Abstract
Purpose
The objective of this work was to determine which embryonic morphokinetic parameters up to D3 of in vitro development have predictive value for implantation for the selection of embryos for transfer in clinical practice based upon information generated from embryo transfers with known implantation data (KID).
Methods
A total of 800 KID embryos (100% implantation rate (IR) per transfer and 0% IR per transfer) cultured in an incubator with Time-Lapse system were retrospectively analysed. Of them, 140 embryos implanted, whereas 660 did not.
Results
The analysis of morphokinetic parameters, together with the embryo morphology assessment on D3, enabled us to develop a hierarchical model that places the classical morphological score, the t4 and t8 morphokinetic values, as the variables with the best prognosis of implantation.
Conclusion
In our decision tree, the classical morphological score is the most predictive parameter. Among embryos with better morphological scores, morphokinetics permits deselection of embryos with the lowest implantation potential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since in vitro fertilization (IVF) treatment in humans began, the assessment of the embryo’s morphology at certain check-points in its development has been the most widely used method to evaluate embryo quality and to select them for transfer [1, 2].
The first publications on human embryo assessment using the dynamic monitoring system (Time-Lapse (TL)) date back to 1996 [3, 4], but only recently has this system been established as routine in assisted reproduction laboratories. Embryo culture in TL-method incubators delivers continuous information on the embryos’ developmental stage and morphokinetics, thus optimizing embryo selection while also providing an uninterrupted and stable culture.
In recent years, several studies in this area have set out to find a correlation between different morphokinetic parameters and the embryo’s potential to reach the blastocyst stage, the presence of aneuploidies in the embryo or the ability of the embryos to implant and result in a healthy live birth. In 2010, Wong [5] postulated that some aspects of embryo development, especially the success or failure to reach blastocyst stage, are determined very early and probably depend on the oocyte, relating the duration of the first cytokinesis and the duration of 2- and 3-cell stages to the embryo’s potential to reach the blastocyst stage. Other authors subsequently confirmed some of these associations [6, 7] or found new predictive parameters of blastocyst formation, such as direct cleavage to 3-cell stage [8], the duration of the 3-cell stage [8, 9], the time for the embryo to reach 4 cells (t4) [8], the time needed to reach 7- and 8-cell stages and the duration of the third division (t8-t5) [9], the time to morula [8] or all the cell divisions and the duration of the cell stages except for the first division (t2) [10].
With regard to the embryo’s chromosomal constitution, Campbell [11] concluded that embryos with simple or complex aneuploidies present a delay in the start of blastocyst formation, needing more time to reach this stage, and described that the presence of aneuploidies in the embryo is correlated with the time of blastulation and full blastulation. Basile [12] found predictive parameters of the presence of embryo aneuploidies in the duration of the 2-cell stage (t3-t2); the moment the embryo reaches 5 cells (t5) and the t5-t3 and t5-t2 time ranges. However, Rienzi [13] did not find any association between morphokinetic variables and the presence of aneuploidies in the embryo.
Other authors have correlated several morphokinetic parameters, such as the moment of extrusion of the second polar body, the time from appearance until the fading of the pronuclei (PN) [14], the time for PN fading [14, 15], synchrony in the appearance of nuclei after first cleavage [16], the duration of 2- and 3-cell stages and t5 [17, 18], t3, t5 and cc2 time ranges [19] or the t8 value [10] to the pregnancy/implantation rate.
Different algorithms for embryo selection based on morphokinetic parameters have been published, which relate the moment that key events of embryo development and implantation potential occur. [17, 19]. However, the usefulness of the TL methodology for embryo selection is controversial, and some authors consider that there is no evidence of the benefits of using it [20, 21]. Despite the criticism, laboratories that have implemented TL systems are reluctant to go back to the traditional observation and selection method due to the advantages of not having to remove the embryos from the incubator for observation, and also of having images of the continuing embryonic development for the selection of embryos. Some authors believe that TL can be a useful tool in IVF laboratories even if it were proven that the morphokinetic models for embryo selection are no better than those based on classical standard morphological evaluation [22].
