation strategies for the treatment of persistent atrial fibrillation: RASTA study. Circ Arrhythm Electrophysiol. 2012;5(2):287–294. https://doi.org/10.1161/CIRCEP.111.966226
Valles E, Fan R, Roux JF, Liu CF, Harding JD, Dhruvakumar S, … Marchlinski FE. Localization of atrial fibrillation triggers in patients undergoing pulmonary vein isolation: importance of the carina region. J Am Coll Cardiol. 2008;52(17):1413–1420. https://doi.org/10.1016/j.jacc.2008.07.025
Kim T-H, Park J, Uhm J-S, Joung B, Lee M-H, Pak H-N. Pulmonary vein reconnection predicts good clinical outcome after second catheter ablation for atrial fibrillation. Europace. 2017;19(6):961–7. https://doi.org/10.1093/europace/euw128.
De Pooter J, Strisciuglio T, El Haddad M, Wolf M, Phlips T, Vandekerckhove Y, … Duytschaever M. Pulmonary vein reconnection no longer occurs in the majority of patients after a single pulmonary vein isolation procedure. JACC. Clin Electrophysiol. 2019;5(3):295–305. https://doi.org/10.1016/j.jacep.2018.11.020
Kautzner J, Neuzil P, Lambert H, Peichl P, Petru J, Cihak R, … Kuck K-H. EFFICAS II: optimization of catheter contact force improves outcome of pulmonary vein isolation for paroxysmal atrial fibrillation. Europace. 2015;17(8):1229–1235. https://doi.org/10.1093/europace/euv057
El Haddad M, Taghji P, Phlips T, Wolf M, Demolder A, Choudhury R, … Duytschaever M. Determinants of acute and late pulmonary vein reconnection in contact force-guided pulmonary vein isolation: identifying the weakest link in the ablation chain. Circ Arrhythm Electrophysiol. 2017;10(4):e004867. https://doi.org/10.1161/CIRCEP.116.004867
Sadek MM, Maeda S, Chik W, Santangeli P, Zado ES, Schaller RD, … Marchlinski FE. Recurrent atrial arrhythmias in the setting of chronic pulmonary vein isolation. Heart Rhythm. 2016;13(11):2174–2180. https://doi.org/10.1016/j.hrthm.2016.08.026
Huo Y, Kronborg MB, Richter U, Guo J, Ulbrich S, Zedda AM, … Piorkowski C. Electrophysiological findings during atrial fibrillation reablation: extending from pulmonary vein reconnection to sequential bipolar voltage map information. J Cardiovasc Electrophysiol. 2020;31(4):885–894. https://doi.org/10.1111/jce.14387
Parkash R, Wells GA, Sapp JL, Healey JS, Tardif J-C, Greiss I, … Tang ASL. Effect of aggressive blood pressure control on the recurrence of atrial fibrillation after catheter ablation: a randomized, open-label clinical trial (SMAC-AF [substrate modification with aggressive blood pressure control]). Circulation. 2017;135(19):1788–1798. https://doi.org/10.1161/CIRCULATIONAHA.116.026230
Steinberg JS, Shabanov V, Ponomarev D, Losik D, Ivanickiy E, Kropotkin E, … Romanov AB. Effect of renal denervation and catheter ablation vs catheter ablation alone on atrial fibrillation recurrence among patients with paroxysmal atrial fibrillation and hypertension: the ERADICATE-AF randomized clinical trial. JAMA. 2020;323(3):248–255. https://doi.org/10.1001/jama.2019.21187
Linz D, McEvoy RD, Cowie MR, Somers VK, Nattel S, Lévy P, … Sanders P. Associations of obstructive sleep apnea with atrial fibrillation and continuous positive airway pressure treatment: a review. JAMA Cardiol. 2018;3(6):532–540. https://doi.org/10.1001/jamacardio.2018.0095
Kanagala R, Murali NS, Friedman PA, Ammash NM, Gersh BJ, Ballman KV, … Somers VK. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20): 2589–2594. https://doi.org/10.1161/01.CIR.0000068337.25994.21
Verma A, Wazni OM, Marrouche NF, Martin DO, Kilicaslan F, Minor S, … Natale A. Pre-existent left atrial scarring in patients undergoing pulmonary vein antrum isolation: an independent predictor of procedural failure. J Am Coll Cardiol. 2005;45(2):285–292. https://doi.org/10.1016/j.jacc.2004.10.035
Masuda M, Fujita M, Iida O, Okamoto S, Ishihara T, Nanto K, … Mano T. Left atrial low-voltage areas predict atrial fibrillation recurrence after catheter ablation in patients with paroxysmal atrial fibrillation. Int J Cardiol. 2018;257: 97–101. https://doi.org/10.1016/j.ijcard.2017.12.089
Rolf S, Kircher S, Arya A, Eitel C, Sommer P, Richter S, … Piorkowski C. Tailored atrial substrate modification based on low-voltage areas in catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 2014; 7(5): 825–833. https://doi.org/10.1161/CIRCEP.113.001251
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In this article the author name "Pasquale Santangeli" was incorrectly written as "Pasquale Santangelli".
Rights and permissions
About this article
Cite this article
Weng, W., Birnie, D.H., Ramirez, F.D. et al. Outcomes of a comprehensive strategy during repeat atrial fibrillation ablation. J Interv Card Electrophysiol 65, 391–399 (2022). https://doi.org/10.1007/s10840-022-01190-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01190-4