Abstract
Previous studies have investigated the cardiovascular activity of Gynura procumbens Merr. single-solvent extracts. The objective of this study was to evaluate the in vitro vasorelaxant properties and the underlying pharmacological mechanisms of serial extracts and fractions of Gynura procumbens (GP). The leaves of GP were serially extracted with petroleum ether, chloroform, methanol and water using the maceration method. Suspended aortic ring preparations were pre-contracted with phenylephrine (PE 1 µM), followed by cumulative addition of GP extracts (0.25–3 mg/mL). The petroleum ether extract (GPPE) was the most potent among the four extracts. Pre-incubation of endothelium-intact aorta with atropine (1 µM), indomethacin (10 µM), methylene blue (10 µM), propranolol (1 µM) and potassium channel blockers such as TEA (1 µM), glibenclamide (10 µM), 4-aminopyridine (1 µM) and barium chloride (10 mM) had no effect on GPPE-induced vasorelaxation. The vasorelaxant effect of GPPE was partly diminished by pretreatment of aortic rings preparations with l-NAME (10 µM) and even more so in endothelium-denuded aortic rings, indicating a minimal involvement of endothelium-dependent pathway in GPPE-induced vasorelaxation. The calcium-induced vasocontractions were antagonized significantly and concentration-dependently by GPPE in calcium free and high potassium medium. These results illustrate that Ca2+ antagonizing actions of GPPE in rat isolated aorta are comparable to that of verapamil and may be mainly responsible for its vasodilation effect. The antioxidant activity of GPPE supports its vasorelaxant effect by attenuating the production of deleterious free radicals and reactive oxygen species in the vasculature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With a preference for traditional medicines by most rural communities in developing countries and the high cost of conventional medical treatment, it is no surprise that the importance of folkloric medicine has gained profound acceptance and is being considered in primary health-care systems as alternative forms of therapy (Benzi and Ceci 1997; WHO 1998). In the context of global disease burden, cardiovascular diseases (CVDs) remain the leading cause of mortality in the world (De Reuck 2010; Kannan and Janardhanan 2014; Lackland et al. 2016). The prevalence of cardiovascular diseases in developing countries is steadily approaching that of developed and industrialized nations (Fuster and Kelly 2010). Agents that can act to modulate arterial wall structure and function in addition to lower blood pressure may lead to a novel approach in the prevention of cardiovascular morbidities.
Gynura procumbens Merr. (GP; Compositae) is an important medicinal plant in Southeast Asia. This tropical herbaceous plant produces purple tubular bisexual flowers, highly branched with hairy green leaves which are arranged alternately on hairy purple stem (Keng et al. 2009). G. procumbens has been used as a herbal remedy for diseases such as diabetes, hypertension, urinary infection, inflammation and allergy (Jiratchariyakul et al. 2000; Bohari et al. 2006). The leaf extracts of G. procumbens has been reported to reduce the high serum cholesterol and triglyceride levels in diabetic rats (Akowuah et al. 2002). The medicinal potency of G. procumbens in the management of cardiovascular-related complications has been well established by previous studies (Abrika et al. 2013; Hoe et al. 2007; Kaur et al. 2012, 2013). While these cited studies can be referred to with regard to its cardiovascular effect, the findings are limited to the overall physiological effect with little emphasis on investigating the putative dynamics of its pharmacological modulation of the vascular system. The extraction method used in these studies focused on the polar constituents, thus shunning the identification of potential non-polar bioactive constituents. Moreover, no tentative effort in identifying the latent constituents underlying the observed effect has been done. In view of these limitations, the current research was conducted to investigate the possible mechanism of action of the active portion of the extract and to also make attempts at identifying the vasoactive moieties within the cocktail of constituents in the extract using an in vitro aorta ring experimental approach.
Materials and methods
Plant material and preparation of crude extract
Fresh green leaves of G. procumbens were collected from the Agricultural Center, Penang. The plant was identified at the Herbarium, School of Biological Sciences, Universiti Sains Malaysia (voucher specimen 10833). The powdered leaves were successively extracted by a maceration process at 45 °C in a water bath, with solvents of ascending polarities to obtain four different solvent extracts, namely petroleum ether (GPPE), chloroform (GPCL), methanol (GPME) and water (GPWE) extract. All the extracts were concentrated by a rotary evaporator (Buchi, Switzerland). The concentrated extracts were dried, and the yields were calculated.