Several publications report that morphokinetic parameters could vary according to the different intrinsic conditions of each IVF programme and laboratory, such as the type of ovarian stimulation, insemination method or culture conditions [23,24,25,26,27]. This makes it more difficult to apply a morphokinetic score model from one centre to another, and it is thus recommended that laboratories with sufficient data set the potentially informative morphokinetic values for their specific laboratory working conditions [28].
The objective of this work is to determine whether, in a large number of cases with known implantation data (KID) embryo transfers, performed only in one ART centre and using the same culture conditions, the embryo morphokinetic parameters up to D3 can have a predictive value of implantation capability and whether they can be routinely used for the selection of embryos in clinical practice.
Materials and methods
Patients
This work was developed in only one ART centre, and all procedures and protocols were approved by its Institutional Review Board (IRB).
A total of 800 KID embryos (100% IR per transfer and 0% IR per transfer) cultured in an incubator with TL system were retrospectively analysed. Of them, 140 embryos implanted, whereas 660 did not. The embryos resulted from 439 fresh ICSI cycles with own gametes performed in our centre from July 2011 to December 2014. Cycles with oocyte donor, vitrified own oocytes, sperm donor, cryopreserved own sperm or with preimplantation genetic diagnosis were excluded from the study.
Patients underwent ovarian stimulation with the use of gonadotropins (FSH or hMG) and GnRH analogues. Patients received hCG when the diameter of the leading follicle(s) >18 mm. 36 h after hCG injection, ultrasound-guided oocyte retrieval was carried out. Embryo replacement was performed on D3 and luteal support consisted of vaginally administered progesterone. Only clinical pregnancies were considered, defined as transvaginal ultrasonography visualization of the gestational sac.
Oocyte retrieval and ICSI
Following retrieval, the oocytes were immediately placed in fertilization culture medium (Vitrolife®) plates. Cumulus-oocyte complexes were denudated 2 h post-retrieval with hyaluronidase and subsequent mechanical pipetting of different tip diameters. Oocytes were microinjected at least 4 h post-retrieval.
Embryo culture and embryo selection
Once the oocytes had been inseminated by ICSI, they were individually cultured in EmbryoSlide dishes (Vitrolife®) pre-equilibrated for at least 4 h at 37 °C and 6% CO2 with embryo culture medium (Vitrolife®). Culture conditions were set at 37 °C, 6% CO2 and 5% O2.
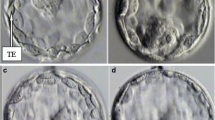
The TL system used was the Embryoscope® (Vitrolife®), and it was set to acquire images every 15 min at 5 different focal planes from each embryo. All the embryo transfers were carried out on D3 of embryo development, and embryo selection was based only on morphological criteria. All the embryos of each patient were evaluated according to our own score that grades embryos from 0 to 10, with the ones with the highest score being chosen for transfer. Embryos were considered as having optimum morphology (score 8–10) when, on D3 of in vitro culture, they presented 6 or more symmetric blastomeres, similar or slightly different, less than 20% fragmentation and absence of multinucleation. Embryos with the presence of multinucleation at any stage of development received a score of 2 directly, regardless of their morphology. The number of embryos to transfer was determined by the number of embryos available from each patient, the number of optimum embryos and patient age. Good morphology embryos that were not transferred were cryopreserved for further attempts. Embryos with the presence of multinucleation or compromised morphology were left in extended culture in sequential media and were cryopreserved if they reached the blastocyst stage.
Morphokinetic parameters analysed
The images acquired from each embryo were analysed with the EmbryoViewer® workstation (EV) in which every embryo developmental event was recorded at the exact moment it occurred, considering t = 0 as the time of microinjection (mean time between initial tICSI and final tICSI).
The timings of the appearance and fading of the PN, as well as the division times from 2-cell to 8-cell, were recorded.
The embryos with direct cleavage (≤5 h) from two to three cells were evaluated [29].
