Abstract
Despite impaired mother-child interactions noted in youth with attention-deficit/hyperactivity disorder (ADHD), there is no such information for their siblings. This study aimed to test whether the affected and unaffected siblings, like youth with ADHD, also encountered impaired mothering and mother-child relationships as compared to typically developing youth (TD). The sample consisted of 122 probands (107 males, 87.7 %), aged 10–16, with DSM-IV ADHD, 44 affected (26 males, 59.1 %) and 78 unaffected (28 males, 35.9 %) siblings, and 122 TD youth. Both participants and their mothers received psychiatric interviews (K-SADS-E) about the participants and reported maternal parenting style, mother-child interactions and child behavioral problems at home. Based on both reports, probands with ADHD and affected siblings (only youth report) had more impaired relationships, more behavioral problems at home, and less perceived family support than unaffected siblings and TD youth. Probands with ADHD had higher maternal authoritarian control than unaffected siblings. The findings suggest that impaired mothering, mother-child interactions, and family support are related to the presence of ADHD diagnosis in both probands and their affected siblings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Having a child with attention-deficit/hyperactivity disorder (ADHD) is associated with increased likelihood of parent-child arguments (Edwards et al. 2001), sibling rivalry and family conflicts (Mikami and Pfiffner 2008). Bidirectional relationships have been observed between child ADHD symptom severity and the quality of parent-child relationship (Lifford et al. 2008). Common comorbidities of ADHD such as oppositional defiant disorder (ODD) or conduct disorder (CD) have consistently been found to further impair mother-child relationships and family interactions in this distinct ADHD subgroup (Johnston and Mash 2001; Kashdan et al. 2004; Psychogiou et al. 2007). Moreover, ADHD youth, regardless of the persistence of symptoms, and their mothers reported more authoritarian mothering, less maternal affection and caring, more impaired mother-child relationships and less perceived family support than typically developing (TD) youth and their mothers (Gau and Chang 2013). Despite extensive research in maternal and family process in children with ADHD, little is known about the mothering and mother-child relationships in siblings of children with ADHD. The few reports that do exist were conducted with TD or siblings unaffected by ADHD in Western populations (Cartwright et al. 2011; Richards et al. 2015; Tarver-Behring et al. 1985).
While much attention has been paid to maternal and family process in children with ADHD, these factors in their siblings have only recently emerged as an important topic of research and clinical interest given that the siblings not only share the same family environment, but are also more likely to have ADHD and other psychiatric comorbidities when compared to TD youth (Yang et al. 2011). Siblings tend to model the maladaptive behaviors of ADHD children, and perhaps increase maternal stress (Kendall 1999). One school of thought suggests that maternal stress from raising an ADHD child tends to “spill over” into the mother’s relationship with her other children; and mother-child conflict in children with ADHD had been closely associated with mother-child conflict in the siblings (Barkley 2006; Tarver-Behring et al. 1985). In contrast, another school of thought suggests that the unaffected siblings may have obtained better adjustment skills through interactions with the siblings with ADHD (Smith et al. 2002), and had lower levels of maternal criticism and mother-child hostility than the index youth with ADHD (Cartwright et al. 2011). Moreover, the unaffected siblings, after observing the conflictual interaction between their mothers and ADHD siblings, may overcompensate by excelling in social competence outside of home (Smith et al. 2002). There has been no study examining these maternal and family factors among affected and unaffected siblings of children with ADHD simultaneously. We assume having a child with ADHD will influence the mother’s parenting and relationships with other children, regardless of ADHD status, and if the sibling also has ADHD symptoms, further impaired maternal and family process would be expected because of the double influence of child ADHD symptoms on maternal parenting and mother-child relationship (Gau and Chang 2013). We will also assess maternal psychopathology including depression and ADHD as covariates, since these problems may affect the mothers’ perspectives of their children’s behaviors, maternal parenting styles and mother-child relationships.
Reports by both parent and child in ADHD research are highly valued; however, there has been limited research regarding parent-child agreement on mothering and family processes in children with ADHD; most of the studies are about parent-child agreement related to quality of life (QoL) in ADHD (Klassen et al. 2006; Marques et al. 2013). The study findings regarding parent-child agreement are controversial with some studies reporting discordance between parent and child perspectives on the severity of symptoms and treatment outcomes in chronic illness including ADHD (Vance et al. 2002), while other studies demonstrate a higher parent-child agreement in QoL reports in children with ADHD compared with TD children (Klassen et al. 2006; Marques et al. 2013). Greater parent-child agreement in observational domains (e.g., physical) rather than non-observational domains (e.g., self-esteem, wellbeing, behavior, psychosocial health) was also suggested (Klassen et al. 2006). Moreover, only one study reported on the parent-child agreement regarding behavior and family cohesion using the Child Health Questionnaire, and children reported better family cohesion and better behaviors than did parents (Klassen et al. 2006). To the best of our knowledge, there has been no study on parent-child agreement regarding mothering and mother-child relationships in children with ADHD.
Thus, it was our intent to study whether mothering, mother-child relationships and family support would differ between ADHD children and their siblings, especially siblings with ADHD. In this study, we investigated maternal and family process among youth with ADHD, their affected and unaffected siblings, and TD youth, and the mother-child agreement on these measures. Our hypotheses were: 1) ADHD youth and their affected siblings would receive less affection/care and more authoritarian control/overprotection than unaffected siblings and TD youth; 2) Siblings, regardless of affected status, would have more impaired mother-child relations and family dysfunction than TD youth; 3) ADHD youth, regardless of the ADHD status of their siblings, and their affected siblings would receive less maternal affection/care and have less perceived family support than unaffected siblings and TD youth; and 4) Youth with ADHD and affected siblings and their mothers would have lower agreement on reporting of maternal parenting style and family functions when compared with unaffected siblings and TD youth and their mothers.
