Abstract
Background
The role of catheter ablation as an adjunct and alternative to ICD implantation is not known in patients at risk for recurrent ventricular tachycardia (VT) and sudden cardiac death (SCD) across Asia. Patients with nonischemic etiologies of cardiomyopathy, which are highly prevalent in Asia, have not been previously enrolled in randomized trials of VT ablation.
Objective
To evaluate whether preemptive catheter ablation in patients with monomorphic VT and an indication for ICD implantation results in improved clinical outcomes compared to ICD implantation with standard medical therapy alone. To examine the natural history of ablation outcomes in the absence of background ICD therapy in patients that refuse randomization.
Methods
The PAUSE-SCD study (NCT02848781) is a prospective, multi-center, randomized controlled trial enrolling patients with structural heart disease (EF < 50%) with an indication for ICD implantation. Patients are randomized in a 1:1 fashion to two treatment arms: ICD with ablation and ICD with standard medical therapy alone. A prospective registry cohort was designed to follow the outcomes of patients who refuse ICD and randomization but elect to receive catheter ablation as primary therapy. The primary endpoint is defined as a composite of recurrent VT, cardiovascular rehospitalization, and death. Pre-specified secondary endpoints include each of the individual components of the primary endpoint in addition to comparison between randomized and registry patients.
Conclusion
The PAUSE-SCD study is a prospective, multi-center, randomized, and controlled trial examining the impact of preemptive catheter ablation on cardiovascular outcomes in patients with an indication for ICD at risk for recurrent VT and SCD. It represents the first multi-center VT ablation study in Asia, with a design intended to provide insights into the role of both ICD and ablation therapy in a predominantly nonischemic population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Sudden cardiac death (SCD) remains the leading cause of death in the USA, with an estimated 450,000 cases annually [1]. Implantable cardioverter defibrillator (ICD) therapy remains the most effective abortive strategy for arrhythmic mortality in the secondary and primary prevention setting. However, ICD therapies are strongly associated with increased rates of hospitalization and all-cause mortality [2]. As catheter ablation of ventricular tachycardia (VT) has been demonstrated to decrease recurrent VT and ICD therapies across various clinical settings [3,4,5,6,7], it is biologically plausible that ablation may have a favorable impact on mortality.
A recent multi-center study of 2061 patients by the International VT Ablation Center Collaboration demonstrated that recurrent VT after failed catheter ablation was associated with a seven-fold subsequent risk for mortality, and freedom for recurrence was associated the improved survival, independent from ejection fraction, and heart failure severity [8]. SMASH VT and VTACH demonstrated statistically significant reductions in subsequent ICD therapy in patients that underwent prophylactic catheter ablation early in the course of their disease [9, 10]. While a trend towards improved survival was seen in those randomized to ablation in SMASH VT, limited sample size of these studies, low event rates, and presence of concomitant ICD therapy in both arms may have limited the discriminatory power to demonstrate mortality benefit from catheter ablation. Both of these two trials exclusively enrolled patients with post-infarction VT and to date; there have been no studies that have included nonischemic etiologies, a growing population referred for both ICD and catheter ablation [11, 12].
The incidence of SCD in Asia is not well known and the population at risk is over four times the size of the USA, as Asia has the largest population amongst any continent in the world [13]. Some estimates suggest that the incidence of SCD in Asia is lower than the rates reported in the USA [14]. However, the penetration and acceptance of both ICD therapy and catheter ablation into routine medical practice and guidelines in Asia is incomplete [15]. In the prospective ASIAN-HF registry from 11 Asian regions, ICD utilization was 12% amongst 3240 ICD-eligible patients studied [16]. The barriers to widespread adoption of ICD implantation across Asia are multifactorial, including financial, cultural, and scientific factors [17]. In Asia, the cost of the device is not fully covered by national insurance, making the technology cost-prohibitive for many patients who are likely to derive benefit. Cultural biases include aversion to surgery and implantation of devices, in addition to attitudes that reflect culture-specific disease progression.