Statistical analysis
The mean and median times of PN appearance and fading, division to 2, 3, 4, 5, 6, 7 and 8 cells (t2, t3, t4, t5, t6, t7 and t8), synchrony (s2 = t4-t3; s3 = t8-t5) and duration of the second and third cell cycle (cc2 = t3-t2; cc3 = t5-t3) were estimated (hours) for every embryo group (implanted or not implanted). The time distribution between both study groups was compared with the Mann-Whitney test. The IBM SPSS STATISTICS v22 application was used, and all the tests were bilateral with a significance level of 5%.
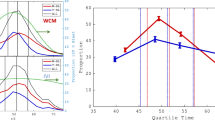
Data from every morphokinetic variable were divided into four quartiles with an even number of embryos. For each quartile, the implantation rate was calculated and compared by chi-square. Quartiles with similar implantation rate were grouped in order to identify the optimal range.
An algorithm was developed to identify the embryonic parameters associated with a higher implantation potential, considering morphokinetics (variables previously grouped in optimal ranges derived from quartile analysis and direct cleavage from two to three cells together) with the morphological embryo score on D3 by applying a decision tree.
The objective of the decision tree is to model a nominal response variable using a set of predictive variables, in order to obtain results that are easy to interpret and to allow the interactions between the predictive variables in their natural form to be taken into account (https://cran.r-project.org/web/packages/rpart/vignettes/longintro.pdf) . The decision tree uses a recursive algorithm. It starts by selecting the variable with the highest discriminatory capacity (at the top of the tree) generating two partitions; within each partition the same procedure is performed until no variable adds value to the tree (we used the stop and pruning model pre-defined by the Rpart package). The decision tree was estimated with the Rpart package [30], using the statistical package R (R version 3.2.3 (2015–12-10)—“Wooden Christmas-Tree” Copyright (C) 2015 The R Foundation for Statistical Computing Platform: x86_64-w64-mingw32/×64 (64 b).
Results
Our analysis included 439 KID cycles. Mean patient age was 37.15 ± 3.89 years. The cause of infertility was female aetiology in 22.1% of cycles, male infertility in 30.8%, 21.6% mixed infertility and 25.5% of the cycles were diagnosed as unexplained.
The group of patients whose embryos were implanted had a lower mean age (34.92 ± 3.21 vs 37.69 ± 3.68), and a higher number of oocytes recovered (9.65 ± 4.46 vs 8.58 ± 4.44) compared to the group of patients whose embryos did not implant, with significant differences (p < 0.05).
Of the total embryos analysed, 96 (12%) underwent direct cleavage from two to three cells. Only ten of the embryos with direct cleavage are implanted (IR 10.4%), while of the 704 embryos transferred that did not show direct cleavage, 130 are implanted (IR 18.5%).
Significant differences were found between the median times for the t4, t7 and s3 values between the embryos that implanted (140 embryos) and those that did not (660 embryos). No significant differences were observed regarding the appearance and fading of the PN, t2, t3, t5, t6 and t8 division times, duration of the second and third cell cycle, cc2 and cc3 or the second cell cycle synchrony s2 (Table 1).
The analysis of the time ranges with highest implantation rate showed significant differences for t2, t3, t4, t7, t8, s2 and cc2 values. For these variables, the highest implantation rate was observed in the three quartiles corresponding to the earlier time ranges (Table 2).
The hierarchical model obtained with the results from the analysis of the morphokinetic parameters (variables previously grouped and direct cleavage) and the embryologic morphology resulted in a decision tree in which the classical morphological score was the variable with the best prognostic factor of implantation. Consequently, the first differentiation was established between the embryos with a poor morphological score (score < 8) and optimal morphological score (score ≥ 8). The next differentiation levels were the morphokinetic parameters t4 and t8, with the time to reach the 4-cell stage being the most determining morphokinetic factor of implantation. Morphologically optimal embryos obtaining the best implantation rates (IR 29%) showed a t4 value <43 h and a t8 value <61.7 h and were named the good group. Morphologically optimal embryos with a t4 value <43 h and t8 value ≥61.7 h had a lower implantation rate (IR 17%) and were classified as the fair group. Embryos with optimal morphology with a slow development (t4 ≥ 43 h) had an implantation rate of 9% and were classified as the poor group (Fig. 1).
