Abstract
Introduction
Evidence suggests that mothers are negative and critical when talking about their children with behaviour problems. However the association with specific types of behaviour problems and the influence of both child and adult psychopathology on these relationships require further clarification.
Methods
Speech samples were gathered from mothers of 100 school-aged boys and coded using standard Expressed Emotion (EE) categories. Levels of maternal and child psychopathology were ascertained using standardised questionnaires completed by the mother.
Results
There were significant and positive correlations between criticism and child ADHD, conduct and emotional symptoms respectively. There were also significant and negative correlations between EOI and child ADHD and conduct problems.
Conclusions
The findings of the current study suggest that when considered together EE is driven more by the child rather than by maternal characteristics and these effects are specific to conduct and emotional problems. The implications of the findings are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parent’s attitudes and behaviour towards their children play a potentially important role in shaping developmental trajectories [21]. The construct of Expressed Emotion (EE) is used to describe the quality of parenting attitudes, emotional relationships and related practices. EE has two dimensions: Criticism (CRIT) which encompasses feelings of negativity and resentment and emotional over involvement (EOI) which involves extreme over-protective and self-sacrificing behaviours. These two components appear to correlate differentially with child internalising and externalising disorders [1]. In a community sample, it was found that child disruptive behaviours were associated with high parental criticism and child anxiety disorders with high emotional over-involvement [24].
These findings, while of interest, are difficult to interpret for two reasons. First, different types of childhood disorder often co-occur and it is hard to identify which aspects of childhood behaviour problems are specifically associated with EE. Second, parents of children with behaviour problems often have mental health difficulties themselves. Therefore child and parental psychopathology are likely to confound the relationship between EE and behaviour [12]. This is especially important as it appears there is a link between parental psychopathology and EE. Previous research has shown that parents’ psychiatric diagnosis was a significant predictor of high EE towards their children [10]. EE could also be a characteristic of the parent (i.e., a trait) or a parental response to specific circumstances or to the child (i.e., state). Some evidence showed that EOI was related to the state of the child and CRIT to parental trait [22].
These findings highlight the importance of considering both child and family influences on parenting as children’s behaviour can influence parents and vice versa. For example, using an experimental design it was found that adult stress and negative mood was influenced by child deviant behaviour [18]. While another study found that parents of ADHD children were more negative and controlling when the child was on placebo medication and more positive and supportive when their child was on active medication [2]. Alternatively, however, according to Patterson’s coercion theory [17] parental criticism might escalate pre-existing child problems. For example, a previous longitudinal study demonstrated that criticism measured in preschool years predicted classification of ADHD symptoms over 4 years later [19].
The problem of comorbidity, the overlap between parent and child psychopathology and the link between parental EE and mental health problems means that associations between psychopathology and EE can only be disentangled by examining both parent and child psychopathology across multiple domains simultaneously. The study reported in this paper was designed with this aim in mind. Three elements of child symptoms of psychopathology; Attention Deficit Hyperactivity Disorder (ADHD), conduct problems (CP) and emotional symptoms (EMO) and three elements of maternal symptoms of psychopathology; ADHD, low mood (LMOOD) and aggression (AGG) were studied together. Maternal depression was selected due to its high prevalence in mothers of school age children and its association with parental criticism and hostility [14]. In a similar way, adult ADHD which often co-exists with aggression is now recognised as a valid disorder in adulthood, and growing evidence suggests it has a negative effect on parenting [16]. The participants were drawn from the community and were restricted to mother-son dyads. The community sample was used to avoid biases associated with the process of clinical referral [26]. The sample was restricted to mothers and son dyads to reduce the complexity of the design of this initial study and to ease interpretation of the results.
Based on previous research it was predicted that:
-
(1)
Child ADHD and CP symptoms would be associated with increased criticism and these effects would be independent of one another.
-
(2)
Child EMO symptoms would be associated with emotional over-involvement.
-
(3)
Adult ADHD, DEP and AGG would be associated with increased criticism and these effects would be independent of one another.
-
(4)
When parent and child psychopathology were considered side by side the child effects would persist suggesting that EE is driven by child characteristics rather than parent related factors. Implicit in this hypothesis is the idea that child behaviours “provoke” the parental response. These “child effects” are based on studies, which have demonstrated that when children with behavioural problems are on medication, parental negativity and hostility is reduced [3].