Chemicals and drugs
Atropine sulfate, acetylcholine chloride (ACh), indomethacin, glibenclamide, phenylephrine hydrochloride (PE), methylene blue, propranolol hydrochloride, l-NAME, verapamil chloride and chemicals for antioxidant assays were purchased from Sigma-Aldrich (Germany). Other chemicals and reagents used were of analytical grade.
Study design and experimental animals
Adult male Sprague–Dawley (SD) rats weighing 250–300 g, were obtained from the Animal Research and Service Centre (ARASC), Universiti Sains Malaysia. The rats were fed normal commercial rat chow (Gold Coin Feed Mills Sdn. Bhd., Malaysia) and water ad libitum. All procedures on animals were carried out with the consent of the Animal Ethics Committee, USM [Animal ethics approval number: USM/Animal Ethics Approval/2015/(h 96)/(670)].
Preparation of rat thoracic aorta rings
Rats were euthanized with carbon dioxide gas in a chamber. The chest was opened by a midline incision from the neck region down to the abdominal cavity to expose the thoracic aorta. The aorta was removed gently and placed in a Petri dish containing Krebs’s physiological solution (KPS) aerated with carbogen gas (95% oxygen and 5% carbon dioxide). The surrounding fat and connective tissue on the aorta tissue was carefully removed, and the cleaned tissue was cut into 3–5 mm-long rings. Aortic rings were suspended horizontally in tissue chambers containing 10 mL KPS. The KPS in the tissue chamber was continuously aerated with carbogen at 37 °C. Suspended aortic rings were equilibrated at a resting tension of 1.0 g for 40 min. The tension was adjusted to 1.0 g if needed throughout the experiment. The KPS in the tissue chamber was replaced every 15 min. Before the protocol was started, contractile responsiveness of the aortic rings was tested by exposure to phenylephrine (PE, 1 µM). Responses were recorded via a force displacement transducer connected to the Power Lab (Ameer et al. 2010; Idris et al. 2015). In all aortic ring experimental protocols, the concentrations represent the final tissue chamber concentration (containing 10 mL KPS).
Pharmacological studies
Vasorelaxation by G. procumbens extracts
After the initial equilibration of the suspended aortic rings, rise in tension (contraction) was induced with phenylephrine (PE 1 µM) until a stable plateau is attained. This is followed by cumulative additions of the four solvent extracts (at a concentration of 0.25, 0.5, 1, 2 and 3 mg/mL in 100 µL) to assess the vasodilation effects of the extracts. A similar protocol was repeated for each solvent extract at the same concentrations. Each experiment was conducted on six to eight aortic ring preparations for statistical analysis. The changes in tension after addition of the extract (at each concentration point) were recorded and the relative vasodilation induced by the extracts (% relaxation) was calculated with the formula below:
where Tc represents the change in resting tension after contraction with PE (1 µM) and Tt represents the change in resting tension after addition of the extract/fraction.
Vasorelaxation mechanism of G. procumbens petroleum ether extract (GPPE)
The most potent of the four solvent extracts was subjected to further assessment. The mechanism study was conducted to examine the role of different intrinsic regulatory pathways on petroleum ether extract (GPPE)-induced vascular relaxation. In the experimental setup, known concentrations of the antagonistic agents were added to the tissue chamber 20 min before the addition of PE (1 µM) and the relaxations induced by GPPE was measured in their presence. The relaxation effect of GPPE on the aortic rings in the absence of the antagonist(s) served as control before pre-incubation of the aortic rings with the antagonist. In experiments requiring endothelium-denuded aortic rings, the endothelium was removed by gentle rubbing of the intimal surface of the aortic rings with a blunted gauge 18 needle, and denudation of endothelium was confirmed by complete lack of relaxations to ACh (1 µM) of rings pre-contracted with PE (1 µM) (Bello et al. 2015).
Involvement of endothelium-dependent pathways
To study the possible involvement of muscarinic receptor, endothelium-derived nitric oxide (EDNO) and prostacyclin (PGI2) pathways, suspended endothelium-intact aortic rings were pre-incubated with atropine (1 µM), a competitive non-selective muscarinic receptor antagonist, l-NG-nitroarginine methyl ester (l-NAME, 10 µM), a nonspecific NOS inhibitor, and indomethacin (10 µM), a non-selective cyclooxygenase inhibitor, respectively, followed by contraction with PE (1 µM). Cumulative concentrations of the extract (0.25–3) were added to the pre-contracted rings and the relaxation effect of the extract in the presence and absence (control) of the antagonists was compared.
