Abstract
Diabetic neuropathy (DN) is characterized as Hyperglycemia activates thdisturbed nerve conduction and progressive chronic pain. Inflammatory mediators, particularly cytokines, have a determinant role in the pathogenesis of neuropathic pain. The activity of adenosine monophosphate protein kinase (AMPK), an energy charge sensor with neuroprotective properties, is decreased in diabetes. It has been reported that activation of AMPK reduces the systemic inflammation through inhibition of cytokines. In this study, we aimed to investigate the probable protective effects of AMPK on DN in a rat of diabetes. DN was induced by injection of streptozotocin (65 mg/kg, i.p.). Motor nerve conduction velocities (MNCV) of the sciatic nerve, as an electrophysiological marker for peripheral nerve damage, were measured. Plasma levels of IL-6, TNF-α, CRP were assessed as relevant markers for inflammatory response. Also, the expression of phosphorylated AMPK (p-AMPK) and non-phosphorylated (non-p-AMPK) was evaluated by western blotting in the dorsal root ganglia. Histopathological assessment was performed to determine the extent of nerve damage in sciatic nerve. Our findings showed that activation of AMPK by metformin (300 mg/kg) significantly increased the MNCV and reduced the levels of inflammatory cytokines. In addition, we showed that administration of metformin increased the expression of p-AMPK as well as decline in the level of non p-AMPK. Our results demonstrated that co-administration of dorsomorphin with metformin reversed the beneficial effects of metformin. In conclusion, the results of this study demonstrated that the activation of AMPK signaling pathway in diabetic neuropathy might be associated with the anti-inflammatory response.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In diabetic neuropathy (DN), demyelination and neuron damage lead to disturbance in nerve conduction (Tracy and Dyck 2008). Nerve conduction study is a noninvasive procedure to measure the nerve function which clinically used for evaluation of neuropathy in patients (Vinik et al. 2006). Reduce motor nerve conduction velocity (MNCV) is described as an indicator of diabetic neuropathy (Yorek et al. 1993).
Previous studies have indicated that tumour necrosis factor-α (TNF-α) plays a key role in the pathophysiology of chronic pain (Zhang et al. 2013). In this regard, it has been shown that levels of inflammatory cytokines increased in the blood of diabetic patients (Gonzalez-Clemente et al. 2005; Uceyler et al. 2007). It is well accepted that the levels of C-reactive protein (CRP) as well as interleukin (IL)-6 increased in the circulation of patients with diabetes which are directly associated with diabetic neuropathy (Hills and Brunskill 2009). Previous studies demonstrated that metformin was able to prevent from the development of neuropathy in diabetic patients (Knowler et al. 2002; Valk et al. 2002).
Ample evidence has determined that activation of adenosine monophosphate protein kinase (AMPK) is the main mechanism of action of metformin in the correction of metabolic syndrome in diabetes (Zhou et al. 2001). Studies have shown that AMPK activity reduced in diabetes (Lee et al. 2007). It is well established that antihyperglycemic effects of metformin are mediated through AMPK stimulation (Cho et al. 2015). AMPK activation decreases the blood glucose level through attenuation of glucose uptake (McGee et al. 2008) and inhibition of gluconeogenesis (Novikova et al. 2015). However, it is shown that metformin diminished gluconeogenesis in an AMPK-independent pathway in a mouse model of diabetes (Foretz et al. 2010).
Steinberg et al. showed that inflammatory cytokines via increase the expression of protein phosphatase 2C (PP2C), an inhibitor of AMPK suppressed the activity of AMPK (Steinberg et al. 2006). It is shown that metformin, an AMPK activator, reduced the systemic inflammation in mild metabolic syndrome (Akbar 2003). Dorsomorphin (Compound C), an AMPK inhibitor, is a known tool for investigating the role of AMPK in biological processes (Novikova et al. 2015; Liu et al. 2014; Kimura et al. 2014).
Previous studies demonstrated the positive effects of metformin in diabetic neuropathy; however, the exact mechanisms of this agent are unclear. In this study, we aimed to examine the anti-inflammatory and protective effects of activation of AMPK signaling pathway using metformin on the diabetes-induced neuropathy considering blood glucose level, inflammatory markers and MNCV in a rat diabetic model. We demonstrated that AMPK signaling loop at least partially modulated the anti-inflammatory and protective effects of metformin in the DN.
