Abstract
Purpose
To detect a possible bias in sperm DNA fragmentation (SDF) testing when performed on semen samples or on those few spermatozoa selected for Intracytoplasmic Sperm Injection (ICSI) treatments.
Methods
A multimethodological analysis of Single- and Double-Strand DNA Breaks (SSB and DSB, respectively) was performed through the Neutral Comet, the Alkaline Comet, the Sperm Chromatin Dispersion (SCD) and the Terminal deoxynucleotidyl transferase dUTP Nick End Labelling (TUNEL) assays. SDF was evaluated in (i) semen samples from 23 infertile patients (not achieving pregnancy or suffering recurrent miscarriage); (ii) samples after a Swim-up and (iii) spermatozoa microselected for ICSI (ICSI-S).
Results
The analysis of 3217 ICSI-S revealed a significant reduction of SSB values compared to the Ejaculate and the Swim-up samples. On the contrary, DSB values were not reduced after any sperm selection method. The No-pregnancy group presented poorer semen parameters and higher SSB values. The Recurrent miscarriage group presented better semen parameters but also higher DSB values.
Conclusion
The analysis of SDF on semen samples may not be fully representative of those few spermatozoa selected for ICSI. Since oxidative stress impairs sperm motility and causes SSB, selecting a motile sperm may intrinsically imply choosing a sperm not affected by this damage. DSB have an enzymatic origin which does not affect motility, making it difficult to select a sperm without this damage. Therefore, ICSI treatments could be effective in patients presenting high SSB values. Patients presenting high DSB values should expect bad ICSI results if this damage is not reduced through other specific methods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The spermatozoon is a highly differentiated cell designed to propel itself through the female genital tract and deliver the paternal genome to the oocyte. However, defects in the normal development of spermatozoa may interfere with this process leading to fertility impairments [1]. It is estimated that the cause may be attributed to the male in 50% of couples with primary infertility. In this sense, male infertility is present in 6–7% of couples of reproductive age and affects approximately 30 million men worldwide [2].
The study of the male factor should include the evaluation of the global fertility potential of spermatozoa [3]. However, this comprehensive evaluation may be challenging since males may present a wide variety of alterations in semen such as impaired chromatin organisation [1, 4]; numerical or structural chromosomal alterations [5, 6]; Y chromosome microdeletions [7]; DNA fragmentation [8]; altered ratio of protamines P1/P2 [9]; epigenetic alterations [10] or the presence of antisperm antibodies in the seminal plasma [11]. The difficulty of performing a comprehensive study leads 30–40% of cases to remain idiopathic [12]. However, the absence of a conclusive diagnosis may occur as a result of only focusing on a standard semen evaluation, which real impact on fertility has been widely discussed [13, 14]. In this regard, some studies found that, at least, 15% of infertile patients present with normal semen parameters [15] and that morphologically normal sperm may be aneuploid [16] or may have DNA fragmentation [17]. Obtaining a diagnosis is even more relevant in couples undergoing Assisted Reproductive Technologies (ART), especially in Intracytoplasmic Sperm Injection (ICSI) treatments. During ICSI cycles, embryologists select a single spermatozoon with normal morphology and motility to be injected to the oocyte. However, these spermatozoa may have a defective genome that could impair embryo development and implantation [6].
The study of Sperm DNA Fragmentation (SDF) has been an emerging field for the diagnosis of male infertility [18]. Different SDF tests are currently available, including the Comet assay; the Sperm Chromatin Dispersion test (SCD); the Sperm Chromatin Structure Assay (SCSA) and the Terminal deoxynucleotidyl transferase dUTP Nick End Labelling test (TUNEL) [19,20,21]. From these methods, the Comet assay can differentiate between Single-Strand Breaks (SSB) and Double-Strand Breaks (DSB) under alkaline and neutral pH conditions, respectively [21, 22]. The impact of SDF on reproductive outcomes in natural conceptions and ART cycles has been widely studied [21]. Some authors reported that high values of SDF are associated with lower pregnancy rates in natural conceptions [23]; intrauterine inseminations [24, 25] and conventional in vitro fertilisation treatments [26,27,28]. However, the relationship between SDF and ICSI outcomes still remains controversial, with some studies showing a correlation between high SDF values and low pregnancy rates [26,27,28,29], while other studies do not find such correlation [30, 31]. This discrepancy may be attributed to several confounding factors such as the use of different analysis tests; the use of different cutoff values or the lack of distinction between SSB and DSB [29]. All these confounding factors led to the American Society for Reproductive Medicine (ASRM) to conclude that there is not a consistent relationship between SDF and ART clinical outcomes [32]. As other authors suggested before [21, 33], in the present study, we propose sperm selection in ICSI, based on sperm morphology and motility, to be an additional factor contributing to these discrepancies.
The main objective of this study was to determine whether SDF values in semen samples are representative of those few spermatozoa selected during ICSI treatments. A multimethodological analysis of SDF was performed using the Neutral Comet, the Alkaline Comet, the SCD and the TUNEL tests. The impact of SDF and ICSI sperm selection on reproductive outcomes was also evaluated in male patients from couples who never achieved pregnancy and couples suffering recurrent miscarriage.
