Abstract
Age-related macular degeneration (AMD) is a retinal degenerative disorder prevalent in the elderly population, which leads to the loss of central vision. The disease progression can be managed, if not prevented, either by blocking neovascularization (“wet” form of AMD) or by preserving retinal pigment epithelium and photoreceptor cells (“dry” form of AMD). Although current therapeutic modalities are moderately successful in delaying the progression and management of the disease, advances over the past years in regenerative medicine using iPSC, embryonic stem cells, advanced materials (including nanomaterials) and organ bio-printing show great prospects in restoring vision and efficient management of either forms of AMD. This review focuses on the molecular mechanism of the disease, model systems (both cellular and animal) used in studying AMD, the list of various regenerative therapies and the current treatments available. The article also highlights on the recent clinical trials using regenerative therapies and management of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Age-related macular degeneration (AMD), an important cause of permanent visual impairment, contributes to 5% of global blindness. AMD is marked by the accretion of lipid/protein depositions known as drusen in the macula of retina, leading to progressive damage in central vision and withering of retinal pigment epithelial (RPE) layer, gradually causing complete loss of sight in advanced stage (Fig. 1) [1]. As conferred through several studies on the physiological and functional changes in RPE during AMD including, mitochondrial DNA damage [2], accumulation of lipofuscin [3] and altered expression of RPE structural proteins [4]; it has been observed that mainly the epithelial monolayer cells are affected with advanced age. The RPE cells show marked significance in sustaining retinal homeostasis majorly through its role as a retinal blood barrier, transporter of metabolic products and ions from subretinal space into the blood, as well as a source of angiogenic growth factors release [5, 6] [e.g., transforming growth factor beta (TGF-β) and vascular endothelial growth factor (VEGF)]. It also delivers nutrients derived from the blood to the photoreceptor cells, conducts the phagocytosis of photoreceptor outer segment [7] and absorbs light. However, RPE’s constant exposure to light makes it highly vulnerable to oxidative stress that may overtime damage the cellular tight junctions eventually disrupting the retinal blood barrier [8].
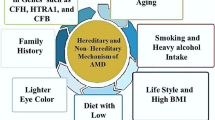
Being an age-related progressive disease, multiple risk factors contribute for the development of AMD, which involves both genetic and environmental factors. Complement pathway genes including complement factor H (CFH), complement C2, C3, CFB, toll-like receptor 3 (TLR3), toll-like receptor 4 (TLR4) and ARMS2/HTRA1 are correlated with AMD [9, 10]. Any dysfunction among the immune components such as CFH and TLR3, that are detected in the drusen can lead to apoptosis of RPE and photoreceptor cells resulting in retinal degeneration [11,12,13]. Environmental and lifestyle susceptible factors including alcohol consumption, smoking, antioxidant intake, hypertension and body mass index (BMI) are also known to induce significant risk on the onset of the disease [14].
An estimated risk of AMD is suspected to reach 288 million by 2040 [15,16,17,18] and the disease prevalence increases from 2% for those aged 50–59 years, to nearly 30% for those over the age of 75 years [19]. Asia Pacific alone accounts for more than one-third of the macular degeneration cases [20]. However, Europeans have a higher prevalence of advanced version of AMD, geographic atrophy, (1.11%) than Africans (0·14%) and Asians (0.21%) [18]. “Dry” AMD (also known as geographic atrophy) is a chronic disorder and is characterized by conflux regions of degenerated RPE cells. In contrast, “Wet” AMD affects only 10–15% of AMD patients, however can rapidly progress into blindness if untreated [21, 22]. Gender is another important factor in AMD prognosis; as in high blood pressure, overweight and obesity are associated with late AMD in women only [23]. Women are potentially at higher risk in developing wet AMD compared to men [24].
Distinctive stages of AMD
AMD is classified into three stages: early, intermediate and late stage. Early stages of the disease show slow progressive painless thinning of the retina (atrophy) caused by an overall loss of neuronal cells due to advanced age and consequently goes unnoticed until later appearing at a severe stage. As the delicate tissue of the retina starts breaking down, the photoreceptor cells (rods and cones) needed for perceiving image also wearies, as a result vision is blurred. Early and intermediate stages of the disease, commonly referred as Dry AMD are distinguished mainly by drusen size (found both internal and external of RPE) [25, 26], changes in the RPE pigments (lipofuscin and melanin) and the degree of loss in vision [27]. Dry AMD shows inflammation and have macrophages and active microglia cells abundant in the atrophic region [28, 29]. It also manifests characteristic degeneration of RPE cells such as loss of melanin and accumulation of lipofuscin pigment, withering of RPE microvilli and disorientation of basal infoldings [30]. Dry AMD is as well associated with photoreceptor cell death, damage of the Bruch’s membrane along with manifestation of few small extracellular “hard” drusen aggregates which are otherwise degraded in healthy adults, is normal with advanced age. Nevertheless, an increase in size and number of such aggregates in the macula, characterized as “soft” drusen with large cluster of undefined edges is the prognosis of an early dry AMD, which can be readily detected by funduscopy. This technique relies on the variations in pigmentation caused due to lipofuscin and lipid–protein accumulations in the retinal fundus as a consequence of drusen inflation [31,32,33]. Late-stage dry atrophic AMD displays blind spot in the visual field, conferring to vision loss. About 65% of the patients with late-stage dry AMD can develop wet AMD, characterized with the appearance of new unusual leaky blood vessels that causes retinal edema, subretinal hemorrhage around the macula, resulting in blurry vision, and consequently interfering with retina’s function leading to vision impairment or blindness [34]. However, early and intermediate stage AMD with leaky chorio-capillaries is not uncommon [35, 36]. Another late-stage form of AMD associated with chronic deficiencies in neuronal photoreceptor, RPE, vascular cells and Bruch’s membrane is called geographic atrophy (GA), which appears in at least 50% of patients with late AMD [37]. GA is characterized by patches of degenerated RPE regions that are even observed to develop in patients with wet AMD; however, they are not mutually exclusive [38]. The recent Age-Related Eye Disease Study (AREDS) on AMD elucidate negligible possibility of the disease manifestation when few small-sized drusen appear in patients. However, if many small drusen to few or many medium-sized drusen appear in one or both the eyes with occasionally one or more large-sized drusen, they can be indicative of early stage to intermediate stage AMD. In the advanced stage of AMD, the central vision is impaired such as blurry or wavy areas due to damaged blood vessels and photoreceptors cells [39, 40] (Fig. 2).
Mechanisms of AMD: initiation and pathogenesis
The advancement of AMD is marked by the degeneration of monolayer RPE, which is incompetent to regeneration, alongside subsequent loss of adhesion junctions and physical separation with neural retina. RPE acting as a blood–retinal barrier tightly regulate the exchange of metabolites between the neural retina and the chorio-capillaries, and its secretion of growth factors including pigment epithelium-derived factor (PEDF) and VEGF is crucial for the protection of photoreceptor cells and angiogenic response, respectively. However, with age, compromised functions in autophagy can lead to increased amyloid deposits in RPE cells resulting in their death and permanent physical separation of photoreceptor cells, consequently interrupting the photo transduction pathways leading to visual impairment [41]. The physical detachment of the photoreceptor cells from RPE layer also causes their subsequent death, inflammation and vascularization further aggravating the disease condition. Detailed molecular mechanisms leading to AMD disease initiation and progression are discussed below.
Drusen formation in AMD
Drusen and constituents
In its earliest stages, AMD is perceived as drusen [42] and their formation may be linked to inflammation (Fig. 3) [43, 44]. This hypothesis stems from the observation that drusen hub several mediators of inflammation (e.g., C-reactive protein, adducts of the carboxyethylpyrrole protein and immunoglobulins) [43, 45,46,47], complement factors (complement factor H) and proteins (C3, C5, C6, C7, C8, C9) [44, 48] in addition to membrane-bound complement inhibitors (complement receptor 1—CR1, i.e., CD35) and (membrane cofactor protein—MCP, i.e., CD46) [49, 50]. Based on immunohistochemical analysis of both hard and soft drusen, a wide range of molecules have been detected that are locally synthesized within the RPE, retina and choroidal cells. These include human leukocyte antigen—DR isotype, apolipoprotein E, amyloid A, vitronectin and complement factors 5 and 9. In addition to such various components, the significant localization of both immunoglobulin and C5b-9 indicates the potential role of immune complex activation in the biogenesis of drusen [38].
Schematic representation of the steps involved during drusen formation and inflammation in AMD RPE cell. The figure depicts the process of lipid–protein aggregates deposition, which can lead to drusen and inflammation. In the process of POS phagocytosis by RPE, the endocytosed material is digested within lysosomes. However, with age, dysregulated lysosomal function and decline in lysosome enzyme activity compromise the digestion process resulting in lipofuscin formation. This event subsequently increases oxidative stress within the cell which consequently induces stress conditions in mitochondria and endoplasmic reticulum, leading to misfolded protein aggregates and dysfunctional autophagy linked to impaired protein clearance in RPE. The disturbed clearance of toxic accumulates in aged RPE cells trigger inflammation and the AMD-associated extracellular drusen formation
Drusen as well accumulate lipofuscin (also known as “age pigment”), advanced glycation end‐products (AGEs), high level of oxidized low‐density lipoproteins and oxysterols which collectively can cause RPE disintegration [51,52,53]. In addition to lipid molecules (e.g., phospholipids and glycolipids), cholesterol and carbohydrates, drusen also harbor various proteins in significant amounts which include apolipoproteins, vitronectin, clusterin, ubiquitin, fibronectin, integrins, to name among many others [52, 54]. Over time, drusen may push through the RPE cells and disrupt the photoreceptors, causing blind spots in the central vision. Although these blind/blank spots go unnoticed by naked eyes, can be clinically detected as the drusen enlarge eventually causing distorted image formation in the retina.
