Abstract
Peer-delivered health models may hold important benefits for family members, yet their prevalence, components, and outcomes are unknown. We conducted a review of peer-delivered services for families of children and adults with serious health problems. Studies of interventions published between 2000 and 2016 were included if the intervention contained a component for family members. Of 88 studies that were assessed for their eligibility, five met criteria. Familial components included information about the health condition and management, strategies to enhance communication and stress, and the provision of emotional support. Outcomes were largely favorable, including reductions in distress and symptoms of trauma, enhanced quality of life, and positive perceptions of the peer therapeutic alliance. Peer-delivered services for family members may hold important benefits to caregivers; however, the research base remains thin. A research agenda to develop and examine these models is discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Family members provide the lion’s share of caregiving to relatives with serious health conditions, with recent estimates indicating that there are approximately 65.7 million people living in the United States, including family members and unpaid caregivers, who are currently providing care to an adult or child with a health problem (Adelman et al. 2014). In many cases, the time commitment, responsibilities, and intensity associated with caregiving are substantial (Reinhard et al. 2008): On average, caregivers spend approximately 20 h per week attending to their relative’s medical needs, coordinating and attending treatment appointments, advocating for their loved one, and providing transportation, information, emotional support, and financial assistance (Adelman et al. 2014; Brown et al. 2008; Dixon et al. 2001; Murphy et al. 2007).
Most informal caregivers, who are also referred to as a shadow workforce (Phillips et al. 2016), and invisible second patients (Brodaty and Donkin 2009), are unprepared to assume the numerous roles and responsibilities associated with caregiving (Adelman et al. 2014; Family Caregiver Alliance 2016), to the detriment of their health and wellbeing. For example, caretaking is associated with role strain and marital discord (Brown et al. 2008; O’Brien et al. 2009), missed workdays, reduced hours and productivity or exiting the workforce completely (Neri et al. 2015; Phillips et al. 2016), significant costs and financial problems (Adelman et al. 2014; Brown et al. 2008). Informal caregivers are at heightened risk for serious threats to their physical and psychological health (Brown et al. 2008; Murphy et al. 2007), including elevated level of stress and emotional distress, particularly if their relative’s illness was unexpected or if the prognosis is uncertain (Brown et al. 2008; O’Brien et al. 2009). One large-scale study of over 10,000 adults, for example, found in comparison to non-caregivers, caregivers of individuals with Alzheimer’s disease evidenced significantly higher rates of minor and major depressive disorder and anxiety, insomnia and high blood pressure, diabetes, and self-reported pain (Laks et al. 2016), while a second study found caregivers of children with cerebral palsy evidenced significantly higher levels of migraines, back pain, ulcers, and general distress comparative to non-caregivers (Murphy et al. 2007).
A constellation of factors, including the availability of resources such as social and financial support, and one’s interpretation of the illness or disease, are thought to portend how family members experience their relative’s illness and accompanying caregiving demands (Desai et al. 2016). However, even families who appear to be managing the various responsibilities associated with caregiving may encounter difficulties periodically, or may need specific supports as they navigate their caretaking role.
One promising effort to support family members is peer-delivered support. Originating in the mental health field alongside the growth of community-based services for families (Hoagwood et al. 2010), peers provide a range of services to adult consumers of the mental health system and caregivers of children with mental health problems, including conveying information about mental illness and treatment, providing emotional support and advocacy services, and facilitating linkages to services (Hoagwood et al. 2010). Defined as persons with similar life experiences who also have a professional role (Hoagwood et al. 2010), peers are perceived as credible role models who instill hope and facilitate engagement in services. Peers are also proposed as a cost-effective alternative to other professionally-run programs, although this has not yet been established (Davidson et al. 2012; Hoagwood et al. 2010).
An important step in understanding the potential utility of peer models in the health field is to describe their prevalence, programmatic components, and benefits to family members. A previous review undertaken (Acri et al. 2016) of peer-delivered programs for family members of children and adults with mental health problems found few were rigorously tested, and while some studies showed family-level benefits in outcomes such as functioning, parental concerns about their child, and parenting skills, other constructs such as parental stress, family support, and coping were unchanged. The authors concluded that future exploration was needed in order to untangle the benefits of peer support for family members, and discern whether there are specific types of services or supports that improve caregiver-level domains for the sake of their own health and wellbeing.