Materials and methods
Materials
Chemicals used in this study consisted of: Streptozotocin (Sigma-Aldrich, USA), metformin and dorsomorphin dihydrochloride (Compound C) (Tocris Bioscience, USA), CRP ELISA kit, IL-6 ELISA kits and TNF-α ELISA kit (Abcam, USA), antibody Thr_172 and PP2C_α (Santa Cruz, CA).
Methods
Subjects and study design
Eighty male Wistar rats (obtained from Department of Pharmacology, School of Medical, Tehran University of Medical Sciences, Tehran, Iran) weighing 210 ± 10 g were used. In order to induction of diabetes, a single injection of streptozotocin (STZ) at the dose of 65 mg/kg, intraperitoneally (i.p.) was used. 24 h before administration of STZ, animals were deprived of food. The Ethics Committee approved all the ethical guidelines of experimental pain in awaked animals (Zimmermann 1983).
Animals randomly assigned into eight groups as follows (n = 10 in each group): (1) saline; (2) STZ; (3) metformin (300 mg/kg); (4) STZ + metformin (300 mg/kg); (5) dorsomorphin (0.2 mg/kg); (6) STZ + dorsomorphin (0.2 mg/kg); (7) metformin (300 mg/kg) + dorsomorphin (0.2 mg/kg); (8) STZ + metformin (300 mg/kg) + dorsomorphin (0.2 mg/kg).
Blood samples were taken from the tail, and glucose levels were measured 48 h after STZ administration. Blood glucose ≥400 mg/dl was considered as diabetic. We wanted to activate the AMPK with an effective dose of metformin. So based on the previous studies, we picked up the dose of 300 mg/kg (Wang et al. 2009; Zhuo et al. 2013). Metformin (AMPK activator) was used in 1 ml of drinking water directly conducted into the stomach by oral gavage, and dorsomorphin (AMPK inhibitor) was used as i.p. injection from 3 days after induction of diabetes until the end of the study. The blood glucose levels were measured using glucometer (Optium Plus, Abbott Diabetes Care, UK) on 7 days before induction of diabetes and 4, 18, 32 and 45 days after induction of diabetes. We selected the 7th day before induction of DN to take blood samples to minimize handling effects and also diminish stress-induced inflammatory reactions.
Electrophysiological experiments
MNCV was determined using a non-invasive procedure in the sciatic-posterior tibial conducting system in a temperature-controlled environment according to the criteria described by Hasegawa et al. (Hasegawa et al. 2006). Motor nerve studies were performed on day 7 before and days 4, 18, 32 and 45 after induction of diabetes using electrophysiological experiments. Briefly, rats were anesthetized with pentobarbital (70 mg/kg), and the body temperature was maintained at 37 °C, followed by stimulation of the sciatic nerve proximal to the sciatic notch and distal to the knee using bipolar electrodes of a NeuropackΣEMG machine (Nihon Kohden, Japan). The action potential of the muscle was recorded from the ankle using unipolar pin electrodes. MNCV was calculated in meters per second as the ratio of the distance in millimeters between both sites of stimulation divided by the difference between the proximal and distal latencies measured in milliseconds.
Enzyme-linked immunosorbent assays (ELISA)
Blood samples were centrifuged at 3000g for 10 min to separate the serum. Serum samples were stored at −70 °C until the measurement of inflammatory markers including TNF-α, CRP, and IL-6 using ELISA kit according to the manufacturer’s guideline (Saeedi Saravi et al. 2016).
Histological and morphological studies
45 days after diabetes induction, the sciatic nerve was isolated and fixed in 10 % formalin. Then, samples were cut into segments of 5-μm sections using microtome and stained with hematoxylin and eosin. A pathologist, blinded to the study, analyzed the slides using previously established scales for perineural inflammation as follows: 0 = no inflammation, 1 = small focal areas of mild edema and/or cellular infiltrate, 2 = locally extensive areas of moderate edema/cellular infiltrate, 3 = diffuse areas of moderate to marked edema/cellular infiltrate. Evaluation of nerve damage performed as the following: 0 = no lesions, 1 = 0–2 % of the fibers with lesions in axons or myelin, 2 = 2–5 % with lesions, 3 = >5 % with lesions (Brummett et al. 2009).