Materials and methods
Sample collection and inclusion criteria
Semen samples from 23 infertile patients (30–46 years of age) seeking infertility screening at the CIMAB Male Fertility Centre in Barcelona (Spain) were included in the study. All couples reported more than 1 year of idiopathic infertility, including no detected female factor (ovarian reserve, tubal factor, endometriosis, hormonal disturbances or karyotype alterations) or male factor (varicocele, hormonal disturbances, genitourinary infection or karyotype alterations). Patients with severe alterations in semen parameters (≤ 0.5 mL of volume; ≤ 5 × 106 sperm/mL or ≤ 10% of motile sperm) were excluded from the study. For the second part of the study, couples were divided in two groups attending on their fertility background: (i) couples who never achieved a natural pregnancy or presenting two or more implantation failures in ICSI cycles (No-pregnancy group) and (ii) couples presenting two or more consecutive pregnancy losses (Recurrent miscarriage group). The study was approved by the Corporació Sanitaria Parc Taulí Ethics Committee (Ref.: 2014676) and signed informed consents were obtained from all patients.
Sample preparation and sperm selection
Samples were obtained by masturbation after 3–4 days of sexual abstinence and semen parameters were assessed using the SCA CASA software (Microptic S.L., Spain) [34]. Samples were divided in two aliquots and centrifuged at 300g for 3 min. The supernatants were discarded and one of the pellets was resuspended in PBS medium (Ejaculate sample). The other pellet was used for a Swim-up procedure by slowly overlaying 500 μL of HAM’s medium (Nutrient Mixture F-10 HAM, Sigma-Aldrich, USA) with at an angle of 45° and incubated at 37°C for 30 min. Finally, 50 μL of the upper fraction was collected (Swim-up sample) [adapted from 33 and 34].
For sperm microselection, 1 μL of the Swim-up sample was placed in a 5-μL drop of 10% polyvinylpyrrolidone (PVP; Origio, Denmark). Spermatozoa with normal morphology and progressive motility (ICSI-S sample) were selected and placed in a neat 1-μL PVP drop using ICSI pipettes (Vitrolife, Sweden) under ×200 magnification connected to a micromanipulation system (Nikon Diaphot microscope and Narishige micromanipulator, Nikon Inc., Japan) [35].
Sperm DNA fragmentation analysis
SDF was analysed using four different tests on Ejaculate samples and after the Swim-up procedure following conventional protocols.
The Alkaline and Neutral Comet assays were carried out under specifically designed conditions to allow for the differentiation of SSB and DSB, respectively [36]. Semen samples were washed in PBS and mixed with 1% low-melting-point agarose (1:2 v/v) (Sigma-Aldrich, USA); 5 μL was placed on a slide and covered with a coverslip. Samples jellified at 4°C and slides were immersed in two consecutive lysis solutions. The Alkaline Comet electrophoresis was performed at 20V for 4 min in 0.03M NaOH buffer (pH 12.2) after a denaturing treatment in a 0.03M NaOH, 0.15M NaCl solution (pH 12). The Neutral Comet electrophoresis was performed at 20V for 12.5 min in TBE buffer (pH 8.5). Finally, both slides were washed in a 0.4M Trizma Base neutralisation solution (pH 7.5), dehydrated in ethanol series and horizontally dried. Samples were stained with DAPI (Diamond Antifade Mountant with DAPI, Invitrogen, USA) and 400 spermatozoa were classified attending on the morphology and the tail-length of the comet according to the criteria reported before [22]. Spermatozoa with non-fragmented DNA (normal) showed a major percentage of DNA in the comet core and a short tail, while spermatozoa with SSB or DSB showed a lower percentage of DNA in the comet core and larger tails [22].
The SCD assay was performed according to the protocol previously described by Fernández et al. [37]. Semen samples were washed in PBS and mixed with agarose (1:2 v/v); 5 μL was placed on a slide and covered with a coverslip. Samples jellified at 4°C for 5 min. Slides were immersed in a 0.1N HCl denaturing solution for 7 min, in lysis solution for 25 min and finally into a neutralisation solution for 5 min. Samples were dehydrated in ethanol series and horizontally dried. Samples were stained with DAPI and 200 spermatozoa were classified as normal or fragmented according to the size of the observed halo following the criteria reported in Fernández et al. [37]. Spermatozoa with non-fragmented DNA (normal) showed big and medium haloes, while fragmented spermatozoa showed small or no halo.
Semen samples for the TUNEL assay were washed twice in fresh Carnoy solution (acetic acid:methanol, 1:3 v/v). After 24 h in Carnoy solution, samples were washed again in fresh Carnoy solution and 5 μL was fixed on a slide. The assay was performed using the In Situ Cell Death Detection Fluorescein kit (Roche, Germany). The Terminal deoxynucleotidyl Transferase (TdT) enzyme was mixed with the labelling solution (1:9 v/v) and 5 μL was placed on each sample. Slides were incubated at 37°C for 1 h. Three washing steps were performed in PBS for 10 min each. A positive control (sample incubated at 37°C for 30 min with 2000U/μL of deoxyribonuclease I from bovine pancreas (Sigma-Aldrich, Germany)) and a negative control (not adding the TdT enzyme) were included on each slide. Samples were stained with DAPI and 200 spermatozoa classified as normal or fragmented according to the manufacturer’s instructions. Spermatozoa with fragmented DNA showed green fluorescence (Nikon Eclipse E200 and Nikon Intensilight C-HGFI, Nikon Inc., Japan).
Sperm DNA fragmentation analysis on ICSI-selected spermatozoa
The former tests were methodologically adapted to analyse DNA damage on individual ICSI-S following two different protocols. Firstly, for the Comet and the SCD assays, 10–20 spermatozoa were aspirated from the neat PVP drop, rapidly placed inside a 1-μL low-melting-point agarose drop on a slide and jellified for 5 min at room temperature. Secondly, for the TUNEL assay, groups of 10–20 spermatozoa were rapidly placed on a 1-μL ultrapure water drop. Samples were allowed drying for 5 min at room temperature. Slides were immersed in Carnoy solution for 24 h and allowed drying vertically. After DNA fixations, conventional versions of each assay were performed. On agarose fixations, 5-min ethanol series were necessary at the end of the procedure to allow a complete dehydration of samples.