Importantly, the vast majority of scientific evidence and randomized data that support current ICD guidelines have been performed in the USA and Europe, and the generalizability of these data to Asian populations remains unknown. Continuity in clinical follow-up remains a challenge in vast Asian countries due to limitations in patient education, cultural attitudes that bias against accepting implanted devices, and geographic distance from specialized centers. However, compliance may potentially be improved in patients with implantable devices due to the need for device interrogations, improved awareness and education, and particularly in those that receive ICD therapy.
In this current state, Asia serves as an optimal environment and setting to systematically examine the efficacy of both ICD therapy and catheter ablation of VT in patients at risk for sudden death due to ventricular arrhythmias. Further, insights into the impact of both ICD and ablation on mortality can be gained as patients with structural heart disease referred for VT ablation often refuse ICD implantation in Asia.
2 Methods
2.1 Primary objective
The purpose of this study is to evaluate whether preemptive VT ablation in patients with monomorphic VT and an indication for ICD implantation reduces arrhythmic and cardiovascular events compared to ICD implantation and standard medical therapy alone. A prospective registry cohort was designed to follow the outcomes of patients who refuse ICD and randomization but elect to receive catheter ablation as primary therapy.
2.2 Study design
PAUSE-SCD is a prospective multi-center, randomized, and controlled clinical trial designed to assess the role of preemptive catheter ablation in patients > 18 years old meeting indications for ICD implantation with structural heart disease (EF < 50%) and monomorphic VT. Patients with nonischemic etiologies, including dilated cardiomyopathy and arrhythmogenic RV cardiomyopathy (RVEF < 50%) are eligible for enrollment. Patients are deemed at higher risk for recurrent VT if they have an indication for ICD for secondary prevention of monomorphic VT or meet criteria for primary prevention ICD implantation and have inducible monomorphic VT during either invasive EP study or noninvasive programmed stimulation.
Patients with STEMI within 60 days, revascularization within 45 days, reversible causes of VT or cardiomyopathy, EF < 15%, NYHA IV status, and life expectancy less than 1 year are excluded from enrollment. The inclusion and exclusion criteria are listed in Table 1.
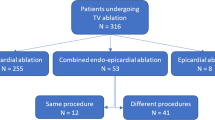
Randomization is assigned in 1:1 fashion between control and catheter ablation (Fig. 1). Those randomized to the control arm will receive ICD implantation (with or without clinically indicated CRT) and standard medical therapy (beta blockers, anti-arrhythmics) at the discretion of the treating physician. Subjects randomized to the ablation arm will undergo catheter ablation within 90 days of ICD implantation. Patients that refuse ICD therapy and randomization who elect to undergo ablation are eligible to be enrolled in a prospective registry cohort. Prior to 10/12/16, the participating sites performed randomization using a table (block size of 4) provided by the coordinating site. After additional in-house statistical review of the protocol, central electronic randomization from the coordinating site was advised. Central randomization commenced on 10/12/2016 and 25 patients were enrolled using the original randomization table schema.
3 Procedural approach
Before ablation, transthoracic echocardiogram (TTE) should be obtained up to 6 months prior to the procedure to assess EF. An MRI or TEE can be performed in lieu of a TTE. Trans-esophageal echocardiogram (TEE) is encouraged if the subject has a history of intra-cardiac thrombus or if there is a history of atrial fibrillation with a CHADS score > 1. A CT or MRI is encouraged within 3 months prior to ablation procedure to allow for anatomy fusion. 12-lead ECG within 6 months prior to the consent visit should be obtained. Medical history and complete assessment of current medications, including anti-arrhythmic drugs and anticoagulation will be collected.
3.1 Ablation procedure
All patients randomized to catheter ablation will undergo a substrate-based strategy using the NAVX electroanatomic 3D mapping system (Ensite, Velocity or Precision, Abbott, Lake Forest, IL, USA). Multi-electrode catheters such as a duodecapolar multielecrode (Livewire 2-2-2 mm spacing) are strongly encouraged to facilitate ultra-high-density mapping [18]. A minimum of 500 points is strongly encouraged for each chamber mapped. Epicardial mapping will be performed at the discretion of the treating physician but is encouraged for patients with arrhythmogenic right ventricular cardiomyopathy (ARVC), nonischemic cardiomyopathy (NICM), and those that do not demonstrate endocardial abnormalities. Scar will be defined as regions of low voltage < 1.5 mV with dense scar as < 0.5 mV [7].