Western blot procedure
Western blotting was performed according to the protocol described by Eslami et al. (Eslami and Lujan 2010). Briefly, 45 days after diabetes induction, the dorsal root ganglia (DRG) was isolated, and the protein was separated by gel electrophoresis (10 % gel) and transferred to polyvinylidene fluoridated (PVDF) membranes. The PVDF membranes were incubated with primary antibody Thr-172 (phosphorylated AMPK) and PP2C-α (non-phosphorylated AMPK). Subsequently, the membranes were treated with the horseradish peroxidase-conjugated secondary antibodies. Immune complexes were visualized using ECL plus detection reagents.
Statistical analysis
All data presented as Mean ± SEM. One-way ANOVA analysis followed by Tukey’s post hoc test was used for evaluation of blood glucose levels, inflammatory markers, MNCV and Western blotting results. One-way ANOVA analysis followed by Dunnett post hoc test was used for data analysis of histopathological findings. p values less than 0.05 were considered as statistically significant. The sample size was calculated by power calculations using G power software (ver.3.1.7, Franz Faul, Universitat Kiel, Germany). We set α error at 0.05 and power (1 − β) at 0.8 and the required total sample size per group was calculated as 8–10 animals. Accordingly, we selected ten rats in each group.
Results
Metformin decreased blood glucose levels
One-way ANOVA analysis showed that there are significant differences between experimental groups in blood glucose levels on days 4 [F(7, 72) = 161.1, p < 0.001], 18 [F(7, 72) = 172.2, p < 0.001], 32 [F(7, 72) = 310.1, p < 0.001] and 45 [F(7, 72) = 233, p < 0.001].
As shown in Fig. 1, the blood glucose concentrations in STZ (diabetic) groups were significantly increased in comparison with saline (control) groups on days 4, 18, 32 and 45 after diabetes induction. Post hoc test analysis demonstrated that administration of metformin significantly decreased blood glucose levels on days 4, 18, 32 and 45 after induction of diabetes. In addition, administration of dorsomorphin did not decrease blood glucose concentrations in STZ groups. Furthermore, administration of dorsomorphin reversed the effects of metformin on the glucose levels on days 4, 18, 32 and 45 after induction of diabetes. Results showed that there was no significant difference between groups in day 7 before induction of diabetes.
Effect of activation of AMPK on blood glucose levels. Data were expressed as mean ± SEM and analyzed with one-way ANOVA and Tukey’s post hoc test (n = 10). STZ considered as diabetic group. Saline considered as control group. ***p < 0.001 compared to control group, #p < 0.5, ##p < 0.01 and ###p < 0.001 compared to STZ group. STZ streptozotocin, MET metformin, DORS dorsomorphin, MET + DORS metformin + dorsomorphin
Metformin restored MNCV
One-way ANOVA analysis showed that there are significant differences between experimental groups in MNCV on days 18 [F(7, 72) = 36.52, p < 0.001], 32 [F(7, 72) = 245.7, p < 0.001] and 45 [F(7, 72) = 676.5, p < 0.001].
As shown in Fig. 2, there is no significant difference between the groups in day 7 before diabetes induction as well as the 4th day after induction of diabetes in the MNCV (Images of MNCV have been shown as supplementary data). MNCV was significantly decreased in diabetic rats compared to control rats (saline) on days 18, 32 and 45 after induction of diabetes. Moreover, our results showed that administration of metformin increased MNCV in a significant manner in days 18, 32 and 45 after induction of diabetes in comparison with STZ group (Fig. 2).
Effect of activation of AMPK on MNCV. Data were expressed as mean ± SEM and analyzed with one-way ANOVA and Tukey’s post hoc test (n = 10). STZ considered as diabetic group. Saline considered as control group. *p < 0.05 and **p < 0.01 compared to control group, #p < 0.5, ##p < 0.01 and ###p < 0.001 compared to STZ group. STZ streptozotocin, MET metformin, DORS dorsomorphin, MET + DORS metformin + dorsomorphin
Metformin reduced the level of CRP
One-way ANOVA analysis showed that there are significant differences between experimental groups in CRP levels on days 18 [F(7, 72) = 4.518, p < 0.0025], 32 [F(7, 72) = 64.94, p < 0.001] and 45 [F(7, 72) = 187, p < 0.001].
