Abstract
Objective
The present study aimed to evaluate the anti-inflammatory and analgesic activities of the ginsenoside metabolite compound K (CK) and its mechanisms.
Methods
Mice model of xylene-induced ear swelling and rat model of carrageenan-induced paw swelling were used to evaluate the effect of CK on acute inflammation. The analgesic effect of CK was evaluated on heat-, acetic acid-, and carrageenan-induced hyperalgesia. The levels of prostaglandin E2 (PGE2), cyclooxygenase-1 (COX-1), and COX-2 in carrageenan-induced rat paw swelling and gastric mucosa were detected by enzyme-linked immunosorbent assay (ELISA). COX-1 and COX-2 expressions in carrageenan-induced rat paw swelling and gastric mucosa were detected by western blotting. In vitro effect of CK (10−9, 10−8, 10−7, 10−6, 10−5 M) on COX-1 and COX-2 activities was evaluated by measuring the production of 6-keto-PGF1α and PGE2 in rat peritoneal macrophages.
Results
CK at doses of 7, 14, 28, 56, 112, and 224 mg/kg alleviated xylene-induced ear oedema, whereas CK at 40, 80, and 160 mg/kg alleviated carrageenan-induced paw oedema. CK at 224 mg/kg showed an analgesic effect against acetic acid-induced pain. CK at 40, 80, and 160 mg/kg significantly increased rat inflammatory pain threshold, but had no effect on heat-induced pain threshold. CK at 10, 20, 40, 80, and 160 mg/kg reduced PGE2 level in the paw tissue, but showed no effect on that in the gastric mucosa. CK at 20, 40, 80, and 160 mg/kg decreased COX-2 expression in the paw tissue and gastric mucosa, but exhibited no effect on COX-1 expression or on COX-1 and COX-2 activities.
Conclusion
CK exerted anti-inflammatory and analgesic effects, possibly by reducing the catalytic synthesis of PGE2 via downregulation of COX-2 expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ginsenoside metabolite compound K [20-O-β-d-glucopyranosyl-20 (S)-ginophenol, CK] belongs to the protopanaxadiol group of saponins. It was isolated by Japanese researchers in 1972 from ginsenosides, such as Rb1, Rb2 and Rc, though various transformation methods (Christensen 2009). Studies have shown that the pharmacological activity of ginsenosides was mainly mediated through its metabolic component CK, which possesses a variety of pharmacological activities such as anti-inflammatory, antitumor, antidiabetes, hepatoprotective, neuroprotective, and cardiovascular protective effects.
Our previous study found that CK exerted immunomodulatory and anti-arthritic activities in animal models of adjuvant-induced arthritis (AA) (Wu et al. 2014; Chen et al. 2014; Chen et al. 2016) and collagen-induced arthritis (CIA) (Chen et al. 2015; Liu et al. 2014). We found that CK significantly reduced the global assessment and arthritis index in CIA mice and AA rats, reduced swelling in the joint, improved joint histopathology, inhibited synovial cell proliferation and angiogenesis, reduced inflammatory cell infiltration in the synovium and prevented bone destruction. In addition, CK exerted immunomodulatory effects in AA rats and CIA mice by reducing abnormal activation of immune cells (dendritic cells, T cells, and B cells) and restoring cytokine balance (Chen et al. 2014; Chen et al. 2016; Chen et al. 2015; Liu et al. 2014). These findings suggest that the immunomodulatory activity of CK may be an important mechanism of its anti-inflammatory effect. However, whether CK exhibited direct anti-inflammatory and analgesic activities remains unclear.
Inflammation is usually associated with pain (Khan et al. 2017). In fact, chemical mediators generated during inflammation, such as serotonin, prostaglandins (PGs), TNF-α, histamine, bradykinin, and protons, stimulate the nociceptive receptors responsible for peripheral pain (Woolf and Max 2001). PGs are lipid mediators synthesized from arachidonic acid by cyclooxygenase (COX) enzymes (Funk 2001). PGE2, the main PG produced during inflammatory response, is a proinflammatory lipid mediator of inflammation. PGE2 participates in the initiation of inflammation and emergence of inflammatory signs such as oedema, fever, and pain (Díaz-Muñoz et al. 2010; Alvarez-Soria et al. 2008; Liao and Milas 2004; Zheng et al. 2011). Previous studies suggest that the inhibition of PGE2 synthesis is necessary to relieve the inflammatory hyperalgesia (Chandrasekhar et al. 2016).