Programmed stimulation is required before ablation procedure with 2-cycle lengths (600 and 400 ms up to triple extra stimuli down to ventricular effective refractory period or 200 ms). This may be performed through the implanted ICD/CRT-D (NIPS). A VT is considered clinical if there is a morphologic match by 12-lead ECG or intracardiac electrogram or has a similar tachycardia cycle length. LV stimulation within scar is recommended if the patient is non-inducible with right ventricular stimulation.
Irrigated ablation technology will be used for mapping and ablation. The choice of the catheter is up to the discretion of the physician performing the procedure. The ablation technique will be targeting of late and abnormal electrograms within scar with prioritization of those with matching pacemaps and multiple exit sites pacemaps [19, 20]. Deceleration zones with isochronal crowding should be targeted by using an isochronal late activation timing display [21]. Activation and entrainment mapping are encouraged if induced VTs are hemodynamically stable. If time allows, homogenization is encouraged, where all other local abnormal electrograms that demonstrate uncoupled activation are eliminated [22,23,24]. Substrate-based ablation strategy targeting abnormal regions of slow conduction can be performed in the event of non-inducibility.
The acute procedural endpoint is non-inducibility of the targeted clinical VT and elimination of abnormal electrograms within scar. Programmed stimulation will be performed in the same fashion as prior to ablation. Complete non-inducibility is encouraged but not required.
An ablation procedure form shall be completed by the operator, which includes patient demographics, number of VTs induced and targeted, predominant strategy, number of VT morphologies terminated during ablation, duration of radiofrequency applications, hemodynamic toleration during VT, and scar location and size.
ICD/CRT-D programming
Uniformity in protocol-mandated programmed settings should be confirmed after the device is enabled at the conclusion of ablation. Recommended settings consist of a VF zone of 230 bpm (ATP during charging) and VT zone of 185 or 10 bpm slower than the clinical VT (induced or spontaneous). Longer detection requiring 30/40 intervals with ATPx3 prior to shock therapy is recommended in the VT zone.
3.2 Postoperative treatment and follow-up
It is recommended that all patients have overnight observation after ablation. In patients that undergo epicardial ablation, an echocardiogram should be performed in the following day. Cardiac medications will be documented and tracked over the duration of the study. All subjects with heart failure should have their heart failure medications optimized including use of beta blockers and ACE inhibitors. A consult with a heart failure specialist is encouraged especially for optimization of drugs and for diuresis after ablation. Use of anti-arrhythmic drugs post-ablation are at the discretion of the treating physician. Subjects who have significant LV endocardial ablation and have LV dysfunction should receive anticoagulation for 4 weeks post-procedure.
Basic demographics and medical history will be collected from subjects enrolled into the registry cohort who refused ICD and randomization. Registry subjects will receive a phone contact and follow-up with clinic visits at 3, 6, 12, 18, and 24 months to check on their overall status. The follow-up schema and schedule are shown in Table 2.
4 Study endpoints
The primary endpoint is defined as freedom from recurrent VT, cardiovascular rehospitalization, and all-cause mortality through a period of 2 years after the procedure (ablation) or randomization (standard medical therapy). Recurrent VT is defined as any appropriate ICD therapy (shock or ATP) or documented sustained monomorphic VT > 30 s. Cardiovascular rehospitalization is defined as a hospital admission after the randomized procedure for heart failure, procedure-associated complication, or arrhythmia-related causes during the follow-up period.
Pre-specified secondary endpoints include each of the individual components of the primary endpoint. Comparison of the ablation-only registry with the randomized patients will serve as an additional secondary outcome measure. Pre-specified subgroup analysis will be performed for patients with RV cardiomyopathy.