The group of embryos with a morphological score < 8 corresponding to embryos showing a poor morphology or multinucleation had an implantation rate of 10% and were therefore assigned to the poor prognosis group (poor group), also regardless of their morphokinetic parameters. For this group of embryos, no associated morphokinetic parameter was found that could be subdivided into different categories depending on the implantation rates (Fig. 1).
Of the 96 embryos with direct cleavage, 85 embryos were in the “poor” category of the decision tree (8/85 implanted), six embryos were “fair” (0/6 implanted) and 5 were “good” (2/5 implanted).
Discussion
This work describes a decision tree for the selection of embryos with the highest implantation potential by means of a combination of morphokinetic parameters and the classical morphological score, the latter resulting, in our hands, as the variable with the best implantation prognostic factor. Unlike other published studies, our study group is homogenous. All the cycles were performed in the same centre, and only fresh own oocyte cycles inseminated with ICSI were included. Cycles with donated gametes, vitrified oocytes or with PGD were excluded. No exclusion criteria were established regarding the characteristics of the couples, such as patient age, stimulation protocol, infertility factor or the number of oocytes retrieved in order to establish embryo selection criteria applicable to all patients undergoing IVF-ICSI. Cycles in which it was not possible to ascertain the implantation of all the embryos transferred were excluded. A total of 800 KID embryos were ultimately analysed.
Regarding the characteristics of the patients in both groups, patients with positive implantation embryos and patients with non-implanted embryos, as expected, show significant differences between them with respect to the mean age and number of oocytes recovered. Of course, from the nature of the group, when working with known implantation embryos, the patients whose embryos implanted presented a better prognostic factor.
For the assessment of the embryonic division rate through the analysis of the morphokinetic parameters, and due to the fact that the time variable does not present a normal distribution, we focused on the analysis of the time medians instead of on the corresponding mean values. The comparison between the median division time of embryos that implanted and those that did not presented significant differences for some specific values, indicating a significant association between these parameters and the implantation capability of the embryos in our laboratory conditions. In general, non-implanting embryos showed minimal and maximal times farthest from the median value for all the morphokinetic parameters analysed.
To compare the timings of the first embryo divisions with those already published by other authors that used the same equipment (Embryoscope®) we compared the mean values, since it is the most commonly used value in other studies. The first thing we observed was that the rate of embryo division varies among the different studies published. Focusing on the data published on embryos that have implanted, the division timings to 4 cells (t4) reported by Meseguer [17] tend to be shorter than our mean time values. However, the data published by Chamayou [31] show longer times, indicating a slower division rate of these embryos. Likewise, the division times of the third cell cycle obtained in our study are faster than those published by Chamayou and the embryos cultured in our centre reached 8-cell stage approximately 3 h earlier. In our hands, embryos with a slower division rate, similarly to what other authors have published, correspond to embryos presenting a lower implantation rate.
The difference in embryo division could be explained by the different laboratory conditions. The culture medium used in our laboratory (Vitrolife®) was different from the one used in the two other studies previously mentioned (Sage®) [17, 31], but although these two laboratories worked with the same medium, their culture conditions were not the same. In our centre, as well as in the case of Chamayou, the culture was carried out with a low oxygen concentration, whereas Meseguer used an oxygen concentration of 20%.
The series that reports embryo division times closest to ours is Del Canto’s [10]. Despite the use of a different culture medium (Origio®), the oxygen concentration for their culture was also low. Although these authors do not differentiate embryos by their implantation ability but rather through their ability to reach the blastocyst stage, we observed, on comparing their reported times to our own, that their initial division times until 6-cell stage (t6) were very similar. However, their t7 and t8 values were longer than ours.
When we compared our mean division times of all the analysed embryos to the control group values reported by Kirkegaard [32], we observed that their t7 and t8 times were also longer than ours, whereas the division rate was faster for the first embryo cleavage. In this case, the culture medium used was Cook®.