Effect of potassium channel blockers
The involvement of potassium channels (K-channels) in the relaxation mechanism of GPPE was assessed on suspended endothelium-denuded aortic rings pre-incubated with different K channel antagonists: tetraethyl ammonium chloride (TEA 10 µM, a non-selective potassium channel blocker), glibenclamide (1 µM, a selective ATP-sensitive potassium channel blocker), 4-aminopyridine (1 µM, voltage-dependent potassium channel inhibitor) and barium chloride (10 µM, inward rectifier potassium (Kir) channel inhibitor).
Involvement of β-adrenergic receptors
To observe the possible participation β-adrenergic receptor activity, relaxations to GPPE (0.25–3 mg/mL) were constructed on endothelium-denuded aortic rings pre-incubated with propranolol (1 µM), a non-selective β-adrenergic receptor blocker, in aortic rings pre-contracted with PE (1 µM).
Inhibition of extracellular influx through L-type Ca2+ channel
To study the role of L-type calcium channels in the relaxation mechanism of the extract solution, denuded aortic rings were stabilized in normal Krebs’s solution for 1 h, which was then replaced with Ca2+ -free Krebs’s solution containing a chelating agent, ethylenediaminetetraacetic acid (EDTA 0.1 mM) for 30 min to remove Ca2+ from the tissue. This solution was then replaced with K+-rich and Ca2+-free Krebs’s solution devoid of EDTA. Following an incubation period of 30 min, the effects of cumulative additions of Ca2+ (1.00E−4 to 3.00E−2 M) to the tissue bath were recorded for 3 min for each concentration before and following tissue incubation (20 min) with three different concentrations of verapamil (0.1, 0.3 and 1 µM) and in another set of experiments with three different concentrations of GPPE (0.5, 1 and 2 mg/mL).
GC–MS analysis preparation and chromatographic condition
GPPE and its fractions (1 mg/mL) were used for gas chromatography–mass spectrometry (GC–MS) analysis. The analysis was carried out on GCMS Agilent 6890N/59731 (Network GC system). Interpretation on mass spectrum of GC–MS was done using the database of the National Institute Standard and Technology (NIST 02). The percentage of the identified constituent was computed using total ion chromatogram.
Antioxidant assays
The antioxidant assays were performed using all the extracts of G. procumbens at 10 mg/mL concentration. All determinations were prepared in triplicate. Absorbance was calculated by Lab-System Multiscan MS microplate reader (Model No. 354; Helsinki, Finland).
Total phenolic content
Total phenolic contents were estimated using Folin–Ciocalteu assay using gallic acid as reference standard (Kumaran and Karunakaran 2006). In this assay, Folin–Ciocalteu reagent, sodium carbonate, standard test samples and distilled water were mixed in a test tube in a ratio of 5:15:1:79 in a total volume of 200 μL. After incubation of 2 h at room temperature, the absorbance at 765 nm of each test sample was recorded. The phenolic content was calculated as μg gallic acid equivalent/mg of dry extract (Tan and Lim 2015).
Total flavonoid content
Aluminum chloride method was used to calculate the total flavonoid content using quercetin as a reference standard (Orhan et al. 2011). The extract and standard solution (100 μL) were mixed with 20 μL (10%, w/v) aluminum chloride, 20 μL of 1 mol/L sodium acetate, 300 μL methanol and 560 μL distilled water. Then, 30 min after incubation at room temperature, the absorbance was calculated at 415 nm. Then results were shown as μg quercetin equivalent/mg dry extract.
DPPH assay
DPPH radical scavenging activity was estimated using the method described by Wang et al. (2007). A known concentration of the test samples was prepared in MeOH:H2O (1:1) and then an aliquot of 100 μL of the sample solution was added to 100 μL of DPPH (200 μmol/L prepared in methanol). The mixed solution was incubated at room temperature for 30 min. Morin and ascorbic acid were used as reference standards. The amount of remaining DPPH was determined at 517 nm. The results were reported as EC50, the concentration at which the scavenging activity is 50%.
ABTS radical scavenging assay
ABTS radical scavenging activity was measured as described by Re et al. (1999). ABTS radical cation (ABTS+) solution was prepared by mixing 14 mmol/L ABTS and 4.9 mmol/L potassium persulfate solutions in equal volumes. The solution was kept in dark at room temperature for 16–20 h to start the reaction. Then, 1 mL of the solution was diluted with 40 mL de-ionized water to yield working ABTS solution with an absorbance of 0.70 ± 0.02 at 734 nm. To 180 μL of ABTS working solution, 20 μL test samples (six concentrations) was added. The absorbance of the samples was interpreted at 734 nm after 6 min. Ascorbic acid was used as reference standards (Re et al. 1999). The results are shown as EC50, which is the concentration at which the scavenging activity is 50%.