5 Statistical analysis
Based on 2-year event rates from the SMASH VT (33% control arm) [9], VTACH (71% control arm) [10] and the AVID (> 60%) study [25]; a 50% reduction in events from ablation is projected with a 50% event rate in the control arm at 2 years. One hundred twenty patients are required to achieve 80% power to detect a true difference of this magnitude with a two-sided alpha error of 0.05. The primary endpoint is a triple composite that includes cardiovascular rehospitalization and death, which will increase event rates at an estimated 10%/year, individually [6, 8, 26, 27].
The primary endpoint analysis will be a time to event analysis and account for censored observations for all randomized subjects. Intention to treat analysis will be used for this endpoint; the analysis will be “analyzed as randomized” regardless of the actual treatment patients receive during the follow-up period. Kaplan-Meier estimates of the primary endpoint and overall survival will be generated along with 95% confidence intervals for the median time to event or death [28]. Log-rank test will be used to compare the hazard functions between the two groups. Cox regression models will be fit to assess and adjust for baseline covariates. The median time to ICD shock as well as the 95% confidence intervals will be reported for both groups. The event free-survival probability as well as the 95% confidence intervals at average 24-month follow-up for both groups will be presented. Adverse events will be tabulated by type and level of severity and compared between groups using chi-square or Fisher exact tests.
Interim analyses will be generated by the coordinating center annually after all sites are activated. A Peto-Haybittle efficacy monitoring boundary will be used: if the p value for the difference between groups is < 0.001, early stopping of the trial will be considered. Using this monitoring bound, the p value for statistical significance at the final analysis will remain at the nominal 0.05 level.
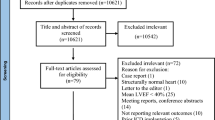
5.1 Study organization and status
We anticipate enrollment of 120 patients at 10–12 institutions with extensive experience in complex ablation procedures. As a conservative estimate, enrollment will occur over a 2–3-year period after all sites are activated. Each participating site will initiate and obtain approval for participation in the study in accordance with their local IRB. Each participating site is responsible for the conduct of the study. Protocol deviations should be tracked and managed by each site, and reported according to the site’s IRB/EC policies. At the completion of the trial, all patient-level data, including protocol deviation should be reported to the study coordinating site at the University of Chicago. The study coordinating site will provide each site with standardized template CRFs to assist with data collection. Data recorded on CRFs must be verifiable by source documentation at the research center such as procedure reports, progress notes, discharge summaries, medication logs, and laboratory reports. Each site is responsible for its own data monitoring and all patient-level data will be reported to the study coordinating site from each participating center at the completion of the trial.
Significant adverse events must be reported to the study sponsor within 24 h in the event of death and 48 h for serious adverse events defined as deteriorations in health that life-threatening, result in permanent impairment, or require surgical intervention to prevent permanent impairment. Unanticipated adverse device effects which are life-threatening should be reported to the coordinating center within 24 h, and at the latest 10 days.
Submission to clinicaltrials.gov from the study-coordinating site was filed on July 26, 2016 and official registration was first posted July 28, 2016. The first patient was randomized on 11/30/15 and a total of 22 patients were randomized at the individual sites prior to registration. Submission to clinicaltrials.gov registration was delayed inadvertently due to institutional relocation of the principal investigator and the need for additional clarification of the role of US coordinating center for a trial conducted exclusively in Asia. During this 7-month period, the study sponsor did not receive any patient-level data regarding procedural information, outcomes, or clinical follow-up.
6 Discussion
PAUSE-SCD is the first prospective, multi-center, and randomized controlled VT ablation trial in Asia. It represents unprecedented collaboration between specialized centers in China, Taiwan, Japan, and Korea and is the first VT ablation trial designed to include patients with nonischemic etiologies. Additionally, prior ablation trials were not performed using multi-electrode catheters with epicardial mapping encouraged in the trial design [29]. As ICD therapy has incomplete penetration across Asia, a prospective cohort examining the natural history of patients undergoing VT ablation as primary therapy that refuse ICD implantation holds promise to provide important insights into the relative efficacy for prevention of SCD between catheter ablation and ICD.