The comparison of the times published by different authors demonstrates that the intrinsic conditions of every laboratory can influence embryonic morphokinetics. Although previous publications found no differences between the culture media used [33], the set of multiple factors that create the conditions of every laboratory and which, as has been described, could amount to more than 200 [34], could be decisive in embryo development.
The division time analysis of all the embryos grouped in quartiles to identify the most relevant morphokinetic parameters to predict implantation showed significant differences for t2, t3, t4, t7, t8, s2 and cc2. Meseguer [17] also found significant differences for t2, t3, t4, s2 and cc2, as well as for t5, which in our series did not reach statistical significance. These authors did not analyse the times later than t5, and therefore, a comparison of later division times cannot be made. In general, our optimal division ranges are wider. This could be explained by the fact that the patients studied in our work correspond to the general ICSI population and not to selected good-prognosis patients and/or oocyte recipients who are the study group of the work mentioned earlier.
Regarding the development of a hierarchical model for embryo classification, in this study, the model was created based on the probability of implantation. The best prediction was obtained from the combination of embryo score based on the classical morphological parameters and the most relevant morphokinetic parameters. While some authors use the classical morphology for discarding non-viable or very abnormal embryos, in the decision tree that we propose the morphological score is the most relevant parameter and leaves morphokinetic parameters as secondary. Among the embryos considered optimal only by morphological criteria, morphokinetics makes it possible to deselect the embryos with the lowest implantation potential.
According to our hierarchical model of embryo selection, the morphokinetic parameters that are most predictive of implantation potential correspond to the time of the last divisions of the second and third cell cycles (t4 and t8). By applying these morphokinetic parameters to optimal morphology embryos, we can discriminate between three groups: those that implant best (good group), those with a fair probability (fair group) and those with fewest probabilities of implantation (poor group).
Despite the importance of classical morphology in the proposed tree, morphokinetic parameters take on great relevance, since they allow us to distinguish embryos which, after being classified as morphologically optimal, have a scant possibility of implantation (morphological score ≥ 8 and t4 ≥ 43 h). In the case of embryos with compromised morphology and embryos with the presence of multinucleation, with a morphological score < 8, no morphokinetic criteria could be found to establish subdivisions depending on their probability of implantation, possibly because the morphological classification is sufficiently robust when categorizing them as poor-prognosis embryos (poor group). It cannot be ruled out that studies on morphokinetics with a larger number of poor-morphology embryos could find a parameter that would make it possible to establish a difference in their classification and help to improve embryo selection in this group.
Although it is important to mention that multinucleated euploid embryos that reach the blastocyst state have the same capacity to implant as embryos from non-multinucleated euploid embryos (own data), and the culturing of multinucleated embryos to the blastocyst stage allows the selection of potentially viable embryos, previously published studies have observed a decreased ability of multinucleated embryos in early stages to reach the blastocysts stage [35, 36]. In addition, according to several authors, multinucleated embryos have a higher number of chromosomal alterations [37,38,39] and a higher rate of miscarriage [40, 41]. Taking into account that our morphological score categorizes embryos on cleavage stage (day 3), not in blastocyst stage, embryos with multinucleation were assigned a score of 2, regardless of their morphology.
Direct cleavage embryos had a lower implantation rate than other embryos studied with a normal cleavage pattern, as other authors had published before [29]. Most of them were “poor” embryos due to a bad morphology or a slow developmental rate (t4 > 43 h). It is important to note that those two of the five embryos that were in the “good” group, implanted despite direct cleavage.
When we compare our decision tree to those published by other authors, we find that the relevant parameters included in the algorithm are different. The parameters that Meseguer [17] includes in his algorithm, also based on implantation ability, are t5, s2 and cc2, and Basile [19], also from the same group, t3, cc2 and t5. These differences among the studies published to date have led some authors to consider that the correlation of morphokinetic parameters with embryonic potential are inconclusive and that neither the isolated morphokinetic parameters with predictive value nor the ranges of each parameter present a consensus among the different groups [20]. The Cochrane review published in 2015 [21] concluded that “For all types of TLS, with or without cell-tracking algorithms, versus conventional embryo incubation there was no conclusive evidence of a difference in live birth, miscarriage, stillbirth and clinical pregnancy rates per couple randomised. The quality of the evidence overall for all outcomes presented in this review is moderate or low, given the scarcity of studies”.