Statistical analysis
SDF was compared between Ejaculate, Swim-up and ICSI-S samples. Moreover, SDF and semen parameters were compared between patients’ groups (No-pregnancy or Recurrent miscarriage).
All parameters were assessed for normality through the Shapiro-Wilk test. As parameters did not show a normal distribution, non-parametric tests were applied. The Wilcoxon test was used for statistical comparisons between samples. All tests were considered significant with a confidence interval of 95%.
Results
Modified sperm DNA fragmentation methodologies
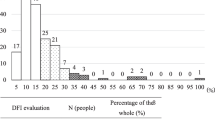
A total of 3217 spermatozoa from 23 infertile patients were individually selected according to the ICSI criteria for sperm morphology and motility. From these, 3117 ICSI-S could be finally visualised on the slides (mean recovery efficiency: 97.0%). About 3% of the spermatozoa were lost during their aspiration and placement on the slides. From the visualised ICSI-S, a total of 2649 could be analysed (mean analysis efficiency: 84.5%) (Table 1). In agarose fixations, about 15% of visualised sperm could not be analysed. In contrast, all ICSI-S fixed in Carnoy solution could be analysed. For each technique, a mean of 662.25 spermatozoa could be analysed (Fig. 1; Table 1).
Sperm DNA fragmentation assessment
Comparisons between samples: Ejaculate, Swim-up and ICSI-selected spermatozoa
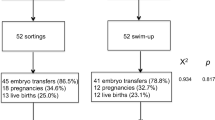
The results obtained using four different methods for the measurement of SDF on the Ejaculate, the Swim-up and the ICSI-S samples are shown in Figs. 1 and 2a. SDF analysis showed a significant reduction of SSB values in Swim-up samples compared to the Ejaculate using the Alkaline Comet, the SCD and the TUNEL tests (reduction of 8.39%, 8.10% and 5.83%, respectively; p values < 0.05). This reduction in SSB values was even more important in ICSI-S compared to the Ejaculate (reduction of 31.35%, 17.85% and 16.00%, respectively; p values < 0.05) and the Swim-up samples (reduction of 22.96%, 9.75% and 10.77%, respectively; p values < 0.05) (Fig. 2a). In contrast, the Neutral Comet assay did not show any differences in DSB values between the Ejaculate, the Swim-up and the ICSI-S (p values > 0.05) (Fig. 2a).
Multimethodological analysis of sperm DNA fragmentation on (a) Ejaculated, Swim-up-selected and ICSI-selected spermatozoa (ICSI-S) and (b) Ejaculate samples according to patients’ fertility background (No-pregnancy and Recurrent miscarriage). Outlier values 3 and 1.5 times out of the Q3 interquartile range are indicated with asterisks and circles in the boxplot, respectively. Horizontal bars with an asterisk symbol indicate significant differences (p value < 0.05)
Comparisons between clinical groups: No-pregnancy and Recurrent miscarriage
Comparison of SDF values between clinical groups indicated statistically significant differences when using the Comet assays but not the SCD or TUNEL tests (Fig. 2b). The No-pregnancy group showed a significant increase of 16.03% in SSB values compared to the Recurrent miscarriage group as measured through the Alkaline Comet (p value = 0.030). The SCD and the TUNEL tests did not show significant differences (2.54% and 1.48%, respectively; p values > 0.05). In contrast, the Recurrent miscarriage group showed a significant increase of 7.73% in DSB values, as measured by the Neutral Comet assay (p value = 0.026) (Fig. 2b).
Semen parameters
Patients from the No-pregnancy group showed poorer semen parameters compared to those patients from the Recurrent miscarriage group. Significant differences were found in sperm concentration, the percentage of sperm with progressive motility and the percentage of immobile sperm (Table 2).
Discussion
Three main findings emerge from this study: firstly, sperm selection using the ICSI criteria of normal morphology and motility results in a reduction of SSB compared to the observed values in Ejaculated and Swim-up samples, as measured by the Alkaline Comet assay, the SCD and the TUNEL tests. On the contrary, ICSI selection does not reduce DSB values, as measured by the Neutral Comet assay. This discrepancy in DNA damage values in semen samples compared to ICSI-S may explain, at least in part, the reported lack of correlation between SDF and reproductive outcomes in ICSI. Secondly, compared to the SCD and TUNEL tests, the Comet assay has a greater sensitivity in detecting SSB and DSB. And thirdly, the Neutral Comet assay is the only SDF test that detects DSB in the studied patients.
In this study, 3217 single spermatozoa were selected under ×200 magnification (Fig. 1). To our knowledge, this is the first time that four different techniques used for SDF testing have been successfully adapted and applied to differentiate SSB and DSB in ICSI-S (Table 1). The sperm recovery efficiency was of 97.0% and the analysis efficiency was of 84.5%. However, some sperm loss occurred between the aspiration of ICSI-S from the neat drop and their fixation in agarose or ultrapure water. During ICSI treatments, one single sperm should be aspirated and kept inside the micropipette between the tip and the elbow until the injection. Due to procedural requirements, groups of 10–20 spermatozoa were aspirated together surpassing the micropipette elbow in some cases. Since after this point the inner diameter of the micropipette is higher, spermatozoa could have been lost in that space. The aspiration of a lower volume of media during aspiration and the selection of a lower number of spermatozoa were considered but did not significantly improve sperm recovery while the experimental time was increased. In this sense, the optimal conditions for ICSI-S fixation were established as described in the “Materials and methods” section. The analysis efficiencies showed that all spermatozoa fixed in ultrapure water and Carnoy solution could finally be analysed using the TUNEL assay. On the other hand, some ICSI-S fixed in agarose could not be analysed due to the incomplete chromatin dispersion and the irregular electrical current that happens in the edge of the agarose drops. This situation is well known as the “edge effect” in agarose electrophoresis. Moreover, some sperm moved from their initial location impairing the correct analysis of other spermatozoa. Keeping ICSI-S further apart during fixations in agarose may reduce analytical interferences.