Figure 3 shows the results of CRP assessment. As shown, the level of CRP significantly increased in the serum of diabetic animals as compared to control (saline) groups on days 45 after induction of diabetes in rats. Results showed that metformin reduced the concentration of CRP in the serum of diabetic rats on days 18, 32 and 45 after induction of diabetes when compared to STZ group. However, administrations of dorsomorphin alone or with metformin have not effected on CRP levels. Metformin failed to change the level of CRP on day 4 after induction of diabetes as well as day 7 before administration of STZ.
Effect of activation of AMPK on CRP. Data were expressed as mean ± SEM and analyzed with one-way ANOVA and Tukey’s post hoc test (n = 10). STZ considered as diabetic group. Saline considered as control group. **p < 0.01 and ***p < 0.001 compared to control group, #p < 0.5 and ##p < 0.01 compared to STZ group. STZ streptozotocin, MET metformin, DORS dorsomorphin, MET + DORS metformin + dorsomorphin
Metformin reduced the level of IL-6
One-way ANOVA analysis showed that there are significant differences between experimental groups in levels of IL-6 on days 18 [F(7, 72) = 39.73, p < 0.001], 32 [F(7, 72) = 21.52, p < 0.001] and 45 [F(7, 72) = 51.79, p < 0.001].
Analysis showed that the level of IL-6 significantly increased in diabetic rats in comparison with control ones on days 18, 32 and 45 after induction of diabetes. Post-test analysis demonstrated that unlike days 7 before and 4 after induction of diabetes, metformin on days 18, 32 and 45 after STZ administration reduced the levels of IL-6 when compared to STZ rats. Furthermore, our findings showed that co-administration of metformin with dorsomorphin in day 18 after diabetes induction decreased the IL-6 levels in comparison with STZ group (Fig. 4).
Effect of activation of AMPK on IL_6. Data were expressed as mean ± SEM and analyzed with one-way ANOVA and Tukey’s post hoc test (n = 10). STZ considered as diabetic group. Saline considered as control group. ***p < 0.001 compared to control group, #p < 0.5 and ###p < 0.001 compared to STZ group. STZ streptozotocin, MET metformin, DORS dorsomorphin, MET + DORS metformin + dorsomorphin
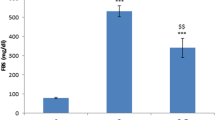
Metformin reduced the level of TNF-α
One-way ANOVA analysis showed that there are significant differences between experimental groups in levels of TNF-α on days 18 [F(7, 72) = 19.1, p < 0.001], 32 [F(7, 72) = 88.43, p < 0.001] and 45 [F(7, 72) = 198.8, p < 0.001].
ANOVA analysis showed that the level of TNF-α significantly increased in diabetic rats in comparison with control (saline) animals on days 18, 32 and 45 after STZ administration. Post hoc test analysis showed that unlike days 7 before and 4 after administration of STZ, metformin on days 18, 32 and 45 after STZ administration significantly reduced the levels of TNF-α in serum samples when compared to diabetic groups (Fig. 5). In addition, co-administration of metformin with dorsomorphin on day 18 after diabetes induction significantly decreased TNF-α in comparison with STZ group.
Effect of activation of AMPK on TNF_α. Data were expressed as mean ± SEM and analyzed with one-way ANOVA and Tukey’s post hoc test (n = 10). STZ considered as diabetic group. Saline considered as control group. ***p < 0.001 compared to control group, #p < 0.5 and ##p < 0.01 compared to STZ group. STZ streptozotocin, MET metformin, DORS dorsomorphin, MET + DORS metformin + dorsomorphin
Activation of AMPK decreases the perineural inflammation
Histological and morphological evaluations on sciatic nerve are shown in Fig. 6. Our findings showed that there are no signs of inflammation or morphological changes in the sciatic nerve among groups in control (saline) animals. Moreover, histopathological observations showed that there was extensive perineural inflammation around the sciatic nerve in STZ, dorsomorphin as well as metformin plus dorsomorphin in diabetic groups (score = 3). Also, the histopathological study demonstrated a low level of inflammation ratio around the sciatic nerve in diabetic rats treated with metformin (score = 1). Moreover, nerve damage was not observed in sciatic nerve of all groups.