Method
Participants
The sample consisted of 100 boys (Mean age = 7.96, SD = 1.87) drawn from 6 schools randomly chosen from those that traditionally collaborate with the University of Southampton for research and training purposes. Initially 168 mothers (19% of those approached) of boys completed and returned questionnaires but only 100 gave their consent to take part in the EE study. There were no differences between mothers who declined and those who agreed to participate in the EE study in terms of socio-demographic variables and child and maternal symptoms of psychopathology.
The sample was predominantly white British (97%) and of mixed socio-economic status. About 72% of mothers were married, 16% were divorced, 4% were co-habitating, and 8% were single. About 30% of mothers had professional and managerial occupations, 24% skilled non-manual occupations, 27% had skilled and partly skilled manual occupations, 1% were retired and 18% were unemployed.
Measures
Child
ADHD, CP and EMO: Child ADHD, conduct problems and emotional symptoms were measured using the Strengths and Difficulties Questionnaire (SDQ; 9). The SDQ is a brief behavioural screening questionnaire that can be completed by parents or teachers of children aged 4–16. The hyperactivity, conduct and emotional scales contain 5 items each with a 3-point response scale, ranging from (0 = Not True) to (2 = Certainly True). Cut-offs are standardised to identify the top 10% of children within the UK [9]. The scale is well validated and has good test–retest reliability (α = 0.85).
Adult
ADHD: Maternal ADHD symptoms were measured with the Adult ADHD Rating Scale (AARS; 2). This is an 18-item self-report scale based on the DSM-IV definition of symptoms of ADHD rated over the past 6 months on a 4-point scale, ranging from (0 = Rarely) to (3 = Very often). It has good psychometric properties and correlates with spousal, parental, and cohabiting partner ratings of symptoms. Scores of nine symptoms or more have been shown to identify adults with a clinical level of difficulty [4]. In the present study, the Cronbach’s alpha was satisfactory at 0.84.
LMOOD: Maternal low mood were measured with the General Health Questionnaire (GHQ12; 8). The GHQ is a widely used, reliable, and well validated questionnaire. Scores from the 12 items are combined to produce an overall rating. Individuals respond on a 4-point scale, ranging from (0 = Better than usual) to (1 = Much less than usual). The presence of three symptoms indicates low mood [6]. In the present study, the Cronbach’s alpha was satisfactory at 0.90.
AGG: Parent AGG was measured using the Aggression Questionnaire [5]. The AQ12 is a reliable (α’s range from 0.88 to 0.92) and valid measure with four subscales: Physical aggression, verbal aggression, anger and hostility. Each contains three items, with a 6-point scale ranging from (1—Extremely uncharacteristic of me) to (6—Extremely characteristic of me). The standard cut-off score of 42 and above was used in the present study to identify elevated levels of anti-social characteristics (2SDs above the mean from a normal population sample; 4).
Expressed Emotion (EE): EE was measured using the Five Minutes Speech Sample (FMSS; 15). Parents were asked to speak for 5 min about their child without any interruption. They were asked to describe their relationship with the child and what their child is like. The coding system considers both tone and content of the entire speech sample.
The FMSS consists of nine components: initial statement (scored as positive, neutral, negative where higher scores represent a negative initial statement), relationship (scored as positive, neutral, negative where higher scores represent negative relationship), criticism (a frequency count), dissatisfaction with the child (present or absent), emotional display during the speech sample (present or absent), statements of attitude toward the child (a frequency count of comments that express strong feelings of positive emotion or a willingness to do anything for the child), self-sacrificing or overprotective behaviour or lack of objectivity (present or absent), excessive detail about the past (present or absent) and number of positive remarks about the child.
The inter-rater reliability was examined on 25% of the tapes (average reliability r = 0.85). For each component the inter-rater reliability was high: initial statement (x 2 = 0.78), relationship (x 2 = 0.80), dissatisfaction (x 2 = 0.77), criticism (r = 0.84), sacrifice (x 2 = 0.90), emotional display (x 2 = 0.91), details about the past (x 2 = 0.98), positive remarks (r = 0.81) and statements of attitude towards the child (r = 0.86).