About SDF, previous studies showed a strong correlation between the Alkaline Comet assay under specific conditions (which mainly detects SSB) and the SCD and the TUNEL assays [38, 39]. The results here obtained using these tests revealed that SSB values are lower in the Swim-up sample compared to the Ejaculate (Fig. 2a). This is in agreement with previous reports using only the SCD test [40, 41]. This reduction in SSB values is even more prominent in ICSI-S compared to the Ejaculate (Fig. 2a) and could be explained based on whether this type of DNA damage is measured on non-motile or motile sperm: SSB values are higher in the Ejaculate sample (which include motile and non-motile sperm) compared to the Swim-up sample (mainly motile sperm) and ICSI-S (only sperm with optimal progressive motility).
Oxidative stress could be responsible of this great reduction in SSB values after sperm selection. Reactive oxygen species (ROS) induce DNA and membrane damage, which are the main cause of both SSB (through the formation of 8-hydroxy-29-deoxyguanosine (8OHdG)) and motility loss (through the alteration of the normal function of mitochondria to produce ATP and/or through alterations at the cell membrane) [42]. It is worth noting that, in some previous reports evaluating DNA damage and motility, SSB and DSB were not differentiated [42, 43]. However, authors tested DNA damage through techniques that correlate with the Alkaline Comet and mainly detect SSB [38, 39]. Concerning the effect of oxidative stress, varicocele is one of the main causes of male infertility and has shown to increase intratesticular ROS levels, while its surgical repair has shown to reduce these values [44, 45]. In a recent study, the effect of ROS-induced DNA and membrane damage was tested in patients with high-grade varicocele, consistently showing a significant reduction in SSB and an improvement in sperm motility after its surgical repair [46].
Related to the latter findings, patients who never achieved pregnancy or showed implantation failures in previous ICSI cycles (No-pregnancy group) presented both lower sperm motility and higher SSB levels compared to patients who achieved clinical pregnancies but who suffered recurrent miscarriage (Recurrent miscarriage group) (Table 2; Fig. 2b). This is in agreement with previous reports that showed a negative correlation between high SSB values and implantation failures [25, 47, 48], and also with those studies which reported an improvement in pregnancy rates after ICSI selection of a motile sperm in patients with high SSB [21, 49]. SSB has been reported to be present in an extensive manner in sperm’s DNA [36]. Even if a sperm with poor motility fertilises an oocyte through natural or assisted reproduction, the repair capacity of the oocyte may not overcome this extensive damage impairing the first mitotic divisions of the embryo and finally leading to a failed pregnancy [36]. Based on these results, in male patients who do not achieve pregnancy or presenting high rates of SSB, an ICSI treatment through a Swim-up procedure to prepare the semen sample followed by sperm microselection under strict criteria of motility could be recommended since these procedures would importantly reduce SSB damage.
In sharp contrast, a correlation between DSB and oxidative stress or decreased sperm motility has never been found [50]. This type of DNA damage is mainly produced during the prophase I stage of meiosis through the action of SPO11 to allow the recombination process between homologous chromosomes and to allow the hypercondensation of chromosomes during the protamination process in the Matrix Attachment Regions (MAR regions) [51,52,53]. These programmed breaks are expected to be repaired after recombination through the mediation of ATM-dependent repair systems. However, when the repair systems are inefficient or when DNA breaks are generated in excess, high rates of DSB may be present in ejaculated spermatozoa [54]. The results of the present study show that DSB values are similar in the Ejaculate sample, the Swim-up sample and ICSI-S, even if these cells present high progressive motility and good morphology (Fig. 2a).
These results provide strong support to a previous study in which human embryo kinetics was monitored by time-lapse microscopy. In that study, oocytes were microinjected with spermatozoa from patients with high SSB or DSB values detected in semen samples [55]. The results showed that the microinjection of motile spermatozoa from samples with high SSB values did not affect embryo kinetics and implantation rates [56], while microinjecting spermatozoa from samples with high DSB values resulted in a delay in embryo kinetics along all stages of embryo development [55]. To explain these results, one must remember that DSB have an enzymatic and controlled origin, so this damage is not produced in an extensive manner such as SSB. Consequently, the oocyte may be able to repair these breaks at some extend. If sperm’s DSB exceed the repair capacity of the oocyte or if non-consecutive ends are ligated by error, the embryo could carry chromosomal abnormalities that may impair embryo development or end up in a miscarriage [36, 57]. Consistently, the present results show that the risk of recurrent pregnancy loss is increased when patients present high DSB values (Fig. 2b) [36] even if these patients present normal semen parameters (Table 2) [58]. Based on these results, in patients with recurrent miscarriage or showing high DSB values, semen processing through a Swim-up or ICSI sperm selection may not have any effect in reducing this damage. Therefore, alternative methods for sperm selection should be considered to specifically reduce DSB values.