Reactive oxygen species (ROS) and inflammation leading to drusen formation
Wear and tear of day-to-day functions including long constant periods of light exposure, normal visual cycle metabolism and phagocytosis of photoreceptor outer segment (POS) by RPE generates oxidative stress and excess reactive oxygen species (ROS) production, leading to increased inflammatory cytokines release that account for the chronic inflammation and drusen development [55]. Augmented ROS production coupled with oxidative stress plays a pivotal role in AMD pathogenesis. Given the fact that retina has the highest oxygen consumption due to photoreceptors high metabolic activity [56], the polyunsaturated fatty acids (PUFA) (e.g., phosphatidylcholine)-rich photoreceptors cell membrane are readily oxidized generating peroxides and organic radicals in addition to carboxyethylpyrrole and 4-hydroxy-2-nonenal, which form adducts with proteins and are accumulated in the outer retina and in drusen [57,58,59]. Subsequently, these newly modified lipoproteins are highly active in promoting nonreactive molecules into epitope-like structures that inevitably induce immune recognition and inflammation [60, 61]. In aged RPE, the digestion of oxidized PUFA is disparaged, and as a consequence, it gets deposited in the form of lipofuscin in drusen. Being a chromophore, lipofuscin absorbs high energy photons, which evokes its photooxidation-generating highly reactive N-retinylidene-N-retinylethanolamine (A2E) [62,63,64]. Subsequently, A2E upon blue light excitation generates singlet oxygen and superoxide, which collectively with A2E escalates ROS generation and RPE damage in the retina [65].
Oxidative stress, on the other hand can jeopardize natural function of RPE to transport nutrients and ions across choriocapillaris and photoreceptors, exposing the cells to ionic changes that can activate inflammasomes [7, 66]. Several other cellular functions induce the production of inflammatory factors, including activation of pathogen- and damage-associated molecular patterns via pathogen recognition receptors [e.g. toll-like receptors (TLRs), receptor for advanced glycation end products (RAGEs) and NOD-like receptors (NLRs)] by their corresponding ligands [e.g. TLRs recognize elastin, hyaluronic acid and fibronectin and secreted heat shock proteins (HSPs), NLR’s sense oxygen radicals, ultraviolet B and potassium (K+) efflux and nuclear factor kappa B is activated with RAGE] [66,67,68,69,70,71,72,73,74,75]. Incomplete degradation of phagocytosed POS is linked to the formation of lipofuscin in RPE cells [76], and it is notable that advanced glycation reactions play an important part in the lipofuscin formation [77]. The oxidized lipoproteins bind to RPE cell via CD36 and lectin-like oxidized lipoprotein receptor 1, activating monocytes and macrophages to secrete cytokines (IL-8) and growth factors (TNF-alpha) [78,79,80]. With growing age, the accumulation of lipofuscin on an account of poor lysosome clearance function in RPE reflects the formation of highly reactive adduct known as advanced glycation end products (AGEs) to concentrate within drusen as a product of protein (e.g., apolipoprotein E, amyloid and vitronectin)/lipid modification in the course of aging [81,82,83]. These adducts binds onto the extracellular receptors on RPE [TLRs, RAGEs and AGE receptors (AGERs)], the course of which follows inflammatory signal activation within the RPE and promotes inflammation [84]. While AGEs are endocytosed and removed by macrophages [85], a failure in macrophage recruitment may consequently lead to accelerated retinal tissue damage [84].
Lysosomal and autophagy dysfunction
Besides oxidative stress induced by lipofuscin sensitization of RPE cells to visible light, environmental strain and POS phagocytosis can also promote aberrant increase in ROS production which may lead to mitochondrial dysfunction (Fig. 4). As a consequence of lipofuscin-containing vitamin A‐derived fluorophores, it inhibits mitochondrial respiration leading to its dysfunction, hereby promoting protein misfolding [86,87,88] and generating metabolic deficiency within RPE [87, 89, 90]. Different cellular processes, including HSPs/molecular chaperones, ubiquitination/proteasomal degradation and autophagy, are involved in clearing the damaged protein overload [91], which ensures cell’s survival during oxidative stress condition [92].
Schematic representation of RPE senescence in AMD. Constant exposure of RPE to light induces increased oxidative stress and lipofuscin photooxidation. This renders detrimental effects on RPE such as A2E production which causes DNA damage. Mitochondrial damage increases due to decrease in autophagy. Impaired lysosome function results in protein misfolding and age compromised activity of chaperons (HSP) and proteasome damage the protein repairing process which in addition to dysfunctional autophagy forms protein aggregates. Protein aggregates are exocytose as drusen, and NLRP3 inflammasome is activated
In aged RPE cells, the capacity to neutralize ROS weakens due to reduced antioxidant production, poor ability to repair DNA or protein damage and disturbed proteolysis [93, 94]. As a consequence of detrimental concentration of ROS deposition, the cellular proteins are damaged leading to harmful protein aggregation. Lipofuscin is one consequence of this protein aggregates conjugated with lipids since oxidized PUFAs from the POS are not efficiently digested in lysosomes of aged RPE cells [95,96,97,98], which consequently induce oxidative stress, ultimately evoking further protein misfolding. Although HSP are available to combat such stress response generated in the cell [92], eventually its capacity also wearies, wherein autophagy fortifies its role in protein degradation [99].
Autophagy, being a lysosome-mediated natural cellular process for clearing damaged cellular substrates, is in particular activated during cellular stress conditions (e.g., oxidative stress, unfolded protein response or inflammation) [100, 101]. The crucial step in autophagic clearance is the fusion of autophagosome with lysosome, a process which is regulated by proteins Rab7, LAMP-2A and soluble N-ethyl-maleimide-sensitive factor attachment protein receptors [102]. Such proteins increase the permeability of lysosome membrane and upregulate the membrane-pore openings, promoting the fusion of the two organelles content [103]; thereafter the lysosome proteases (e.g., cathepsins D, B and L) degrade the enclosed cargo proteins [104, 105]. However, during oxidative stress, the enzyme activity of the proteases is decelerated by oxidized lipoproteins [106]. Subsequently, the lysosome function is impaired, which eventually results in decreased autophagy flux and may lead to RPE cell degeneration and AMD development [107]. Degraded autophagy function can also ensue from lipofuscin accumulates that incline to suppress lysosomal functions resulting into impaired autophagy [92]. Lipofuscin deposits once formed are hard to degrade, and upon photooxidation produces A2E [92, 108]. A2E, a photosensitive generator of oxygen free radicals and superoxide can impose toxic effect on RPE cell functions causing increase in DNA damage and inhibiting proteolysis [64, 109]. Additionally, impaired lysosomal function can stem from the event when chronic A2E accumulates tend to inhibit (vacuolar) V-ATPase (a proton-pump), thereby elevating lysosomal pH. As lysosomal enzymes (e.g., acid hydrolases and proteases) are highly sensitive to pH change, thereby any aberration can lead to its dysfunction causing impaired digestion of phagocytosed POS [96, 97, 110, 111].
Studies conducted showed that normal RPE rapidly induced autophagy after starvation in the absence of insulin growth factor (IGF)-1, whereas AMD RPE failed to increase the autophagic flux, ratio of LC3-II/LC3-I (microtubule-associated protein 1 light chain LC3-I, after lipidation becomes LC3-II), under the same conditions [112], [113], wherein the conversion of LC3-I to the autophagic vesicle-associated form LC3-II is the determinant factor of autophagy flux [114]. The addition of IGF-1, expected to suppress autophagy through activation of the AKT/mTOR signaling in normal cells, did not seem to decrease the ratio of LC3-II/LC3-I in AMD RPE [112]. In spite of accumulation of autophagosomes in AMD RPE, the ratio of LC3-II/LC3-I under starvation revealed reduced autophagy [112]. These observations collectively fortify that autophagy is rendered dysfunctional during AMD.
Retinal and photoreceptor cell death
The inception of photoreceptor cell (PC) breakdown is marked by deposits of cellular debris in the form of lipofuscin/drusen underlying the retinal epithelial layer. This results in gradual and permanent retinal detachment cutting off PC’s nutrient supply from the RPE cells and the choroid vessels (choriocapillaris), as so compromising their renewal essential for maintaining vision. The constant shedding of the POS, accompanied by their phagocytosis in the RPE cells is crucial to PCs survival. This phenomenon occurs naturally due to retina’s long exposure to visual light stimulus which promotes POS phagocytosis, followed by its lysosomal digestion that consequently induce the formation of superoxide radicals (ROS production) in RPE. Conversely, abnormalities can be seen in various diseases, ranging from early-onset retinal dystrophies, such as retinitis pigmentosa or Usher’s syndrome to age-related diseases affecting the central retina, such as AMD [115]. Subsequently, POS phagocytosis generates oxidative stress and these cellular phenomena are crucially interrelated to lipofuscin formation. The toxic A2E component of lipofuscin [116, 117] inhibits RPE’s phagocytic functions, finally leading to RPE cell death [118,119,120]. Elevated oxidative stress in addition to advanced age is ultimate because that can compromise normal functioning of cellular proteins such as ubiquitin. Ergo, ubiquitinated proteins in RPE do not undergo degradation and resultantly accumulates as aggregates in subretinal space which consequently leads to RPE degeneration [118, 120, 121]. The incompetency of RPE cells lysosomes to completely degrade the digested POS is a critical consequence of advanced age, which encourages the accumulation of nondegradable lipofuscin (vitamin A metabolites) within the lysosomes that can potentially cause RPE damage associated with inflammation [43]. Once damaged, the RPE can secrete growth factors like VEGF, basic fibroblast growth factor (bFGF) and TGF-β that are crucial for neovascularization in AMD [122]. To combat the effect, an endogenous anti-angiogenic growth factor known as PEDF has been studied as a potential inhibitor of VEGF [123]. However, in AMD patients, the PEDF levels in the vitreous have been reported to decrease vividly [124].
Ultrastructural pathology studies have suggested cell death in AMD is predominantly through necroptosis and pyroptosis, while apoptosis may have a minor contribution [125]. Necroptosis is reportedly predominant in RPE cell death associated with dry AMD [126], whereas pyroptosis occurs after the NLRP3 (NLR-with pyrin domains) inflammasome priming by IL-1α or C5a that activates inflammasome and alters the death mode induced by photooxidation from apoptosis to pyroptosis [127], 128. Hanus et al. [129] have reported necrosis in ARPE-19 cells when treated with H2O2/tert‐butyl hydroperoxide in order to induce oxidative stress; the cells subsequently featured characteristics of necrosis such as depletion in ATP and receptor-interacting protein (RIP3) aggregation. An interaction between apoptosis and pyroptosis was studied using ARPE-19 cell line and primary human RPE cells loaded with lipofuscin, irradiated with blue light [130]. The irradiated lipofuscin-mediated oxidative stress resulted in damage to the lysosomal membrane leaking lysosomal enzymes into the cytosol and eventually causing cell death by apoptosis. Tso et al. in 1996, first demonstrated that apoptosis is active in dry AMD [131, 132]. Further Dunaief et al. [133] described an increase in apoptosis in the inner choroid, RPE, photoreceptors and inner nuclear layer with RPE atrophy.