Ferric reducing antioxidant power (FRAP) assay
The FRAP assay was performed by the method of Benzie and Strain (1996). Each test sample (50 μL) was added to FRAP working solution (150 μL; contains 300 mmol/L acetate buffer, pH 3.6, 10 mmol/L TPTZ in 40 mmol/L HCl and 20 mmol/L FeCl3 in a ratio of 10:1:1). The reaction mixtures were incubated for 8 min and the absorbance was measured at 600 nm. Ferrous sulfate (FeSO4·7H2O) was used as reference standard. The results were shown as nmol Fe2+ equivalent/μg dry extract.
Statistical analyses and data presentation
All values were given as mean ± SEM and n indicates the number of determinations performed for each experiment. The data were analyzed using two-way ANOVA, followed by Dunnett post hoc test. Probability values (p values) of less than 5% (p < 0.05) are considered significant when compared with control experiments. p values are expressed as #p < 0.001, **p < 0.01 and *p < 0.05.
Results
Vasorelaxation effect of the G. procumbens extracts
Addition of PE (1 µM) induced a sustained contraction in the isolated aortic ring preparations. It was observed that with cumulative addition of GP extracts to the tissue chamber, there was concentration-dependent reduction in the PE contractions. G. procumbens petroleum ether extract (GPPE) was the most potent vasorelaxant among the four extracts with a maximum relaxation (Rmax) of 89.4 ± 5.8%, followed by chloroform extract with 64.7 ± 5.4%. Methanol extract gave a mild relaxation of 15.7 ± 13.2%. In contrast, cumulative addition of water extract rather increases the tonic contraction of the aortic rings (Rmax = − 31.0 ± 5.8%) (Fig. 1a).
Concentration-dependent vascular effects of a extracts of Gynura procumbens (0.25–3 mg/mL) and b fractions of Gynura procumbens petroleum ether extract (0.25–3 mg/mL) on rat aortic rings pre-contracted with PE. Contractions are expressed as percentage of the initial contraction induced by PE (1 µM). Results are expressed as mean ± SEM (n = 8)
Liquid–liquid fractionation of GPPE gave two fractions: the acetone-soluble and -insoluble fractions (AF and AIF), of which AF was more active in the vasodilation of aortic rings. Compared to its fractions, GPPE showed more potent vasorelaxant activity (Fig. 1b).
Vasorelaxation mechanism of GPPE
The following experiments were conducted to explore the underlying pharmacological mechanisms of GPPE.
Involvement of endothelium-dependent pathways
Removal of the endothelium caused a rightward shift (decrease) in the relaxation curve of GPPE (0.25–3 mg/mL) at a concentration of 1 and 2 mg/mL (p < 0.01–0.05). However, the maximum relaxation (Rmax) was not significantly affected. Similarly, pre-incubation of endothelium-intact aortic rings with l-NAME (10 µM) did mildly inhibit the vasorelaxant effects of GPPE (0.125–3 mg/mL) with a p < 0.05 at 1 mg/mL, but not statistically significant at other concentrations (Fig. 2). Interestingly, pretreatments with atropine (1 µM) and indomethacin (10 µM) caused a statistically significant left shift (increase) in the vasorelaxant responses to GPPE (Fig. 3).
Relaxation effect of Gynura procumbens petroleum ether extract on rat aortic rings with intact endothelium (E+; control) and denuded endothelium (E−) on aortic rings pre-incubated with the NOS inhibitor, l-NAME (10 µM). Values are expressed as mean ± SEM (n = 8) aortic ring experiments. Statistical significance (p value) was measured by two-way ANOVA. *p < (0.05), **p < (0.01) vs control

Effect of atropine (10 µM) and indomethacin (1 µM) on the Gynura procumbens petroleum ether extract (GPPE)-induced relaxation on endothelium-intact aortic rings pre-contracted with phenylephrine (1 µM). Results are expressed as the mean ± SEM of at least eight aortic ring experiments. Statistical significance (p value) was measured by two-way ANOVA. *p < (0.05), **p < (0.01) vs control

Involvement of endothelium-independent pathways
Pretreatments of endothelium-denuded aortic rings with propranolol (1 µM) and methylene blue (10 µM) did not elicit significant effect on GPPE-induced vasorelaxant responses (Fig. 4).
Effect of potassium channel blockers in GPPE-induced relaxation
Denuded aortic rings showed no significant variation in the vasorelaxation effect of GPPE after incubation with various K+ channel blockers, except in glibenclamide pretreated rings at 3.0 mg/mL (p < 0.05, Fig. 5). It is obvious that K+ channel blockers do not have any major influence on GPPE-induced vasodilatation.