In our opinion, the algorithms proposed by the different groups that include different relevant parameters reinforce the idea that the intrinsic conditions of every laboratory may probably affect embryonic morphokinetics, and that the algorithm used in the daily routine must be designed in accordance with the relevant parameters specific to each centre. It would be advisable, where possible, for each laboratory to record the division times of its embryos and to define the criteria of each measurement [42] exactly following a well-defined standard operating procedure (SOP) and avoiding differences between operators. Moreover, the morphokinetic parameters of better prognosis should be identified according to the working conditions of the specific laboratory since, as we have described, they could vary from one centre to another. And finally, an algorithm should be created to select the best embryos for transfer according to the relevant parameters chosen and eventually integrate it into daily clinical practice (Fig. 2). An alternative to this individual approach could be to adopt one of the general algorithms commercially proposed which have been described to be independent of culture conditions and fertilization method [43].
The main limitations of this study derive from the retrospective nature of the data, an embryonic selection strategy based on classical morphology and the use of embryos with known implantation data (KID), which does not make it possible to know what will happen when the decision tree is applied in a different population. Other limitations derive from the nature of the decision tree that does not allow either specifying or quantifying the relative importance of each variable in the model or calculating the odds ratio for each parameter, as a logistic model would allow. However, the advantage of a hierarchical classification model is that it could be applied more intuitively. Due to the limitations of the selected model, the results of the decision tree should be taken with caution. A prospective validation with embryos without known implantation data would be relevant to confirm its effectiveness in any other scenario.
In conclusion, in our hands, the morphokinetic parameters make it possible to differentiate the embryos with the best implantation ability, although the classical morphological score continues to be the most important parameter in our decision tree. We recommend that centres that include TL technology in their laboratories adopt their own embryo selection protocol in accordance with their relevant morphokinetic parameters, since there are slight differences in each centre’s division times.
References
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26(6):1270–83.
ASEBIR. Cuaderno de embriología Clínica. Criterios ASEBIR de valoración Morfológica de Oocitos, Embriones Tempranos y Blastocistos Humanos. 2015. 3ª ed.
Capmany G, Taylor A, Braude PR, Bolton VN. The timing of pronuclear formation, DNA synthesis and cleavage in the human 1-cell embryo. Mol Hum Reprod. 1996;2(5):299–306.
Gonzales DS, Jones JM, Pinyopummintr T, Carnevale EM, Ginther OJ, Shapiro SS, et al. Trophectoderm projections: a potential means for locomotion, attachment and implantation of bovine, equine and human blastocysts. Hum Reprod. 1996;11(12):2739–45.
Wong CC, Loewke KE, Bossert NL, Behr B, De Jonge CJ, Baer TM, et al. Non-invasive imaging of human embryos before embryonic genome activation predicts development to the blastocyst stage. Nat Biotechnol. 2010;28(10):1115–21.
Kirkegaard K, Kesmodel US, Hindkjær JJ, Ingerslev HJ. Time-lapse parameters as predictors of blastocyst development and pregnancy outcome in embryos from good prognosis patients: a prospective cohort study. Hum Reprod. 2013;28(10):2643–51.
Conaghan J, Chen AA, Willman SP, Ivani K, Chenette PE, Boostanfar R, et al. Improving embryo selection using a computer-automated time-lapse image analysis test plus day 3 morphology: results from a prospective multicenter trial. Fertil Steril. 2013;100(2):412–9.
Cruz M, Garrido N, Herrero J, Pérez-Cano I, Muñoz M, Meseguer M. Timing of cell division in human cleavage-stage embryos is linked with blastocyst formation and quality. Reprod BioMed Online. 2012;25(4):371–81.
Hashimoto S, Kato N, Saeki K, Morimoto Y. Selection of high-potential embryos by culture in poly (dimethylsiloxane) microwells and time-lapse imaging. Fertil Steril. 2012;97(2):332–7.