Procedure
Ethical approval to conduct the study was received from the Ethics Committee at the University of Southampton. Head teachers of schools were contacted and were provided with information about the study. After teachers’ consent was received, information letters, consent forms and packs of questionnaires together with free post envelopes were sent to the parents. Parents were instructed to complete the questionnaires and return them upon completion. The confidentiality of the information provided by parents was emphasized on the covering letter. Parents who completed the questionnaires and gave their consent to participate in the EE phase of the study were contacted by telephone and they were asked to talk for 5 min about their child and their relationship with the child over the last 6 months. Speech samples were audio-taped and coded for subsequent analysis.
Results
Table 1 displays correlations among child and maternal symptoms of psychopathology. Most of the correlations were significant and as expected. In addition, most of the correlations among components of EE were significant (Tables 2 and 3).
Following the standard instructions for scoring EE [15], negative initial statement, negative relationship, criticism and dissatisfaction were collapsed into one variable—criticism (CRIT). Emotional display, statements of attitude, self-sacrificing behaviour, details about the past and all positive remarks, not only the excessive ones [15], were collapsed into a second variable—emotional over-involvement (EOI). Table 4 displays the correlations among CRIT and EOI and symptoms of psychopathology. CRIT correlated with increased child symptoms and EOI with decreased child ADHD and conduct problems (Table 4).
Stepwise multiple regression analyses were used to examine the independent contribution of child and adult symptoms to CRIT and EOI. For each dependent variable, CRIT and EOI, two hierarchical regression models were examined: the first one with child symptoms in Step 1 and maternal symptoms in Step 2; the second one with the reversed order.
When CRIT was the outcome variable, and child symptoms were entered in Step 1, the results revealed significant and positive associations between CRIT and child conduct problems and emotional symptoms respectively (Table 5). These associations remained significant after entering maternal symptoms in Step 2. Furthermore, quite surprisingly, the results revealed a negative association between CRIT and maternal depressive symptoms. In the second model, when maternal symptoms were entered in Step 1 (Table 6), the results revealed a significant and positive association between CRIT and maternal ADHD symptoms. In Step 2, when child symptoms were entered in the model, this association became non-significant. However there were significant and positive associations between CRIT and child conduct problems and emotional symptoms respectively. There was also a negative association between CRIT and maternal low mood.
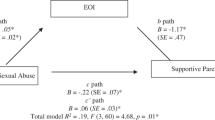
When EOI was the outcome variable, and child symptoms were entered in Step 1, the results revealed a significant and negative association between EOI and child conduct problems. This association remained significant in Step 2, when maternal symptoms were entered in the model (Table 7). This association was replicated in the second regression model, when maternal symptoms were entered in Step 1 and child symptoms in Step 2 (Table 8).
Further analysis was conducted in order to examine whether the inverse association between EOI and child conduct problems was accounted for by the positive remarks and statements of attitude. For this purpose, a new variable was created by collapsing together positive remarks and statements of attitude (termed positive attitude—POSAT). When child problems were entered in Step 1, the results revealed a significant and negative association between POSAT and conduct problems (α = −0.38, P = 0.000). This association remained significant after entering maternal symptoms in Step 2. The results were the same when maternal symptoms entered in Step 1 and child symptoms in Step 2 (α = −0.38, P = 0.006).
Discussion
The primary goal of the study was to examine the relationship between EE and child and maternal symptoms of psychopathology considered together. In general, the results provide evidence for the specific role of child conduct and emotional problems in contributed to elevated parental EE. The first hypothesis was partially supported as children with elevated conduct problems had mothers who expressed more criticism towards them. Previous studies have also established that parents of children with conduct problems are more critical than parents of children without conduct problems [1, 10, 11, 19, 24]. Mothers were also more critical towards children with elevated ADHD. This finding is consistent with what was found in a previous study, using a clinical sample of preschool children with ADHD [6]. However, in the regression models this association became non significant.
Furthermore while child emotional symptoms were associated with greater criticism the predicted association between emotional problems and increased maternal emotional over-involvement did not occur. The results do not support suggestions within the literature that EOI is high among parents of children with anxiety disorders [24] or among parents of children at risk for anxiety [11]. However the study used a 5-item scale measuring both anxious and affective symptoms, and maybe was not precise enough to show the predicted association.