Inhibition of extracellular influx through L-type Ca2+ channel
Pre-incubation of aortic rings with GPPE (0.5, 1 and 2 mg/mL) in high K+- and Ca2+-free Krebs’s solution significantly antagonized the maximum contraction induced by the addition of extracellular CaCl2 (1–5 mol/L) in a concentration-dependent manner (Fig. 6a). In comparison, verapamil also significantly attenuated the CaCl2-induced vasoconstriction (Fig. 6b). These results showed that GPPE-induced vasodilations may be mediated via inhibiting extracellular Ca2+ influx in smooth muscle cells in a manner comparable to verapamil.
Inhibitory effect of a GPPE (0.5, 1 and 2 mg/mL) and b verapamil (0.1, 0.3 and 1 µM) on the contraction–response curves for CaCl2 (1–5 mol/L) determined in Ca2+-free solution containing KCl (80 mM). Results are expressed as the mean ± SEM of eight aorta ring experiments. Statistical significance (p value) was measured by two-way ANOVA. *p < (0.05), **p < (0.01), #p < (0.001) vs control

GC–MS analysis
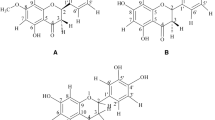
GC–MS analysis of GPPE allowed the identification of volatile components. The compounds with library quality of more than 90% and their concentration (peak area %) are presented in Table 1. Two compounds from the library have been reported to possess vasorelaxant activity: ursolic acid (chromatogram is shown in Fig. 7) and spathulenol (chromatogram is shown in Fig. 8).
Antioxidant assay
The chemical analysis of GPPE is summarized in Table 2.
Discussion
It is evident from the current findings that modulation of blood vessel diameter is involved in the vasodilatory activity of G. procumbens with the petroleum ether extract showing the highest potency.
Further assessment of the vasodilation effect of GPPE on isolated intact aortic ring preparations pre-incubated with atropine (a non-selective muscarinic receptor antagonist) did not antagonize the vasorelaxant properties of GPPE. This observation allowed us to conclude that there is no participation of direct muscarinic receptor activation in the vasorelaxant effect of GPPE (Fukumura et al. 2001; Guedes et al. 2004). The participation of the vasodilator cyclooxygenase (COX) products (prostacyclins, thromboxanes) was also explored in intact aortic ring preparations that were pre-incubated with indomethacin, a non-selective COX inhibitor (Tibiriçá et al. 2007). The inhibition of PE-induced contraction by GPPE was rather augmented by indomethacin pretreatment. It can be deduced that GPPE contains active constituents that neutralize the inhibitory effect of indomethacin while enhancing the activity of COX enzymes (Herrmann et al. 1990).
Kim et al. (2006) investigated the antihypertensive potential of the water extract of GP and postulated a functional involvement of nitric oxide (NO) release in the positive result. This postulation contrasts with our findings where incubation with l-NAME, a competitive inhibitor of NOS, indicates an overall non-significant decrease in GPPE-induced relaxation. It should be noted that the serial extraction technique used in our studies differ from the single extraction approach, which may account for the variant results. Moreover, the previous study was conducted in vivo. Denudation of the endothelium was observed to have minimal effect on the relaxation curve of GPPE. This further confirms the negligible role played by endothelium-derived factors.
The effect of NO on smooth muscle cells is mediated via the activation of the soluble guanylate cyclase–cGMP pathway (Ajay et al. 2003; Tibiriçá et al. 2007). To assess the possible direct activation of the sGC/cGMP pathway by GPPE, endothelium-denuded aortic rings were incubated with methylene blue, a non-selective sGC blocker. According to our results, methylene blue did not block the vasorelaxant properties of GPPE. Similarly, pre-incubation with propranolol (1 µM) and potassium channel blockers, glibenclamide (10 µM), TEA, BaCl2 and 4-AP, did not block the vasorelaxant responses of GPPE.
The contraction of vascular smooth muscle is mediated by an increase in free cytoplasmic Ca2+ level by the opening of voltage-dependent calcium channel (VDCCs) and receptor-operated calcium channels (ROCCs) located on cell membranes (Thorneloe and Nelson 2005; Xiong and Sperelakis 1995). These channels might be activated by high extracellular K+ for VDCC and PE for ROCC, but by different pathways (Karaki et al. 1997; Meisheri et al. 1981; Somlyo and Somlyo 1994). GPPE was observed to exert a significant (p < 0.001) inhibitory effect against the attainment of maximum contraction by aortic rings in a Ca2+-free depolarized medium upon the addition of CaCl2. Verapamil, a classical L-type VDCC blocker, displayed similar inhibitory effect on CaCl2-induced contraction. This suggests that GPPE appears to bring about relaxation of the vascular smooth muscle (VSM) by blocking the Ca2+ channels of the VSM in a similar pattern to verapamil. Similar finding is reported by Hoe et al. (2011).
