Abstract
Background
Obstructive sleep apnoea (OSA) is associated with cardiovascular morbidity and mortality, including atrial arrhythmias. Continuous positive airway pressure (CPAP) is the gold standard treatment for OSA; its impact on atrial electrical remodelling has not been fully investigated. Signal-averaged p-wave (SAPW) duration is an accepted marker for atrial electrical remodelling.
Objective
The objective of this study is to determine whether CPAP induces reverse atrial electrical remodelling in patients with severe OSA.
Methods
Consecutive patients attending the Sleep Disorder Clinic at Kingston General Hospital underwent full polysomnography. OSA-negative controls and severe OSA were defined as apnoea–hypopnea index (AHI) < 5 events/hour and AHI ≥ 30 events/hour, respectively. SAPW duration was determined at baseline and after 4–6 weeks of CPAP in severe OSA patients or without intervention controls.
Results
Nineteen severe OSA patients and 10 controls were included in the analysis. Mean AHI and minimum oxygen saturation were 41.4 ± 10.1 events/hour and 80.5 ± 6.5 % in severe OSA patients and 2.8 ± 1.2 events/hour and 91.4 ± 2.1 % in controls. At baseline, severe OSA patients had a greater SAPW duration than controls (131.9 ± 10.4 vs 122.8 ± 10.5 ms; p = 0.02). After CPAP, there was a significant reduction of SAPW duration in severe OSA patients (131.9 ± 10.4 to 126.2 ± 8.8 ms; p < 0.001), while SAPW duration did not change after 4–6 weeks in controls.
Conclusion
CPAP induced reverse atrial electrical remodelling in patients with severe OSA as represented by a significant reduction in SAPW duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Obstructive sleep apnoea (OSA) is the most common form of sleep-disordered breathing caused by the complete or partial occlusion of the upper airway, resulting in the reduction or cessation of breathing during sleep. It is estimated that amongst the middle-aged population, 4 % of men and 2 % of women are affected by sleep apnoea, and up to 5 % of adults in western countries have undiagnosed OSA [1]. The gold standard for diagnosis of OSA is overnight polysomnography, during which severity can be characterised by the number of apnoeas and hypopneas per hour of sleep, the apnoea–hypopnea index (AHI). Accepted AHI cut-points of 5, 15, and 30 are used to indicate mild, moderate, and severe OSA, respectively. The standard treatment for OSA is continuous positive airway pressure (CPAP) with a mask connected to equipment that continuously delivers positive pressure to prevent the airway from collapsing during sleep [2].
OSA has been increasingly recognised as a significant cause of morbidity and mortality, particularly through its effects on the cardiovascular system. It is associated with systemic and pulmonary hypertension, coronary artery disease, congestive heart failure, and arrhythmias [3]. Atrial fibrillation (AF) has received substantial attention as an arrhythmia associated with OSA, since it is the most common arrhythmia and is responsible for a third of arrhythmia hospitalisations [4]. Moreover, since OSA is an independent risk factor for stroke, it may increase stroke risk in patients with AF [5]. Many studies have established a connection between OSA severity and the frequency of AF [6]. The pathophysiology linking OSA to AF is multifactorial and may involve repetitive hypoxemia, increased sympathetic drive, fluctuations in intrathoracic pressure and systemic inflammation [7]. These physiological changes may induce structural and electrical remodelling serving as a substrate to the development of AF [8].