Cellular and animal model systems to study cell death mechanism
Retinal detachment triggers apoptosis of photoreceptor cells was observed among rat models with an increase in caspase-3, 7, 8, 9 activities [134, 135]. Along with intrinsic mechanism of apoptosis, elevated expression of TNF-α, Fas-L and Fas, that regulate apoptosis’s extrinsic pathway [136, 137] were also reported, indicating caspases might not be the sole mediators of cell death post-retinal detachment [138, 139]. The mitochondria–nuclear translocation of apoptosis-inducing factor (AIF) was observed after retinal detachment (RD) in experimental rats [138], mice as well as in human retina [140], providing strong evidence of AIF contribution to RD-associated photoreceptor apoptosis. Poly (ADP-ribose) polymerase (PARP) is regarded as an important factor in the regulation of cellular death in AMD. High concentrations of hydrogen peroxide-induced necrotic cell death, mediated by the activation of PARP1 in human RPE cells in culture, while nicotinamide adenine dinucleotide (NAD+) protected the cells against this effect [141]. Injection of Fas receptor inhibitor, Fas receptor-neutralizing antibody, small inhibitory RNA against the Fas receptor, all have shown to decrease the rate of apoptosis of photoreceptors after retinal detachment [133, 135]. When caspases are inhibited by benzyloxycarbonyl-Val-Ala-Asp (OMe) fluoromethylketone (Z-VAD-fmk), necrosis is induced by RIP kinases, which then regulates photoreceptor cell death post RD, where RIP1 and RIP3 act as mediators of necrosis [142]. To further confirm necrosis form of photoreceptor death, it was studied that in human eyes with RD; there was an increased level of box1 protein, a factor released only from necrotic cells but not apoptotic cells [143]. As both necrosis and apoptosis cause photoreceptor cell death after RD, so it could be an effective way to protect photoreceptor degeneration by simultaneously inhibiting caspases and RIP kinase.
Endoplasmic reticulum (ER) stress-induced apoptosis in retinal cell death has been observed during AMD in both cultured RPE cells and in animal model retinas. Expression of a mutant (R14W) of carbonic anhydrase IV, a glycosylphosphatidylinositol-anchored protein, highly expressed in the choriocapillaris of human eye, upregulate Bip (ER chaperone that facilitates protein folding and reduces ER stress), protein kinase R (PKR)-like endoplasmic reticulum kinase (PERK) and CCAAT/enhancer-binding protein homologous protein, a central mediator of ER stress-induced apoptosis (CHOP), markers of ER stress and the unfolded protein response, is accompanied by apoptosis [144]. Overexpression of Bip attenuates CHOP expression, apoptotic cascade activation and restored the retinal photoreceptor function in P23H rats [145]. Similarly, enhanced ER stress was reported in retinitis pigmentosa induced by the rhodopsin mutation P23H in Xenopus laevis [146] and also in rats [147]. In degenerating rd1 mouse retina, translocation of caspase-12 from the inner segments to the nuclei of the photoreceptors was studied with a further study confirming caspase-12 involvement in rd1 cell death and along with other ER stress-related factors such as GRP78/BiP, EIF2a and PERK [148, 149].
Clinical management
In spite of the progressive loss of vision caused by AMD, currently the prospect of preventing or curing macular degeneration is highly limited. Until recently the only available treatment to seal leaking blood vessels associated with wet AMD was with a laser called laser photocoagulation. Currently, clinical interventions for AMD involve intravitreal injection of anti-VEGF drugs such as pegaptanib sodium injection, aflibercept and the United States Food and Drug Administration (FDA) approved ranibizumab. However, these treatments do not target the underlying degeneration inherent in wet AMD, and there is high rate of recurrence when such treatments are discontinued [150]. In case of surgical removal of the choroidal neovascular membrane, vision improvement is often limited due to the previous damage already caused within the RPE, and the procedure might as well risk the amputation of remaining RPE and photoreceptor cells. So far treatment administered for dry AMD encompasses allogeneic transplantation of RPE cells derived from human fetuses, nevertheless this was usually observed to be risked with graft rejection [151, 152]. Transplantation of RPE cell sheet is an uprising technique to treat dry AMD, still it’s invasive and complex surgical procedure that is associated with a high risk of massive hemorrhage and retinal detachment. One of the commonly used treatments for wet AMD is photodynamic therapy (PDT), which is based on the delivery of a photosensitizer to the choroidal neovascularization (CNV) site via a liposomal formulation of verteporfin [153], which in combination with anti-VEGF is known to maintain visual function during CNV [154]. Besides, AREDS studies also assessed the use of vitamins in the progression of AMD treatment [155]. Current AREDS studies suggest that omega-3 fatty acids, antioxidants and zinc might reduce AMD or may even restrict the rate of its progression [156]. The researchers of AREDS investigated a formula of antioxidant vitamins C and E, beta-carotene and zinc (known as the AREDS formula) to be orally administered on AMD patients. However, it was observed to initiate the risk of lung cancer in patients addicted to smoking [157]. To counter the side effects, the formula was later modified in 2006 and renamed as AREDS2 design, that may test the effectiveness of the study by administering omega-3 fatty acids or lutein and/or zeaxanthin [156, 158].
Current treatments
Neuroprotective treatments and gene therapy as can be aided to prevent initial stages of degeneration are however found to be inefficient when comes to treating the later stage of the disease. In cases of severe vision loss, retinal prosthesis devices were approved by FDA although it provides resolution below the level of functional vision and use external sensors for light detection [159,160,161,162]. Contrariwise, targeted replacement of photoreceptors can overcome such challenges and similar to RPE replacement, uses both embryonic stem cells (ESC) and induced pluripotent stem cell (iPSC)-derived in vitro cultures in cell replacement therapies [163,164,165,166,167]. The current gold standard in treatment of neovascular AMD has been through the advent of intravenous VEGF inhibitors (e.g., ranibizumab/bevacizumab, aflibercept approved by FDA) [168], though the recovery rate has been estimated to be only 30% in patients [169]. The limitation of this treatment resides for the fact that sustained blocking of VEGF, an essential factor for cell survival, can accentuate to chorio-retinal atrophy.
Regenerative therapy
Photoreceptor replacement
During cellular degeneration, it is much easier to replace RPE cells than photoreceptors as the latter clump rather than forming a single layer. Photoreceptors, however, after being transplanted into the retina must connect with the retinal neurons and form synapses in order to conduct their signals. Though this normally occurs in the developing retina, it is much harder to accomplish in an adult retina. Inspired by the early trials of RPE replacement, photoreceptor replacement was initially attempted using full-thickness retinal sheets or patches [170,171,172]. Later on, direct subretinal transplantation was attempted using undifferentiated retinal progenitor cells, photoreceptor precursors and forebrain-derived neuronal progenitors, which were expected to differentiate into photoreceptors due to the subretinal space microenvironment [173,174,175,176,177,178]. Various methods are tested for rod photoreceptor cells generation from pluripotent stem cell sources, though it appears to be more challenging to consistently generate high numbers of cone photoreceptors from stem cells in vitro [179,180,181,182,183,184]. However, encouraging data are emerging on methods to increase the fraction of cone photoreceptor cells generated in culture and transplantation [185,186,187,188,189].
RPE transplantation as a therapeutic model
Recently, gene therapy was proven efficient in restoring RPE function [190, 191], yet RPE replacement remains a viable strategy for retinal degenerative diseases. Stem cells are used to replace the damaged RPE cells specifically in atrophy AMD by transplanting ESCs- or iPSC-derived products into the macula, paracentral retina or vitreous cavity so as to restore vision. Subretinal transplantation of human embryonic stem cell (hESC)-derived RPE cells has been reported [180, 192,193,194]. Similarly, autologous iPSC-derived RPE cells were safely transplanted into an AMD patient without immunosuppression [195]. The advancement in stem cell research, has escalated the possibility of maintaining retinal neurons in vitro [196], followed by the de novo differentiation of retinal neurons from either ESC or iPSC lines [197, 198]. Major strategies for cell transplantation are injection of a suspension of cells (less invasive) and surgical implantation of an RPE monolayer, with or without a supporting membrane. Studies by Carr et al. [185] demonstrated that injection of RPE cells in rat models tend to form clusters and show limited phagocytosis of photoreceptor outer segments. An experiment comparing injection and implantation of hESC-RPE revealed that implanted monolayers survived longer (for at least 12 months) without evidence of tumor formation in immunocompromised rats [199]. A scaffold-free layer of iPSC-RPE, designed for clinical use showed no immune rejection or tumor formation when implanted in a primate model [200]. Furthermore, human clinical trials using suspension injections of hESC-RPE had no uncalled safety issues related to the injected cells [201]. Based on this research, first individual with AMD to ever receive a transplanted layer of autologous iPSC-RPE cells was reported [202].
Biomaterials
The use of purified extracellular matrix proteins (such as collagen IV and laminin) differentially influences hESC-RPE growth, pigmentation, barrier function and also improves the production of differentiated iPSC-RPE cells [203]. Bioengineered polymers used as matrices promote the formation of a single layer of polarized RPE cells with specialized apical and basal features, the disruption of the same that is implicated in retinal diseases [204]. Synthetic Bruch’s membranes were constructed from fibroin, supported the co-cultivation of RPE cells and microvascular endothelial cells [205]. Biodegradable and biocompatible biomaterials working as curative matrices either individually or along with the cell transplants or drug-loaded matrices, are widely explored. The commonly used polymers are polylactide, polylactide-co-glycolide and acrylic polymers, which can be degraded in vivo to form natural metabolites. Porous poly(ε-caprolactone) (PCL) is biocompatible, helps metabolite transport and improve human fetal retinal pigment epithelium cell function compared with non-porous PCL or porous polyester [206]. Other polymers engineered for RPE transplantation, include parylene [207]. Parylene, a xylene-based hydrocarbon polymer approved for biomedical use and can be engineered with ultrathin regions such that it has permeability similar to Bruch’s membrane [208]. hESC-RPE cultured on these ultrathin parylene-C membranes are able to adhere, proliferate, develop polarized monolayers and maintain RPE characteristics [208]. Advanced surgical techniques were developed to implant the parylene substrates into a rat model of AMD, where more than 98% of the transplanted RPE cells survived the procedure [209]. Future RPE implants might include biocompatible scaffolds that mimic a healthy Bruch’s membrane [210].