Intrinsic production of free radicals and reactive oxygen species (ROS) plays a pivotal role in the pathophysiology of many diseases. Studies have shown that vascular cells, including endothelial cells, smooth muscle cells, adventitial fibroblasts and resident macrophages, produce ROS (Maxwell and Lip 1997). These deleterious molecules disrupt the functional integrity of the vasculature and can cause vascular injury, leading to atherosclerosis and other forms of CVDs. Chemical analysis of GPPE showed the presence of considerable amounts of polyphenolic and flavonoid constituents having potential free radical scavenging and antioxidant actions. It can be postulated that the antioxidant activity of GPPE further augments its vascular function.
According to GC–MS reports of GPPE as shown in Table 1, ursolic acid, spathulenol, vitamin E, squalene and phytols are present. Phenols, phytol and alkaloids obtained from therapeutic plants possess antihypertensive and vasorelaxant activities (Maione et al. 2013). Squalene fully blocked the effects of squalestatin or simvastatin on homocysteine-induced endothelial dysfunction. These suggestions explain that the mevalonate pathway mediates homocysteine-induced dysfunction of endothelium as well the oxidative pathway. Interference in the mevalonate pathway and oxidative pathway provides effective protection of endothelial function (Zhang et al. 2012). The vitamin E supplement of 200 IU/day is effective in hypertensive patients in the long term, maybe due to nitric oxide (Boshtam et al. 2002). Ursolic acid has many pharmacological activities including vasorelaxant effect in endothelium-intact rat aorta rings, through release of NO to vascular smooth muscle (Luna-Vázquez et al. 2016). Spathulenol has been isolated and is a possible smooth muscle relaxant agent (Akter et al. 2016; Perez-Hernandez et al. 2009).
In this context, researches are in progress to deliver new data to clarify the precise mechanism. Yet, there is need for further investigations. The presence of various bioactive compounds and their therapeutic properties justify the use of whole plants for various ailments by traditional healers. The identification of compounds is based on GC–MS library match, which is not sufficient for a tentative conclusion; thus, further detailed chemical analyses are suggested in future studies.
Conclusions
The vasorelaxant effect of GPPE was mainly mediated through a direct effect on the arterial smooth muscle and mildly through the endothelium. These results showed that Ca2+ channels blockade on smooth muscle cells was mainly responsible for the vasodilatation effect of GPPE. The calcium-induced vasoconstrictions were antagonized by GPPE concentration dependently. This study conclusively demonstrates that the leaves of G. procumbens may contain active principles that have vasorelaxant effect in in vitro studies. We consider that the vasodilator effect could be related to the presence of ursolic acid, vitamin E, spathulenol and polyphenolic or flavonoid constituents.
References
Abrika OSS et al (2013) Effects of extracts and fractions of Gynura procumbens on rat atrial contraction. J Acupunct Meridian Stud 6:199–207
Ajay M, Gilani AU, Mustafa MR (2003) Effects of flavonoids on vascular smooth muscle of the isolated rat thoracic aorta. Life Sci 74:603–612
Akowuah G, Sadikun A, Mariam A (2002) Flavonoid identification and hypoglycaemic studies of the butanol fraction from Gynura procumbens. Pharm Biol 40:405–410
Akpuaka A, Ekwenchi MM, Dashak DA, Dildar A (2013) Biological activities of characterized isolates of n-Hexane extract of Azadirachta Indica A.Juss (Neem) leaves. Nat Sci 11(5):141–147
Akter K et al (2016) Phytochemical profile and antibacterial and antioxidant activities of medicinal plants used by aboriginal people of New South Wales, Australia. Evid Based Complement Altern Med eCAM 2016:4683059
Alok P, Suneetha V (2014) Punica granatum (Pomegranate) rind extract as a potent substitute for LAscorbic acid with respect to the antioxidant activity. RJPBCS 5:597