Methods
Participants
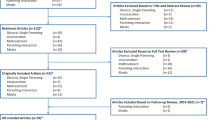
We assessed 122 youth (male, 87.7 %) at the mean age of 12.83 (standard deviation, SD = 1.5), who had a DSM-IV diagnosis of ADHD (APA 1994), from a university hospital and 122 comparison (or TD) youth (males, 87.7 %) without ADHD at the mean age of 12.87 (SD = 1.6) from the similar school districts as the ADHD group. In addition, 122 siblings, including 44 affected siblings (male, 59.1 %; mean age ± SD, 11.58 ± 2.5 years) and 78 unaffected siblings (male, 35.9 %; mean age ± SD, 12.70 ± 2.8 years), participated. The clinical diagnosis of ADHD was confirmed by psychiatric interviews with the participants and parents using the Chinese Kiddie epidemiologic version of the Schedule for Affective Disorders and Schizophrenia, K-SADS-E ( Gau et al. 2005) for past and current (past 6 month) diagnosis of ADHD and other psychiatric disorders. The youth with ADHD enrolled in the study only had one sibling, regardless of the affected status. The TD group and their parents also received K-SADS-E interviews to confirm that they did not have a lifetime diagnosis of ADHD, and the family history method was used to ensure that none of the siblings of TD were affected with ADHD or other major neuropsychiatric disorders before enrollment into the study. The final diagnosis was decided based on the best estimate. All participants who had psychosis, autism spectrum disorders, or a full-scale IQ score less than 80 were excluded.
Measures
All the measures were completed by both the youth and their mothers; the only exception was the assessment for maternal psychopathology including the Adult ADHD Self-Report Scale and the Adult Self-Report Inventory-4, which were used to assess mother’s ADHD symptoms and other psychopathology as covariates in the analysis.
The Chinese Version of the K-SADS-E
The Chinese K-SADS-E (Gau and Soong 1999) is a semi-structured interview scale for the systematic assessment of both past and current episodes of mental disorders in children and youth (Gau et al. 2005). The overall sensitivity and specificity of the screening interview for any Chinese K-SADS-E diagnostic category were calculated to be 78 % and 98 % (Gau et al. 2005; Gau et al. 2010a), the generalized kappa coefficients among interviewers ranging from 0.73 to 0.96 for all mental disorders included in the Chinese K-SADS-E, and it has been widely used in clinical (e.g., Chiang et al. 2015; Chiang et al. 2013; Chou et al. 2015) and epidemiological (e.g., Gau et al. 2005) studies. The Cronbach’s alpha values used to measure the internal consistency for the inattention and hyperactivity-impulsivity symptoms were 0.97 and 0.94, respectively.
The Chinese Version of the Parental Bonding Instrument (PBI)
The PBI is a 25-item instrument (item-rated on a 4-point Likert scale from very likely to very unlikely) measuring the parental behaviors and attitudes toward their child during the child’s first 16 years (Parker 1979). Half of the items were reverse-coded. The PBI consists of three principle dimensions: Affectionate/Care (12 items), Overprotection (7 items), and Authoritarian Control (6 items) ( Gau 2007; Parker 1979). The Chinese PBI is a reliable instrument with Cronbach’s alphas of 0.75 to 0.84, and has been widely used in Taiwanese studies (Chen et al. 2015; Gau 2007; Lai et al. 2010; Lin and Gau 2013). The internal consistency (Cronbach’s alpha, α) of the PBI in this study was high for the Affectionate/Care (Mother, α = 0.73; Child, α = 0.89), and Authoritarian Control (Mother, α = 0.80; Child, α = 0.82) and moderate for Overprotection (Mother, α = 0.72; Child, α = 0.67).
The Chinese Version of the Social Adjustment Inventory for Children and Adolescents (SAICA)
The SAICA is a 77-item semi-structured interview scale designed for administration to school-age children aged 6–18 about themselves, or to parents completed about their children (John et al. 1987). The SAICA was used to assess the child’s current functioning in the school, spare time, peer relations, and home behaviors domains. The intraclass correlations for test-retest reliability and the Cronbach’s alpha for internal consistency of the subscales ranged from 0.45 to 0.84 and from 0.71 to 0.86, respectively (Gau et al. 2006). The measure has been widely used in several studies (Chen et al. 2015; Hsiao et al. 2013; Kawabata et al. 2012; Lin et al. 2012).
We used two subscales of the home relations domain: (1) interactions with mother (three items): does things with mother, is friendly/affectionate toward mother, and talks with mother (rating from 1, very true to 4, not at all true); and (2) problems at home (four items): strong negative reaction or refusal to do chores or honor restrictions, dangerous irresponsibility around home, damages home or family property, and physically threatens or attacks parents (rating from 1, not a problem to 4, a severe problem). A higher mean score indicated either less active interactions with mothers or more severe problems at home (John et al. 1987). The internal consistency (Cronbach’s alpha, α) of the two subscales used in this study was high for the interactions with mother (Mother, α = 0.82; Child, α = 0.81), and moderate for behavioral problems at home (Mother, α = 0.66; Child, α = 0.60).
The Chinese Family APGAR
The Family APGAR was designed to assess the five family functioning domains: Adaptation, Partnership, Growth, Affection, and Resolve (0 for hardly ever, 1 for some of the time, and 2 for almost always) with a higher score indicating greater perceived family support (Smilkstein et al. 1982). The Chinese Family APGAR has been reported as a reliable instrument with Cronbach’s alpha of 0.89, and has been used in recent clinic-based (e.g., Chang et al. 2013; Lin et al. 2015) and community-based (e.g., Chen et al. 2015; Lai et al. 2010) studies. The Cronbach’s alpha for this scale in this study was high (Mother, α = 0.90; Child, α = 0.90).