Nano-therapeutics
Nanoparticles (NPs) may be used to deliver drugs for easier (topical) and sustained delivery, reducing the frequency of intravitreal injections. NPs loaded with ganciclovir administered into the vitreous, showed prolonged presence of the drug in the eye with least toxicity manifestation [211]. Inorganic NPs are observed to have anti-angiogenic properties as reported by Kim et al. [212] and Jo et al. [213] in their studies using gold and silicate nanoparticles, respectively, which could be considered as a viable treatment for neovascularization. The use of yttrium oxide nanoparticles (Y2O3) as free radical scavengers has been reported to prevent photoreceptor cell death and an alternative treatment for oxidative stress associated retinal degeneration [214, 215]. Therapeutic genes may also be delivered to RPE and photoreceptor cells by NPs. For example, studies reported using murine model of retinitis pigmentosa photoreceptor cells that were treated with CK30PEG10k-compacted DNA nanoparticles, which led to transgene expression in RPE [216]. Also, liposome–protamine–DNA complex was used as delivery system for RPE65 gene in knock-out mice, which efficiently expressed RPE65 gene for a long time [217].
Indeed, NPs were shown to be taken up by RPE cells both in vitro and in vivo [218,219,220,221]. Recent studies using NPs as a delivery system for marker gene encoding green fluorescent protein (GFP) into the subretinal space or vitreous of adult mice showed significant levels of GFP expression in photoreceptors and RPE cells [222, 223]. Interestingly, nanoparticles, in advantage to their small size (< 100 nm), when injected in the vitreous can migrate through the retinal layers and tend to accumulate in the RPE cells [219, 220]. For instance, nanoparticles (1–1000 nm, generally 20–300 nm) of liposomes can be developed for sustained release of intraocular drug [224]. Sakurai et al. [225] reported that the size of nanoparticles is correlated with the efficiency of drug delivery in vitreous humor through the study using intravitreous injection of three sizes of nanoparticles (50 nm, 200 nm and 2 µm) in rabbit eyes. VEGF antisense oligonucleotides impregnated with NPs were successfully delivered to ARPE-19 cells and inhibit VEGF secretion and mRNA expression [218]. Also, studies with bFGF-loaded NPs showed significant protection against photoreceptor degeneration in RCS rats due to sustained release of bFGF following intravitreal injection [226]. Nanotechnology-based PDT has been recently tested in laser-induced CNV animal models. The use of a dendritic photosensitizer (dendrimer porphyrin encapsulated by a polymeric micelle) led to a highly selective accumulation of photosensitizer in the CNV lesions, and significantly enhance the efficacy of PDT [227]. These data provide a novel paradigm for the treatment of AMD through dendrimer-based nanomedicine. Hence, the intracellular delivery of molecules by NPs to RPE or photoreceptor cells may open a wide range of therapeutic avenues for AMD.
Conclusion
Regenerative therapies though have addressed the different forms of AMD pathogenesis, there is currently no treatment approved that may completely cure the disease. However, several ongoing trials are aiming to find way to at least cease the progression of early AMD into an even serious stage. Several challenges need to be tackled in order to restore the damaged epithelial cells, neural layers and avert atrophy manifestation. Nevertheless, the progress in clinical translational research in replacement of RPE using stem cells is currently in progress, but the overall advancement in using in vitro models for retina neural cell replacement is still not promising. Although positivity is seen with in vivo models in understanding the effectiveness and safety of new therapies for AMD, the next leap toward clinical translation must be carefully approached and with treatments made available to the patients at financially reasonable level.
References
Birch DG, Liang FQ (2007) Age-related macular degeneration: a target for nanotechnology derived medicines. Int J Nanomed 2(1):65–77
Lin H, Xu H, Liang FQ, Liang H, Gupta P et al (2011) Mitochondrial DNA damage and repair in rpe associated with aging and age-related macular degeneration. Invest Ophthalmol Vis Sci 52(6):3521–3529
Schmitz-Valckenberg S, Fleckenstein M, Scholl HP, Holz FG (2009) Fundus autofluorescence and progression of age-related macular degeneration. Surv Ophthalmol 54(1):96–117
Gu X, Neric NJ, Crabb JS, Crabb JW, Bhattacharya SK et al (2012) Age-related changes in the retinal pigment epithelium (RPE). PLoS ONE 7(6):e38673
Dornonville de la Cour M (1993) Ion transport in the retinal pigment epithelium. A study with double barrelled ion-selective microelectrodes. Acta Ophthalmol Suppl 209:1–32
Hamann S (2002) Molecular mechanisms of water transport in the eye. Int Rev Cytol 215:395–431
Strauss O (2005) The retinal pigment epithelium in visual function. Physiol Rev 85(3):845–881
Negi A, Marmor MF (1984) Experimental serous retinal detachment and focal pigment epithelial damage. Arch Ophthalmol 102(3):445–449
Klein RJ, Zeiss C, Chew EY, Tsai JY, Sackler RS et al (2005) Complement factor H polymorphism in age-related macular degeneration. Science 308(5720):385–389
Yang Z, Stratton C, Francis PJ, Kleinman ME, Tan PL et al (2008) Toll-like receptor 3 and geographic atrophy in age-related macular degeneration. N Engl J Med 359(14):1456–1463
Collard CD, Vakeva A, Morrissey MA, Agah A, Rollins SA et al (2000) Complement activation after oxidative stress: role of the lectin complement pathway. Am J Pathol 156(5):1549–1556
Gao ML, Wu KC, Deng WL, Lei XL, Xiang L et al (2017) Toll-like receptor 3 activation initiates photoreceptor cell death in vivo and in vitro. Invest Ophthalmol Vis Sci 58(2):801–811
Murakami Y, Matsumoto H, Roh M, Giani A, Kataoka K et al (2014) Programmed necrosis, not apoptosis, is a key mediator of cell loss and damp-mediated inflammation in dsrna-induced retinal degeneration. Cell Death Differ 21(2):270–277
de Jong PT (2006) Age-related macular degeneration. N Engl J Med 355(14):1474–1485
Group* TEDPR (2004) Prevalence of open-angle glaucoma among adults in the united states. JAMA Ophthalmol 122(4):532–538
Pascolini D, Mariotti SP (2012) Global estimates of visual impairment: 2010. Br J Ophthalmol 96(5):614–618
Friedman DS, Wolfs RC, O’Colmain BJ, Klein BE, Taylor HR et al (2004) Prevalence of open-angle glaucoma among adults in the united states. Arch Ophthalmol 122(4):532–538
Wong WL, Su X, Li X, Cheung CM, Klein R et al (2014) Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2(2):e106-116
Klein R, Klein BE (2013) The prevalence of age-related eye diseases and visual impairment in aging: current estimates. Invest Ophthalmol Vis Sci 54(14):Orsf5–Orsf13
Thapa R, Bajimaya S, Paudyal G, Khanal S, Tan S, Thapa SS, van Rens G (2017) Prevalence of and risk factors for age-related macular degeneration in Nepal: the Bhaktapur Retina Study. Clin Ophthalmol 11:963–972
Guyer DR, Fine SL, Maguire MG, Hawkins BS, Owens SL et al (1986) Subfoveal choroidal neovascular membranes in age-related macular degeneration. Visual prognosis in eyes with relatively good initial visual acuity. Arch Ophthalmol 104(5):702–705
Wong TY, Chakravarthy U, Klein R, Mitchell P, Zlateva G et al (2008) The natural history and prognosis of neovascular age-related macular degeneration: a systematic review of the literature and meta-analysis. Ophthalmology 115(1):116–126
Erke MG, Bertelsen G, Peto T, Sjølie AK, Lindekleiv H, Njølstad I (2014) Cardiovascular risk factors associated with age-related macular degeneration: the tromsø study. Acta Ophthalmol 92(7):662–669
Rudnicka AR, Jarrar Z, Wormald R, Cook DG, Fletcher A, Owen CG (2012) Age and gender variations in age-related macular degeneration prevalence in populations of European ancestry: a meta-analysis. Ophthalmology 119(3):571–580
Klein R, Meuer SM, Knudtson MD, Iyengar SK, Klein BE (2008) The epidemiology of retinal reticular drusen. Am J Ophthalmol 145(2):317–326
Klein ML, Ferris FL, 3rd, Francis PJ, Lindblad AS, Chew EY et al (2010) Progression of geographic atrophy and genotype in age-related macular degeneration. Ophthalmology 117(8):1554–1559, 1559.e1551
Schlanitz FG, Baumann B, Kundi M, Sacu S, Baratsits M et al (2017) Drusen volume development over time and its relevance to the course of age-related macular degeneration. Br J Ophthalmol 101(2):198–203
Al Gwairi O, Thach L, Zheng W, Osman N, Little PJ (2016) Cellular and molecular pathology of age-related macular degeneration: potential role for proteoglycans. J Ophthalmol 2016:2913612
van Lookeren CM, LeCouter J, Yaspan BL, Ye W (2014) Mechanisms of age-related macular degeneration and therapeutic opportunities. J Pathol 232(2):151–164
Boulton M, Dayhaw-Barker P (2001) The role of the retinal pigment epithelium: topographical variation and ageing changes. Eye (Lond) 15(Pt 3):384–389
Köse C, Sevik U, Gençalioğlu O (2008) Automatic segmentation of age-related macular degeneration in retinal fundus images. Comput Biol Med 38(5):611–619