Ameer OZ et al (2010) Pharmacological mechanisms underlying the vascular activities of Loranthus ferrugineus Roxb. in rat thoracic aorta. J Ethnopharmacol 127:19–25
Awad AB, Chan KC, Downie AC, Fink CS (2000) Peanuts as a source of beta-sitosterol, a sterol with anticancer properties. Nutrition Cancer 36:238–241
Bello I, Usman NS, Mahmud R, Asmawi MZ (2015) Mechanisms underlying the antihypertensive effect of Alstonia scholaris. J Ethnopharmacol 175:422–431
Benzi G, Ceci A (1997) Herbal medicines in European regulation. Pharm Res 35:355–362
Benzie IF, Strain J (1996) The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: the FRAP assay. Anal Biochem 239:70–76
Bohari M et al (2006) Glucose uptake: stimulatory activity of Gynura procumbens in 3T3-F442A adipocytes, Malaysian medicinal plant: chemistry and biological activity. UNIMAS and Malaysian Natural Products Society, Sarawak
Boshtam M, Rafiei M, Sadeghi K, Sarraf-Zadegan N (2002) Vitamin E can reduce blood pressure in mild hypertensives. Int J Vitam Nutr Res 72:309–314
De Reuck J (2010) Stroke characteristics in patients with pretreated arterial hypertension. Eur Neurol 64:355–359
Elena S, Kagan V, Han D, Packer L (1991) Free radical recycling and intramembrane mobility in the antioxidant properties of alpha-tocopherol and alpha-tocotrienol. Free Radical Biol Med 10:263–275
Fukumura D et al (2001) Predominant role of endothelial nitric oxide synthase in vascular endothelial growth factor-induced angiogenesis and vascular permeability. Proc Natl Acad Sci 98:2604–2609
Fuster V, Kelly BB (2010) Promoting cardiovascular health in the developing world: a critical challenge to achieve global health. National Academies Press, Washington
Guedes DN, Silva D, Barbosa-Filho J, De Medeiros IA (2004) Endothelium-dependent hypotensive and vasorelaxant effects of the essential oil from aerial parts of Menthax villosa in rats. Phytomedicine 11:490–497
Herrmann F, Lindemann A, Gauss J, Mertelsmann R (1990) Cytokine-stimulation of prostaglandin synthesis from endogenous and exogenous arachidonic acids in polymorphonuclear leukocytes involving activation and new synthesis of cyclooxygenase. Eur J Immunol 20:2513–2516
Hoe SZ, Kamaruddin MY, Lam SK (2007) Inhibition of angiotensin-converting enzyme activity by a partially purified fraction of Gynura procumbens in spontaneously hypertensive rats. Med Princ Pract Int J Kuwait Univ Health Sci Cent 16:203–208
Hoe SZ et al (2011) Gynura procumbens Merr. decreases blood pressure in rats by vasodilatation via inhibition of calcium channels. Clinics 66:143–150
Idris B et al (2015) Antihypertensive and vasorelaxant effect of Alstonia scholaris stem bark extracts and fractions. Int J Pharmacol 11:327–334
Jiratchariyakul W et al (2000) Antiherpes simplex viral compounds from Gynura procumbens Merr. Mahidol University Annual Research, Salaya
Kaliyan B et al (2016) Chemical analysis of Punica granatum fruit peel and its in vitro and in vivo biological properties. BMC Complementary Alternative Med 16:264
Kannan A, Janardhanan R (2014) Hypertension as a risk factor for heart failure. Curr Hypertens Rep 16:447
Karaki H et al (1997) Calcium movements, distribution, and functions in smooth muscle. Pharmacol Rev 49:157–230
Karunamoorthy K et al (2011) Chemical composition, antimicrobial, antioxidant and anticancer activity of leaves of Syzygium benthamianum (Wight ex Duthie) gamble. JBAPN 1:273–278
Kaur N et al (2012) Cardio-vascular activity of Gynura procumbens Merr. leaf extracts. Int J Pharm Sci Res 3:1393
Kaur N et al (2013) Antihypertensive effect of Gynura procumbens water extract in spontaneously hypertensive rats. Int J Appl Res Nat Prod 6:20–27
Keng CL, Yee LS, Pin PL (2009) Micropropagation of Gynura procumbens (Lour.) Merr. an important medicinal plant. J Med Plants Res 3:105–111
Kim MJ, Lee HJ, Wiryowidagdo S, Kim HK (2006) Antihypertensive effects of Gynura procumbens extract in spontaneously hypertensive rats. J Med Food 9:587–590
Kumaran A, Karunakaran RJ (2006) Antioxidant and free radical scavenging activity of an aqueous extract of Coleus aromaticus. Food Chem 97:109–114