During ART procedures, different techniques are available for semen preparation with the objective of selecting optimal spermatozoa. Conventional methods such as Swim-up or Density Gradients procedures are based on sperm’s motility; therefore, these approaches are only expected to reduce SSB (Fig. 2a) [59]. New microfluidic sorting devices have recently emerged for the selection of sperm with optimal progressive motility. In agreement with the results here presented, these methods showed to strongly reduce SSB, nearly to undetectable values through the SCD and the TUNEL tests [60,61,62]. Moreover, these filters based on microfluidics pretend to mimic the natural sperm selection produced through the female genital track [63, 64]. Recent studies showed that these devices increase clinical outcomes in ICSI treatments (more high-quality euploid embryos and higher implantation and pregnancy rates) [62, 65]. We hypothesise that these great results could be related to the reduction of both SSB and DSB since the detrimental effects of DSB on embryo kinetics are not observed after the use of these new devices [55]. Further investigations studding the capacity of these microfluidic sorting devices to specifically reduce DSB values and its effect on ICSI clinical outcomes may be enlightening.
Since ICSI is the most commonly used ART technique worldwide [66], in this study, we focused on the utility of the ICSI criteria in selecting sperm with low levels of SDF. Interestingly, previous studies analysed SDF values in single spermatozoa based on morphology criteria analysed under high magnification (Motile Sperm Organelle Morphology Examination, MSOME) [67,68,69,70]. Despite their differences, all these studies revealed that spermatozoa with abnormal morphology (e.g. nuclear vacuoles) present higher SDF rates while sperm with normal morphology present lower values. Concerning the utility of sperm selection under high magnification in ICSI cycles (Intracytoplasmic Morphological Sperm Injection, IMSI), some studies found that this procedure improves reproductive outcomes compared to conventional ICSI treatments [71, 72]. However, other studies, such as a recent meta-analysis of the Cochrane database, found opposite conclusions [73,74,75,76]. From these studies, only Pastuszek et al. analysed SSB and DSB separately, although using a different version of the Comet assay [69]. Results showed that 70–80% of sperm presenting normal morphology without vacuoles have low SDF values. However, about 20–30% of these morphologically normal sperm present SSB and DSB. In this sense, the IMSI procedure could increase the chances of selecting a sperm not affected by SDF, thus increasing ART results in this subpopulation of patients with SDF detected in semen samples. More studies analysing a large number of ICSI and IMSI cycles after detecting SSB and DSB would be necessary to confirm this hypothesis.
The findings from this study may also help to explain, at least in part, the controversy in the apparent lack of correlation between SDF values and ICSI reproductive outcomes [31]. The published guidelines from the ASRM claimed that most studies comparing SDF values with reproductive outcomes included confounding factors [32]. The analysis of all these studies led the authors to conclude that there is not enough evidence to support SDF testing to predict reproductive outcomes in natural or ART cycles. One of the main findings emerging from the present study is that, in order to find a correlation between SDF and reproductive outcomes, SSB and DSB must be differentiated. Since most tests do not differentiate between SSB and DSB damage and since SSB values in ejaculated spermatozoa do not correlate with those values obtained in ICSI-S, a lack of correlation between high SDF values in ejaculated spermatozoa and poor reproductive outcome might be misleading.
In view of these results, new possible biomarkers for the diagnosis of the male factor or predictors of ART success such as the analysis of the following: mitochondrial DNA [77]; free sperm DNA in semen [78]; surface charge; membrane integrity or membrane proteins [1], among others, should demonstrate that their analysis on the Ejaculate sample is representative of those few spermatozoa finally injected into the oocytes. If present in ICSI-S, these new biomarkers could open new investigations on possible diagnostics and treatments for male infertile patients.
In conclusion, the results of this study show that sperm selection using the ICSI criteria selects spermatozoa with lower SSB values compared to the Ejaculate and the Swim-up samples, as measured by the Alkaline Comet, the SCD and the TUNEL assays. On the contrary, these selection methods may not have any effect in selecting sperm with lower DSB values, as measured by the Neutral Comet assay. Compared to the SCD and TUNEL tests, the Comet assay has a greater sensitivity in detecting SDF in the studied patients. In terms of reproductive outcomes, the ICSI procedure in itself could be considered an effective technique for sperm selection in patients with high SSB values or in patients who never achieved pregnancy. In contrast, ICSI may not be effective in reducing DSB in spermatozoa from patients with recurrent miscarriage or in patients with high DSB values. Therefore, a specific sperm selection technique should be recommended to select sperm with lower DSB for ICSI.
Code availability
Not applicable.
References
Vaughan DA, Sakkas D. Sperm selection methods in the 21st century. Biol Reprod. 2019;101:1076–82.
Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015;13:1–9.
Jeyendran RS, Caroppo E, Rouen A, Anderson A, Puscheck E. Selecting the most competent sperm for assisted reproductive technologies. Fertil Steril. 2019;111:851–63.
Agarwal A, Said TM. Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum Reprod Update. 2003;9:331–45.
Ioannou D, Griffin DK. Male fertility, chromosome abnormalities, and nuclear organization. Cytogenet Genome Res. 2011;133:269–79.
Hamada A, Esteves SC, Agarwal A. Genetics and male infertility. Androl Clin. 2006:462–80.
Dhanoa JK, Mukhopadhyay CS, Arora JS. Y-chromosomal genes affecting male fertility: a review. Vet World. 2016;9:783–91.
Simon L, Emery BR, Carrell DT. Sperm DNA fragmentation consequences for reproduction. Adv Exp Med Biol. 2019;1166.