An indirect marker for such electrical remodelling is the prolongation of atrial conduction time, represented by increased maximum p-wave duration. Atrial conduction time can be quantitatively measured using an electrocardiogram (ECG) by measuring the maximum p-wave duration (Pmax) and/or p-wave dispersion (Pd), the difference between maximum and minimum p-wave duration. In various clinical settings, increases in Pmax and Pd indicate prolonged atrial conduction and an inhomogeneous propagation of sinus impulses, a predictor for AF development [9]. An increased Pmax and Pd has been associated with OSA [8]. Signal-averaged p-wave (SAPW) duration was used as a marker for atrial electrical remodelling [10]. The SAPW duration represents the average of all p-wave durations in a given number of consecutive heart beats. The shortening of SAPW duration and surface p-wave duration represents more rapid inter-atrial conduction and provides evidence for reverse atrial electrical remodelling [11]. In addition, an increase in the root mean square voltage of the last 20 ms of the signal-averaged p wave (RMS-20) suggests a reduction in low amplitude terminal p-wave signals (atrial late potentials) [12, 13]. Although CPAP has been proven to be beneficial in reducing respiratory symptoms accompanied by OSA, there is growing evidence to suggest that CPAP also lowers the incidence of AF [14].
The purpose of this study was to quantify SAPW duration in patients with severe OSA and to determine whether CPAP induced reverse atrial electrical remodelling, manifested by a shortened SAPW duration after 4–6 weeks.
2 Methods
2.1 Overview
During March 2009 to March 2011, patients who visited the Sleep Disorder Clinic at Kingston General Hospital in Kingston, ON, Canada, were clinically screened by attending physicians for potential recruitment to the study. The details of the study were presented and explained thoroughly to the patient in both oral and written form. After obtaining informed consent, the patient’s age, weight, height, medical history, and medications were collected and recorded. An initial SAPW recording was performed immediately. The patients subsequently attended their scheduled polysomnography or split-night polysomnography as per standard clinical practice, and their AHI and/or post-CPAP AHI was documented.
Each patient was assigned to one of two groups: severe OSA (AHI ≥ 30) or control (AHI <5). Exclusion criteria included patients who had/were unable to provide informed consent, a history of abnormal baseline ECG abnormalities, a permanent pacemaker or implantable cardioverter defibrillator, a history of congenital heart disease, previous mitral valve surgery, taking beta-blockers or anti-arrhythmics, central sleep apnoea or unanalysable SAPW data.
Patients in the severe OSA group were given an appropriate prescription of CPAP treatment and were invited for a second SAPW recording following 4–6 weeks of compliant treatment. Patients in the control group received no treatment and were also asked to return for a second SAPW recording 4–6 weeks after the initial recording.
2.2 Polysomnography
Standard overnight polysomnography was conducted on all patients after the initial clinical visit. This included four electroencephalography channels (two central, C3-A2 and C4-A1, and two occipital, O2-A1 and O1-A2), two extraoculography channels, submental electromyography (EMG), finger pulse oximetry, lead II ECG, thoracic and abdominal movement (piezoelectric bands), right and left anterior tibialis EMG, diaphragmatic surface EMG, and snore vibration sensor. Airflow was measured with a nasal cannula pressure transducer and an oral thermistor. Blood pressure was also monitored throughout the study using a finger cuff. The recording duration was the patient’s total sleep time. Standard criteria were used by sleep lab technicians for sleep stage scoring [15] and scoring of respiratory events [16]. The diagnosis of OSA was determined by physicians primarily based on the AHI and nadir oxygen saturation.
2.3 Split-night Polysomnography
After the initial clinical examination, if considered appropriate by the physician, a split-night polysomnography was carried out. In this case, the sleep lab technicians would introduce CPAP treatment during polysomnography after making adequate observations supporting the presence OSA and the need for CPAP. The patient would be awakened during polysomnography to be connected to the CPAP machine. Post-CPAP AHI and nadir oxygen saturation were recorded.
2.4 High-resolution p-wave signal averaging
SAPW recordings were conducted on all patients at initial visit and 4–6 weeks thereafter for controls and after 4–6 weeks of CPAP treatment for OSA patients. Careful skin preparation and positioning of silver–silver chloride electrodes in an orthogonal manner preceded the recordings. Shielded cables were attached to the digital Holter monitor (SpiderView, Milan, Italy), and the patients lay still for 10 min during data acquisition. Derived analogue signals were amplified 10,000 times and band pass filtered between 1 and 300 Hz. The lead exhibiting the clearest p-wave was then further band pass filtered between 20 and 50 Hz and used as a trigger to align subsequent p-waves for signal averaging. The analogue data was sampled at 1 kHz with 12-bit resolution. Approximately 600 beats were stored for offline analysis, and 100 beats with a final filtered noise of <0.2 mV were averaged using SAPW analysis software in order to provide one value for SAPW duration and one value for RMS-20 [11]. The investigator scoring SAPW was blinded to the polysomnographic results.