In this study, based on previous studies, the direct anti-inflammatory activity of CK was evaluated in acute inflammatory animal models of xylene-induced ear swelling and carrageenan-induced paw oedema. The hot plate test, acetate-induced writhing test, and carrageenan induction inflammatory pain model were established to evaluate the analgesic effect of CK. The possible mechanism was explored by detecting PGE2, COX-1, and COX-2.
Materials and methods
Animals and cells
Male Sprague–Dawley rats (130–170 g) and Kunming mice (16–20 g) were purchased from the Experimental Animal Center of Anhui Province [production license number: SCXK (Anhui) 2011-002]. All animals were maintained in a specific pathogen-free animal laboratory of Anhui Medical University (Hefei, China). All experiments were approved on 6 Mar 2015 by the Ethics Review Committee for Animal Experimentation of the Institute of Clinical Pharmacology, Anhui Medical University.
To collect 10-ml peritoneal macrophage cells, ice-cold DMEM was injected into the rat abdominal cavity. The cells were allowed to adhere for 3 h, washed three times with phosphate buffered saline (PBS) to remove non-adherent cells, and then used for analyses.
Reagents
CK (molecular weight: 622.18, lot NO. S090301) was provided by Hisun Pharmaceutical Co., Ltd (Taizhou, China), intragastrically administered in suspension with 0.5% sodium carboxymethyl cellulose (CMC-Na). Celecoxib (lot NO. BK13CCEK164) was obtained from Pfizer Pharmaceuticals Ltd. Sufentanil was purchased from Yichang Renfu Medicine Co., Ltd. (Hubei, China). DMEM was obtained from Biological Industries. Fetal bovine serum (FBS) was purchased from Gemini. COX, 6-keto-PGF1α, and PGE2 enzyme-linked immunosorbent assay (ELISA) kit were purchased from Cusabio Biotech Co., Ltd. (Wuhan, China). Acetic acid (SCXK [Su] xk13-011-00020) was obtained from China Sun Speciality Products Co., Ltd. (Jiangsu, China). Anti-COX-2 Ab was purchased from Abcam (Lot.GR-38765-22), whereas anti-COX-1 Ab was purchased from Proteintech (Rocky Hill, USA). Lipopolysaccharide (LPS) and arachidonic acid were purchased from Sigma (St. Louis, MO, USA).
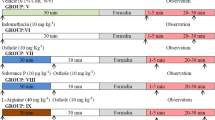
Xylene-induced ear swelling
Xylene-induced ear swelling model was used to evaluate the anti-inflammatory effect of CK on acute inflammation. A total of 90 male Kunming mice were divided into the following groups (n = 10): normal, vehicle-treated control, CK (7, 14, 28, 56, 112, 224 mg/kg), and positive control (celecoxib 28 mg/kg). The test substances were administered intragastrically every day for 5 days. 1 h after the last administration, xylene (20 μl) was coated on the mouse left ear. After 1.5 h, the mice were anesthetized and killed, and the ears were cut using a hole punch and weighed. The investigator evaluating the oedema was blinded to the experimental groups. Finally, the degree of swelling was measured by calculating the difference in weight between the left and right ears. The swelling inhibition rate of each drug group was thus calculated.
Carrageenan induction of paw oedema
In the carrageenan-induced paw oedema model, rats were subjected to intraplantar carrageenan injection and the foot volume was measured. Ninety male Sprague–Dawley rats were randomly divided into nine groups (n = 10), namely, normal, vehicle-treated control, CK (5, 10, 20, 40, 80, and 160 mg/kg), and positive control celecoxib (20 mg/kg) groups. CK was orally administrated every day for 5 days. 1 h after the last administration, 50 μl of carrageenan (1%) was injected intraplantar into the right hind paw. oedema was measured using a plethysmometer (YLS-7B, Shandong, China) at various times points (0, 1, 2, 3, 4, 5, and 6 h) after the injection of the phlogistic agent. The investigator evaluating the oedema was blinded to the experimental groups. Finally, the degree of swelling was measured by calculating the difference in volume between the anterior and posterior paws. The oedema inhibitory rate of each drug group was calculated.
oedema inhibition (%) = 1 − (Vt/Vc) × 100%, in which Vt is the mean value of paw volume in rats treated with CK or celecoxib and Vc is the mean value of paw volume in the model control group.