Oliva R. Protamines and male infertility. Hum Reprod Update. 2006;12:417–35.
Gunes S, Arslan MA, Hekim GNT, Asci R. The role of epigenetics in idiopathic male infertility. J Assist Reprod Genet. 2016;33:553–69.
Samplaski MK, Agarwal A, Sharma R, Sabanegh E. New generation of diagnostic tests for infertility: review of specialized semen tests. Int J Urol. 2010;17:839–47.
Katz DJ, Teloken P, Shoshany O. Male infertility - the other side of the equation. Aust Fam Physician. 2017;46:641–6.
Wang C, Swerdloff RS. Limitations of semen analysis as a test of male fertility and anticipated needs from newer tests. Fertil Steril. 2014;102:1502–7.
Esteves SC. Clinical relevance of routine semen analysis and controversies surrounding the 2010 World Health Organization criteria for semen examination. Int Braz J Urol. 2014;40:443–53.
Agarwal A, Allamaneni SSR. Sperm DNA damage assessment: a test whose time has come. Fertil Steril. 2005;84:850–3.
Celik-Ozenci C, Jakab A, Kovacs T, Catalanotti J, Demir R, Bray-Ward P, et al. Sperm selection for ICSI: shape properties do not predict the absence or presence of numerical chromosomal aberrations. Hum Reprod. 2004;19:2052–9.
Avendaño C, Franchi A, Taylor S, Morshedi M, Bocca S, Oehninger S. Fragmentation of DNA in morphologically normal human spermatozoa. Fertil Steril. 2009;91:1077–84.
Majzoub A, Agarwal A, Esteves SC. Clinical utility of sperm DNA damage in male infertility. Panminerva Med. 2019;61:118–27.
Panner Selvam MK, Agarwal A. A systematic review on sperm DNA fragmentation in male factor infertility: Laboratory assessment. Arab J Urol. 2018;16:65–76.
Bach PV, Schlegel PN. Sperm DNA damage and its role in IVF and ICSI. Basic Clin Androl. 2016;26:1–10.
Agarwal A, Barbăroșie C, Ambar R, Finelli R. The impact of single- and double-strand DNA breaks in human spermatozoa on assisted reproduction. Int J Mol Sci. 2020;21:1–14.
Ribas-Maynou J, García-Peiró A, Abad C, Amengual MJ, Navarro J, Benet J. Alkaline and neutral Comet assay profiles of sperm DNA damage in clinical groups. Hum Reprod. 2012;27:652–8.
Zini A. Are sperm chromatin and DNA defects relevant in the clinic? Syst Biol Reprod Med. 2011;57:78–85.
Alkhayal A, San Gabriel M, Zeidan K, Alrabeeah K, Noel D, McGraw R, et al. Sperm DNA and chromatin integrity in semen samples used for intrauterine insemination. J Assist Reprod Genet. 2013;30:1519–24.
Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2007;22:174–9.
Simon L, Proutski I, Stevenson M, Jennings D, McManus J, Lutton D, et al. Sperm DNA damage has a negative association with live-birth rates after IVF. Reprod BioMed Online. 2013;26:68–78.
Osman A, Alsomait H, Seshadri S, El-Toukhy T, Khalaf Y. The effect of sperm DNA fragmentation on live birth rate after IVF or ICSI: a systematic review and meta-analysis. Reprod BioMed Online. 2015;30:120–7.
Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damage is associated with an increased risk of pregnancy loss after IVF and ICSI: Systematic review and meta-analysis. Hum Reprod. 2008;23:2663–8.
Simon L, Zini A, Dyachenko A, Ciampi A, Carrell D. A systematic review and meta-analysis to determine the effect of sperm DNA damage on in vitro fertilization and intracytoplasmic sperm injection outcome. Asian J Androl. 2017;19:80–90.
Yang H, Li G, Jin H, Guo Y, Sun Y. The effect of sperm DNA fragmentation index on assisted reproductive technology outcomes and its relationship with semen parameters and lifestyle. Transl Androl Urol. 2019;8:356–65.
Anifandis G, Bounartzi T, Messini CI, Dafopoulos K, Markandona R, Sotiriou S, et al. Sperm DNA fragmentation measured by Halosperm does not impact on embryo quality and ongoing pregnancy rates in IVF/ICSI treatments. Andrologia. 2015;47:295–302.
The practice committee of the American Society for Reproductive Medicine. The clinical utility of sperm DNA integrity testing: a guideline. Fertil Steril. 2013;99:673–7.
Avendaño C, Oehninger S. DNA fragmentation in morphologically normal spermatozoa: how much should we be concerned in the ICSI era? J Androl. 2011;32:356–63.
WHO. WHO laboratory manual for the examination and processing of human semen. World Heal Organ Press 2010; 5th Editio.
Balaban B, Sakkas D, Gardner DK. Laboratory procedures for human in vitro fertilization. Semin Reprod Med. 2014;32:272–82.
Ribas-Maynou J, García-Peiró A, Fernandez-Encinas A, Amengual M, Prada E, Cortés P, et al. Double stranded sperm DNA breaks, measured by Comet assay, are associated with unexplained recurrent miscarriage in couples without a female factor. PLoS One. 2012;7:e44679.
Fernández JL, Muriel L, Goyanes V, Segrelles E, Gosálvez J, Enciso M, et al. Simple determination of human sperm DNA fragmentation with an improved sperm chromatin dispersion test. Am Soc Reprod Med. 2005;84:833–42.