2.5 Statistical analysis
Data were entered into a Microsoft Excel spreadsheet and imported into SPSS (Version 16.0, SPSS Incorporated, Chicago, IL, USA, 2007). All data were expressed as the mean ± SD or frequency expressed as percentage. For continuous variables, statistical differences were determined using independent t test between groups and paired Student’s t test within groups. Fisher’s exact test was performed for discrete clinical variables. Associations of SAPW measurements with clinical and polysomnographic variables were assessed by the Pearson’s correlation coefficient. A two-tailed p < 0.05 was considered statistically significant.
3 Results
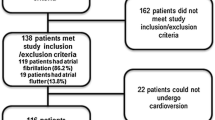
Baseline clinical characteristics and polysomnography measurements of the study population are shown in Table 1. A total of 73 patients were recruited to the study. Forty-four patients were excluded for the following reasons: mild or moderate OSA (n = 18), lost to follow-up (n = 8), no polysomnography results (n = 6), patient withdrawal (n = 4), no CPAP treatment (n = 3), central sleep apnoea (n = 2), unanalysable SAPW recording (n = 2), and history of AF (n = 1). Of the 29 patients included in the final analysis, 19 were severe OSA patients and 10 were controls. Mean AHI and minimum O2 saturation were 41.4 ± 10.1 events/hour (range, 30–60) and 80.5 ± 6.5 % in severe OSA and 2.8 ± 1.2 (range, 1.4–4.7) events/hour and 91.4 ± 2.1 % in controls, respectively. Amongst the clinical characteristics, only body mass index (BMI) was significantly different, with the severe OSA patients demonstrating an overall greater BMI than controls (34.3 ± 5.4 vs 26.6 ± 4.6 kg/m2; p < 0.001).
The mean SAPW duration of severe OSA patients and controls are summarised in Table 2. At baseline, severe OSA patients had a greater SAPW duration than control patients (131.9 ± 10.4 vs 122.8 ± 10.5 ms; p = 0.04). After treating with CPAP for 4–6 weeks, there was a significant reduction of SAPW duration in severe OSA patients (131.9 ± 10.4 to 126.2 ± 8.8 ms; p < 0.001), and the SAPW duration post-CPAP in severe OSA did not differ significantly from control patients (126.2 ± 8.8 vs 122.6 ± 10.9 ms; p = 0.4). Similarly, the subgroup of severe OSA patients who underwent split-night polysomnography (n = 8) also demonstrated a reduction in SAPW duration after 4–6 weeks of CPAP treatment (132.3 ± 10.8 to 125.6 ± 8.8 ms; p < 0.001). In control patients, the mean SAPW duration did not change after 4–6 weeks (122.8 ± 10.5 to 122.6 ± 10.9 ms; p = 0.8). A sample SAPW recording is shown in Fig. 1.
Sample signal-averaged p-wave analyses (SAPW) for a severe obstructive sleep apnoea (OSA) patient (a, b) and control patient (c, d). There is a reduction in SAPW duration after 4–6 weeks of continuous positive airway pressure (CPAP) in the severe OSA patient, but no change in the control patient. The area in grey represents the average p-wave of 100 beats. The x-axis represents time in milliseconds, while the y-axis represents amplitude in microvolts. Reproduced with permission [24]
At baseline, SAPW duration was moderately positively correlated with AHI (r = 0.40; p = 0.03; Fig. 2). Baseline SAPW duration was also positively correlated with age (r = 0.49; p = 0.007) and BMI (r = 0.43; p = 0.02).