van Grinsven MJ, Lechanteur YT, van de Ven JP, van Ginneken B, Hoyng CB et al (2013) Automatic drusen quantification and risk assessment of age-related macular degeneration on color fundus images. Invest Ophthalmol Vis Sci 54(4):3019–3027
Bartlett H, Eperjesi F (2007) Use of fundus imaging in quantification of age-related macular change. Surv Ophthalmol 52(6):655–671
Mettu PS, Wielgus AR, Ong SS, Cousins SW (2012) Retinal pigment epithelium response to oxidant injury in the pathogenesis of early age-related macular degeneration. Mol Asp Med 33(4):376–398
Seddon JM, McLeod DS, Bhutto IA, Villalonga MB, Silver RE et al (2016) Histopathological insights into choroidal vascular loss in clinically documented cases of age-related macular degeneration. JAMA Ophthalmol 134(11):1272–1280
Borrelli E, Sarraf D, Freund KB, Sadda SR (2018) Oct angiography and evaluation of the choroid and choroidal vascular disorders. Prog Retinal Eye Res 67:30–55
Cherepanoff S, McMenamin P, Gillies MC, Kettle E, Sarks SH (2010) Bruch’s membrane and choroidal macrophages in early and advanced age-related macular degeneration. Br J Ophthalmol 94(7):918–925
Ashraf M, Souka AAR (2017) Aflibercept in age-related macular degeneration: evaluating its role as a primary therapeutic option. Eye (Lond) 31(11):1523–1536
Friberg TR, Bilonick RA, Brennen P (2012) Is drusen area really so important? An assessment of risk of conversion to neovascular amd based on computerized measurements of drusen. Invest Ophthalmol Vis Sci 53(4):1742–1751
Vitale S, Agrón E, Clemons TE, Keenan TDL, Domalpally A et al (2020) Association of 2-year progression along the AREDS AMD scale and development of late age-related macular degeneration or loss of visual acuity: AREDS report 41. JAMA Ophthalmol 138(6):610–617
Ambati J, Atkinson JP, Gelfand BD (2013) Immunology of age-related macular degeneration. Nat Rev Immunol 13(6):438–451
De Jong PTVM (2018) Elusive drusen and changing terminology of amd. Eye 32(5):904–914
Anderson DH, Mullins RF, Hageman GS, Johnson LV (2002) A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol 134(3):411–431
Hageman GS, Luthert PJ, Victor Chong NH, Johnson LV, Anderson DH et al (2001) An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-bruch’s membrane interface in aging and age-related macular degeneration. Prog Retinal Eye Res 20(6):705–732
Mullins RF, Russell SR, Anderson DH, Hageman GS (2000) Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease. FASEB J 14(7):835–846
Gu X, Meer SG, Miyagi M, Rayborn ME, Hollyfield JG et al (2003) Carboxyethylpyrrole protein adducts and autoantibodies, biomarkers for age-related macular degeneration. J Biol Chem 278(43):42027–42035
Mullins RF, Aptsiauri N, Hageman GS (2001) Structure and composition of drusen associated with glomerulonephritis: implications for the role of complement activation in drusen biogenesis. Eye (Lond) 15(Pt 3):390–395
Anderson DH, Radeke MJ, Gallo NB, Chapin EA, Johnson PT et al (2010) The pivotal role of the complement system in aging and age-related macular degeneration: hypothesis re-visited. Prog Retinal Eye Res 29(2):95–112
Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ et al (2005) A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA 102(20):7227–7232
Johnson LV, Leitner WP, Staples MK, Anderson DH (2001) Complement activation and inflammatory processes in drusen formation and age related macular degeneration. Exp Eye Res 73(6):887–896
Ishibashi T, Murata T, Hangai M, Nagai R, Horiuchi S et al (1998) Advanced glycation end products in age-related macular degeneration. Arch Ophthalmol 116(12):1629–1632
Crabb JW, Miyagi M, Gu X, Shadrach K, West KA et al (2002) Drusen proteome analysis: an approach to the etiology of age-related macular degeneration. Proc Natl Acad Sci USA 99(23):14682–14687
Javitt NB, Javitt JC (2009) The retinal oxysterol pathway: a unifying hypothesis for the cause of age-related macular degeneration. Curr Opin Ophthalmol 20(3):151–157
Mullins RF, Johnson LV, Anderson DH, Hageman GS (1997) Characterization of drusen-associated glycoconjugates. Ophthalmology 104(2):288–294
Kaarniranta K, Salminen A (2009) Age-related macular degeneration: activation of innate immunity system via pattern recognition receptors. J Mol Med (Berl) 87(2):117–123
Yu DY, Cringle SJ (2001) Oxygen distribution and consumption within the retina in vascularised and avascular retinas and in animal models of retinal disease. Prog Retinal Eye Res 20(2):175–208
Tokarz P, Kaarniranta K, Blasiak J (2013) Role of antioxidant enzymes and small molecular weight antioxidants in the pathogenesis of age-related macular degeneration (AMD). Biogerontology 14(5):461–482
Arstila AU, Smith MA, Trump BF (1972) Microsomal lipid peroxidation: morphological characterization. Science 175(4021):530–533
De La Paz MA, Anderson RE (1992) Lipid peroxidation in rod outer segments. Role of hydroxyl radical and lipid hydroperoxides. Invest Ophthalmol Vis Sci 33(7):2091–2096
Shaw PX, Zhang L, Zhang M, Du H, Zhao L et al (2012) Complement factor H genotypes impact risk of age-related macular degeneration by interaction with oxidized phospholipids. Proc Natl Acad Sci 109(34):13757–13762
Shaw PX, Hörkkö S, Chang M-K, Curtiss LK, Palinski W et al (2000) Natural antibodies with the T15 idiotype may act in atherosclerosis, apoptotic clearance, and protective immunity. J Clin Investig 105(12):1731–1740
Sparrow JR, Boulton M (2005) RPE lipofuscin and its role in retinal pathobiology. Exp Eye Res 80(5):595–606
Wu Y, Yanase E, Feng X, Siegel MM, Sparrow JR (2010) Structural characterization of bisretinoid A2E photocleavage products and implications for age-related macular degeneration. Proc Natl Acad Sci USA 107(16):7275–7280
Sparrow JR, Nakanishi K, Parish CA (2000) The lipofuscin fluorophore A2E mediates blue light-induced damage to retinal pigmented epithelial cells. Invest Ophthalmol Vis Sci 41(7):1981–1989
Sparrow JR, Vollmer-Snarr HR, Zhou J, Jang YP, Jockusch S et al (2003) A2E-epoxides damage DNA in retinal pigment epithelial cells. Vitamin E and other antioxidants inhibit A2E-epoxide formation. J Biol Chem 278(20):18207–18213
Pétrilli V, Dostert C, Muruve DA, Tschopp J (2007) The inflammasome: a danger sensing complex triggering innate immunity. Curr Opin Immunol 19(6):615–622
Masters SL, De Nardo D (2014) Innate immunity. Curr Opin Immunol 26:v–vi
Kawai T, Akira S (2010) The role of pattern-recognition receptors in innate immunity: update on toll-like receptors. Nat Immunol 11(5):373–384
Kumar H, Kawai T, Akira S (2011) Pathogen recognition by the innate immune system. Int Rev Immunol 30:16–34
Bianchi ME (2007) Damps, pamps and alarmins: all we need to know about danger. J Leukoc Biol 81(1):1–5
Miyake K (2007) Innate immune sensing of pathogens and danger signals by cell surface toll-like receptors. Semin Immunol 19(1):3–10
Yamada Y, Ishibashi K, Ishibashi K, Bhutto IA, Tian J et al (2006) The expression of advanced glycation endproduct receptors in RPE cells associated with basal deposits in human maculas. Exp Eye Res 82(5):840–848
Howes KA, Liu Y, Dunaief JL, Milam A, Frederick JM et al (2004) Receptor for advanced glycation end products and age-related macular degeneration. Invest Ophthalmol Vis Sci 45(10):3713–3720
Holtkamp GM, Kijlstra A, Peek R, de Vos AF (2001) Retinal pigment epithelium-immune system interactions: cytokine production and cytokine-induced changes. Prog Retinal Eye Res 20(1):29–48
Yang D, Elner SG, Bian ZM, Till GO, Petty HR et al (2007) Pro-inflammatory cytokines increase reactive oxygen species through mitochondria and NADPH oxidase in cultured RPE cells. Exp Eye Res 85(4):462–472
Boulton M, McKechnie NM, Breda J et al (1989) The formation of autofluorescent granules in cultured human RPE. Invest Ophthalmol Vis Sci 30:82–89
Yin D (1996) Biochemical basis of lipofuscin, ceroid, and age pigment-like fluorophores. Free Radic Biol Med 21(6):871–888
Vohra RS, Murphy JE, Walker JH, Ponnambalam S, Homer-Vanniasinkam S (2006) Atherosclerosis and the lectin-like oxidized low-density lipoprotein scavenger receptor. Trends Cardiovasc Med 16(2):60–64
Duncan KG, Bailey KR, Kane JP, Schwartz DM (2002) Human retinal pigment epithelial cells express scavenger receptors BI and BII. Biochem Biophys Res Commun 292(4):1017–1022
Xu H, Chen M, Manivannan A, Lois N, Forrester JV (2008) Age-dependent accumulation of lipofuscin in perivascular and subretinal microglia in experimental mice. Aging Cell 7(1):58–68
Li YM, Dickson DW (1997) Enhanced binding of advanced glycation endproducts (AGE) by the ApoE4 isoform links the mechanism of plaque deposition in Alzheimer’s disease. Neurosci Lett 226(3):155–158
Tabaton M, Perry G, Smith M, Vitek M, Angelini G et al (1997) Is amyloid beta-protein glycated in Alzheimer’s disease? NeuroReport 8(4):907–909
Hammes HP, Weiss A, Hess S, Araki N, Horiuchi S et al (1996) Modification of vitronectin by advanced glycation alters functional properties in vitro and in the diabetic retina. Lab Invest 75(3):325–338
Lin T, Walker GB, Kurji K, Fang E, Law G et al (2013) Parainflammation associated with advanced glycation endproduct stimulation of RPE in vitro: implications for age-related degenerative diseases of the eye. Cytokine 62(3):369–381