Ribas-Maynou J, García-Peiró A, Fernández-Encinas A, Abad C, Amengual MJ, Prada E, et al. Comprehensive analysis of sperm DNA fragmentation by five different assays: TUNEL assay, SCSA, SCD test and alkaline and neutral Comet assay. Andrology. 2013;1:715–22.
García-Peiró A, Oliver-Bonet M, Navarro J, Abad C, Guitart M, Amengual MJ, et al. Dynamics of sperm DNA fragmentation in patients carrying structurally rearranged chromosomes. Int J Androl. 2011;34:e546–53.
Gosálvez J, Caballero P, López-Fernández C, Ortega L, Guijarro JA, Fernández JL, et al. Can DNA fragmentation of neat or swim-up spermatozoa be used to predict pregnancy following ICSI of fertile oocyte donors? Asian J Androl. 2013;15:812–8.
Oguz Y, Guler I, Erdem A, Mutlu MF, Gumuslu S, Oktem M, et al. The effect of swim-up and gradient sperm preparation techniques on deoxyribonucleic acid (DNA) fragmentation in subfertile patients. J Assist Reprod Genet. 2018;35:1083–9.
Agarwal A, Virk G, Ong C, du Plessis SS. Effect of oxidative stress on male reproduction. World J Mens Health. 2014;32:1.
Henkel R, Kierspel E, Hajimohammad M, Stalf T, Hoogendijk C, Mehnert C, et al. DNA fragmentation of spermatozoa and assisted reproduction technology. Reprod BioMed Online. 2003;7:477–84.
Agarwal A, Sharma R, Harlev A, Esteves SC. Effect of varicocele on semen characteristics according to the new 2010 World Health Organization criteria: a systematic review and meta-analysis. Asian J Androl. 2016;18:163–70.
Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, Sabanegh E, et al. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007;70:532–8.
Lara-Cerrillo S, Gual-Frau J, Benet J, Abad C, Prats J, Amengual MJ, et al. Microsurgical varicocelectomy effect on sperm telomere length, DNA fragmentation and seminal parameters. Hum Fertil. 2020;9:1–7.
Zhao J, Zhang Q, Wang Y, Li Y. Whether sperm deoxyribonucleic acid fragmentation has an effect on pregnancy and miscarriage after in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil Steril 2014; 102:998-1005.e8.
Simon L, Lutton D, McManus J, Lewis SEM. Sperm DNA damage measured by the alkaline Comet assay as an independent predictor of male infertility and in vitro fertilization success. Fertil Steril. 2011;95:652–7.
Chi H, Kim S, Kim Y, Park J, Yoo C, Park I, et al. ICSI significantly improved the pregnancy rate of patients with a high sperm DNA fragmentation index. Clin Exp Reprod Med. 2017;44:132–40.
Coban O, Serdarogullari M, Yarkiner Z, Serakinci N. Investigating the level of DNA double-strand break in human spermatozoa and its relation to semen characteristics and IVF outcome using phospho-histone H2AX antibody as a biomarker. Andrology. 2019:1–6.
Paiano J, Wu W, Yamada S, Sciascia N, Callen E, Paola Cotrim A, et al. ATM and PRDM9 regulate SPO11-bound recombination intermediates during meiosis. Nat Commun. 2020;11:1–15.
Lange J, Pan J, Cole F, Thelen MP, Jasin M, Keeney S. ATM controls meiotic double-strand-break formation. Nature. 2011;479:237–40.
Keeney S, Lange J, Mohibullah N. Self-organization of meiotic recombination initiation: general principles and molecular pathways. Annu Rev Genet. 2014;48:187–214.
García-Rodríguez A, Gosálvez J, Agarwal A, Roy R, Johnston S. DNA damage and repair in human reproductive cells. Int J Mol Sci. 2019;20:1–22.
Casanovas A, Ribas-Maynou J, Lara-Cerrillo S, Jimenez-Macedo AR, Hortal O, Benet J, et al. Double-stranded sperm DNA damage is a cause of delay in embryo development and can impair implantation rates. Fertil Steril. 2019;111:699–707.e1.
Green KA, Patounakis G, Dougherty MP, Werner MD, Scott RT, Franasiak JM. Sperm DNA fragmentation on the day of fertilization is not associated with embryologic or clinical outcomes after IVF/ICSI. J Assist Reprod Genet. 2020;37:71–6.
Gunes S, Sertyel S. Sperm DNA damage and oocyte repair capability. A Clin Guid to Sperm DNA Chromatin Damage. 2018:321–46.
Eisenberg ML, Sapra KJ, Kim SD, Chen Z, Buck Louis GM. Semen quality and pregnancy loss in a contemporary cohort of couples recruited before conception: Data from the LIFE Study. Fertil Steril. 2017;108:613–9.
Marzano G, Chiriacò MS, Primiceri E, Dell’Aquila ME, Ramalho-Santos J, Zara V, et al. Sperm selection in assisted reproduction: a review of established methods and cutting-edge possibilities. Biotechnol Adv. 2020;40:107498.
Quinn MM, Jalalian L, Ribeiro S, Ona K, Demirci U, Cedars MI, et al. Microfluidic sorting selects sperm for clinical use with reduced DNA damage compared to density gradient centrifugation with swim-up in split semen samples. Hum Reprod. 2018;33:1388–93.
Xiao S, Riordon J, Simchi M, Lagunov A, Hannam T, Jarvi K, et al. FertDish: microfluidic sperm selection-in-a-dish for intracytoplasmic sperm injection. Lab Chip. 2021;21:775–83.