The RMS-20 in the severe OSA group was 3.52 ± 2.37 μV at baseline and 3.05 ± 1.94 μV post-CPAP (p = NS). In the control group, the RMS-20 was 2.75 ± 1.44 μV and 2.87 ±1.92 μV (p = NS); respectively.
After treating with CPAP for 4–6 weeks, all severe OSA patients demonstrated a shortening of SAPW duration ranging from 1 to 11 ms. The reduction in SAPW duration was positively correlated with AHI (r = 0.450; p = 0.05) and baseline SAPW duration (r = 0.640; p = 0.003).
4 Discussion
The main findings of this study are that in patients with severe OSA: (1) SAPW duration is increased compared to control patients, (2) SAPW is correlated with the severity of the disease and (3) CPAP treatment reduces the SAPW duration.
Our population of severe OSA patients demonstrated a greater SAPW duration than control patients before receiving CPAP treatment (p = 0.04). The increase in SAPW, approximating 10 ms, may represent inter-atrial conduction disturbance and slowed atrial conduction. Furthermore, this study also showed that SAPW duration increases with OSA severity (p = 0.03). Although the specific pathophysiology involved in this process is not fully known, OSA is associated with multiple cardiac structural and functional abnormalities such as atrial enlargement, ventricular hypertrophy and left ventricular dysfunction [7]. Repetitive inspiratory efforts against the occluded airway generate significant shifts in intrathoracic pressure that can approach −65 mmHg, increasing cardiac wall stress and atrial size [7]. Heightened sympathetic tone and endothelial dysfunction associated with OSA elevate systemic blood pressure, increase afterload, and consequently promote ventricular hypertrophy [7]. Furthermore, OSA has been reported to induce atrial remodelling at the structural and electrical level, which may be implicated in the development of cardiac arrhythmias [8, 17]. This may account for a prior observation that the AF prevalence is almost 5 % in patients with an AHI ≥ 30, about fivefold higher than those with an AHI ≤ 5 [18]. Similarly, the proportion of OSA patients is significantly higher in patients with AF than in high-risk cardiovascular patients without AF (49 % vs 32 %; p = 0.0004) [19].
This is the first study to measure SAPW duration in OSA patients. The findings of this study are consistent with a recent study that reported an increase in Pmax of 7.6 ms and Pd (14.6 ± 7.5 vs 8.9 ± 3.1 ms; p < 0.001) in moderate–severe OSA patients [8]. An earlier study also consistently reported an increased Pmax in severe OSA compared to controls (128.9 ± 10.7 vs 101.2 ± 11.8 ms; p < 0.001) and in mild–moderate OSA compared to controls (117.5 ± 13.7 vs 101.2 ± 11.8 ms; p < 0.001) [20]. In the latter study, the increase in p-wave duration in severe OSA patients was almost 30 ms, about threefold greater than our findings. However, their electrocardiographic data were derived from 12-lead surface ECG tracings with manually derived measurements, a less reliable technique than SAPW duration. Therefore, differences in the chosen p-wave duration markers and/or the study population may account for this discrepancy.
Although prolongation of p-wave duration is a known predictor for AF, the direct measurement of SAPW as a predictor for AF has not been established. Healey et al. and Chalfoun et al. [21, 22] demonstrated that the change in SAPW, not the direct measurement of SAPW, can predict the recurrence of AF. Can et al. [20] showed that the severity of OSA was positively correlated with Pmax (r = 0.44; p = 0.002) and Pd (r = 0.56; p < 0.001). Clinically, these findings at the electrophysiological level may translate into a greater risk of AF. A Japanese study involving 1,763 patients reported an odds ratio for AF of 2.47 for mild sleep apnoea (5 ≤ AHI < 15) and 5.66 for moderate–severe sleep apnoea (AHI ≥ 15) after adjusting for confounders, suggesting the association of sleep apnoea and AF is correlated with the severity of OSA [23]. In another cohort of 3,542 patients with no previous history of AF, the diagnosis and severity of OSA predicted the incidence of AF over a period of 5 years [24]. Although cardiovascular co-morbidities shared by OSA and AF obscure an obvious etiological link between them, the findings of the present study at least strengthen the relationship observed between them.