Kumari STK, Muthukumarasamy S, Mohan VR (2012) GC-MS analysis of ethanol extract of sarcostemma secamone (l) bennet (asclepiadaceae). Sci Res Reporter 2:187–191
Lackland DT, Voeks JH, Boan AD (2016) Hypertension and stroke: an appraisal of the evidence and implications for clinical management. Expert Rev Cardiovasc Ther 14:609–616
Loizou S, Lekakis I, Chrousos GP, Moutsatsou P (2010) β-Sitosterol exhibits anti-inflammatory activity in human aortic endothelial cells. Mol Nutrition Food Res 54:551–558
Luna-Vázquez FJ et al (2016) Role of nitric oxide and hydrogen sulfide in the vasodilator effect of ursolic acid and uvaol from black cherry Prunus serotina fruits. Molecules 21:78
Maione F et al (2013) Phenols, alkaloids and terpenes from medicinal plants with antihypertensive and vasorelaxant activities. A review of natural products as leads to potential therapeutic agents. Nat Prod Commun 8:539–544
Mallikadevi TSP, Jamuna S, Karthikka K (2012) Analysis for phytoceuticals and bioinformatics approach for the evaluation of therapetic properties of whole plant methanolic extract of Mukia maderaspatana (l.) m.Roem. (cucurbitaceae)—a traditional medicinal plant in western districts of Tamil Nadu, India. Asian J Pharm Clin Res 5(4):163–168
Maxwell SR, Lip GY (1997) Free radicals and antioxidants in cardiovascular disease. Br J Clin Pharmacol 44:307–317
Meisheri KD, Hwang O, van Breemen C (1981) Evidence for two separate Ca2+ pathways in smooth muscle plasmalemma. J Membr Biol 59:19–25
Orhan N, Orhan IE, Ergun F (2011) Insights into cholinesterase inhibitory and antioxidant activities of five Juniperus species. Food Chem Toxicol 49:2305–2312
Perez-Hernandez N et al (2009) Structure–activity relationships of aromadendranes in uterus-relaxant activity. Zeitschrift fur Naturforschung C J Biosci 64:840–846
Re R et al (1999) Antioxidant activity applying an improved ABTS radical cation decolorization assay. Free Radic Biol Med 26:1231–1237
Samuel ES et al (2012) Antihypertensive effect of Lepechinia caulescens extract on spontaneously hypertensive rats. Phytopharmacology 2:170–178
Sheela D, Uthayakumari F (2013) GC-MS analysis of bioactive constituents from coastal sand dune taxon–sesuvium portulacastrum (l.). Biosci Discovery 4: 47–53
Somlyo AP, Somlyo AV (1994) Signal transduction and regulation in smooth muscle. Nature 372:231–236
Tan JBL, Lim YY (2015) Critical analysis of current methods for assessing the in vitro antioxidant and antibacterial activity of plant extracts. Food Chem 172:814–822
Thorneloe KS, Nelson MT (2005) Ion channels in smooth muscle: regulators of intracellular calcium and contractility. Can J Physiol Pharmacol 83:215–242
Tibiriçá E et al (2007) Pharmacological mechanisms involved in the vasodilator effects of extracts from Echinodorus grandiflorus. J Ethnopharmacol 111:50–55
Wang K-J, Yang C-R, Zhang Y-J (2007) Phenolic antioxidants from Chinese toon (fresh young leaves and shoots of Toona sinensis). Food Chem 101:365–371
WHO (1998) Guidelines for the appropriate use of herbal medicines, WHO. WHO Regional Publications. Western Pacific Series; No. 23, p 88
Xiong Z, Sperelakis N (1995) Regulation of L-type calcium channels of vascular smooth muscle cells. J Mol Cell Cardiol 27:75–91
Zhang B, Qiu L, Fu M, Hu S (2012) Interference in mevalonate pathway ameliorates homocysteine-induced endothelium-dysfunction. Eur J Pharmacol 692:61–68
Acknowledgements
This research was funded by the Malaysian Ministry of High Education (MOHE) with a grant provided to Professor Mohd Zaini Bin Asmawi (Grant no. 203/PFARMASI/6711451). We thank Mr. Roseli Hassan and Mr. Selva for their kind assistance during this study. We also acknowledge the Institute of Postgraduate Studies (IPS), USM, Penang, Malaysia, for the USM fellowship award to the first author, Ref. P-FD0019/12(R).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Iqbal, Z., Bello, I., Asmawi, M.Z. et al. Vasorelaxant activities and the underlying pharmacological mechanisms of Gynura procumbens Merr. leaf extracts on rat thoracic aorta. Inflammopharmacol 27, 421–431 (2019). https://doi.org/10.1007/s10787-017-0422-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-017-0422-4