Hot plate test in mice
Since the scrotal skin of male mice is sensitive to heat, male mice will frequently jump during the hot plate test, hindering the observation for hind paw licking. Thus, female mice are more suitable for hot plate test. Female mice weighing 18 ± 2 g were placed on a hot plate with temperature detector (YLS-6B, Shandong, China). The metal plate was preheated to 50–55 °C and maintained at a constant temperature within ± 0.5 °C. The reaction time between the foot contact with the hot plate and the moment of licking, which was the latent period of hot plate reaction, was recorded and used for calculation of the pain threshold index. First, the basal pain threshold of each group was determined with normal values of 5–30 s. Mice with pain threshold lower than 5 s or higher than 30 s were removed from the study. Ninety mice were randomly divided into nine groups (n = 10): normal, vehicle-treated control, CK (7, 14, 28, 56, 112, and 224 mg/kg), and positive control sufentanil (40 µg/kg) groups. The test substances were orally administrated daily for 5 days. 1 h after the last administration, the pain threshold of each mouse was determined by investigator who was blinded to the experimental groups. In mice whose latent period was up to 60 s, the test was terminated and the latent period was recorded as 60 s to avoid tissue damage. Experimental results were indicated by pain threshold value.
Introduction of acetic acid-induced writhing model
Ninety male Kunming mice (18 ± 2 g) were randomly divided into nine groups (n = 10): normal, vehicle-treated control, CK (7, 14, 28, 56, 112, and 224 mg/kg), and positive control celecoxib (28 mg/kg) groups. The test substances were orally administrated daily for 5 days. 1 h after the last administration, each mouse was intraperitoneally injected with 0.4 ml 0.6% acetic acid solution. The number of mouse body writhing was recorded within 5 min post-injection by investigator who was blinded to the experimental groups. Inhibition rate of acetic acid-induced writhing in the mice was calculated to evaluate the analgesic effect of CK.
Analgesic capacity (%) = (1 − Wt/Wc) × 100%, in which Wt is the average number of writhing in mice treated with CK or celecoxib, whereas Wc is the average number of writhing in the model group.
Assessment of mechanical allodynia
To assess mechanical allodynia, the number of paw withdrawal responses to a mechanical nociceptive stimulation was measured in carrageenan-induced paw oedema rat model. Ninety male Sprague–Dawley rats were randomly divided into nine groups (n = 10), including normal, vehicle-treated control, CK (5, 10, 20, 40, 80, and 160 mg/kg), and positive control celecoxib (20 mg/kg) groups. The test substances were orally administrated every day for 5 days. 1 h after the last administration, 50 μl of carrageenan (1%) was administered via intraplantar injection to the right hind paw. The pain threshold was measured at 1, 2, 3, 4, 5, and 6 h after the intraplantar carrageenan injection using a von Frey filament with a force of 4.0 g (Electronic von Frey anesthesiometer, IITC Inc., Life Science Instruments, Woodland Hills, CA, USA). The investigator evaluating the mechanical allodynia was blinded to the experimental groups. Rats were placed in acrylic cages with a wire grid floor 15–30 min before the beginning of the tests in a quiet room. During this adaptation period, the paws were poked 2–3 times. Before paw stimulation, the animals were quiet, without exploratory defecation or urination movements and not resting over the paws. The tests consisted of poking the hind paw to provoke a flexion reflex followed by a clear flinch response after paw withdrawal. The stimulation of the paw was repeated until the animal presented three similar measurements (the difference between the highest and the lowest measurement should be less than 10 g). The animals were tested before and after the treatments and the results are reported as withdrawal threshold (g).
PGE2 and COX detection by ELISA
The swollen right foot was peeled, cut, soaked in 5-ml normal saline for 1 h, and centrifuged to obtain the supernatant for detection of PGE2, COX-1, and COX-2 levels using commercial kits. The assays were performed according to the manufacturers’ instructions. The absorbance of the produced color was measured spectrophotometrically at 450 nm using a microplate reader (infinite M1000 PRO, TECAN).
Analysis of COX-1 and COX-2 expressions
Western blot analysis was performed to evaluate the COX-1 and COX-2 protein levels in the paw tissue of rats submitted to carrageenan-induced paw oedema. For protein extraction, 50 mg of paw or gastric mucosal tissues was added to 0.6-ml tissue lysate solution and centrifuged at 12,000×g for 10 min at 4 °C. The supernatant was then used for western blotting. Protein samples were separated using 10% SDS-polyacrylamide gel electrophoresis and transferred onto polyvinylidene fluoride (PVDF) microporous membranes (Bio-Rad, Shanghai, China). The membrane was blocked by incubation for 1 h at room temperature in 5% skimmed milk. The membrane was further incubated with primary antibodies overnight at 4 °C, and with horseradish peroxidase conjugated secondary antibodies for 2 h at room temperature. The protein bands were visualized using ECL.