There is growing evidence that suggests CPAP can lower the incidence of arrhythmias in OSA patients. Kanagala et al. [14] reported a lower rate of AF recurrence after cardioversion in OSA patients treated with CPAP compared to untreated patients (42 vs 82 %; p = 0.01). Moreover, control patients without diagnosed OSA showed a recurrence rate of 53 %, significantly lower than that of untreated OSA patients. In another study, the use of CPAP abolished pathologically significant rhythm disturbances in seven of the eight severe OSA patients [25].
In this study, the use of CPAP for 4–6 weeks reduced SAPW duration by approximately 6 ms in the severe OSA patient group (131.9 ± 10.4 to 126.2 ± 8.8 ms; p < 0.001), indicating a reversal of atrial electrical remodelling associated with OSA. Furthermore, no change in SAPW duration was observed in controls, which supports that the change observed in severe OSA was not due to variability of the SAPW measurement. Previous studies have reported a decrease of about 6 ms 3 days post-cardioversion [21], and 13 ms 30 days post-cardioversion [22], which continued for at least 3 months.
The changes in SAPW duration demonstrated may indicate a restoration of electrical and structural changes. Previous studies have observed concurrent reduction in left atrial (LA) volume and SAPW duration in other clinical settings, such as mitral commissurotomy [26]. LA volume has also been shown to be reduced following catheter ablation of AF, resulting in a reduction of AF recurrence [26]. In the setting of sleep apnoea, Oliveira et al. [27] found that patients who received CPAP treatment for 24 weeks demonstrated a significantly increased LA passive emptying fraction (28.8–46.8 %; p = 0.01) and a decreased LA active emptying fraction (42.7–25.7 %; p < 0.01) compared to those who received sham CPAP. Another study demonstrated an increase in LA volume in CPAP-noncompliant patients (15.5 ± 22.3 mL; p < 0.006) after a mean of approximately 16 months [17]. Despite a non-significant decrease in LA volume in CPAP-compliant patients (3.5 ± 16.6 mL; p = 0.65), CPAP showed a protective effect in the prevention of LA structural remodelling. The mechanisms by which CPAP induces structural and/or electrical changes ultimately decreasing the incidence of AF are likely multifactorial and may involve beneficial physiological effects involving reversal of hypertension, increased sympathetic drive, and systemic inflammation [7]. The knowledge that current OSA therapies may potentially reduce the incidence or recurrence of AF not only emphasises the importance of treating OSA but also strengthens the causative relationship between OSA and AF.
5 Limitations
This study had several limitations. The study group involved a small number of patients. A larger sample size would have permitted multiple linear regressions to identify predictors for SAPW duration independent of confounders. For instance, there was a positive correlation between SAPW duration and BMI in our study. At baseline, BMI was significantly greater in severe OSA, which may have contributed to the increased SAPW duration compared to controls. However, the reduction in SAPW after CPAP despite a constant BMI and age supports that the prolongation of SAPW was primarily a result of the disease itself.
Our study took place over 4–6 weeks. A longer study period would allow for more frequent analyses and longer-term data providing additional insight into the temporality of reverse atrial electrical remodelling and the incidence of outcomes such as AF.
There were no echocardiographic data available to correlate changes in SAPW duration with changes in atrial size, if any, after CPAP treatment. The echocardiographic data would allow for the determination of whether reverse atrial electrical remodelling is associated with structural changes of the atria and may further elucidate the pathophysiology of electrical remodelling in OSA. Nonetheless, the findings of this study suggest that atrial electrical remodelling could be reversed by CPAP. Finally, no electrolyte status was measured during the course of the study.