a Histological and morphological studies in sciatic nerve at 45 days after diabetes induction. In untreated diabetic rats (B), the sciatic nerve has diffuse areas of moderate to marked edema/cellular infiltrate. In the metformin-treated diabetic rats (D), the finding is small focal areas of mild edema and/or cellular infiltrate. In the dorsomorphin-treated diabetic rats (F) and metformin plus dorsomorphin-treated diabetic rats (H), the sciatic nerves has diffuse areas of moderate to marked edema/cellular infiltrate. b Scoring of sciatic nerves for the presence of inflammation. A saline, B STZ, C metformin, D STZ + metformin, E dorsomorphin, F STZ + dorsomorphin, G metformin + dorsomorphin, H STZ + metformin + dorsomorphin. #p < 0.5, ##p < 0.01 and ###p < 0.01 compared to STZ group
Metformin increased p-AMPK in DRG
To evaluate the expression of AMPK in phosphorylated and non-phosphorylated forms in DRG samples, western blotting was used. Western blotting experiment showed that the level of phosphorylated AMPK (Thr-172) increased in diabetic group treated with metformin when compared to the diabetic group. Results showed that levels of non-phosphorylated AMPK (PP2C_α) increased in STZ (diabetic) group. Additionally, the level of PP2C_α increased in diabetic rats treated with metformin plus dorsomorphin (Fig. 7).
a Effects of treated with or without metformin (MET) or dorsomorphin (DORS) alone, or MET plus DORS at indicated doses on the levels of phosphorylated (Thr172) and non-phosphorylated (PP2C-α) activity of AMPK in dorsal root ganglia of control and experimental rats. b Graphical representation of data from Western blotting analysis. A saline, B STZ, C metformin, D STZ + metformin, E dorsomorphin, F STZ + dorsomorphin, G metformin + dorsomorphin, H STZ + metformin + dorsomorphin. #p < 0.5, ##p < 0.01 and ###p < 0.01 compared to STZ group
Discussion
In the current study, diabetes was induced by the administration of STZ. Using metformin, an AMPK activator, and dorsomorphin, an AMPK inhibitor we evaluated the protective effects of AMPK signaling pathway in the diabetic neuropathy. We showed that the activation of AMPK significantly increased the MNCV and decreased the levels of inflammatory parameters such as TNF-α, IL-6, and CRP in diabetic rats. Administration of metformin notably decreased glucose levels when compared to untreated diabetic rats. Our results showed that treatment with dorsomorphin did not decrease blood glucose levels in diabetic rats, and also co-administration of dorsomorphin with metformin reversed the beneficial effects of metformin on blood glucose concentration, inflammatory cytokines, and MNCV. Furthermore, we evaluated the expression of AMPK in phosphorylated (p-AMPK) and non-phosphorylated forms in DRG samples. Findings demonstrated that metformin increased the level of p-AMPK which was decreased in diabetes. These results were in agreement with our histological observations.
It is well established that hyperglycemia is associated with over-production of inflammatory cytokines, nerve conduction impairment as well as mitochondrial dysfunction which consequently lead to the damage of sensory neurons in DRG of the spinal cord (Bordet et al. 2008; Leinninger et al. 2006). Streptozotocin is a selective agent used to destroy the islets of Langerhans and employ to induce experimental DN in animal models (Jin et al. 2009). The beneficial effects of metformin (AMPK activator) are mediated through action on the hepatocytes and muscle cells, as well as reduced glucose production and increased glucose uptake (Cheng et al. 2006). Dorsomorphin is an AMPK inhibitor which reverses the beneficial effects of AMPK signaling pathway on the glucose levels (Kimura et al. 2014).
Ample evidence reported that metformin via activation of AMPK decreases the blood glucose levels in diabetes (Zakikhani et al. 2008). Metformin acts as a neuroprotective agent. In this regard, it has been shown that metformin in neurodegenerative diseases possessed neuroprotective effects (Correia et al. 2008; Ullah et al. 2012).