Assay of COX-1 and COX-2 activity
Cells were washed in PBS and were then incubated at 37 °C with DMEM alone or with CK (10−9, 10−8, 10−7, 10−6, 10−5 M) dissolved in DMEM. After incubation for 30 min, 3 μM arachidonic acid was added to each well and COX-1 enzyme activity was assessed by measuring 6-keto-PGF1α production over 15 min. After the specified time period, the culture medium was centrifuged at 1500×g for 3 min at 4 °C and the concentration of 6-keto-PGF1α in the supernatant was measured using an assay kit.
For the COX-2 assay, cells were seeded in DMEM containing 0.5% FBS and 300-μM aspirin was added to the cells to irreversibly block the constitutive expression of COX-1. After 30 min of incubation, plates were washed three times to remove non-adherent cells and any residual aspirin. The adherent cells were incubated for 20 h at 37 °C with 1 μg/ml LPS in DMEM containing 5% FBS. Subsequently, the cells were washed with DMEM three times and the inhibition assay of induced COX-2 was performed by incubating the cells at 37 °C with CK (10−9, 10−8, 10−7, 10−6, 10−5 M), dissolved in DMEM or with DMEM alone. After 30 min, 3 μM arachidonic acid was added to each well and COX-2 enzyme activity was assessed by measuring PGE2 production over 15 min. After this period, the culture medium was centrifuged at 1500 g for 3 min at 4 °C and the concentration of PGE2 in the supernatant was measured using an assay kit.
Statistical analysis
Statistical analyses were performed using SPSS. Data were expressed as mean ± standard deviation (SD). The analysis of variance (ANOVA) was used to determine significant differences between groups. Values of P less than 0.05 were considered to be significant.
Results
CK inhibited xylene-induced ear oedema
In comparison with that of the normal group, xylene induced redness in the left ear of mice in the model group. Compared with that in the model group, CK (7, 14, 28, 56, 112, and 224 mg/kg) and celecoxib (28 mg/kg) significantly reduced xylene-induced swelling in the mouse ear. The inhibitory effect of CK was dose-dependent, with CK at the highest dose of 224 mg/kg exhibiting a maximum inhibition efficiency of 93.9% (Table 1, Fig. 1).
CK alleviated carrageenan-induced oedema in rat paws
Compared with that of the normal group, oedema appeared in the paw 1 h after intradermal injection of carrageenan reached the peak 4 h, and then remitted. The paw oedema in the drug-treated groups showed no statistical difference with that in the normal group at 1 h post-injection. However, CK at 80 and 160 mg/kg and celecoxib 20 mg/kg reduced paw oedema after 2, 3, 4, 5, and 6 h post-injection, whereas CK at 40 mg/kg reduced paw oedema after 4, 5, and 6 h post-carrageenan injection (Tables 2, 3, Fig. 2).
Analgesic effect of CK on heat-induced pain in mice
Hot plate was used to inflict heat-induced pain in mice for measurement of pain threshold. Compared with the control group, CK (7, 14, 28, 56, 112, and 224 mg/kg) exhibited no effect on the pain threshold of the mice, whereas sufentanil (40 μg/kg) showed a significant increase in pain threshold, indicating that CK exerted no analgesic effect on heat-induced pain in mice (Table 4).
Analgesic effect of CK on writhing response in mice
In this study, acetic acid-induced writhing response was used to evaluate the peripheral analgesic effect of CK. 5 min after intraperitoneal injection of 0.6% acetic acid, the mice showed a significant number of writhing responses. Compared with those of the model group, CK 224 mg/kg and celecoxib 28 mg/kg significantly reduced acetic acid-induced writhing responses in mice (Table 5, Fig. 3).
Analgesic effect of CK on carrageenan-induced mechanical hyperalgesia
Carrageenan-induced inflammatory pain was used to evaluate the analgesic effect of CK on pain induced by mechanical stimulus. Compared with that of the normal group, rat pain threshold decreased 2 h after intradermal injection of carrageenan, reached peak after 4 h, and then increased. Compared with that of the model group, CK 40, 80, 160 and mg/kg and celecoxib 20 mg/kg significantly increased the pain threshold of rats at 3 h, 4 h, 5 h and 6 h after carrageenan injection (Fig. 4).