Ohgami N, Nagai R, Ikemoto M, Arai H, Kuniyasu A et al (2001) Cd36, a member of the class b scavenger receptor family, as a receptor for advanced glycation end products. J Biol Chem 276(5):3195–3202
Sparrow JR, Cai B, Fishkin N, Jang YP, Krane S et al (2003) A2E, a fluorophore of RPE lipofuscin: can it cause rpe degeneration? Adv Exp Med Biol 533:205–211
Terman A, Brunk UT (2004) Lipofuscin. Int J Biochem Cell Biol 36(8):1400–1404
Nordgaard CL, Karunadharma PP, Feng X, Olsen TW, Ferrington DA (2008) Mitochondrial proteomics of the retinal pigment epithelium at progressive stages of age-related macular degeneration. Invest Ophthalmol Vis Sci 49(7):2848–2855
Algvere PV, Seregard S (2002) Age-related maculopathy: pathogenetic features and new treatment modalities. Acta Ophthalmol Scand 80(2):136–143
Algvere PV, Marshall J, Seregard S (2006) Age-related maculopathy and the impact of blue light hazard. Acta Ophthalmol Scand 84(1):4–15
Ferrington DA, Sinha D, Kaarniranta K (2016) Defects in retinal pigment epithelial cell proteolysis and the pathology associated with age-related macular degeneration. Prog Retinal Eye Res 51:69–89
Ryhänen T, Hyttinen JM, Kopitz J, Rilla K, Kuusisto E et al (2009) Crosstalk between Hsp70 molecular chaperone, lysosomes and proteasomes in autophagy-mediated proteolysis in human retinal pigment epithelial cells. J Cell Mol Med 13(9b):3616–3631
Kaarniranta K, Salminen A, Eskelinen EL, Kopitz J (2009) Heat shock proteins as gatekeepers of proteolytic pathways-implications for age-related macular degeneration (AMD). Ageing Res Rev 8(2):128–139
Blasiak J, Glowacki S, Kauppinen A, Kaarniranta K (2013) Mitochondrial and nuclear DNA damage and repair in age-related macular degeneration. Int J Mol Sci 14(2):2996–3010
Schütt F, Bergmann M, Holz FG, Kopitz J (2002) Isolation of intact lysosomes from human RPE cells and effects of A2-E on the integrity of the lysosomal and other cellular membranes. Graefes Arch Clin Exp Ophthalmol 240(12):983–988
Bergmann M, Schütt F, Holz FG, Kopitz J (2004) Inhibition of the ATP-driven proton pump in RPE lysosomes by the major lipofuscin fluorophore A2-E may contribute to the pathogenesis of age-related macular degeneration. FASEB J 18(3):562–564
Vives-Bauza C, Anand M, Shiraz AK, Magrane J, Gao J et al (2008) The age lipid A2E and mitochondrial dysfunction synergistically impair phagocytosis by retinal pigment epithelial cells. J Biol Chem 283(36):24770–24780
Valapala M, Wilson C, Hose S, Bhutto IA, Grebe R et al (2014) Lysosomal-mediated waste clearance in retinal pigment epithelial cells is regulated by CRYBA1/βA3/A1-crystallin via V-ATPase-MTORC1 signaling. Autophagy 10(3):480–496
Hyttinen JM, Amadio M, Viiri J, Pascale A, Salminen A et al (2014) Clearance of misfolded and aggregated proteins by aggrephagy and implications for aggregation diseases. Ageing Res Rev 18:16–28
Levine B, Kroemer G (2008) Autophagy in the pathogenesis of disease. Cell 132(1):27–42
Arjamaa O, Nikinmaa M, Salminen A, Kaarniranta K (2009) Regulatory role of HIF-1α in the pathogenesis of age-related macular degeneration (AMD). Ageing Res Rev 8(4):349–358
Hyttinen JM, Niittykoski M, Salminen A, Kaarniranta K (2013) Maturation of autophagosomes and endosomes: a key role for Rab7. Biochim Biophys Acta 1833(3):503–510
Zucchi PC, Zick M (2011) Membrane fusion catalyzed by a Rab, SNAREs, and SNARE chaperones is accompanied by enhanced permeability to small molecules and by lysis. Mol Biol Cell 22(23):4635–4646
Behrends C, Sowa ME, Gygi SP, Harper JW (2010) Network organization of the human autophagy system. Nature 466(7302):68–76
Cullen V, Lindfors M, Ng J, Paetau A, Swinton E et al (2009) Cathepsin D expression level affects alpha-synuclein processing, aggregation, and toxicity in vivo. Mol Brain 2:5
O’Neil J, Hoppe G, Sayre LM, Hoff HF (1997) Inactivation of cathepsin B by oxidized LDL involves complex formation induced by binding of putative reactive sites exposed at low PH to thiols on the enzyme. Free Radic Biol Med 23(2):215–225
Kaarniranta K, Sinha D, Blasiak J, Kauppinen A, Veréb Z et al (2013) Autophagy and heterophagy dysregulation leads to retinal pigment epithelium dysfunction and development of age-related macular degeneration. Autophagy 9(7):973–984
Krohne TU, Kaemmerer E, Holz FG, Kopitz J (2010) Lipid peroxidation products reduce lysosomal protease activities in human retinal pigment epithelial cells via two different mechanisms of action. Exp Eye Res 90(2):261–266
Perusek L, Sahu B, Parmar T, Maeno H, Arai E, Le YZ, Subauste CS, Chen Y, Palczewski K, Maeda A (2015) Di-retinoid-pyridinium-ethanolamine (A2E) accumulation and the maintenance of the visual cycle are independent of Atg7-mediated autophagy in the retinal pigmented epithelium. Mol Bases Dis Cell Biol 290(48):29035–29044
Finnemann SC, Leung LW, Rodriguez-Boulan E (2002) The lipofuscin component A2E selectively inhibits phagolysosomal degradation of photoreceptor phospholipid by the retinal pigment epithelium. Proc Natl Acad Sci USA 99(6):3842–3847
Lamb LE, Simon JD (2004) A2e: a component of ocular lipofuscin. Photochem Photobiol 79(2):127–136
Golestaneh N, Chu Y, Xiao YY, Stoleru GL, Theos AC (2017) Dysfunctional autophagy in RPE, a contributing factor in age-related macular degeneration. Cell Death Dis 8(1):e2537
Mizushima N, Yoshimori T (2007) How to interpret LC3 immunoblotting. Autophagy 3(6):542–545
Schaaf MB, Keulers TG, Vooijs MA, Rouschop KM (2016) LC3/gabarap family proteins: autophagy-(un)related functions. FASEB J 30(12):3961–3978
Nandrot EF (2014) Animal models, in “the quest to decipher RPE phagocytosis.” Adv Exp Med Biol 801:77–83
Fine SL (2005) Age-related macular degeneration 1969–2004: a 35-year personal perspective. Am J Ophthalmol 139(3):405–420
Kopitz J, Holz FG, Kaemmerer E, Schutt F (2004) Lipids and lipid peroxidation products in the pathogenesis of age-related macular degeneration. Biochimie 86(11):825–831
Kinnunen K, Petrovski G, Moe MC, Berta A, Kaarniranta K (2012) Molecular mechanisms of retinal pigment epithelium damage and development of age-related macular degeneration. Acta Ophthalmol 90(4):299–309
Wolf G (2003) Lipofuscin and macular degeneration. Nutr Rev 61(10):342–346
Tate DJ Jr, Miceli MV, Newsome DA (1995) Phagocytosis and H2O2 induce catalase and metallothionein gene expression in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 36(7):1271–1279
Shang F, Taylor A (2004) Function of the ubiquitin proteolytic pathway in the eye. Exp Eye Res 78(1):1–14
Lutty G, Grunwald J, Majji AB, Uyama M, Yoneya S (1999) Changes in choriocapillaris and retinal pigment epithelium in age-related macular degeneration. Mol Vis 5:35
Bhutto IA, McLeod DS, Hasegawa T, Kim SY, Merges C et al (2006) Pigment epithelium-derived factor (PEDF) and vascular endothelial growth factor (VEGF) in aged human choroid and eyes with age-related macular degeneration. Exp Eye Res 82(1):99–110
Holekamp NM, Bouck N, Volpert O (2002) Pigment epithelium-derived factor is deficient in the vitreous of patients with choroidal neovascularization due to age-related macular degeneration. Am J Ophthalmol 134(2):220–227
Ardeljan CP, Ardeljan D, Abu-Asab M, Chan CC (2014) Inflammation and cell death in age-related macular degeneration: an immunopathological and ultrastructural model. J Clin Med 3(4):1542–1560
Hanus J, Kolkin A, Chimienti J, Botsay S, Wang S (2015) 4-acetoxyphenol prevents rpe oxidative stress-induced necrosis by functioning as an NRF2 stabilizer. Invest Ophthalmol Vis Sci 56(9):5048–5059
Tseng WA, Thein T, Kinnunen K, Lashkari K, Gregory MS et al (2013) NLRP3 inflammasome activation in retinal pigment epithelial cells by lysosomal destabilization: implications for age-related macular degeneration. Invest Ophthalmol Vis Sci 54(1):110–120
Gelfand BD, Wright CB, Kim Y, Yasuma T, Yasuma R et al (2015) Iron toxicity in the retina requires Alu RNA and the NLRP3 inflammasome. Cell Rep 11(11):1686–1693
Hanus J, Zhang H, Wang Z, Liu Q, Zhou Q et al (2013) Induction of necrotic cell death by oxidative stress in retinal pigment epithelial cells. Cell Death Dis 4(12):e965
Brandstetter C, Patt J, Holz FG, Krohne TU (2016) Inflammasome priming increases retinal pigment epithelial cell susceptibility to lipofuscin phototoxicity by changing the cell death mechanism from apoptosis to pyroptosis. J Photochem Photobiol B 161:177–183
Gavrieli Y, Sherman Y, Ben-Sasson SA (1992) Identification of programmed cell death in situ via specific labeling of nuclear DNA fragmentation. J Cell Biol 119(3):493–501
Xu GZ, Li WW, Tso MO (1996) Apoptosis in human retinal degenerations. Trans Am Ophthalmol Soc 94:411–430; discussion 430–411
Dunaief JL, Dentchev T, Ying GS, Milam AH (2002) The role of apoptosis in age-related macular degeneration. Arch Ophthalmol 120(11):1435–1442
Zacks DN, Hanninen V, Pantcheva M, Ezra E, Grosskreutz C et al (2003) Caspase activation in an experimental model of retinal detachment. Invest Ophthalmol Vis Sci 44(3):1262–1267
Zacks DN, Zheng QD, Han Y, Bakhru R, Miller JW (2004) Fas-mediated apoptosis and its relation to intrinsic pathway activation in an experimental model of retinal detachment. Invest Ophthalmol Vis Sci 45(12):4563–4569