Previous studies have determined that the activity of AMPK signaling cascade decreased in diabetes (Roy Chowdhury et al. 2012). Clinical studies have shown that there is an indirect association between the activity of AMPK pathway with the incidence of neuropathy in diabetic patients (Gerich et al. 2005). It is documented that the activation of AMPK signaling pathway ameliorated the inflammatory reactions in diabetes (Gaskin et al. 2007; Ido et al. 2002). Hyperglycemia activates the NF-κB signaling pathway, subsequently leading to the production of inflammatory mediators such as IL-6, CRP, and TNF-α resulting in nerve damage and development of neuropathy (Takeuchi et al. 2010; Wada and Yagihashi 2005). In line with aforementioned studies, our results showed that inflammatory reaction decreased the following administration of metformin in which levels of IL-6, CRP and TNF-α decreased when compared to the untreated diabetic rats.
Several lines of evidence have shown that diabetic patients have electrophysiological conduction abnormalities indicating peripheral neuropathy (Zangiabadi et al. 2007). In this context, it is determined that progressive slowing of motor nerve conduction velocity (MNCV) is an important complication related to the neuropathy (Coste et al. 2004). In agreement with previously published study demonstrated that diabetes led to decrease in conduction speed of sciatic nerve we showed that MNCV decreased in diabetic rats which significantly reversed following metformin treatment (Coste et al. 2004).
According to previous researches, metformin repaired sciatic nerve degeneration in diabetic rats. Pathomorphological assessment indicated that metformin regenerated sciatic nerve damage consequent of diabetes (Ma et al. 2015). In the current study, we observed that the activation of AMPK signaling pathway using metformin notably improved histopathological alterations in the DRG samples of diabetic rats.
It is well accepted that protein phosphatase 2C (PP2C) is a dephosphorylate enzyme which inactivates p-AMPK (Wang and Unger 2005; Wu et al. 2007). Considering phosphorylation form of AMPK is the active form which is reduced in diabetes, agents capable of decreasing the PP2C has potential positive effect in diabetes. Our western blotting finding showed that metformin significantly increased the expression of p-AMPK as well as decreased the expression of PP2C in DRG samples of diabetic rats. Previous studies have been shown gender differences in pain sensitivity in rodents. Different response to painful stimuli in male and female rats attributed to biological systems and physiological factors such as sex hormones and pathway of brain μ-receptors activation (Fillingim and Maixner 1995; Wiesenfeld-Hallin 2005). Boyer et al. showed that male rats exhibited greater analgesia in response to morphine application into rostral ventromedial medulla (Boyer et al. 1998). Considering the influence of hormonal and genetic difference between female rats in pain perception, in this study we used only male rats. The authors suggested that additional study may be worthwhile to perform in female rat.
Conclusion
In conclusion, results of the present work showed that anti-inflammatory effects of AMPK signaling pathway improved the complications of diabetes in experimental diabetes. Our results showed that activation of AMPK signaling decreased glucose levels, attenuated inflammatory markers (such as IL-6, CRP, and TNF-α), increased MNCV of the sciatic nerve and also improved histopathological scores of sciatic nerves.
References
Akbar DH (2003) Effect of metformin and sulfonylurea on C-reactive protein level in well-controlled type 2 diabetics with metabolic syndrome. Endocrine 20:215–218. doi:10.1385/endo:20:3:215
Bordet T et al (2008) Specific antinociceptive activity of cholest-4-en-3-one, oxime (TRO19622) in experimental models of painful diabetic and chemotherapy-induced neuropathy. J Pharmacol Exp Ther 326:623–632. doi:10.1124/jpet.108.139410