Assessment of Maternal Psychopathology
Maternal reports of psychopathology were included in multivariate analyses as covariates to control for potential reporter bias. The mothers were assessed for current ADHD symptoms with the Chinese version of the Adult ADHD Self-Report Scale (ASRS, 18-item) (Gau and Chiang 2009; Kessler et al. 2005; Yeh et al. 2008), and for depressive symptoms with the sum score of major depressive disorder and dysthymia subscales of the Chinese Version of the Adult Self-Report Inventory-4, or ASRI-4 (Chien et al. 2011). The Chinese ASRS has a high test-retest reliability (Intraclass correlation = 0.80 to 0.85) and internal consistency (α = 0.83 to 0.91) (Yeh et al. 2008), and it has been previously used in adult ADHD studies (e.g., Gau et al. 2007). The internal consistency of the Chinese ASRS in this study was high (Inattention, α = 0.81; Hyperactivity-Impulsivity, α = 0.82). The Chinese ASRI-4 has been used to assess the DSM-IV psychopathology in epidemiologic (Hsu et al. 2012; Lai et al. 2010; Lin and Gau 2013; Tseng et al. 2014) and clinical (Chang et al. 2013; Gau and Chang 2013; Lin et al. 2015) studies in Taiwan. The depression symptoms score from the Chinese ASRI-4 has a high test-retest reliability (Intraclass correlation = 0.75) and internal consistency (α = 0.83) (Chien et al. 2011). The internal consistency for the combined depressive scores used in this study was high (α = 0.90).
Procedures
The Research Ethics Committee approved this study prior to study implementation. Written informed consent was obtained from both participants and their parents. All participants and their parents were interviewed independently by well-trained interviewers to make the lifetime and current (past 6 months) diagnoses of ADHD and other psychiatric disorders of the participants according to the DSM-IV diagnostic criteria using the Chinese K-SADS-E. The participants and their mothers also reported on the SAICA to provide information about participants’ interactions with their mothers and behavioural problems at home. Both informants then completed the self-administered questionnaires about parenting and perceived family support and maternal ADHD and depressive symptoms (mother’s reports only) at the laboratory. The information regarding the youths’ medication history was obtained by interviews and validated by medical records of prescription.
Data Analyses
The SAS 9.1 (2004) was used for data analysis. The four (five) comparison groups were: youth with ADHD (with affected siblings and with unaffected siblings), their affected and unaffected siblings, and TD youth. The descriptive results of the demographics were displayed as frequencies and percentages and tested for significance by chi-square test; for continuous variables, mean and SD, and analysis of variance. We used a linear multi-level model with a random effect to take the lack of independence of 122 youth with ADHD and their 122 siblings from the same family (an index youth with ADHD and his/her sibling within the same family, random effect) into account and fixed effects from the comparison groups and other covariates in the model to compare the mean scores of the maternal parenting style and family functions between different comparison groups (the fixed effect). Level 1 was the youth participants, while Level 2 was the family, and the variables tested were maternal parenting styles (affectionate/care, overprotection, authoritarian control), mother-child relations, problems at home, and perceived family support. The Bonferroni method was used to adjust p values in post hoc analysis owing to multiple comparisons. The age, sex, comorbidity of youth, medication use and maternal ADHD and depression symptoms were controlled in the model. All the continuous independent variables were centered around the means prior to the analyses.
We also calculated Pearson’s correlations (r) and intraclass correlations and performed paired t-tests for the agreement and differences between youths’ and mothers’ reports on maternal and family measures. Furthermore, in order to understand whether ADHD status and sibling status predicts discrepancy between mother’s and child’s reports, we conducted a multi-level linear regression model treating the discrepancy between parent and child reports as a dependent variable and comparison groups as independent variables controlling for sex, age, and random effect from the same family.
Results
Sample Description
Males were more prevalent in the ADHD and TD groups than the sibling group (Table 1). The affected siblings were younger than the ADHD (Cohen’s d = 0.61) and TD groups (Cohen’s d = 0.62), mothers of children with ADHD were younger than those of TD (Cohen’s d = 0.31), and both parents of the ADHD group were less educated than those of the TD group. Affected siblings had a later onset age than youth with ADHD (Cohen’s d = 0.41). Although youth with ADHD and their affected siblings had more severe inattention (Cohen’s d = 1.36 ~ 3.72) and hyperactivity-impulsivity symptoms (Cohen’s d = 1.29 ~ 1.91) than unaffected siblings and TD youth, ADHD youth were more likely to receive medication than their affected siblings (Cohen’s d = 0.41) (Table 1).
Mothering in Youth with ADHD, the Siblings, and TD Youth
Both unaffected siblings (Cohen’s d = 0.46 ~ 0.47, p < 0.01) and TD youth (Cohen’s d = 0.40 ~ 0.77, p < 0.001) received more maternal affection and care (Table 2, Supplementary Fig. S1) and less control (Cohen’s d = −0.56 ~ −0.76) than youth with ADHD based on reports from both mothers and youth. Moreover, affected siblings received more authoritarian controls from their mothers than unaffected siblings did (Cohen’s d = 0.56, p < 0.001), but less control than the youth with ADHD (Cohen’s d = 0.56, p < 0.001, Table 2). Youth with ADHD also reported greater maternal overprotection than TD youth (Cohen’s d = 0.44, p < 0.01, Table 2).
Mother-Child Relationship and Family Function in Youth with ADHD and the Siblings
Based on mother and youth reports, ADHD youth had more impaired interactions with their mothers (Cohen’s d = 0.56, p < 0.001 and Cohen’s d = 0.79, p < 0.001, respectively) (Table 2, Supplementary Fig. S2) and more behavioral problems at home (Cohen’s d = 0.48, p < 0.001 and Cohen’s d = 1.15, p < 0.001, respectively) than their unaffected siblings and TD youth. Meanwhile, based on maternal reports, affected siblings had less impaired interactions with mothers (Cohen’s d = 0.46), fewer problems at home (Cohen’s d = 0.31) than ADHD youth, but more problems at home than TD youth (Cohen’s d = 0.77). Youth with ADHD and their siblings, regardless of affected status, reported less perceived family support (Cohen’s d = 0.43 ~ 0.90) than TD (Table 2, Supplementary Fig. S3).
Mothering, Mother-Child Relationships, and Family Functions among Youth with ADHD (Subgrouped by Affected Status of Siblings), Siblings, and TD Youth
Next, we did a subgroup analysis to see if sibling affected status influenced maternal and family processes in youth with ADHD. We compared the measures among five groups: ADHD youth with affected siblings (n = 44) and with unaffected siblings (n = 78), their affected (n = 44) and unaffected siblings (n = 78), and TD youth (n = 122). The demographic data comparisons among five groups (Supplementary Table S1) were similar to those among four groups (Table 1) as described above.