The purpose of this review is to present the state of the evidence regarding peer models that involve families of children and adults with ongoing health conditions, including their prevalence, the types of supports provided, and their impact upon caregiver and relative outcomes. This exploration is essential given the practical needs of caregivers and the consequences of unmet need upon the child or adult with chronic health problems. Among families of both children (Murphy et al. 2007) and adults (Schulz and Martire 2004), caregivers who experience high levels of burden or adverse outcomes are more likely to place their family member outside of the home, and their relatives are more likely to experience functional impairment and hospitalizations. Thus, the identification of supports to reduce the strain associated with caregiving could potentially enhance both caregiver and patient outcomes.
Method
A comprehensive review of peer-delivered models for family members of adults and children with health problems was conducted. The methodological approach that we undertook was identical to our previous review (see Hoagwood et al. 2012). To locate studies, the first author developed a list of search terms within two categories: (1) peers (e.g., peer advocate, lay visitor), which were obtained from keywords cited by experts in the peer health and mental health literature, and (2) health conditions including the general term health, as well as specific conditions and diseases such as diabetes, cancer, and HIV. Search terms were shortened to their base word where applicable, and an asterisk was added to each word to capture all derivatives of that particular term.
Next, search terms within each category were linked with “or,” and larger categories were linked with “and” to capture studies that included at least one search term from all of the categories (e.g., peer interventions for childhood asthma). The search was executed using the PsycINFO and Medline (OVID SP) databases through a university library system. Database search limits included year (2000–2016), and articles written in English.
Inclusion and Exclusion Criteria
Programs were included in they met the following criteria: (1) they were intervention studies, meaning the purpose of the study was to examine the effect of an intervention; (2) they were models, programs, or interventions that were solely or co-delivered by a peer; (3) they provided a service to family members of adults or children with a health condition or disease; (4) they were published between 2000–2016; and, (5) they published data about outcomes. Adhering to Davidson et al. (2006) distinction between peer support services as unidirectional, from peer to recipient, rather than bidirectional and mutually supportive as a way to differentiate these models from consumer-run and self-help groups, programs are excluded if they were peer support groups or consumer-run programs. Additionally, primary prevention programs that did not directly address existing health problems were excluded.
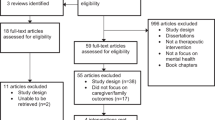
Figure 1 presents the search history and results.
Coding and Analysis
Coding proceeded in multiple stages. First, the lead author reviewed the results of the electronic search. Full text articles of potentially eligible programs were reviewed based upon the previously described inclusion and exclusion criteria. The lead author then developed a coding scheme to assess program elements across studies. Two authors (MA, SZ) separately check coded each of the studies that met initial eligibility. Weekly meetings were held to address questions regarding coding the program elements, and any discrepancies in coding were discussed with all three authors until consensus was met.
Results
As presented in Table 1, five total articles were eligible for inclusion. Of them, three were for adult health problems, and two were for families of children with health problems
Peer Models
Health condition and participants
Two of the three adult health models were for individuals with cancer and their families (Peer Connect; Allicock et al. 2014; ProsCan; Chambers et al. 2013), and the third program, by Tam et al. (2012), was for persons living with HIV and their families. Of the two child health models, one was designed for families of children with Type 1 Diabetes Mellitus (STEP; Sullivan-Bolyai et al. 2010), and the other, the Parent Buddy Program, was for caregivers of infants who were in the NICU due to very preterm birth (Preyde and Ardal 2003). With the exception of Peer Connect (Allicock et al. 2014), the programs were for families of individuals who were either newly diagnosed (Chambers et al. 2013; Preyde and Ardal 2003; Sullivan-Bolyai et al. 2010), or new to start a treatment regimen (Tam et al. 2012). Peer Connect did not restrict eligibility to newly-diagnosed or treated individuals.
Peer characteristics and qualifications
Peers who delivered the adult health models were referred to as Peer Support Volunteers (Chambers et al. 2013), Guides (Allicock et al. 2014), and External Supporters (Tam et al. 2012). A primary requirement for the peer was that they either personally experienced the health condition (Chambers et al. 2013; Tam et al. 2012), or had experience caring for someone with the health condition (Allicock et al. 2014). Peers who delivered both cancer programs had to be at least 1 year post-treatment (Allicock et al. 2014; Chambers et al. 2013). Peers in Tam et al.’s (2012) program were required to take antiretroviral medication, but no stipulations were noted with respect to when they received a diagnosis.