Boyer JS, Morgan MM, Craft RM (1998) Microinjection of morphine into the rostral ventromedial medulla produces greater antinociception in male compared to female rats. Brain Res 796:315–318. doi:10.1016/S0006-8993(98)00353-9
Brummett CM, Padda AK, Amodeo FS, Welch KB, Lydic R (2009) Perineural dexmedetomidine added to ropivacaine causes a dose-dependent increase in the duration of thermal antinociception in sciatic nerve block in rat. Anesthesiology 111:1111–1119. doi:10.1097/ALN.0b013e3181bbcc26
Cheng JT, Huang CC, Liu IM, Tzeng TF, Chang CJ (2006) Novel mechanism for plasma glucose-lowering action of metformin in streptozotocin-induced diabetic rats. Diabetes 55:819–825. doi:10.2337/diabetes.55.03.06.db05-0934
Cho K et al (2015) Antihyperglycemic mechanism of metformin occurs via the AMPK/LXR [agr]/POMC pathway. Sci Rep 5:8145. doi:10.1038/srep08145
Correia S et al (2008) Metformin protects the brain against the oxidative imbalance promoted by type 2 diabetes. Med Chem [Shariqah (United Arab Emirates)] 4:358–364. doi:10.2174/157340608784872299
Coste T, Gerbi A, Vague P, Maixent J, Pieroni G, Raccah D (2004) Peripheral diabetic neuropathy and polyunsaturated fatty acid supplementations: natural sources or biotechnological needs? Cell Mol Biol (Noisy-le-Grand, France) 50:845–853. doi:10.1070/T578
Eslami A, Lujan J (2010) Western blotting: sample preparation to detection. J Vis Exp JoVE. doi:10.3791/2359
Fillingim RB, Maixner W (1995) Gender differences in the responses to noxious stimuli. Pain Forum 4:209–221. doi:10.1016/S1082-3174(11)80022-X
Foretz M et al (2010) Metformin inhibits hepatic gluconeogenesis in mice independently of the LKB1/AMPK pathway via a decrease in hepatic energy state. J Clin Investig 120:2355–2369. doi:10.1172/jci40671
Gaskin FS, Kamada K, Yusof M, Korthuis RJ (2007) 5′-AMP-activated protein kinase activation prevents postischemic leukocyte-endothelial cell adhesive interactions. Am J Physiol Heart Circ Physiol 292:H326–H332. doi:10.1152/ajpheart.00744.2006
Gerich J, Raskin P, Jean-Louis L, Purkayastha D, Baron MA (2005) PRESERVE-beta: two-year efficacy and safety of initial combination therapy with nateglinide or glyburide plus metformin. Diabetes Care 28:2093–2099. doi:10.2337/diacare.28.9.2093
Gonzalez-Clemente JM et al (2005) Diabetic neuropathy is associated with activation of the TNF-alpha system in subjects with type 1 diabetes mellitus. Clin Endocrinol 63:525–529. doi:10.1111/j.1365-2265.2005.02376.x
Hasegawa T et al (2006) Amelioration of diabetic peripheral neuropathy by implantation of hematopoietic mononuclear cells in streptozotocin-induced diabetic rats. Exp Neurol 199:274–280. doi:10.1016/j.expneurol.2005.11.001
Hills CE, Brunskill NJ (2009) Cellular and physiological effects of C-peptide. Clin Sci (London, England: 1979) 116:565–574. doi:10.1042/cs20080441
Ido Y, Carling D, Ruderman N (2002) Hyperglycemia-induced apoptosis in human umbilical vein endothelial cells: inhibition by the AMP-activated protein kinase activation. Diabetes 51:159–167. doi:10.2337/diabetes.51.1.159
Jin HY, Liu WJ, Park JH, Baek HS, Park TS (2009) Effect of dipeptidyl peptidase-IV (DPP-IV) inhibitor (Vildagliptin) on peripheral nerves in streptozotocin-induced diabetic rats. Arch Med Res 40:536–544. doi:10.1016/j.arcmed.2009.09.005
Kimura T, Kato E, Machikawa T, Kimura S, Katayama S, Kawabata J (2014) Hydroxylamine enhances glucose uptake in C2C12 skeletal muscle cells through the activation of insulin receptor substrate 1. Biochem Biophys Res Commun 445:6–9. doi:10.1016/j.bbrc.2014.01.039
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403. doi:10.1056/NEJMoa012512
Lee MJ et al (2007) A role for AMP-activated protein kinase in diabetes-induced renal hypertrophy. Am J Physiol Ren Physiol 292:F617–F627. doi:10.1152/ajprenal.00278.2006