CK reduced the level of PGE2 and downregulated COX-2 expression
PGE2 level in the swollen paw of the carrageenan-induced paw oedema model rats was higher than that of the normal group, and was lowered by CK treatments at 10, 20, 40, 80, and 160 mg/kg. In contrast, PGE2 level in the gastric mucosa of the model group was not significantly different than that of the normal and CK groups. Compared with the normal group, the expression of COX-2 expressions in the swollen paw and gastric mucosa the model group were higher than those of the normal group, which was lowered by treatment with CK at 20, 40, 80, and 160 mg/kg. However, COX-1 expressions in the swollen paw and gastric mucosa of the model group were not significantly different than those of the normal and CK groups (Figs. 5, 6).
Effects of CK on paw levels of PGE2, COX-1, and COX-2. a The level of PGE2 in paw tissue detected by ELISA. Data are expressed as the mean ± SD of 10 animals. b, c COX-1 and COX-2 levels in paw tissue detected by ELISA. Data are expressed as the mean ± SD of 10 animals. d–f COX-1 and COX-2 expressions in paw tissue detected by western blot. Data are shown as the mean ± SD of three replicate experiments. #P < 0.05, ##P < 0.01 vs normal, *P < 0.05, **P < 0.01 vs model
Effects of CK on the level of PGE2, COX-1 and COX-2 in gastric mucosa. a The level of PGE2 in gastric mucosa assayed by ELISA. Data are expressed as the mean ± SD of 10 animals. b–d COX-1 and COX-2 expressions in gastric mucosa assayed by western blot. Data are shown as the mean ± SD of 3 replicate experiments. #P < 0.05, ##P < 0.01 vs normal, *P < 0.05, **P < 0.01 vs model
The effect of CK on COX-1 and COX-2 activity
Normal rat peritoneal macrophages were treated with CK at concentrations of 10−9, 10−8, 10−7, 10−6, 10−5 M, but showed no change in 6-keto-PGF1α production, suggesting that CK had no effect on COX-1 activity. After blocking COX-1 expression, PGE2 expression in rat peritoneal macrophages was increased by LPS (1 μg/ml) treatment for 20 h. However, CK at concentrations of 10−9, 10−8, 10−7, 10−6, 10−5 M showed no effect on PGE2 production in rat peritoneal macrophages, suggesting that CK had no effect on COX-2 activity (Fig. 7).
Discussion
CK reportedly shows anti-inflammatory effect in vitro (Joh et al. 2011; Yang et al. 2008). The present study provided a direct evidence of an anti-inflammatory effect of CK in animal models. Xylene-induced mouse ear oedema and carrageenan-induced rat paw oedema are classical acute inflammatory models widely used to evaluate anti-inflammatory drugs. The present study showed that CK reduced xylene-induced mouse ear oedema and carrageenan-induced rat paw swelling, suggesting that CK possess an anti-inflammatory effect against acute inflammation.
Inflammatory process is often accompanied by pain. In this study, the analgesic activity of CK was evaluated on pain threshold, acetic acid-induced writhing response, and carrageenan-induced mechanical hyperalgesia. Hot plate test is a classical method for pain threshold measurement, widely used to evaluate central analgesic activities of drugs (Shajib et al. 2018; Hishe et al. 2018). The acetic acid-induced writhing response test and carrageenan-induced mechanical hyperalgesia test are classical methods widely used to evaluate peripheral analgesic activities of drugs, which are affected by the release of endogenous mediators, such as histamine, serotonin, bradykinin, and PGs, that are involved in both proinflammatory and peripheral pain mechanisms (Sandes et al. 2018; Mao et al. 2017). Thus, they are sensitive to the action of non-steroidal anti-inflammatory drugs (NSAIDs) (Abdel-Salam 2005; Atta and Abo EL-Sooud 2004). The current study showed that CK exerted analgesic effect against acetic acid-induced writhing response and carrageenan-induced mechanical hyperalgesia, but exhibited no effect on pain threshold. These findings indicated that CK exerted a peripheral analgesic activity, which may be attributed to endogenous mediators.