Nakazawa T, Kayama M, Ryu M, Kunikata H, Watanabe R et al (2011) Tumor necrosis factor-alpha mediates photoreceptor death in a rodent model of retinal detachment. Invest Ophthalmol Vis Sci 52(3):1384–1391
Nakazawa T, Matsubara A, Noda K, Hisatomi T, She H et al (2006) Characterization of cytokine responses to retinal detachment in rats. Mol Vis 12:867–878
Hisatomi T, Sakamoto T, Murata T, Yamanaka I, Oshima Y et al (2001) Relocalization of apoptosis-inducing factor in photoreceptor apoptosis induced by retinal detachment in vivo. Am J Pathol 158(4):1271–1278
Trichonas G, Murakami Y, Thanos A, Morizane Y, Kayama M et al (2010) Receptor interacting protein kinases mediate retinal detachment-induced photoreceptor necrosis and compensate for inhibition of apoptosis. Proc Natl Acad Sci USA 107(50):21695–21700
Hisatomi T, Nakazawa T, Noda K, Almulki L, Miyahara S et al (2008) HIV protease inhibitors provide neuroprotection through inhibition of mitochondrial apoptosis in mice. J Clin Invest 118(6):2025–2038
Zhu Y, Zhao KK, Tong Y, Zhou YL, Wang YX et al (2016) Exogenous nad(+) decreases oxidative stress and protects H2O2-treated RPE cells against necrotic death through the up-regulation of autophagy. Sci Rep 6:26322
Vandenabeele P, Galluzzi L, Vanden Berghe T, Kroemer G (2010) Molecular mechanisms of necroptosis: an ordered cellular explosion. Nat Rev Mol Cell Biol 11(10):700–714
Arimura N, Ki-i Y, Hashiguchi T, Kawahara K, Biswas KK et al (2009) Intraocular expression and release of high-mobility group box 1 protein in retinal detachment. Lab Invest 89(3):278–289
Rebello G, Ramesar R, Vorster A, Roberts L, Ehrenreich L et al (2004) Apoptosis-inducing signal sequence mutation in carbonic anhydrase IV identified in patients with the RP17 form of retinitis pigmentosa. Proc Natl Acad Sci USA 101(17):6617–6622
Gorbatyuk MS, Knox T, LaVail MM, Gorbatyuk OS, Noorwez SM et al (2010) Restoration of visual function in P23H rhodopsin transgenic rats by gene delivery of BiP/Grp78. Proc Natl Acad Sci USA 107(13):5961–5966
Tam BM, Moritz OL (2006) Characterization of rhodopsin P23H-induced retinal degeneration in a Xenopus laevis model of retinitis pigmentosa. Invest Ophthalmol Vis Sci 47(8):3234–3241
Shinohara T, Mulhern ML, Madson CJ (2008) Silencing gene therapy for mutant membrane, secretory, and lipid proteins in retinitis pigmentosa (RP). Med Hypotheses 70(2):378–380
Sanges D, Marigo V (2006) Cross-talk between two apoptotic pathways activated by endoplasmic reticulum stress: differential contribution of caspase-12 and AIF. Apoptosis 11(9):1629–1641
Yang LP, Wu LM, Guo XJ, Tso MO (2007) Activation of endoplasmic reticulum stress in degenerating photoreceptors of the rd1 mouse. Invest Ophthalmol Vis Sci 48(11):5191–5198
Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K (2013) Seven-year outcomes in ranibizumab-treated patients in anchor, marina, and horizon: a multicenter cohort study (seven-up). Ophthalmology 120(11):2292–2299
Peyman GA, Blinder KJ, Paris CL, Alturki W, Nelson NC Jr et al (1991) A technique for retinal pigment epithelium transplantation for age-related macular degeneration secondary to extensive subfoveal scarring. Ophthalmic Surg 22(2):102–108
Algvere PV, Gouras P, Dafgard Kopp E (1999) Long-term outcome of RPE allografts in non-immunosuppressed patients with amd. Eur J Ophthalmol 9(3):217–230
Renno RZ, Miller JW (2001) Photosensitizer delivery for photodynamic therapy of choroidal neovascularization. Adv Drug Deliv Rev 52(1):63–78
Han DP, McAllister JT, Weinberg DV, Kim JE, Wirostko WJ (2010) Combined intravitreal anti-VEGF and verteporfin photodynamic therapy for juxtafoveal and extrafoveal choroidal neovascularization as an alternative to laser photocoagulation. Eye (Lond) 24(4):713–716
Chew EY, Clemons TE, Agrón E, Sperduto RD, SanGiovanni JP et al (2014) Ten-year follow-up of age-related macular degeneration in the age-related eye disease study: AREDS report no. 36. JAMA Ophthalmol 132(3):272–277
Chew EY, Clemons TE, Keenan TDL, Agron E, Malley CE et al (2021) The results of the 10 year follow-on study of the age-related eye disease study 2 (AREDS2). Invest Ophthalmol Vis Sci 62(8):1215–1215
Group* TA-REDSR (2013) Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA 309(19):2005–2015
Chew EY, Clemons TE, Agrón E, Domalpally A, Keenan TDL et al (2022) Long-term outcomes of adding lutein/zeaxanthin and ω-3 fatty acids to the AREDS supplements on age-related macular degeneration progression: AREDS2 report. JAMA Ophthalmol 140:692–698
da Cruz L, Dorn JD, Humayun MS, Dagnelie G, Handa J et al (2016) Five-year safety and performance results from the Argus II retinal prosthesis system clinical trial. Ophthalmology 123(10):2248–2254
Lewis PM, Ayton LN, Guymer RH, Lowery AJ, Blamey PJ et al (2016) Advances in implantable bionic devices for blindness: a review. ANZ J Surg 86(9):654–659
Jung JH, Aloni D, Yitzhaky Y, Peli E (2015) Active confocal imaging for visual prostheses. Vis Res 111(Pt B):182–196
Luo G, Peli E (2011) Development and evaluation of vision rehabilitation devices. In: Conference proceedings: annual international conference of the IEEE engineering in medicine and biology society, pp 5228–5231
Gonzalez-Cordero A, Kruczek K, Naeem A, Fernando M, Kloc M et al (2017) Recapitulation of human retinal development from human pluripotent stem cells generates transplantable populations of cone photoreceptors. Stem Cell Rep 9(3):820–837
Kruczek K, Gonzalez-Cordero A, Goh D, Naeem A, Jonikas M et al (2017) Differentiation and transplantation of embryonic stem cell-derived cone photoreceptors into a mouse model of end-stage retinal degeneration. Stem Cell Rep 8(6):1659–1674
Decembrini S, Koch U, Radtke F, Moulin A, Arsenijevic Y (2014) Derivation of traceable and transplantable photoreceptors from mouse embryonic stem cells. Stem Cell Rep 2(6):853–865
Wahlin KJ, Maruotti JA, Sripathi SR, Ball J, Angueyra JM et al (2017) Photoreceptor outer segment-like structures in long-term 3D retinas from human pluripotent stem cells. Sci Rep 7(1):766
Zhong X, Gutierrez C, Xue T, Hampton C, Vergara MN et al (2014) Generation of three-dimensional retinal tissue with functional photoreceptors from human iPSCs. Nat Commun 5:4047
Chang TS, Bressler NM, Fine JT, Dolan CM, Ward J et al (2007) Improved vision-related function after ranibizumab treatment of neovascular age-related macular degeneration: results of a randomized clinical trial. Arch Ophthalmol 125(11):1460–1469
Fernandez-Robredo P, Sancho A, Johnen S, Recalde S, Gama N et al (2014) Current treatment limitations in age-related macular degeneration and future approaches based on cell therapy and tissue engineering. J Ophthalmol 2014:510285
Arai S, Thomas BB, Seiler MJ, Aramant RB, Qiu G et al (2004) Restoration of visual responses following transplantation of intact retinal sheets in rd mice. Exp Eye Res 79(3):331–341
Ghosh F, Wong F, Johansson K, Bruun A, Petters RM (2004) Transplantation of full-thickness retina in the rhodopsin transgenic pig. Retina 24(1):98–109
Aramant RB, Seiler MJ (2002) Transplanted sheets of human retina and retinal pigment epithelium develop normally in nude rats. Exp Eye Res 75(2):115–125
Eberle D, Santos-Ferreira T, Grahl S, Ader M (2014) Subretinal transplantation of macs purified photoreceptor precursor cells into the adult mouse retina. J Vis Exp 84:e50932
MacLaren RE, Pearson RA, MacNeil A, Douglas RH, Salt TE et al (2006) Retinal repair by transplantation of photoreceptor precursors. Nature 444(7116):203–207
Liu Y, Chen SJ, Li SY, Qu LH, Meng XH et al (2017) Long-term safety of human retinal progenitor cell transplantation in retinitis pigmentosa patients. Stem Cell Res Ther 8(1):209
Klassen H, Kiilgaard JF, Warfvinge K, Samuel MS, Prather RS et al (2012) Photoreceptor differentiation following transplantation of allogeneic retinal progenitor cells to the dystrophic rhodopsin Pro347Leu transgenic pig. Stem Cells Int 2012:939801
Jones MK, Lu B, Saghizadeh M, Wang S (2016) Gene expression changes in the retina following subretinal injection of human neural progenitor cells into a rodent model for retinal degeneration. Mol Vis 22:472–490
McGill TJ, Cottam B, Lu B, Wang S, Girman S et al (2012) Transplantation of human central nervous system stem cells-neuroprotection in retinal degeneration. Eur J Neurosci 35(3):468–477
Tham YC, Li X, Wong TY, Quigley HA, Aung T et al (2014) Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 121(11):2081–2090
Mandai M, Watanabe A, Kurimoto Y, Hirami Y, Morinaga C et al (2017) Autologous induced stem-cell-derived retinal cells for macular degeneration. N Engl J Med 376(11):1038–1046
Kamao H, Mandai M, Ohashi W, Hirami Y, Kurimoto Y et al (2017) Evaluation of the surgical device and procedure for extracellular matrix-scaffold-supported human iPSC-derived retinal pigment epithelium cell sheet transplantation. Invest Ophthalmol Vis Sci 58(1):211–220
Assawachananont J, Mandai M, Okamoto S, Yamada C, Eiraku M et al (2014) Transplantation of embryonic and induced pluripotent stem cell-derived 3D retinal sheets into retinal degenerative mice. Stem Cell Rep 2(5):662–674