Dal Canto M, Coticchio G, Mignini Renzini M, De Ponti E, Novara PV, Brambillasca F, et al. Cleavage kinetics analysis of human embryos predicts development to blastocyst and implantation. Reprod BioMed Online. 2012;25(5):474–80.
Campbell A, Fishel S, Bowman N, Duffy S, Sedler M. Hickman, C.F.M odelling a risk classification of aneuploidy in human embryos using non-invasive morphokinetics. Reprod BioMed Online. 2013;26(5):477–85.
Basile N, Nogales, Mdel C, Bronet F, Florensa M, Riqueiros M, et al. Increasing the probability of selecting chromosomally normal embryos by time-lapse morphokinetics analysis. Fertil Steril. 2014;101(3):699–704.
Rienzi L, Capalbo A, Stoppa M, Romano S, Maggiulli R, Albricci L, et al. No evidence of association between blastocyst aneuploidy and morphokinetic assessment in a selected population of poor-prognosis patients: a longitudinal cohort study. Reprod BioMed Online. 2015;30(1):57–66.
Aguilar J, Motato Y, Escribá MJ, Ojeda M, Muñoz E, Meseguer M. The human first cell cycle: impact on implantation. Reprod BioMed Online. 2014;28(4):475–84.
Azzarello A, Hoest T, Mikkelsen AL. The impact of pronuclei morphology and dynamicity on live birth outcome after time-lapse culture. Hum Reprod. 2012;27(9):2649–57.
Lemmen JG, Agerholm I, Ziebe S. Kinetic markers of human embryo quality using time-lapse recordings of IVF/ICSI-fertilized oocytes. Reprod BioMed Online. 2008;17(3):385–91.
Meseguer M, Herrero J, Tejera A, Hilligsoe KM, Ramsing NB, Remohí J. The use of morphokinetics as a predictor of embryo implantation. Hum Reprod. 2011;26(10):2658–71.
Rubio I, Galán A, Larreategui Z, Ayerdi F, Bellver J, Herrero J, et al. Clinical validation of embryo culture and selection by morphokinetic analysis: a randomized, controlled trial of the EmbryoScope. Fertil Steril. 2014;102(5):1287–94.
Basile N, Vime P, Florensa M, Aparicio Ruiz B, García Velasco JA, Remohí J, et al. The use of morphokinetics as a predictor of implantation: a multicentric study to define and validate an algorithm for embryo selection. Hum Reprod. 2015;30(2):276–83.
Kaser DJ, Racowsky C. Clinical outcomes following selection of human preimplantation embryos with time-lapse monitoring: a systematic review. Hum Reprod Update. 2014;20(5):617–31.
Armstrong S, Arroll N, Cree LM, Jordan V, Farquhar C. Time-lapse systems for embryo incubation and assessment in assisted reproduction. Cochrane Database Syst Rev. 2015;27(2):CD011320. doi:10.1002/14651858.CD011320.pub2.
Kirkegaard K, Ahlström A, Ingerslev HJ, Hardarson T. Choosing the best embryo by time lapse versus standard morphology. Fertil Steril. 2015;103(2):323–32.
Muñoz M, Cruz M, Humaidan P, Garrido N, Pérez-Cano I, Meseguer M. The type of GnRH analogue used during controlled ovarian stimulation influences early embryo developmental kinetics: a time-lapse study. Eur J Obstet Gynecol Reprod Biol. 2013;168(2):167–72.
Cruz M, Garrido N, Gadea B, Muñoz M, Pérez-Cano I, Meseguer M. Oocyte insemination techniques are related to alterations of embryo developmental timing in an oocyte donation model. Reprod BioMed Online. 2013;27(4):367–75.
Bodri D, Sugimoto T, Serna JY, Kondo M, Kato R, Kawachiya S, et al. Influence of different oocyte insemination techniques on early and late morphokinetic parameters: retrospective analysis of 500 time-lapse monitored blastocysts. Fertil Steril. 2015;104(5):175–81.