Parrella A, Keating D, Cheung S, Xie P, Stewart JD, Rosenwaks Z, et al. A treatment approach for couples with disrupted sperm DNA integrity and recurrent ART failure. J Assist Reprod Genet. 2019;36:2057–66.
Smith GD, Takayama S. Application of microfluidic technologies to human assisted reproduction. Mol Hum Reprod. 2017;23:257–68.
Samuel R, Feng H, Jafek A, Despain D, Jenkins T, Gale B. Microfluidic-based sperm sorting & analysis for treatment of male infertility. Transl Androl Urol. 2018;7:S336–47.
Anbari F, Khalili MA, Sultan Ahamed AM, Mangoli E, Nabi A, Dehghanpour F, et al. Microfluidic sperm selection yields higher sperm quality compared to conventional method in ICSI program: a pilot study. Syst Biol Reprod Med. 2021;00:1–7.
Palermo GD, O’Neill CL, Chow S, Cheung S, Parrella A, Pereira N, et al. Intracytoplasmic sperm injection: State of the art in humans. Reproduction. 2017;154:F93–F110.
Franco J, Baruffi R, Mauri A, Petersen C, Oliveira J, Vagnini L. Significance of large nuclear vacuoles in human spermatozoa: implications for ICSI. Reprod BioMed Online. 2008;17:42–5.
Gosálvez J, Migueles B, López-Fernández C, Sanchéz-Martín F, Sáchez-Martín P. Single sperm selection and DNA fragmentation analysis: the case of MSOME/IMSI. Nat Sci. 2013;05:7–14.
Pastuszek E, Kiewisz J, Skowronska P, Liss J, Lukaszuk M, Bruszczynska A, et al. An investigation of the potential effect of sperm nuclear vacuoles in human spermatozoa on DNA fragmentation using a neutral and alkaline Comet assay. Andrology. 2017;5:392–8.
Hammoud I, Boitrelle F, Ferfouri F, Vialard F, Bergere M, Wainer B, et al. Selection of normal spermatozoa with a vacuole-free head (x6300) improves selection of spermatozoa with intact DNA in patients with high sperm DNA fragmentation rates. Andrologia. 2013;45:163–70.
Luna D, Hilario R, Dueñas-Chacón J, Romero R, Zavala P, Villegas L, et al. The IMSI procedure improves laboratory and clinical outcomes without compromising the aneuploidy rate when compared to the classical ICSI procedure. Clin Med Insights Reprod Heal. 2015;9:CMRH.S33032.
Wilding M, Coppola G, Di Matteo L, Palagiano A, Fusco E, Dale B. Intracytoplasmic injection of morphologically selected spermatozoa (IMSI) improves outcome after assisted reproduction by deselecting physiologically poor quality spermatozoa. J Assist Reprod Genet. 2011;28:253–62.
Duran-Retamal M, Morris G, Achilli C, Gaunt M, Theodorou E, Saab W, et al. Live birth and miscarriage rate following intracytoplasmic morphologically selected sperm injection vs intracytoplasmic sperm injection: an updated systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2019:1–10.
Setti AS, De Almeida Ferreira Braga DP, Iaconelli A, Aoki T, Borges E. Twelve years of MSOME and IMSI: a review. Reprod BioMed Online. 2013;27:338–52.
Teixeira D, Barbosa M, Ferriani R, Navarro P, Nastri C. Regular ( ICSI ) versus ultra-high magnification ( IMSI ) sperm selection for assisted reproduction ( Review ). Cochrane Libr. 2013.
López G, Lafuente R, Checa MA, Carreras R, Brassesco M. Diagnostic value of sperm DNA fragmentation and sperm high-magnification for predicting outcome of assisted reproduction treatment. Asian J Androl. 2013;15:790–4.
Simopoulou M, Sfakianoudis K, Antoniou N, Maziotis E, Rapani A, Bakas P, et al. Making IVF more effective through the evolution of prediction models: is prognosis the missing piece of the puzzle? Syst Biol Reprod Med. 2018;64:305–23.
Bounartzi T, Dafopoulos K, Anifandis G, Messini CI, Koutsonikou C, Kouris S, et al. Pregnancy prediction by free sperm DNA and sperm DNA fragmentation in semen specimens of IVF/ICSI-ET patients. Hum Fertil. 2016;19:56–62.
Aknowledgements
We thank Dr. Denny Sakkas for his useful comments on the final manuscript.
Funding
SLC received an Industrial Doctorate grant (Doctorados Industriales) given by the Economy, Industry and Competitivity Ministry of Spain (Ministerio de Economía, Industria y Competitividad) and the State Investigation Agency (Agencia Estatal de Investigación) (Ref.: DI-16-08429).
Author information
Authors and Affiliations
Contributions
SLC performed the experiments and participated in the study design, the data analysis and the manuscript writing and review. JRM participated in the study design and data analysis. TLR and CRI performed the experiments. JB contributed to the manuscript review. AGP contributed to the study design, analysis of data and manuscript review and final approval.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Corporació Sanitaria Parc Taulí Ethics Committee (Ref.: 2014676) and signed informed consents were obtained from all patients.
Consent to participate
Patients consented to participate.
Consent for publication
Patients consented to participate.
Conflict of interest
AGP is the director of the CIMAB centre, a university spin-out company with a commercial interest in SDF testing. No other author has a conflict of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lara-Cerrillo, S., Ribas-Maynou, J., Rosado-Iglesias, C. et al. Sperm selection during ICSI treatments reduces single- but not double-strand DNA break values compared to the semen sample. J Assist Reprod Genet 38, 1187–1196 (2021). https://doi.org/10.1007/s10815-021-02129-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02129-w