Analgesic and anti-inflammation activities of substances share many common chemical mediators and mechanisms, and their inhibitions are even concomitant in some cases (Woolf and Max 2001). Carrageenan-induced rat paw oedema is an extensively used model of inflammation and pain, and PGE2 plays a key role in its pathology (Cunha et al. 2005) The intraplantar carrageenan injection also induces mechanical hyperalgesia in mice by triggering a cytokine cascade initiated by TNF-α and CXCL-1 productions, which activates IL-1β-dependent PGE2 production. In turn, PGE2 sensitizes the nociceptor, generating the phenomenon called mechanical hyperalgesia (Cunha et al. 2005; Valério et al. 2007). Furthermore, endothelin-1 (ET-1) mediates carrageenan-induced mechanical hyperalgesia, which is dependent on PGE2 production (Baamonde et al. 2004). Recruited neutrophils also contribute to carrageenan-induced mechanical hyperalgesia by producing PGE2. PGE2 injection into the hind metatarsal foot pad of rats reportedly causes short-term and persistent noxious and mechanical pain (Eldahshan and Abdel-Daim 2015). In this study, CK significantly reduced carrageenan-induced inflammation, increased the pain threshold of rats, and decreased PGE2 level in swollen paw. These findings suggested that the anti-inflammatory and analgesic effects of CK may be attributed to a decrease in PGE2.
COX is a key enzyme in the biosynthetic pathway that leads to the formation of PGs. This enzyme exists mainly in two isoforms, COX-1 and COX-2 (Rajakrishnan et al. 2008). COX-1 is constitutively expressed in many organs, including the kidney, lung, stomach, ileum, colon, and cecum of both rats and humans. The activation of COX-1 is thought to be responsible for producing cytoprotective PGs, such as prostacyclin and PGE2, which are considered critical in maintaining the integrity of gastric mucosa (Williams et al. 1999). COX-1-mediated production of PGs in the stomach serves to protect the mucosa against the ulcerogenic effects of acids and other injuries, whereas COX-1-mediated production of thromboxane in the platelets promotes normal blood clotting. COX-2 is not only activated, but also constitutively expressed, and responsible for the release of inflammatory mediator PGE2 during inflammation and in the early hyperalgesic response to tissue injury (Alhouayek and Muccioli 2014). Inhibitions of COX activity and PGE2 generation are the mechanisms of NSAIDs, but COX-induced endogenous PGE2 plays an important physiological role in inhibiting COX activity, resulting in the adverse reactions of NSAIDs, including gastrointestinal damage, adverse cardiovascular reactions, and kidney damage.
CK reportedly reduced the expression levels of COX-2 proteins and inhibited the activation of NF-κB without directly inhibiting COX-1 and COX-2 activities in LPS-induced RAW264.7 cells in vitro (Park et al. 2005). In this study, we determined PGE2 level and COX-1 and COX-2 expressions in swollen paw and gastric mucosa, as well as COX-1 and COX-2 activities in macrophages. Our current results showed that CK decreased PGE2 level and COX-2 expression in swollen rat paw, suggesting that the anti-inflammatory and analgesic effects of CK were related to the decrease in COX-2 expression and PGE2 level. CK exerted no effect on PGE2 level and COX-1 in expression the gastric mucosa, indicating that CK might possess no effect on the physiological function of PGE2 in the gastric mucosa, and exerted no adverse drug reaction, unlike NSAIDs.
CK also reportedly exerted suppressive effects on immune cells, endothelial cells, and fibroblast synovial cells. The mechanisms of these effects may be mediated by different signaling pathways, including glucocorticoid receptors, toll-like receptors, ion channels, NF-κB, and MAPKs. CK inhibited NF-κB activation, reduced nuclear translocation of p65, upregulated IκBα, downregulated p-IκBα (Li et al. 2014), inhibited MAPK activation, and reduced p38, ERK, and JNK phosphorylations (Woolf and Max 2001). However, the main target of CK is still not clear.
Glucocorticoid exerts a broad immunosuppressive effect through various immune cells. The mechanism of these effects is mediated by the glucocorticoid receptors (GR). CK has a steroid ring structure similar to glucocorticoid, and a study has shown that CK combined with GR and induced GR activation (Yang et al. 2008). Our previous study found that CK inhibited T-cell proliferation and CD25 expression, and inhibited the proliferation, migration, and cytokine production of AA fibroblast synoviocytes in adjuvant-induced arthritis rats (Wang et al. 2016); GR antagonists (RU486) could block these effects. These findings suggest that the role of CK in immune regulation and joint protection may be associated with a GR and its receptor-mediated signaling pathway. The target of the anti-inflammatory and analgesic effects of CK still needs to be elucidated in further research.
Conclusion
In summary, the present study showed a therapeutic potential of CK against inflammatory diseases and pain. However, further pharmacological studies are required to clarify the mechanisms responsible for the anti-inflammatory and analgesic effects of CK.