6 Conclusion
SAPW duration is prolonged in severe OSA patients and is correlated with sleep apnoea severity. SAPW duration is decreased over 4–6 weeks of CPAP use. This provides evidence for reverse atrial electrical remodelling that may be resolved by treating the underlying disease. Larger long-term studies are needed confirm these findings and extend them to clinically applicable situations.
Abbreviations
- AF:
-
Atrial fibrillation
- AHI:
-
Apnoea–hypopnea index
- BMI:
-
Body mass index
- CPAP:
-
Continuous positive airway pressure
- ECG:
-
Electrocardiogram
- EMG:
-
Electromyography
- Hz:
-
Hertz
- kHz:
-
Kilohertz
- LA:
-
Left atrial
- OSA:
-
Obstructive sleep apnoea
- mL:
-
Milliliter
- ms:
-
Millisecond
- mV:
-
Millivolt
- Pd:
-
p-Wave dispersion
- Pmax:
-
Maximum p-wave duration
- SAPW:
-
Signal-averaged p-wave
References
Young, T., Peppard, P. E., & Gottlieb, D. J. (2002). Epidemiology of obstructive sleep apnea: a population health perspective. American Journal of Respiratory and Critical Care Medicine, 165, 1217–1239.
Ballester, E., Badia, J. R., Hernandez, L., Carrasco, E., de Pablo, J., Fornas, C., et al. (1999). Evidence of the effectiveness of continuous positive airway pressure in the treatment of sleep apnea/hypopnea syndrome. American Journal of Respiratory and Critical Care Medicine, 159, 495–501.
Young, T., Skatrud, J., & Peppard, P. E. (2004). Risk factors for obstructive sleep apnea in adults. JAMA: The Journal of the American Medical Association, 291, 2013–2016.
Fuster, V., Ryden, L. E., Cannom, D. S., Crijns, H. J., Curtis, A. B., Ellenbogen, K. A., et al. (2006). ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines. Circulation, 114, e257–e354.
Yazdan-Ashoori, P., & Baranchuk, A. (2011). Obstructive sleep apnea may increase the risk of stroke in AF patients: refining the CHADS2 score. International Journal of Cardiology, 146, 131–133.
Todd, K., McIntyre, W. F., & Baranchuk, A. (2010). Obstructive sleep apnea and atrial fibrillation: a review of the literature. Nature and Science of Sleep, 2, 39–45.
Somers, V. K., White, D. P., Amin, R., Abraham, W. T., Costa, F., Culebras, A., et al. (2008). Sleep apnea and cardiovascular disease: an American Heart Association/American College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. Circulation, 118, 1080–1111.
Baranchuk, A., Parfrey, B., Lim, L., Morriello, F., Simpson, C. S., Hopman, W. H., et al. (2011). Interatrial block in patients with obstructive sleep apnea. Cardiology Journal, 18, 171–175.
Dilaveris, P. E., & Gialafos, J. E. (2001). P-wave dispersion: a novel predictor of paroxysmal atrial fibrillation. Annals of Noninvasive Electrocardiology, 6, 159–165.
Fukunami, M., Yamada, T., Ohmori, M., Kumagai, K., Umemoto, K., Sakai, A., et al. (1991). Detection of patients at risk for paroxysmal atrial fibrillation during sinus rhythm by P wave-triggered signal-averaged electrocardiogram. Circulation, 83, 162–169.
Redfearn, D. P., Skanes, A. C., Lane, J., & Stafford, P. J. (2006). Signal-averaged P wave reflects change in atrial electrophysiological substrate afforded by verapamil following cardioversion from atrial fibrillation. Pacing and Clinical Electrophysiology, 29, 1089–1095.
Stafford, P. J., Robinson, D., & Vincent, R. (1995). Optimal analysis of the signal averaged P wave in patients with paroxysmal atrial fibrillation. British Heart Journal, 74, 413–418.
Opolski, G., Ścisłoa, J. S., Góreckia, A., Steckiewiczb, R., & Torbickia, R. (1997). Detection of patients at risk for recurrence of atrial fibrillation after successful electrical cardioversion by signal-averaged P-wave ECG. International Journal of Cardiology, 60(2), 181–185.