Ciray HN, Aksoy T, Goktas C, Ozturk B, Bahceci M. Time-lapse evaluation of human embryo development in single versus sequential culture media- a sibling oocyte study. J Assist Reprod Genet. 2012;29(9):891–900.
Kirkegaard K, Hindkjaer JJ, Ingerslev HJ. Effect of oxygen concentration on human embryo development evaluated by time-lapse monitoring. Fertil Steril. 2013;99(3):738–44.
Boada M. Is there time for time-lapse in the art laboratory? Abstract book of the 30th ESHRE annual meeting, Munich, Germany. Hum Reprod. 2014;29(Suppl 1):i1–i389.
Rubio I, Kuhlmann R, Agerholm I, Kirk J, Herrero J, Escribá MJ, et al. Limited implantation success of direct-cleaved human zygotes: a time-lapse study. Fertil Steril. 2012;98(6):1458–63.
Therneau, T., Atkinson, B., Ripley, B. Rpart: recursive partitioning and regression trees. R package version 4.1–10. 2015.
Chamayou S, Patrizio P, Storaci G, Tomaselli V, Alecci C, Ragolia C, et al. The use of morphokinetic parameters to select all embryos with full capacity to implant. J Assist Reprod Genet. 2013;30(5):703–10.
Kirkegaard K, Hindkjaer JJ, Ingerslev HJ. Human embryonic development after blastomere removal: a time-lapse analysis. Hum Reprod. 2012;27(1):97–105.
Basile N, Morbeck D, García-Velasco J, Bronet F, Meseguer M. Type of culture media does not affect embryo kinetics: a time-lapse analysis of sibling oocytes. Hum Reprod. 2013;28(3):634–41.
Pool, T.B., Schoolfield, J., Han, D. Embryo Culture. 2012; Volumen 912 of the series Methods in Molecular Biology. Pp 367–386.
Alikani M, Calderon G, Tomkin G, Garrisi J, Kokot M, Cohen J. Cleavage anomalies in early human embryos and survival after prolonged culture in-vitro. Hum Reprod. 2000;15(12):2634–43.
Yakin K, Balaban B, Urman B. Impact of the presence of one or more multinucleated blastomeres on the developmental potential of the embryo to the blastocyst stage. Fertil Steril. 2005;83(1):243–5.
Hardarson T, Hanson C, Sjögren A, Lundin K. Human embryos with unevenly sized blastomeres have lower pregnancy and implantation rates: indications for aneuploidy and multinucleation. Hum Reprod. 2001;16(2):313–8.
Munné S. Chromosome abnormalities and their relationship to morphology and development of human embryos. Reprod BioMed Online. 2006;12(2):234–53.
Agerholm IE, Hnida C, Crüger DG, Berg C, Bruun-Petersen G, Kølvraa S, et al. Nuclei size in relation to nuclear status and aneuploidy rate for 13 chromosomes in donated four cells embryos. J Assist Reprod Genet. 2008;25(2–3):95–102.
Scott L, Finn A, O'Leary T, McLellan S, Hill J. Morphologic parameters of early cleavage-stage embryos that correlate with fetal development and delivery: prospective and applied data for increased pregnancy rates. Hum Reprod. 2007;22(1):230–40.
Fauque P, Audureau E, Leandri R, Delaroche L, Assouline S, Epelboin S, et al. Is the nuclear status of an embryo an independent factor to predict its ability to develop to term? Fertil Steril. 2013;99(5):1299–1304.e3.
Kirkegaard K, Agerholm IE, Ingerslev HJ. Time-lapse monitoring as a tool for clinical embryo assessment. Hum Reprod. 2012;27(5):1277–85.
Petersen BM, Boel M, Montag M, Gardner DK. Development of a generally applicable morphokinetic algorithm capable of predicting the implantation potential of embryos transferred on day 3. Hum Reprod. 2016;31(10):2231–44.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carrasco, B., Arroyo, G., Gil, Y. et al. Selecting embryos with the highest implantation potential using data mining and decision tree based on classical embryo morphology and morphokinetics. J Assist Reprod Genet 34, 983–990 (2017). https://doi.org/10.1007/s10815-017-0955-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-0955-x