Thomas BB, Zhu D, Zhang L, Thomas PB, Hu Y et al (2016) Survival and functionality of hESC-derived retinal pigment epithelium cells cultured as a monolayer on polymer substrates transplanted in RCS rats. Invest Ophthalmol Vis Sci 57(6):2877–2887
Wang J, Westenskow PD, Fang M, Friedlander M, Siuzdak G (2016) Quantitative metabolomics of photoreceptor degeneration and the effects of stem cell-derived retinal pigment epithelium transplantation. Philos Trans R Soc Math Phys Eng Sci 374:20150376
Carr AJ, Vugler AA, Hikita ST, Lawrence JM, Gias C et al (2009) Protective effects of human iPS-derived retinal pigment epithelium cell transplantation in the retinal dystrophic rat. PLoS ONE 4(12):e8152
Becker S, Eastlake K, Jayaram H, Jones MF, Brown RA et al (2016) Allogeneic transplantation of muller-derived retinal ganglion cells improves retinal function in a feline model of ganglion cell depletion. Stem Cells Transl Med 5(2):192–205
Singhal S, Bhatia B, Jayaram H, Becker S, Jones MF et al (2012) Human muller glia with stem cell characteristics differentiate into retinal ganglion cell (RGC) precursors in vitro and partially restore RGC function in vivo following transplantation. Stem Cells Transl Med 1(3):188–199
Wang SZ, Ma W, Yan RT, Mao W (2010) Generating retinal neurons by reprogramming retinal pigment epithelial cells. Expert Opin Biol Ther 10(8):1227–1239
Aftab U, Jiang C, Tucker B, Kim JY, Klassen H et al (2009) Growth kinetics and transplantation of human retinal progenitor cells. Exp Eye Res 89(3):301–310
Ashtari M, Zhang H, Cook PA, Cyckowski LL, Shindler KS et al (2015) Plasticity of the human visual system after retinal gene therapy in patients with Leber’s congenital amaurosis. Sci Transl Med 7(296):296ra110
Maguire AM, Simonelli F, Pierce EA, Pugh EN Jr, Mingozzi F et al (2008) Safety and efficacy of gene transfer for Leber’s congenital amaurosis. N Engl J Med 358(21):2240–2248
Bertolotti E, Neri A, Camparini M, Macaluso C, Marigo V (2014) Stem cells as source for retinal pigment epithelium transplantation. Prog Retinal Eye Res 42:130–144
Schwartz SD, Hubschman JP, Heilwell G, Franco-Cardenas V, Pan CK et al (2012) Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet 379(9817):713–720
Song WK, Park KM, Kim HJ, Lee JH, Choi J et al (2015) Treatment of macular degeneration using embryonic stem cell-derived retinal pigment epithelium: preliminary results in Asian patients. Stem Cell Rep 4(5):860–872
Han L, Ma Z, Wang C, Dou H, Hu Y et al (2013) Autologous transplantation of simple retinal pigment epithelium sheet for massive submacular hemorrhage associated with pigment epithelium detachment. Invest Ophthalmol Vis Sci 54(7):4956–4963
Kelley MW, Turner JK, Reh TA (1995) Regulation of proliferation and photoreceptor differentiation in fetal human retinal cell cultures. Invest Ophthalmol Vis Sci 36(7):1280–1289
Sinha D, Phillips J, Joseph Phillips M, Gamm DM (2016) Mimicking retinal development and disease with human pluripotent stem cells. Invest Ophthalmol Vis Sci 57(5):ORSFf1–ORSFf9
Ohlemacher SK, Iglesias CL, Sridhar A, Gamm DM, Meyer JS (2015) Generation of highly enriched populations of optic vesicle-like retinal cells from human pluripotent stem cells. Curr Protoc Stem Cell Biol 32:1h.8.1-1h.8.20
Diniz B, Thomas P, Thomas B, Ribeiro R, Hu Y, Brant R, Ahuja A, Zhu D, Liu L, Koss M et al (2013) Subretinal implantation of retinal pigment epithelial cells derived from human embryonic stem cells: improved survival when implanted as a monolayer. Invest Ophthalmol Vis Sci 54:5087–5096
Kamao H, Mandai M, Okamoto S, Sakai N, Suga A et al (2014) Characterization of human induced pluripotent stem cell-derived retinal pigment epithelium cell sheets aiming for clinical application. Stem Cell Rep 2(2):205–218
Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ et al (2015) Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet 385(9967):509–516
Cyranoski D (2014) Japanese woman is first recipient of next-generation stem cells. Nature 12
Rowland TJ, Blaschke AJ, Buchholz DE, Hikita ST, Johnson LV et al (2013) Differentiation of human pluripotent stem cells to retinal pigmented epithelium in defined conditions using purified extracellular matrix proteins. J Tissue Eng Regen Med 7(8):642–653
Nasonkin IO, Merbs SL, Lazo K, Oliver VF, Brooks M, Patel K, Enke RA, Nellissery J, Jamrich M, Le YZ et al (2013) Conditional knockdown of DNA methyltransferase 1 reveals a key role of retinal pigment epithelium integrity in photoreceptor outer segment morphogenesis. Development 140:1330–1341
Shadforth AM, George KA, Kwan AS, Chirila TV, Harkin DG (2012) The cultivation of human retinal pigment epithelial cells on Bombyx mori silk fibroin. Biomaterials 33(16):4110–4117
McHugh KJ, Tao SL, Saint-Geniez M (2014) Porous poly(ε-caprolactone) scaffolds for retinal pigment epithelium transplantation. Invest Ophthamol Vis Sci 55:1754–1762
Croze RH, Clegg DO (2014) Differentiation of pluripotent stem cells into retinal pigmented epithelium. Dev Opthalmol 53:81–96
Lu B, Zhu D, Hinton D, Humayun MS, Tai YC (2012) Mesh-supported submicron parylene-c membranes for culturing retinal pigment epithelial cells. Biomed Microdevices 14(4):659–667
Hu Y, Liu L, Lu B, Zhu D, Ribeiro R et al (2012) A novel approach for subretinal implantation of ultrathin substrates containing stem cell-derived retinal pigment epithelium monolayer. Ophthalmic Res 48(4):186–191
Liu Z, Yu N, Holz FG, Yang F, Stanzel BV (2014) Enhancement of retinal pigment epithelial culture characteristics and subretinal space tolerance of scaffolds with 200 nm fiber topography. Biomaterials 35(9):2837–2850
Merodio M, Irache JM, Valamanesh F, Mirshahi M (2002) Ocular disposition and tolerance of ganciclovir-loaded albumin nanoparticles after intravitreal injection in rats. Biomaterials 23(7):1587–1594
Kim JH, Kim MH, Jo DH, Yu YS, Lee TG et al (2011) The inhibition of retinal neovascularization by gold nanoparticles via suppression of VEGFR-2 activation. Biomaterials 32(7):1865–1871
Jo DH, Kim JH, Yu YS, Lee TG, Kim JH (2012) Antiangiogenic effect of silicate nanoparticle on retinal neovascularization induced by vascular endothelial growth factor. Nanomedicine 8(5):784–791
Mitra RN, Merwin MJ, Han Z, Conley SM, Al-Ubaidi MR et al (2014) Yttrium oxide nanoparticles prevent photoreceptor death in a light-damage model of retinal degeneration. Free Radic Biol Med 75:140–148
Zhou HY, Hao JL, Wang S, Zheng Y, Zhang WS (2013) Nanoparticles in the ocular drug delivery. Int J Ophthalmol 6(3):390–396
Koirala A, Makkia RS, Cooper MJ, Naash MI (2011) Nanoparticle-mediated gene transfer specific to retinal pigment epithelial cells. Biomaterials 32(35):9483–9493
Rajala A, Wang Y, Zhu Y, Ranjo-Bishop M, Ma JX et al (2014) Nanoparticle-assisted targeted delivery of eye-specific genes to eyes significantly improves the vision of blind mice in vivo. Nano Lett 14(9):5257–5263
Aukunuru JV, Ayalasomayajula SP, Kompella UB (2003) Nanoparticle formulation enhances the delivery and activity of a vascular endothelial growth factor antisense oligonucleotide in human retinal pigment epithelial cells. J Pharm Pharmacol 55(9):1199–1206
Bourges JL, Gautier SE, Delie F, Bejjani RA, Jeanny JC et al (2003) Ocular drug delivery targeting the retina and retinal pigment epithelium using polylactide nanoparticles. Invest Ophthalmol Vis Sci 44(8):3562–3569
Bejjani RA, BenEzra D, Cohen H, Rieger J, Andrieu C et al (2005) Nanoparticles for gene delivery to retinal pigment epithelial cells. Mol Vis 11:124–132
Moshfeghi AA, Peyman GA (2005) Micro- and nanoparticulates. Adv Drug Deliv Rev 57(14):2047–2052
Naash M (2006) Applications of nanotechnology to gene delivery in ophthalmology. Invest Ophthalmol Vis Sci 2006:53
Liu J, Min SH, Chiodo V, Boye SL, Alexander J et al (2006) Linear polyethylenimine-based DNA nanoparticle delivery into mouse retinas. Invest Ophthalmol Vis Sci 47(13):844–844
Xu Q, Kambhampati SP, Kannan RM (2013) Nanotechnology approaches for ocular drug delivery. Middle East Afr J Ophthalmol 20(1):26–37
Sakurai E, Ozeki H, Kunou N, Ogura Y (2001) Effect of particle size of polymeric nanospheres on intravitreal kinetics. Ophthalmic Res 33(1):31–36
Sakai T, Kuno N, Takamatsu F, Kimura E, Kohno H et al (2007) Prolonged protective effect of basic fibroblast growth factor-impregnated nanoparticles in royal college of surgeons rats. Invest Ophthalmol Vis Sci 48(7):3381–3387
Ideta R, Tasaka F, Jang WD, Nishiyama N, Zhang GD et al (2005) Nanotechnology-based photodynamic therapy for neovascular disease using a supramolecular nanocarrier loaded with a dendritic photosensitizer. Nano Lett 5(12):2426–2431
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria, educational grants, participation in speakers’ bureaus, membership, employment, consultancies, stock ownership or other equity interest and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shome, I., Thathapudi, N.C., Aramati, B.M.R. et al. Stages, pathogenesis, clinical management and advancements in therapies of age-related macular degeneration. Int Ophthalmol 43, 3891–3909 (2023). https://doi.org/10.1007/s10792-023-02767-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02767-2