Peers who delivered the child health programs were referred to as Parent Buddies (Preyde and Ardal 2003) and Parent Mentors (Sullivan-Bolyai et al. 2010). In Parent Buddies, caregivers who served as peers were required to demonstrate that they had adjusted to having had a very preterm birth and did not evidence mental health problems such as depression or anxiety (Preyde and Ardal 2003). Peers also needed to display an adequate adjustment in Parent Mentors, and display qualities such as being knowledgeable, adaptable, competent, and work well with members of the child’s medical team (Sullivan-Bolyai et al. 2010).
Peer program components
Four of the programs were delivered primarily by phone; the fifth consisted of in-home visits (Tam et al. 2012). Programs were flexible and relatively short-term, with the frequency of meetings depending on the needs of the family. ProsCan, for example, took place over eight sessions, and sessions were timed to occur before and after the patient’s surgery (prostatectomy). For all programs, families were involved in a wider array of medical and social services and were not restricted from receiving additional supports.
Family member component
The main service provided to family members in Peer Connect (Allicock et al. 2014) and ProsCan (Chambers et al. 2013) was information about the disease and its management. Additionally, peers who delivered ProsCan, which was a program for individuals with prostate cancer and their spouses, provided information about how they could support each other, enhance their communication, manage stress, and on other topics including aging and sexuality. The remaining adult health program for HIV, directed most of the services to the individual; however, the family was involved in identifying barriers to treatment adherence, and the peer worked with family members to resolve and address obstacles to engagement (Tam et al. 2012). For both child models, STEP (Sullivan-Bolyai et al. 2010) and the Parent Buddy Program (Preyde and Ardal 2003) peers provided caregivers, and primarily parents, with information about the health condition and its management and emotional support.
Research Design
Of the three studies of adult health models, one employed a control group drawn from a larger, randomized controlled trial (Tam et al. 2012), Chambers et al. (2013) employed a pre/post design, and Allicock et al. (2014), used a post-only design. In contrast, both studies of the child health models compared the intervention to a control or comparison group; of them, one was a randomized controlled trial (Sullivan-Bolyai et al. 2010); in the second, samples were not randomly selected (Preyde and Ardal 2003).
Outcomes
Adult health models
Studied outcomes focused on the individual, such as quality of life (Allicock et al. 2014; Tam et al. 2012) and treatment adherence (Tam et al. 2012), and both the individual and relatives, including therapeutic alliance (between the couple and the peer), and cancer-related distress (Chambers et al. 2013). Results showed enhancements in the quality of life among persons with severe infections and suppression of their immune system (there was no difference for those without or with mild symptoms) (Tam et al. 2012), reductions in distress post-surgery and improvements in trauma symptoms (e.g., intrusion, avoidance) (Chambers et al. 2013), and enhanced optimism about the future, improved quality of life, and improved perception of their decision making regarding healthcare choices (Allicock et al. 2014).
Child health models
In the two child health model studies, only caregiver outcomes were assessed: Preyde and Ardal (2003) evaluated the impact of the intervention on parent emotional health (e.g., stress, state and trait anxiety, depression). Sullivan-Bolyai et al. (2010) assessed caregiver concerns and confidence about managing their child’s diabetes, as well as the impact of their child’s illness on the family. Both assessed the parents’ perception of social support.
Results were mixed: Sullivan-Bolyai et al. (2010) did not find statistically significant differences between groups on parental concern and confidence about diabetes management, although individuals receiving the peer program noted they found them to be a source of support and advice; however, Preyde and Ardal (2003) did find caregivers, and primarily mothers, who received the program had statistically lower rates of stress, state anxiety, and depression, and higher levels of social support in comparison to the control group.
Discussion
The purpose of this review was to present an overview of peer-delivered interventions for family members of children and adults with health problems. This review, which describes the commonness and components of peer programs and their impact, has important implications for the field, given family members are the defacto providers of care for relatives with health problems, are often called upon to provide a range of supports that they may lack experience or comfort it providing, and are at high risk for strain, burden and distress.
Several findings of this review are notable. First, only five of the 88 articles that were assessed for eligibility met criteria for inclusion. The remainder were excluded primarily because they did not offer support to family members, were not peer-delivered interventions, or did not examine an intervention. The low number of eligible studies suggests that similar to the review of peer models in mental health (Acri et al. 2016), either peer health models have not been developed to the point that evaluations have been conducted, or they have been evaluated using weaker research designs. A future research agenda to develop and test peer health models is needed in order to move the knowledge base forward.
Second, program recipients viewed the programs favorably, and reported important benefits to their emotional health and wellbeing, including enhanced quality of life, reduced symptoms of distress and trauma, and enhanced confidence in healthcare decision-making and treatment adherence. Further, process-related benefits, such as viewing the peer favorably and perceived positive therapeutic alliance, were found across studies. Although promising, these results again suggest a need for subsequent research using more rigorous designs that can more closely discern whether there was some unique benefit derived from having peers deliver the intervention.