Child conduct problems were associated with decreased emotional over-involvement and this association remained significant after controlling for maternal symptoms. Some evidence suggests that EOI consists of positive elements such as positive remarks about the child and positive statements of attitude. Thus EOI might reflect more than two dimensions. In support of this suggestion, in a sample of parents of children with asthma [25] it was found that parents with high EOI fell into two groups: in the first group, parents scored high on EOI because of the presence of a statement of attitude and more than five positive remarks while in the second group, parents scored high on EOI because of the other scoring criteria. Interestingly, parents in the second group reported problems with roles, affect responsiveness, general functioning, and boundary problems in their parent-child relationship whereas the first group had better functioning in their roles and affect responsiveness. In the current study, we examined this hypothesis, and it was found that the association between EOI and conduct problems was accounted by positive remarks and statements of attitude about the future. Certainly more research is needed to clarify the components of EOI and their implications for child’s adjustment. EOI might be developmentally appropriate for a young child who needs guidance and support but quite intrusive for an adolescence who builds autonomy and independence.
There were few associations between maternal psychopathology and EE. The study provided evidence that mothers with elevated ADHD symptomatology expressed more criticism. However this association was not significant after controlling for child symptoms. In other words, as predicted, maternal criticism seems to be driven by child rather than maternal characteristics. There was no support that mothers with increased aggressive symptoms were more critical. Surprisingly, and contrary to what it was predicted, maternal depressive symptoms were negatively associated with criticism. This finding might reflect the fact that mothers with low mood may be less talkative and have fewer opportunities to express critical comments about the child. The sample was also drawn from the community. Previous studies using community samples have found that EE was not related to maternal mental health, such as depression, anxiety, distress and introspectiveness [24].
In summary, the results from the stepwise regressions revealed that the associations between criticism and child emotional and conduct problems remained significant after controlling for maternal psychopathology. The findings suggest that it is child rather than parent psychopathology that contributes to the high EE. However the study was cross sectional and did not allow us to test cause-effect relationships. It is likely that characteristics of the child influence parental EE and parental EE may influence child adjustment. Longitudinal data would be required to test this hypothesis.
Other methodological limitations should be taken into account. Part of the analysis was based on mothers’ reports on both their child and their own symptoms and this might have led to inflated correlations. The reliance on self-reports may pose a problem for objectivity and rater bias. Mothers reported on their own and their child symptoms and their responses might have been influenced by systematic personal biases associated with factors such as expectations and attributions about child difficult behaviour, or other factors such as parental depression [7]. It is possible that mothers with symptoms of psychopathology were biased and negative, and they tended to report more problems in themselves and their children [20]. A better option would be to use independent reports. For example, husbands could report on mothers’ symptoms and teachers to report on child symptoms. Teachers see the children in a structured environment on a daily basis and have children without any behavioural problems to which they can compare the child being assessed.
Finally, the study examined EE in mothers only and did not take into account fathers EE. Considering that EE measures the home environment, it is worth examining whether there are differences in the EE of mothers and fathers or whether EE is a reflection of common experiences with the child. In a related way, the study did not explore the role of the gender of the child and it is not known if the results can be generalised to girls. Future research will explore these effects in mother–daughter and father–son and father–daughter dyads. Finally the study was based on a community sample and it is not clear if the results are generalised to clinically referred samples. The study did not take into account the role of maternal personality which might had influenced levels of EE. Evidence suggests that individuals who scored high on EE were more conventional in their attitudes and behaviour, and they felt less capable and optimistic about their lives. Individuals who scored low on EE showed higher levels of empathy and tolerance and they had a stronger tendency towards achievement via independence [13].
Despite the limitations, the findings of the study have important implications for interventions and clinical practice. Criticism should be a target of interventions as mothers high in criticism might engage in negative interactions with their child thus contributing to the escalation of child conduct problems. Criticism also increases the risk for psychological disorder in children beyond the risk of parental affective disorder [23].