ICD therapy remains the most effective abortive strategy for sudden death due to ventricular arrhythmias. The recent DANISH trial demonstrated that data from post-infarction studies may not be generalizable to the patients with nonischemic etiologies of cardiomyopathy, where the relative efficacy of ICD was not demonstrated [30]. However, patients that receive ICD shocks and therapies are at increased risk for mortality. Whether the association between ICD shocks and subsequent mortality reflects VT as a surrogate marker of end-stage heart failure or highlights the deleterious effects of electrical shocks on myocardial function remains unknown. The recurrence of VT after ablation has been shown to portend a seven-fold risk for transplant and mortality in the largest retrospective multi-center collaborative study to date [8]. Randomized prospective trials are necessary and PAUSE-SCD presents an important opportunity to advance the current scientific and clinical understanding of the management of patients at risk for SCD.
7 Conclusion
The PAUSE-SCD catheter ablation trial is a prospective, multi-center, randomized, and controlled clinical trial that will examine the impact of preemptive catheter ablation on cardiovascular outcomes in patients with an indication for ICD at risk for recurrent VT and SCD. It represents the first multi-center VT ablation study in Asia, with a design intended to provide insights into the role of both ICD and ablation therapy in a predominantly nonischemic population.
References
Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–63.
Poole JE, Johnson GW, Hellkamp AS, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359:1009–17.
Carbucicchio C, Santamaria M, Trevisi N, Maccabelli G, Giraldi F, Fassini G, et al. Catheter ablation for the treatment of electrical storm in patients with implantable cardioverter-defibrillators: short- and long-term outcomes in a prospective single-center study. Circulation. 2008;117:462–9.
Della Bella P, Baratto F, Tsiachris D, et al. Management of ventricular tachycardia in the setting of a dedicated unit for the treatment of complex ventricular arrhythmias: long-term outcome after ablation. Circulation. 2013;127:1359–68.
Tanner H, Hindricks G, Volkmer M, Furniss S, Kuhlkamp V, Lacroix D, et al. Catheter ablation of recurrent scar-related ventricular tachycardia using electroanatomical mapping and irrigated ablation technology: results of the prospective multicenter Euro-VT-study. J Cardiovasc Electrophysiol. 2010;21:47–53.
Stevenson WG, Wilber DJ, Natale A, et al. Irrigated radiofrequency catheter ablation guided by electroanatomic mapping for recurrent ventricular tachycardia after myocardial infarction: the multicenter thermocool ventricular tachycardia ablation trial. Circulation. 2008;118:2773–82.
Marchlinski FE, Callans DJ, Gottlieb CD, Zado E. Linear ablation lesions for control of unmappable ventricular tachycardia in patients with ischemic and nonischemic cardiomyopathy. Circulation. 2000;101:1288–96.
Tung R, Vaseghi M, Frankel DS, et al. Freedom from recurrent ventricular tachycardia after catheter ablation is associated with improved survival in patients with structural heart disease: an International VT Ablation Center Collaborative Group study. Heart Rhythm. 2015;12:1997–2007.
Reddy VY, Reynolds MR, Neuzil P, Richardson AW, Taborsky M, Jongnarangsin K, et al. Prophylactic catheter ablation for the prevention of defibrillator therapy. N Engl J Med. 2007;357:2657–65.
Kuck KH, Schaumann A, Eckardt L, Willems S, Ventura R, Delacretaz E, et al. Catheter ablation of stable ventricular tachycardia before defibrillator implantation in patients with coronary heart disease (VTACH): a multicentre randomised controlled trial. Lancet. 2010;375:31–40.
Sacher F, Tedrow UB, Field ME, Raymond JM, Koplan BA, Epstein LM, et al. Ventricular tachycardia ablation: evolution of patients and procedures over 8 years. Circ Arrhythm Electrophysiol. 2008;1:153–61.
Tung R, Michowitz Y, Yu R, et al. Epicardial ablation of ventricular tachycardia: an institutional experience of safety and efficacy. Heart Rhythm. 2013;10:490–8.
Murakoshi N, Aonuma K. Epidemiology of arrhythmias and sudden cardiac death in Asia. Circ J. 2013;77:2419–31.