References
Abdel-Salam OM (2005) Anti-inflammatory, antinociceptive, and gastric effects of Hypericum perforatum in rats. Sci World J 5:586–595
Alhouayek M, Muccioli GG (2014) COX-2-derived endocannabinoid metabolites as novel inflammatory mediators. Trends Pharmacol Sci 35:284–292
Alvarez-Soria MA, Herrero-Beaumont G, Moreno-Rubio J, Calvo E, Santillana J, Egido J, Largo R (2008) Long-term NSAID treatment directly decreases COX-2 and mPGES-1 production in the articular cartilage of patients with osteoarthritis. Osteoarthr Cartil 16:1484–1493
Atta AH, Abo EL-Sooud K (2004) The antinociceptive effect of some Egyptian medicinal plant extracts. J Ethnopharmacol 95(2–3):235–238
Baamonde A, Lastra A, Villazón M, Bordallo J, Hidalgo A, Menéndez L (2004) Involvement of endogenous endothelins in thermal and mechanical inflammatory hyperalgesia in mice. Naunyn Schmiedebergs Arch Pharmacol 369:245–251
Chandrasekhar S, Harvey AK, Yu XP, Chambers MG, Oskins JL, Lin C, Seng TW, Thibodeaux SJ, Norman BH, Hughes NE, Schiffler MA, Fisher MJ (2016) Identification and characterization of novel microsomal prostaglandin E synthase-1 inhibitors for analgesia. J Pharmacol Exp Ther 356:635–644
Chen J, Wu H, Wang Q, Chang Y, Liu K, Song S, Yuan P, Fu J, Sun W, Huang Q, Liu L, Wu Y, Zhang Y, Zhou A, Wei W (2014) Ginsenoside metabolite compound k alleviates adjuvant-induced arthritis by suppressing T cell activation. Inflammation 37:1608–1615
Chen J, Wu H, Wang Q, Chang Y, Liu K, Wei W (2015) Ginsenoside metabolite compound K suppresses T-cell priming via modulation of dendritic cell trafficking and costimulatory signals, resulting in alleviation of collagen-induced arthritis. J Pharmacol Exp Ther 353:71–79
Chen J, Wang Q, Wu H, Liu K, Wu Y, Chang Y, Wei W (2016) The ginsenoside metabolite compound K exerts its anti-inflammatory activity by downregulating memory B cell in adjuvant-induced arthritis. Pharm Biol 54(7):1280–1288
Christensen LP (2009) Ginsenosides chemistry, biosynthesis, analysis, and potential health effects. Adv Food Nutr Res 55:1–99
Cunha TM, Verri WA Jr, Silva JS, Poole S, Cunha FQ, Ferreira SH (2005) A cascade of cytokines mediates mechanical inflammatory hypernociception in mice. Proc Natl Acad Sci USA 102:1755–1760
Díaz-Muñoz MD, Osma-García IC, Cacheiro-Llaguno C, Fresno M, Iñiguez MA (2010) Coordinated upregulation of cyclooxygenase-2 and microsomal prostaglandin E synthase 1 transcription by nuclear factor kappa B and early growth response-1 in macrophages. Cell Signal 22(10):1427–1436
Eldahshan OA, Abdel-Daim MM (2015) Phytochemical study, cytotoxic, analgesic, antipyretic and anti-inflammatory activities of strychnos nux-vomica. Cytotechnology 67:831–844
Funk CD (2001) Prostaglandins and leukotrienes: advances in eicosanoid biology. Science 294:1871–1875
Hishe HZ, Ambech TA, Hiben MG, Fanta BS (2018) Anti-nociceptive effect of methanol extract of leaves of Senna singueana in mice. J Ethnopharmacol 217:49–53
Joh EH, Lee IA, Jung IH, Kim DH (2011) Ginsenoside Rb1 and its metabolite compound K inhibit IRAK-1 activation–the key step of inflammation. Biochem Pharmacol 82(3):278–286
Khan MJ, Saraf S, Saraf S (2017) Anti-inflammatory and associated analgesic activities of HPLC standardized alcoholic extract of known ayurvedic plant Schleichera oleosa. J Ethnopharmacol 197:257–265
Li J, Zhong W, Wang W, Hu S, Yuan J, Zhang B, Hu T, Song G (2014) Ginsenoside metabolite compound K promotes recovery of dextran sulfate sodium-induced colitis and inhibits inflammatory responses by suppressing NF-κB activation. PLoS One 9(2):e87810
Liao Z, Milas L (2004) COX-2 and its inhibition as a molecular target in the prevention and treatment of lung cancer. Expert Rev Anticancer Ther 4:543–560