Based on youths’ reports, ADHD youth with affected siblings had less maternal affection/care than unaffected siblings (Cohen’s d = 0.54) ( p < 0.05, Supplementary Table S2); based on maternal reports, youth with ADHD, regardless of sibling affected status, had less affection/care than both sibling groups (Cohen’s d = 0.44 ~ 0.56) and TD youth (Cohen’s d = 0.76 ~ 0.90). Both reports revealed that youth with ADHD, regardless of sibling affected status, had more authoritarian control than both sibling groups (Cohen’s d = 0.50 ~ 0.72) and the TD group (Cohen’s d = 0.48 ~ 0.86). Yet affected siblings reported more authoritarian control than unaffected siblings (Cohen’s d = 0.56); while based on youth reports, youth with ADHD with unaffected siblings received a higher level of maternal overprotection than TD youth (Cohen’s d = 0.57) (Supplementary Table S2, Supplementary Fig. S4).
Both mother and youth reports showed that youth with ADHD, regardless of sibling affected status, had more impaired interactions with mother (Cohen’s d = 0.47 ~ 0.92) (Supplementary Table S2, Supplementary Fig. S5), more problems at home (Cohen’s d = 0.45 ~ 1.06) and less perceived family support (Cohen’s d = 0.47 ~ 0.93) than their unaffected siblings and TD youth (Supplementary Table S2). Meanwhile, based on maternal reports, youth with ADHD with affected siblings had more impaired mother-child relationship (Cohen’s d = 0.57) and problems with parents (Cohen’s d = 0.45) than affected siblings. In addition, the siblings had less perceived family support than TD youth (Cohen’s d = 0.69 ~ 0.90) (Supplementary Table S2, Supplementary Fig. S6).
Agreement and Difference between Youth’s and Mother’s Reports
Our last hypothesis regarding a low agreement between youth’s and mother’s reports was partially supported in the ADHD proband and affected sibling groups. In general, there were significant, but low to moderate correlations for affection/care, impaired interactions with mothers, and authoritarian control for most of the groups except in the particular group of the ADHD youth who had affected siblings. In this group, they did not show significant correlations for any maternal/family measures. Moreover, only ADHD youth who had unaffected siblings, and unaffected siblings had significant positive correlations between mothers’ and youths’ reports on behavioral problems at home, while only ADHD youth who had unaffected siblings demonstrated a positive correlation with their mothers on reports for perceived family support (Table 3). Furthermore, there were no significant correlations for reports of maternal overprotection across the five groups (Table 3).
Paired t-tests revealed that youth reported significantly higher maternal control than mothers did in all five groups; mothers reported greater maternal affection/care to the index youth than youth did in the affected sibling and TD groups; youth reported more behavioral problems at home than mothers did in the unaffected sibling and TD groups; and mothers reported greater perceived family support than youth did in the TD group (Table 3).
We also found that ADHD status did not influence the degree of discrepancy between mother’s and youth’s reports based on the overall group effects. Further investigating each individual group as compared to the TD group, the discrepancy did not vary across different groups except for the following two conditions. First, compared to the TD group, there was a greater magnitude of mothers’ reports of more severe behavioral problems at home than youth’s self-reports in the ADHD group. Second, compared to the TD group, the discrepancy of mother-youth reports on affection/care maternal parenting is less in the unaffected sibling group than the TD group (Table 4).
Comorbidity with ODD and Mothering and Family Function in Youth with ADHD, Siblings, and TD Youth
We did an additional analysis to investigate whether the comorbidity with ODD affected mothering and family function in the present study. The number of youth and rates of ODD were 61.5 %, 31.8 %, 12.8 % and 4.1 % for the ADHD (75/122), affected siblings (14/44), unaffected siblings (10/78) and TD (5/122) groups. Youth with ADHD + ODD reported that they obtained less affection and care (Cohen’s d = 0.43) and more overprotection (Cohen’s d = 0.53) from their mothers than youth with ADHD only; and maternal reports showed that youth with ADHD + ODD had more impaired mother-child interactions (Cohen’s d = 0.58), more behavioral problems at home (Cohen’s d = 0.97), and perceived less family support (Cohen’s d = 0.45) than youth with ADHD only (Supplementary Table S3).
Discussion
The current work is the first study focusing on the maternal and family process in siblings of youth with ADHD, focused on the affected status of siblings. We found that youth with ADHD, and their affected siblings obtained less affection/care and more authoritarian control from their mothers, had more impaired interactions with the mothers and more problems at home than unaffected siblings and TD youth. All children in families with a child with ADHD perceived less support than TD youth, based on the reports of youth and/or their mothers.
Maternal Parenting in ADHD, Siblings, and TD Youth
Our first hypothesis was partially supported in this study, where youth with ADHD and the affected siblings, but not unaffected siblings, had lower affection/care and more authoritarian control from the mother when compared with TD youth. It is suggested that inattentive and hyperactive symptoms of the affected child place multiple demands on the mother, increase maternal parenting challenges (Barkley 1985) and negative mothering practices such as increased maternal rejection (Pimentel et al. 2011), and decrease maternal responsiveness (Woodward et al. 1998). Moreover, it should be noted that approximately two-thirds of the affected siblings did not have the clinical diagnosis of ADHD but met the criteria for ADHD based on clinical evaluation and the K-SADS-E interview with the parents in this study. Thus, mothers, within the context of not knowing that the affected sibling had ADHD, may feel more distressed as the discrepancy between their expectations and the actual performance of affected siblings widens.
Smith et al. (2002) pointed out that unaffected siblings often overcompensate for the actions of the index ADHD child by demonstrating adjustment and social competence outside the family, or trying to be extra good in school and avoid causing trouble. Thus, mothers may be more likely to practice similar mothering styles with unaffected siblings and TD youth, and practice similar mothering styles, such as less affection/care and more authoritarian control, to index ADHD youth and the affected siblings. This assumption is further supported by a previous study, where parents reported unaffected siblings shared more similarities with the TD group, while the index youth with ADHD and the affected siblings shared similar emotional and conduct problems (Steinhausen et al. 2012).