Kanagala, R., Murali, N. S., Friedman, P. A., Ammash, N. M., Gersh, B. J., Ballman, K. V., et al. (2003). Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation, 107, 2589–2594.
Rechtschaffen, A., & Kales, A. (1968). A manual of standardized terminology, techniques, and scoring system for sleep stages of human subjects. Washington: US Government Printing Office, US Public Health Service. NIH publication no. 204.
(1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep, 22, 667–89.
Khan, A., Latif, F., Hawkins, B., Tawk, M., Sivaram, C. A., & Kinasewitz, G. (2008). Effects of obstructive sleep apnea treatment on left atrial volume and left atrial volume index. Sleep & Breathing, 12, 141–147.
Mehra, R., Benjamin, E. J., Shahar, E., Gottlieb, D. J., Nawabit, R., Kirchner, H. L., et al. (2006). Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. American Journal of Respiratory and Critical Care Medicine, 173, 910–916.
Gami, A. S., Pressman, G., Caples, S. M., Kanagala, R., Gard, J. J., Davison, D. E., et al. (2004). Association of atrial fibrillation and obstructive sleep apnea. Circulation, 110, 364–367.
Can, I., Aytemir, K., Demir, A. U., Deniz, A., Ciftci, O., Tokgozoglu, L., et al. (2009). P-wave duration and dispersion in patients with obstructive sleep apnea. International Journal of Cardiology, 133, e85–e89.
Healey, J. S., Theoret-Patrick, P., Green, M. S., Lemery, R., Birnie, D., & Tang, A. S. (2004). Reverse atrial electrical remodelling following atrial defibrillation as determined by signal-averaged ECG. Canadian Journal of Cardiology, 20, 311–315.
Chalfoun, N., Harnick, D., Pe, E., Undavia, M., Mehta, D., & Gomes, J. A. (2007). Reverse electrical remodeling of the atria post cardioversion in patients who remain in sinus rhythm assessed by signal averaging of the P-wave. Pacing and Clinical Electrophysiology, 30, 502–509.
Tanigawa, T., Yamagishi, K., Sakurai, S., Muraki, I., Noda, H., Shimamoto, T., et al. (2006). Arterial oxygen desaturation during sleep and atrial fibrillation. Heart, 92, 1854–1855.
Gami, A. S., Hodge, D. O., Herges, R. M., Olson, E. J., Nykodym, J., Kara, T., et al. (2007). Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. Journal of the American College of Cardiology, 49, 565–571.
Harbison, J., O’Reilly, P., & McNicholas, W. T. (2000). Cardiac rhythm disturbances in the obstructive sleep apnea syndrome: effects of nasal continuous positive airway pressure therapy. Chest, 118, 591–595.
Pang, H., Ronderos, R., Pérez-Riera, A., Femenía, F., & Baranchuk, A. (2011). Reverse atrial electrical remodelling: a systematic review. Cardiology Journal, 18, 625–631.
Oliveira, W., Campos, O., Cintra, F., Matos, L., Vieira, M. L., Rollim, B., et al. (2009). Impact of continuous positive airway pressure treatment on left atrial volume and function in patients with obstructive sleep apnoea assessed by real-time three-dimensional echocardiography. Heart, 95, 1872–1878.
Acknowledgements
We would like to thank Dr. Peter Munt and Dr. Ron Wigle for helping in recruiting patients for the study. This study was supported by an unrestricted grant from the Clinical Teachers’ Association of Queen’s University.
Conflicts of interest
None
Financial disclosures
This study received an unrestricted grant from the Clinical Teachers’ Association of Queen’s University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baranchuk, A., Pang, H., Seaborn, G.E.J. et al. Reverse atrial electrical remodelling induced by continuous positive airway pressure in patients with severe obstructive sleep apnoea. J Interv Card Electrophysiol 36, 247–253 (2013). https://doi.org/10.1007/s10840-012-9749-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-012-9749-3