Liu KK, Wang QT, Yang SM, Chen JY, Wu HX, Wei W (2014) Ginsenoside compound K suppresses the abnormal activation of T lymphocytes in mice with collagen-induced arthritis. Acta Pharmacol Sin 35:599–612
Mao Q, Shi L, Wang ZG, Luo YH, Wang YY, Li X, Lu M, Ju JM, Xu JD, Kong M, Zhou SS, Shen MQ, Li SL (2017) Chemical profiles and pharmacological activities of Chang-Kang-Fang, a multi-herb Chinese medicinal formula, for treating irritable bowel syndrome. J Ethnopharmacol 201:123–135
Park EK, Shin YW, Lee HU, Kim SS, Lee YC, Lee BY, Kim DH (2005) Inhibitory effect of ginsenoside Rb1 and compound K on NO and prostaglandin E2 biosyntheses of RAW264.7 cells induced by lipopolysaccharide. Biol Pharm Bull 28(4):652–656
Rajakrishnan V, Manoj VR, Subba Rao G (2008) Computer-aided, rational design of a potent and selective small peptide inhibitor of cyclooxygenase 2 (COX2). J Biomol Struct Dyn 25:535–542
Sandes S, Heimfarth L, Brito RG, Santos PL, Gouveia DN, Carvalho A, Quintans JSS, da Silva-Júnior EF, de Aquino TM (2018) Evidence for the involvement of TNF-α, IL-1β and IL-10 in the antinociceptive and anti-inflammatory effects of indole-3-guanyl hydrazone hydrochloride, an aromatic aminoguanidine, in rodents. Chem Biol Interact 286:1–10
Shajib MS, Rashid RB, Ming LC, Islam S, Sarker M, Moklesur R, Nahar L, Sarker SD, Datta BK, Rashid MA (2018) Polymethoxyflavones from Nicotiana plumbaginifolia (Solanaceae) exert antinociceptive and neuropharmacological effects in mice. Front Pharmacol 9:85
Valério DA, Cunha TM, Arakawa NS, Lemos HP, Da Costa FB, Parada CA, Ferreira SH, Cunha FQ, Verri WA Jr (2007) Anti-inflammatory and analgesic effects of the sesquiterpene lactone budlein A in mice: inhibition of cytokine production-dependent mechanism. Eur J Pharmacol 562:155–163
Wang Y, Chen J, Luo X, Zhang Y, Si M, Wu H, Yan C, Wei W (2016) Ginsenoside metabolite compound K exerts joint-protective effect by interfering with synoviocyte function mediated by TNF-α and Tumor necrosis factor receptor type 2. Eur J Pharmacol 771:48–55
Williams CS, Mann M, DuBois RN (1999) The role of cyclooxygenases in inflammation, cancer, and development. Oncogene 18:7908–7916
Woolf CJ, Max MB (2001) Mechanism-based pain diagnosis: issues for analgesic drug development. Anesthesiology 95:241–249
Wu H, Chen J, Wang Q, Jia X, Song S, Yuan P, Liu K, Liu L, Zhang Y, Zhou A, Wei W (2014) Ginsenoside metabolite compound K attenuates inflammatory responses of adjuvant-induced arthritis rats. Immunopharmacol Immunotoxicol 36:124–129
Yang CS, Ko SR, Cho BG, Shin DM, Yuk JM, Li S, Kim JM, Evans RM, Jung JS, Song DK, Jo EK (2008) The ginsenoside metabolite compound K, a novel agonist of glucocorticoid receptor, induces tolerance to endotoxin-induced lethal shock. J Cell Mol Med 12(5A):1739–1753
Zheng S, Wang Q, He Q, Song X, Ye D, Gao F, Jin S, Lian Q (2011) Novel biphasic role of Lipoxin A (4) on expression of cyclooxygenase-2 in lipopolysaccharide-stimulated lung fibroblasts. Mediat Inflamm 2011:745340
Acknowledgements
This work was financially supported by the National Natural Science Foundation of China (Nos. 81503084, 81330081).
Author information
Authors and Affiliations
Contributions
WW contributed to the design of the study, served as the study coordinator, and helped to review the manuscript. JC designed the study, performed the experiments, collected the data and wrote the manuscript. MS, YW, LL, YZ, AZ helped perform the experiments and interpret the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Chen, J., Si, M., Wang, Y. et al. Ginsenoside metabolite compound K exerts anti-inflammatory and analgesic effects via downregulating COX2. Inflammopharmacol 27, 157–166 (2019). https://doi.org/10.1007/s10787-018-0504-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-018-0504-y