Hua W, Zhang LF, Wu YF, et al. Incidence of sudden cardiac death in China: analysis of 4 regional populations. J Am Coll Cardiol. 2009;54:1110–8.
Chan NY. Sudden cardiac death in Asia and China: are we different? J Am Coll Cardiol. 2016;67:590–2.
Chia YMF, Teng TK, Tan ESJ, et al. Disparity between indications for and utilization of implantable cardioverter defibrillators in Asian patients with heart failure. Circ Cardiovasc Qual Outcomes. 2017;10.
Chan LL, Lim CP, Aung ST, Quetua P, Ho KL, Chong D, et al. Patient barriers to implantable cardioverter defibrillator implantation for the primary prevention of sudden cardiac death in patients with heart failure and reduced ejection fraction. Singap Med J. 2016;57:182–7.
Tung R, Nakahara S, Maccabelli G, Buch E, Wiener I, Boyle NG, et al. Ultra high-density multipolar mapping with double ventricular access: a novel technique for ablation of ventricular tachycardia. J Cardiovasc Electrophysiol. 2011;22:49–56.
Stevenson WG, Sager PT, Natterson PD, Saxon LA, Middlekauff HR, Wiener I. Relation of pace mapping QRS configuration and conduction delay to ventricular tachycardia reentry circuits in human infarct scars. J Am Coll Cardiol. 1995;26:481–8.
Tung R, Mathuria N, Michowitz Y, Yu R, Buch E, Bradfield J, et al. Functional pace-mapping responses for identification of targets for catheter ablation of scar-mediated ventricular tachycardia. Circ Arrhythm Electrophysiol. 2012;5:264–72.
Irie T, Yu R, Bradfield JS, et al. Relationship between sinus rhythm late activation zones and critical sites for scar-related ventricular tachycardia: systematic analysis of isochronal late activation mapping. Circ Arrhythm Electrophysiol. 2015;8:390–9.
Di Biase L, Santangeli P, Burkhardt DJ, et al. Endo-epicardial homogenization of the scar versus limited substrate ablation for the treatment of electrical storms in patients with ischemic cardiomyopathy. J Am Coll Cardiol. 2012;60:132–41.
Jais P, Maury P, Khairy P, et al. Elimination of local abnormal ventricular activities: a new end point for substrate modification in patients with scar-related ventricular tachycardia. Circulation. 2012;125:2184–96.
Vergara P, Trevisi N, Ricco A, Petracca F, Baratto F, Cireddu M, et al. Late potentials abolition as an additional technique for reduction of arrhythmia recurrence in scar related ventricular tachycardia ablation. J Cardiovasc Electrophysiol. 2012;23:621–7.
Raitt MH, Klein RC, Wyse DG, et al. Comparison of arrhythmia recurrence in patients presenting with ventricular fibrillation versus ventricular tachycardia in the Antiarrhythmics Versus Implantable Defibrillators (AVID) trial. Am J Cardiol. 2003;91:812–6.
Gokoglan Y, Mohanty S, Gianni C, et al. Scar homogenization versus limited-substrate ablation in patients with nonischemic cardiomyopathy and ventricular tachycardia. J Am Coll Cardiol. 2016;68:1990–8.
Di Biase L, Burkhardt JD, Lakkireddy D, et al. Ablation of stable VTs versus substrate ablation in ischemic cardiomyopathy: the VISTA randomized multicenter trial. J Am Coll Cardiol. 2015;66:2872–82.
Brookmeyer RCJ. A confidence interval for the median survival time. Biometrics. 1982;38:29–41.
Yamashita S, Cochet H, Sacher F, et al. Impact of new technologies and approaches for post-myocardial infarction ventricular tachycardia ablation during long-term follow-up. Circ Arrhythm Electrophysiol. 2016;9.
Kober L, Thune JJ, Nielsen JC, et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med. 2016;375:1221–30.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, M., Wu, S., Yao, Y. et al. Pan-Asia United States PrEvention of Sudden Cardiac Death Catheter Ablation Trial (PAUSE-SCD): rationale and study design. J Interv Card Electrophysiol 57, 271–278 (2020). https://doi.org/10.1007/s10840-019-00535-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00535-w