Mother-Child Relationship and Family Function in ADHD, Siblings, and TD Youth
Our second hypothesis was also partially supported, where the affected siblings, but not the unaffected siblings, had more impaired mother-child relationship than TD youth. This further supports a close association between ADHD symptom severity and difficulties in mother-child relationship (Lifford et al. 2008). In addition, mothers reported that ADHD youth had more impaired mother-child relationships than the affected siblings. Mothers may be more likely to view the index child with ADHD, who has received psychiatric service, as more problematic than the affected sibling; especially those siblings who have not utilized psychiatric service. Our earlier study also showed that parents of children with ADHD in a clinic-based sample reported more social impairment including poor parent-child relationships and behavioral problems than did parents of community-based children with ADHD (Gau et al. 2010b).
Child ADHD symptoms may also trigger mother-child hostility and negative interactions concurrently and longitudinally, leading to the development of child CD/ODD later in life (Lifford et al. 2009), and subsequently impair the mother-child relations in the long term ( Barkley et al. 1991; Gau and Chang 2013; Lee et al. 2013). The presence of ODD in youth with ADHD in our study was related to less affectionate and more overprotective parenting, more impaired interaction with mothers and perceived family support and more behavioral problems at home, although the reports between youth and mothers were not always consistent. This finding was in agreement with previous literature where comorbidity of ODD in youth with ADHD was associated with more impaired mother-child relationships and family relations (Kashdan et al. 2004; Psychogiou et al. 2007).
Youth with ADHD and their siblings had more problems at home in the present study, while all the youth from families with ADHD had less perceived family support than TD youth (maternal report). Unaffected siblings did not have more problems at home when compared to TD youth, since unaffected siblings usually behave “properly” and have generally good social coping skills (Smith et al. 2002). Moreover, the unaffected siblings are often asked to be the “caretaker” and the “responsible one” among the siblings (Smith et al. 2002), which may positively reinforce their “good” behaviors at home.
It draws our attention that mothers reported that all youth from the families with ADHD children, including the unaffected siblings, had less perceived family support than TD youth in our study. This is compatible with a previous study finding that having one or more family members with the diagnosis of ADHD was associated with a less resourced and more non-supportive family environment (Corwin et al. 2012). Families with children with ADHD are at risk for a variety of family dysfunctions including maternal depression (Brown and Pacini 1989; Pelham and Lang 1999), marital discord (Brown and Pacini 1989), parent-child conflicts (Lifford et al. 2008), and sibling rivalry (Mikami and Pfiffner 2008) all of which may be linked to less perceived family support. Furthermore, unaffected siblings might have less family support, since their needs may be masked by their good behaviors and under-recognized by the family. On the whole, ADHD may serve as a catalyst for negative family interactions, where affected youth have more impaired mother-child interactions and more problems at home, and all youth from the family perceive less family support.
Affected Status of Siblings, Mothering, and Family Function
Our third hypothesis was partially supported by the findings of this study, where only ADHD youth with affected siblings received less maternal affection/care than the siblings, regardless of affected status, and TD youth. ADHD symptoms of the child may place great demands on the mothers, and child ADHD is associated with maternal mood and anxiety symptoms (Edwards et al. 2001; Gau 2007; Pelham and Lang 1999); which are associated with negative parenting (Nelson et al. 2009) and impaired mother-child interactions (Chi and Hinshaw 2002). The core ADHD symptoms of the index children and affected siblings may interact synergically to influence maternal parenting, the mother-child relationship, and functioning in families having at least two children with ADHD. Mothers may have difficulty providing equal care between the index youth with ADHD and affected siblings and may be more frustrated with exacerbated family dysfunction, widening the gap between child’s need and mother’s care. For example, mothers need to make efforts to take care of the affected siblings, those without formal diagnosis and treatment, which may negatively impact their care for the index youth with ADHD. In short, lower maternal affection/care for the ADHD youth with affected siblings may be attributed to both maternal distress for caring for more than one child with ADHD and the severity of child’s ADHD symptoms. Lastly, as we hypothesized in the second part of the third hypothesis, youth with ADHD, regardless of affected status of their siblings, and their affected siblings had less perceived family support. As we had discussed earlier, this may be due to the challenges encountered by families of children with ADHD, leading to a less resourced and supportive environment (Corwin et al. 2012).
Similar or Different Perception of Maternal and Family Process between Youth and their Mothers
We addressed the issue of agreement and differences between mother’s and child’s report on the perception of mothering, the mother-child relationship and family functioning in our last hypothesis. We found that the affected siblings and TD youth and their mothers perceive maternal affection/care differently, with youth reporting less maternal affection/care than the mothers. Secondly, mothers and youth were consistent in reporting more impaired interactions with mothers but inconsistent reports of maternal control. Adolescence marks the beginning of independence and bargaining for autonomy, and is associated with more conduct problems and risk taking behaviors. Mothers, adjusting to the changes in relations with their children might exert more control to protect their children from the risks and danger, and the mother-child relationships in adolescence may be more conflictual and less intimate than in childhood (Edwards et al. 2001). As for family functioning, unaffected siblings and TD youth, when compared to their mothers’ reports, reported more problems at home. Unaffected siblings and TD, when compared with affected youth, are less likely to overburden their parents with behavioral and conduct problems, and injuries (Shilon et al. 2012) or to cause trouble at home. Moreover, the problems and behavioral abnormalities of unaffected siblings may be overlooked or neglected since mothers may have their time and attention occupied by the ADHD youth and affected siblings (Steinhausen et al. 2012).
ADHD youth with an unaffected sibling and TD youth reported less perceived family support than the mothers. This emphasizes the different views youth and mothers have on family functioning. Moreover, it is interesting that TD youth reported less perceived family support than their mothers, which may be due to different perspectives on family support held by the youth and the mother. Chinese culture emphasizes “xiao-shun” for parent-child relationships, where children should be obedient and not upset the parents; while parents were expected to practice “guan” and “chao” (Chao 1994), meaning to provide authoritarian teaching and caring, during child-rearing. Hence, in the context of Chinese culture, Taiwanese youth may perceive less family support since they were less likely to disclose their problems to or discuss their perspectives to avoid confronting and disappointing their parents.