And third, both studies of child health models were notable in that all of the outcomes under investigation pertained to the caregiver. Although this may be indicative of an important movement in the management of child health, and specifically, the importance of the health and wellbeing of caregivers, the assessment of child outcomes is also important in its own right. Given an extensive literature that shows the health and wellbeing of caregivers impacts patient health, wellbeing, and institutionalization (Murphy et al. 2007; Schulz and Martire 2004), it is important to also investigate how peer models may influence child outcomes, either independently or mediated by improvements in caregiver health and wellbeing.
This review has important implications for social work practice. At a minimum, it exposes the needs of relatives caring for adults and children with serious health problems, and supports the move from an individualized model of service delivery to a family centered standard of care. At the root of family centered care is the value placed upon family involvement, and core principles of this model include the active collaboration between the family and healthcare providers, respect for the family’s decisions, and the provision of information and parent-delivered support (Foster et al. 2010). Many institutions are moving in this direction: As a case in point, pediatric cancer centers including St. Jude Children’s Research Hospital (2016) and Yale New Haven Hospital (2016) have adopted this model of care, purporting that they see the family as partners in their child’s treatment, are respectful and honor the choices of the family in treatment decisions, share information with the family, and are responsive to the family’s needs. Peer models are complimentary to family centered care, and embedding peer health programs into this system of care may, as seen through this review, hold important benefits to individuals and their families.
Although promising, the above-noted limitations, and in particular that three studies did not include a comparison group, should be considered when interpreting the findings. Additionally, with the exception of one study (Tam et al. 2012), sample sizes were small, which limits the generalizability of the findings and suggests future research with larger samples is needed in order to discern the true benefits of peer models in health for family members.
Nonetheless, this review contributes to our knowledge about peer models and future research directions that are needed in order to advance the peer movement. Specifically, a future research agenda that would advance knowledge in this domain would include developing peer models that address the needs of families, such as providing assistance with navigating the health care system, offering emotional support, and linking families to financial assistance. Although all of the programs included in this review provided information about the health condition and how to manage it, there were few additional supports offered, which is concerning given the numerous and varied responsibilities family members assume when caregiving. To this end, collaborating with family members in the development of peer models will be more likely to enhance the acceptability and relevance of the program, address where family members need the most support, and potentially reduce burden and distress.
Second, testing the outcomes associated with peer models, using larger sample sizes, more rigorous experimental designs, and focusing on outcomes that derive from the literature, such as caregiver distress, work productivity, relationships with others and physical health, will advance knowledge about whether peer models can effectively support family members and enhance the health and wellbeing of children, adult consumers, and their families.
References
Acri, M., Hooley, C.D., Richardson, N., & Moaba, L.B. (2016). Peer models in mental health for caregivers and families. Community Mental Health Journal, 1–9.
Adelman, R. D., Tmanova, L. L., Delgado, D., Dion, S., & Lachs, M. S. (2014). Caregiver burden: A clinical review. The Journal of the American Medical Association, 311(10), 1052–1060.
Allicock, M., Carr, C., Johnson, L. S., Smith, R., Lawrence, M., Kaye, L., et al. (2014). Implementing a one-on-one peer support program for cancer survivors using a motivational interviewing approach: Results and lessons learned. Journal of Cancer Education, 29(1), 91–98.
Brodaty, H., & Donkin, M. (2009). Family caregivers of people with dementia. Dialogues in Clinical Neuroscience, 11(2), 217.
Brown, R. T., Wiener, L., Kupst, M. J., Brennan, T., Behrman, R., Compas, B. E., et al. (2008). Single parents of children with chronic illness: An understudied phenomenon. Journal of Pediatric Psychology, 33(4), 408–421.
Chambers, S. K., Schover, L., Halford, K., Ferguson, M., Gardiner, R. A., Occhipinti, S., et al. (2013). ProsCan for couples: A feasibility study for evaluating peer support within a controlled research design. Psycho‐Oncology, 22(2), 475–479.
Davidson, L., Bellamy, C., Guy, K., & Miller, R. (2012). Peer support among persons with severe mental illnesses: A review of evidence and experience. World psychiatry: official journal of the World Psychiatric Association (WPA), 11(2), 123–128.