References
Asarnow J, Tompson M, Hamilton E, Goldstein M, Guthrie D (1994) Family expressed emotion, childhood-onset depression, and childhood-onset schizophrenia spectrum disorders: Is expressed emotion a nonspecific correlate of child psychopathology or a specific risk factor for depression? J Abnor Child Psychol 22:129–146
Barkley R (1989) Attention-deficit hyperactivity disorder. In: Mash E, Barkley R (eds) Treatment of childhood disorders. New York: Guildford Press, pp 39–72
Barkley R, Karlsson J, Pollard S, Murphy J (1985) Developmental changes in the mother-child interactions of hyperactive boys: Effects of two dose levels of Ritalin. J Child Psychol Psychiatry 26:705–715
Barkley R, Murphy K (1998) Attention deficit hyperactivity disorder: a Clinical Workbook. Guildford, New York
Bryant F, Smith B (2001) Refining the architecture of aggression: a measurement model for the Buss-Perry Aggression Questionnaire. J Res Personal 35:138–167
Daley D, Sonuga-Barke E, Thompson M (2003) Assessing expressed emotion in mothers of preschool AD/HD children: psychometric properties of a modified speech sample. Brit J Clin Psychol 42:53–67
Eddy J, Dishion T, Stoolmiller M (1998) The analysis of intervention change in children and families: methodological and conceptual issues embedded in intervention studies. J Abnorm Child Psychol 26:53–71
Goldberg D (1982) General health questionnaire manual. Windsor, NFER
Goodman R (1997) The strengths and difficulties questionnaire: a research note. J Child Psychol Psych Allied Disciplin 38:581–586
Hibbs E, Hamburger S, Lenane M, Rapoport J, Kruesi M, Keysor C, Goldstein M (1991) Determinants of expressed emotion in families of disturbed and normal children. J Child Psychol Psychiat 32:757–770
Hirshfeld D, Biederman J, Brody L, Faraone S, Rosenbaum J (1997) Associations between expressed emotion and child behavioural inhibition and psychopathology: a pilot study. J Am Acad Child Adol Psychiat 36:205–212
Hirshfeld D, Biederman J, Faraone S, Rosenbaum J (1997) Expressed emotion toward children with behavioral inhibition: associations with maternal anxiety disorder. J Am Acad Child Adol Psychiat 36:910–917
Hooley J, Hiller J (2000) Personality and expressed emotion. J Abnorm Psychol 109:40–44
Lovejoy M, Graczyk P, O’Hare, Neuman G (2000) Maternal depression and parenting behaviour: a meta-analytic review. Clin Psychol Rev 20:561–592
Magana A, Goldstein M, Karno M, Miklowitz D, Jenkins J, Falloon I (1986) A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatric Res 17:203–212
Murray C, Johnston C (2006) Parenting in mothers with and without attention deficit/hyperactivity disorder. J Abnorm Psychol 115:52–61
Patterson G (1982) Coercive family process. Castalia, Eugene, OR
Pelham W, Lang A, Atkeson B, Murphy D, Gnagy E, Greiner A, Wodde-Hamilton M, Greenslade K (1997) Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. J Abnorm Child Psychol 25:413–424
Peris T, Baker B (2000) Applications of the expressed emotion construct to young children with externalising behavior: stability and prediction over time. J Child Psychol Psychiat 41:457–482
Richters J (1992) Depressed mothers as informants about their children: a critical review of the evidence for distortion. Psycholog Bull 112:485–499
Rothbaum F, Weisz J (1994) Parental caregiving and child externalizing behavior in nonclinical samples: a meta-analysis. Psycholog Bull 116:55–74
Schreiber J, Breier A, Pickar D (1995) Expressed emotion. Trait or state? Brit J Psychiat 166:647–649
Schwartz C, Dorer D, Beardslee W, Lavori P, Keller M (1990) Maternal expressed emotion and parental effective disorder: risk for childhood depressive disorder, substance abuse, or conduct disorder. J Psychiat Res 24:231–250
Stubbe D, Zahner G, Goldstein M, Leckman J (1993) Diagnostic specificity of a brief measure of expressed emotion: A community study of children. J Child Psychol Psychiat 34:139–154
Wamboldt F, O’Connor S, Wamboldt M, Gavin L, Klinnert M (2000) The 5 min speech sample in children with asthma: deconstructing the construct of expressed emotion. J Child Psychol Psychiat 41:887–898
Weisz J, Weiss B (1991) Studying the “referrability” of child clinical problems. J Consult Clin Psychol 59:266–273
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Psychogiou, L., Daley, D.M., Thompson, M.J. et al. Mothers’ expressed emotion toward their school-aged sons. Eur Child Adolesc Psychiatry 16, 458–464 (2007). https://doi.org/10.1007/s00787-007-0619-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-007-0619-y