Limitations and Strengths
Our study has two major limitations. First, the measures of maternal and family process were based on subjective reports from the participants and their mothers. Second, the cross-sectional design prevented us from making causal inferences. Another limitation to our study was that we only recruited adolescents with ADHD who had one sibling, regardless of affected or unaffected status of the siblings, and we did not record the data of birth order for each proband-sibling dyad. In contrast, the study has the strength of being the first study to target family processes among youth with ADHD, their affected and unaffected siblings and TD controls with both mother and youth as informants. Future studies should consider reports of other sources (e.g., the fathers) and inclusion of objective assessments of mother-child interactions with a longitudinal design.
Conclusion
As the first large-scale research targeting the maternal and family processes among youth with ADHD and their affected and unaffected siblings as compared to TD with comprehensive maternal and family measures, our findings suggested that the presence of ADHD had an impact on a wide-range of maternal parenting behavior and family functioning. Children in a family with any ADHD children, regardless of affected status, perceive less family support than TD. The findings suggest that problems of unaffected children in these families may be overlooked. Individual needs and resources of family members, especially the siblings of individuals with ADHD, should be carefully assessed.
References
American Psychiatric Association (1994). DSM-IV: diagnostic and statistical manual of mental disorders, fourth edition (4th ed.). Washington DC: American Psychiatric Association.
Barkley, R. A. (1985). The social behavior of hyperactive children: developmental changes, drug effects, and situational variation. In R. P. McMahon & R. Peters (Eds.), Childhood disorders: behavioural-developmental approaches (pp. 218–243). New York: Bruner/Mazel.
Barkley, R. A. (2006). Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment (3rd ed.). New York: Guilford.
Barkley, R. A., Fischer, M., Edelbrock, C., & Smallish, L. (1991). The adolescent outcome of hyperactive children diagnosed by research criteria--III. Mother-child interactions, family conflicts and maternal psychopathology. Journal of Child Psychology and Psychiatry, 32, 233–255.
Brown, R. T., & Pacini, J. N. (1989). Perceived family functioning, marital status, and depression in parents of boys with attention deficit disorder. Journal of Learning Disabilities, 22, 581–587.
Cartwright, K. L., Bitsakou, P., Daley, D., Gramzow, R. H., Psychogiou, L., Simonoff, E., et al. (2011). Disentangling child and family influences on maternal expressed emotion toward children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 1042–1053. doi:10.1016/j.jaac.2011.07.006.
Chang, L. R., Chiu, Y. N., Wu, Y. Y., & Gau, S. S. (2013). Father's parenting and father-child relationship among children and adolescents with attention-deficit/hyperactivity disorder. Comprehensive Psychiatry, 54, 128–140. doi:10.1016/j.comppsych.2012.07.008.
Chao, R. K. (1994). Beyond parental control and authoritarian parenting style: understanding Chinese parenting through the cultural notion of training. Child Development, 65, 1111–1119.
Chen, Y. L., Chen, S. H., & Gau, S. S. (2015). ADHD and autistic traits, family function, parenting style, and social adjustment for internet addiction among children and adolescents in Taiwan: a longitudinal study. Research in Developmental Disabilities, 39, 20–31. doi:10.1016/j.ridd.2014.12.025.
Chi, T. C., & Hinshaw, S. P. (2002). Mother-child relationships of children with ADHD: the role of maternal depressive symptoms and depression-related distortions. Journal of Abnormal Child Psychology, 30, 387–400.
Chiang, H. L., Huang, L. W., Gau, S. S., & Shang, C. Y. (2013). Associations of symptoms and subtypes of attention-deficit hyperactivity disorder with visuospatial planning ability in youth. Research in Developmental Disabilities, 34, 2986–2995. doi:10.1016/j.ridd.2013.06.020.
Chiang, H. L., Chen, Y. J., Lo, Y. C., Tseng, W. Y., & Gau, S. S. (2015). Altered white matter tract property related to impaired focused attention, sustained attention, cognitive impulsivity and vigilance in attention-deficit/ hyperactivity disorder. Journal of Psychiatry & Neuroscience, 40, 325–335. doi:10.1503/jpn.140106.
Chien, Y. L., Gau, S. S., & Gadow, K. D. (2011). Sex difference in the rates and co-occurring conditions of psychiatric symptoms in incoming college students in Taiwan. Comprehensive Psychiatry, 52, 195–207. doi:10.1016/j.comppsych.2010.03.009.
Chou, T. L., Chia, S., Shang, C. Y., & Gau, S. S. (2015). Differential therapeutic effects of 12-week treatment of atomoxetine and methylphenidate on drug-naive children with attention deficit/hyperactivity disorder: a counting Stroop functional MRI study. European Neuropsychopharmacology, 25, 2300–2310. doi:10.1016/j.euroneuro.2015.08.024.
Corwin, M., Mulsow, M., & Feng, D. (2012). Perceived family resources based on number of members with ADHD. Journal of Attention Disorders, 16, 517–529. doi:10.1177/1087054710397133.
Edwards, G., Barkley, R. A., Laneri, M., Fletcher, K., & Metevia, L. (2001). Parent-adolescent conflict in teenagers with ADHD and ODD. Journal of Abnormal Child Psychology, 29, 557–572.
Gau, S. S. (2007). Parental and family factors for attention-deficit hyperactivity disorder in Taiwanese children. Australian & New Zeland Journal of Psychiatry, 41, 688–696. doi:10.1080/00048670701449187.
Gau, S. S., & Chang, J. P. (2013). Maternal parenting styles and mother-child relationship among adolescents with and without persistent attention-deficit/hyperactivity disorder. Research in Developmental Disabilities, 34, 1581–1594. doi:10.1016/j.ridd.2013.02.002.