Davidson, L., Chinman, M., Sells, D., & Rowe, M. (2006). Peer support among adults with serious mental illness: A report from the field. Schizophrenia Bulletin, 32(3), 443–450.
Desai, P. P., Rivera, A. T., & Backes, E. M. (2016). Latino caregiver coping with children’s chronic health conditions: An integrative literature review. Journal of Pediatric Health Care, 30(2), 108–120.
Dixon, L., McFarlane, W. R., Lefley, H., Lucksted, A., Cohen, M., Falloon, I., et al. (2001). Evidence-based practices for services to families of people with psychiatric disabilities. Psychiatric Services, 52(7), 903–910.
Family Caregiver Alliance (2016). A population at risk. https://www.caregiver.org/caregiver-health.
Foster, M., Whitehead, L., & Maybee, P. (2010). Parents’ and health professionals’ perceptions of family centered care for children in hospital, in developed and developing countries: A review of the literature. International Journal of Nursing Studies, 47(9), 1184–1193.
Hoagwood, K., Cavaleri, M. A., Olin, S., Burns, B., Slaton, E., Gruttadaro, D., et al. (2010). Family support in children’s mental health: A review and synthesis. Clinical Child and Family Psychology Review, 13, 1–45.
Hoagwood, K. E., Jensen, P., Acri, M., Olin, S. S., Lewandowski, E., & Herman, R. (2012). Outcome domains in child mental health research since 1996: Have they changed and why does it matter? Journal of the American Academy of Child & Adolescent Psychiatry, 51(12), 1241–1260.
Laks, J., Goren, A., Dueñas, H., Novick, D., & Kahle‐Wrobleski, K. (2016). Caregiving for patients with alzheimer’s disease or dementia and its association with psychiatric and clinical comorbidities and other health outcomes in Brazil. International Journal of Geriatric Psychiatry, 31(2), 176–185.
Murphy, N. A., Christian, B., Caplin, D. A., & Young, P. C. (2007). The health of caregivers for children with disabilities: Caregiver perspectives. Child: Care, Health and Development, 33(2), 180–187.
Neri, L., Lucidi, V., Catastini, P., & Colombo, C. (2015). Caregiver burden and vocational participation among parents’ of adolescents with CF. Pediatric Pulmonology, 51(3), 243–252.
O’Brien, I., Duffy, A., & Nicholl, H. (2009). Impact of childhood chronic illnesses on siblings: A literature review. British Journal of Nursing, 18(22), 1358–1365
Phillips, S. S., Ragas, D. M., Hajjar, N., Tom, L. S., Dong, X., & Simon, M. A. (2016). Leveraging the experiences of informal caregivers to create future healthcare workforce options. Journal of the American Geriatrics Society, 64(1), 174–180.
Preyde, M., & Ardal, F. (2003). Effectiveness of a parent “buddy” program for mothers of very preterm infants in a neonatal intensive care unit. Canadian Medical Association Journal, 168(8), 969–973.
Reinhard, S. C., Given, B., Petlick, N. H., & Bemis, A. (2008). Supporting family caregivers in providing care. In R. G. Hughes (Ed.), Patient safety and quality: An evidence-based handbook for nurses (Chapter 14). Rockville, MD: Agency for Healthcare Research and Quality.
Schulz, R., & Martire, L. M. (2004). Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. The American Journal of Geriatric Psychiatry, 12(3), 240–249.
St. Jude Children’s Research Hospital (2016). What is patient family centered care? https://www.stjude.org/treatment/patient-resources/family-centered-care.html.
Sullivan-Bolyai, S., Bova, C., Leung, K., Trudeau, A., Lee, M., & Gruppuso, P. (2010). Social support to empower parents (STEP) An intervention for parents of young children newly diagnosed with type 1 diabetes. The Diabetes Educator, 36(1), 88–97.
Tam, V. V., Larsson, M., Pharris, A., Diedrichs, B., Nguyen, H. P., & Nguyen, C. T. K., et al. (2012). Peer support and improved quality of life among persons living with HIV on antiretroviral treatment: A randomised controlled trial from north-eastern Vietnam. Health and Quality of Life Outcomes, 10(1), 1.
Yale New Haven Hospital (2016). What is patient and family centered care? https://www.ynhh.org/services/quality-safety/patient-and-family-centered-care.aspx.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing financial interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Acri, M., Zhang, S., Adler, J.G. et al. Peer-Delivered Models for Caregivers of Children and Adults with Health Conditions: A Review. J Child Fam Stud 26, 337–344 (2017). https://doi.org/10.1007/s10826-016-0616-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-016-0616-1