Gau, S. S., & Chiang, H. L. (2009). Sleep problems and disorders among adolescents with persistent and subthreshold attention-deficit/hyperactivity disorders. Sleep, 32, 671–679.
Gau, S. F., & Soong, W. T. (1999). Psychiatric comorbidity of adolescents with sleep terrors or sleepwalking: a case-control study. Australian & New Zeland Journal of Psychiatry, 33, 734–739.
Gau, S. S., Chong, M. Y., Chen, T. H., & Cheng, A. T. (2005). A 3-year panel study of mental disorders among adolescents in Taiwan. American Journal of Psychiatry, 162, 1344–1350. doi:10.1176/appi.ajp.162.7.1344.
Gau, S. S., Shen, H. Y., Soong, W. T., & Gau, C. S. (2006). An open-label, randomized, active-controlled equivalent trial of osmotic release oral system methylphenidate in children with attention-deficit/hyperactivity disorder in Taiwan. Journal of Child and Adolescent Psychopharmacology, 16, 441–455. doi:10.1089/cap.2006.16.441.
Gau, S. S., Kessler, R. C., Tseng, W. L., Wu, Y. Y., Chiu, Y. N., Yeh, C. B., & Hwu, H. G. (2007). Association between sleep problems and symptoms of attention-deficit/hyperactivity disorder in young adults. Sleep, 30, 195–201.
Gau, S. S., Lin, Y. J., Cheng, A. T., Chiu, Y. N., Tsai, W. C., & Soong, W. T. (2010a). Psychopathology and symptom remission at adolescence among children with attention-deficit-hyperactivity disorder. Australian & New Zeland Journal of Psychiatry, 44, 323–332. doi:10.3109/00048670903487233.
Gau, S. S., Lin, Y. J., Shang, C. Y., Liu, S. K., Chiu, Y. N., & Soong, W. T. (2010b). Emotional/behavioral problems and functional impairment in clinic- and community-based children with attention-deficit/hyperactivity disorder in Taiwan. Journal of Abnormal Child Psychology, 38, 521–532. doi:10.1007/s10802-009-9381-6.
Hsiao, M. N., Tseng, W. L., Huang, H. Y., & Gau, S. S. (2013). Effects of autistic traits on social and school adjustment in children and adolescents: the moderating roles of age and gender. Research in Developmental Disabilities, 34, 254–265. doi:10.1016/j.ridd.2012.08.001.
Hsu, C. Y., Gau, S. S., Shang, C. Y., Chiu, Y. N., & Lee, M. B. (2012). Associations between chronotypes, psychopathology, and personality among incoming college students. Chronobiology International, 29, 491–501. doi:10.3109/07420528.2012.668995.
John, K., Gammon, G. D., Prusoff, B. A., & Warner, V. (1987). The social adjustment inventory for children and adolescents (SAICA): testing of a new semistructured interview. Journal of the American Academy of Child and Adolescent Psychiatry, 26, 898–911.
Johnston, C., & Mash, E. J. (2001). Families of children with attention-deficit/hyperactivity disorder: review and recommendations for future research. Clinical Child and Family Psychology Review, 4, 183–207.
Kashdan, T. B., Jacob, R. G., Pelham, W. E., Lang, A. R., Hoza, B., Blumenthal, J. D., & Gnagy, E. M. (2004). Depression and anxiety in parents of children with ADHD and varying levels of oppositional defiant behaviors: modeling relationships with family functioning. Journal of Clinical Child and Adolescent Psychology, 33, 169–181.
Kawabata, Y., Tseng, W. L., & Gau, S. S. (2012). Symptoms of attention-deficit/hyperactivity disorder and social and school adjustment: the moderating roles of age and parenting. Journal of Abnormal Child Psychology, 40, 177–188. doi:10.1007/s10802-011-9556-9.
Kendall, J. (1999). Sibling accounts of attention deficit hyperactivity disorder (ADHD). Family Process, 38, 117–136.
Kessler, R. C., Adler, L., Ames, M., Demler, O., Faraone, S., Hiripi, E., et al. (2005). The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychological Medicine, 35, 245–256.
Klassen, A. F., Miller, A., & Fine, S. (2006). Agreement between parent and child report of quality of life in children with attention-deficit/hyperactivity disorder. Child: Care, Health and Development, 32, 397–406. doi:10.1111/j.1365-2214.2006.00609.x.
Lai, M. C., Chiu, Y. N., Gadow, K. D., Gau, S. S., & Hwu, H. G. (2010). Correlates of gender dysphoria in Taiwanese university students. Archives of Sexual Behavior, 39, 1415–1428. doi:10.1007/s10508-009-9570-y.
Lee, P. C., Lin, K. C., Robson, D., Yang, H. J., Chen, V. C., & Niew, W. I. (2013). Parent-child interaction of mothers with depression and their children with ADHD. Research in Developmental Disabilities, 34, 656–668. doi:10.1016/j.ridd.2012.09.009.
Lifford, K. J., Harold, G. T., & Thapar, A. (2008). Parent-child relationships and ADHD symptoms: a longitudinal analysis. Journal of Abnormal Child Psychology, 36, 285–296. doi:10.1007/s10802-007-9177-5.
Lifford, K. J., Harold, G. T., & Thapar, A. (2009). Parent-child hostility and child ADHD symptoms: a genetically sensitive and longitudinal analysis. Journal of Child Psychology and Psychiatry, 50, 1468–1476. doi:10.1111/j.1469-7610.2009.02107.x.
Lin, Y. H., & Gau, S. S. (2013). Association between morningness-eveningness and the severity of compulsive internet use: the moderating role of gender and parenting style. Sleep Medicine, 14, 1398–1404. doi:10.1016/j.sleep.2013.06.015.
Lin, Y. J., Lai, M. C., & Gau, S. S. (2012). Youths with ADHD with and without tic disorders: comorbid psychopathology, executive function and social adjustment. Research in Developmental Disabilities, 33, 951–963. doi:10.1016/j.ridd.2012.01.001.
Lin, Y. J., Lo, K. W., Yang, L. K., & Gau, S. S. (2015). Validation of DSM-5 age-of-onset criterion of attention deficit/hyperactivity disorder (ADHD) in adults: comparison of life quality, functional impairment, and family function. Research in Developmental Disabilities, 47, 48–60. doi:10.1016/j.ridd.2015.07.026.
Marques, J. C., Oliveira, J. A., Goulardins, J. B., Nascimento, R., O., L., M., A., & Casella, E. B. (2013). Comparison of child self-reports and parent proxy-reports on quality of life of children with attention deficit hyperactivity disorder. Health and Quality of Life Outcomes, 11, 186. doi:10.1186/1477-7525-11-186.
Mikami, A. Y., & Pfiffner, L. J. (2008). Sibling relationships among children with ADHD. Journal of Attention Disorders, 11, 482–492.
Nelson, J. A., O'Brien, M., Blankson, A. N., Calkins, S. D., & Keane, S. P. (2009). Family stress and parental responses to children's negative emotions: tests of the spillover, crossover, and compensatory hypotheses. Journal of Family Psychology, 23, 671–679. doi:10.1037/a0015977.
Parker, G. (1979). Parental characteristics in relation to depressive disorders. British Journal of Psychiatry, 134, 138–147.
Pelham Jr., W. E., & Lang, A. R. (1999). Can your children drive you to drink? Stress and parenting in adults interacting with children with ADHD. Alcohol Research & Health, 23, 292–298.
Pimentel, M. J., Vieira-Santos, S., Santos, V., & Vale, M. C. (2011). Mothers of children with attention deficit/hyperactivity disorder: relationship among parenting stress, parental practices and child behaviour. ADHD Attention Deficit Hyperactivity Disorders, 3, 61–68. doi:10.1007/s12402-011-0053-3.
Psychogiou, L., Daley, D. M., Thompson, M. J., & Sonuga-Barke, E. J. (2007). Mothers' expressed emotion toward their school-aged sons. Associations with child and maternal symptoms of psychopathology. European Child & Adolescent Psychiatry, 16, 458–464. doi:10.1007/s00787-007-0619-y.
Richards, J. S., Hartman, C. A., Franke, B., Hoekstra, P. J., Heslenfeld, D. J., Oosterlaan, J., et al. (2015). Differential susceptibility to maternal expressed emotion in children with ADHD and their siblings? Investigating plasticity genes, prosocial and antisocial behaviour. European Child & Adolescent Psychiatry, 24, 209–217. doi:10.1007/s00787-014-0567-2.
SAS 9.1 [Computer software]. (2004). Cary, NC: SAS Institute Inc.
Shilon, Y., Pollak, Y., Aran, A., Shaked, S., & Gross-Tsur, V. (2012). Accidental injuries are more common in children with attention deficit hyperactivity disorder compared with their non-affected siblings. Child: Care, Health and Development, 38, 366–370. doi:10.1111/j.1365-2214.2011.01278.x.
Smilkstein, G., Ashworth, C., & Montano, D. (1982). Validity and reliability of the family APGAR as a test of family function. The Journal of Family Practice, 15, 303–311.
Smith, A. J., Brown, R. T., Bunke, V., Blount, R. L., & Christophersen, E. (2002). Psychosocial adjustment and peer competence of siblings of children with attention-deficit/hyperactivity disorder. Journal of Attention Disorders, 5, 165–177.
Steinhausen, H. C., Zulli-Weilenmann, N., Brandeis, D., Muller, U. C., Valko, L., & Dreschsler, R. (2012). The behavioural profile of children with attention- deficit/hyperactivity disorder and of their siblings. European Child and Adolescent Psychiatry, 21, 157–164. doi:10.1007/s0078–012-0249-x.
Tarver-Behring, S., Barkley, R. A., & Karlsson, J. (1985). The mother-child interactions of hyperactive boys and their normal siblings. American Journal of Orthopsychiatry, 55, 202–209.
Tseng, M. C., Gau, S. S., Tseng, W. L., Hwu, H. G., & Lee, M. B. (2014). Co-occurring eating and psychiatric symptoms in Taiwanese college students: effects of gender and parental factors. Journal of Clinical Psychology, 70, 224–237. doi:10.1002/jclp.22014.
Vance, A., Costin, J., Barnett, R., Luk, E., Maruff, P., & Tonge, B. (2002). Characteristics of parent and child reported anxiety in psychostimulant medication naïve clinically referred children with attention deficit hyperactivity disorder combined type (ADHD-CT). Australian and New Zealand Journal of Psychiatry, 36, 234–239.
Woodward, L., Taylor, E., & Dowdney, L. (1998). The parenting and family functioning of children with hyperactivity. Journal of Child Psychology and Psychiatry, 39, 161–169.
Yang, L. K., Shang, C. Y., & Gau, S. S. (2011). Psychiatric comorbidities in adolescents with attention-deficit hyperactivity disorder and their siblings. Canadian Journal of Psychiatry, 56, 281–292.
Yeh, C. B., Gau, S. S., Kessler, R. C., & Wu, Y. Y. (2008). Psychometric properties of the Chinese version of the adult ADHD self-report scale. International Journal of Methods in Psychiatric Research, 17, 45–54. doi:10.1002/mpr.241.
Acknowledgments
This work was supported by grants from the National Health Research Institute (NHRI-EX95-9407PC, NHRI-EX96-9407PC, NHRI-EX97-9407PC, NHRI-EX98-9407PC, NHRI-EX100-0008PI, NHRI-EX101-0008PI), Taiwan. We would like to express our thanks to the participants, their siblings and parents for their contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study has been approved by the Research Ethics Committee (approval number: 9361700470; ClinicalTrials.gov number, NCT00417781) of National Taiwan University Hospital Institutional Review Board and therefore all procedures performed in studies involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interests
There is no conflict of interest with regard to this work.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(DOCX 1162 kb)
Rights and permissions
About this article
Cite this article
Chang, J.PC., Gau, S.SF. Mother-Child Relationship in Youths with Attention-Deficit Hyperactivity Disorder and their Siblings. J Abnorm Child Psychol 45, 871–882 (2017). https://doi.org/10.1007/s10802-016-0218-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-016-0218-9