Leinninger GM, Edwards JL, Lipshaw MJ, Feldman EL (2006) Mechanisms of disease: mitochondria as new therapeutic targets in diabetic neuropathy. Nat Clin Pract Neurol 2:620–628. doi:10.1038/ncpneuro0320
Liu X, Chhipa RR, Nakano I, Dasgupta B (2014) The AMPK inhibitor compound C is a potent AMPK-independent antiglioma agent. Mol Cancer Ther 13:596–605. doi:10.1158/1535-7163.mct-13-0579
Ma J, Liu J, Yu H, Chen Y, Wang Q, Xiang L (2015) Beneficial effect of metformin on nerve regeneration and functional recovery after sciatic nerve crush injury in diabetic rats. Neurochem Res 1–8. doi:10.1007/s11064-015-1803-y
McGee SL, van Denderen BJ, Howlett KF, Mollica J, Schertzer JD, Kemp BE, Hargreaves M (2008) AMP-activated protein kinase regulates GLUT4 transcription by phosphorylating histone deacetylase 5. Diabetes 57:860–867. doi:10.2337/db07-0843
Novikova DS, Garabadzhiu AV, Melino G, Barlev NA, Tribulovich VG (2015) AMP-activated protein kinase: structure, function, and role in pathological processes. Biochem Biokhimiia 80:127–144. doi:10.1134/s0006297915020017
Roy Chowdhury SK et al (2012) Impaired adenosine monophosphate-activated protein kinase signalling in dorsal root ganglia neurons is linked to mitochondrial dysfunction and peripheral neuropathy in diabetes. Brain J Neurol 135:1751–1766. doi:10.1093/brain/aws097
Saeedi Saravi SS, Hasanvand A, Shahkarami K, Dehpour AR (2016) The protective potential of metformin against acetaminophen-induced hepatotoxicity in BALB/C mice. Pharm Biol 1–8. doi:10.1080/13880209.2016.1185633
Steinberg GR et al (2006) Tumor necrosis factor alpha-induced skeletal muscle insulin resistance involves suppression of AMP-kinase signaling. Cell Metab 4:465–474. doi:10.1016/j.cmet.2006.11.005
Takeuchi M, Takino J, Yamagishi S (2010) Involvement of the toxic AGEs (TAGE)-RAGE system in the pathogenesis of diabetic vascular complications: a novel therapeutic strategy. Curr Drug Targets 11:1468–1482. doi:10.2174/1389450111009011468
Tracy JA, Dyck PJB (2008) The spectrum of diabetic neuropathies physical medicine and rehabilitation clinics of North America 19:1–26. doi:10.1016/j.pmr.2007.10.010
Uceyler N, Rogausch JP, Toyka KV, Sommer C (2007) Differential expression of cytokines in painful and painless neuropathies. Neurology 69:42–49. doi:10.1212/01.wnl.0000265062.92340.a5
Ullah I, Ullah N, Naseer MI, Lee HY, Kim MO (2012) Neuroprotection with metformin and thymoquinone against ethanol-induced apoptotic neurodegeneration in prenatal rat cortical neurons. BMC Neurosci 13:11. doi:10.1186/1471-2202-13-11
Valk GD, Kriegsman DM, Assendelft WJ (2002) Patient education for preventing diabetic foot ulceration a systematic review. Endocrinol Metab Clin N Am 31:633–658. doi:10.1016/S0889-8529(02)00021-X
Vinik AI, Kong X, Megerian JT, Gozani SN (2006) Diabetic nerve conduction abnormalities in the primary care setting. Diabetes Technol Ther 8:654–662. doi:10.1089/dia.2006.8.654
Wada R, Yagihashi S (2005) Role of advanced glycation end products and their receptors in development of diabetic neuropathy. Ann N Y Acad Sci 1043:598–604. doi:10.1196/annals.1338.067
Wang MY, Unger RH (2005) Role of PP2C in cardiac lipid accumulation in obese rodents and its prevention by troglitazone. Am J Physiol Endocrinol Metab 288:E216–E221. doi:10.1152/ajpendo.00004.2004
Wang S, Xu J, Song P, Viollet B, Zou MH (2009) In vivo activation of AMP-activated protein kinase attenuates diabetes-enhanced degradation of GTP cyclohydrolase I. Diabetes 58:1893–1901. doi:10.2337/db09-0267
Wiesenfeld-Hallin Z (2005) Sex differences in pain perception. Gend Med 2:137–145. doi:10.1016/S1550-8579(05)80042-7
Wu Y, Song P, Xu J, Zhang M, Zou M-H (2007) Activation of protein phosphatase 2A by palmitate inhibits AMP-activated protein kinase. J Biol Chem 282:9777–9788. doi:10.1074/jbc.M608310200
Yorek MA et al (1993) Reduced motor nerve conduction velocity and Na (+)-K(+)-ATPase activity in rats maintained on L-fucose diet. Reversal by myo-inositol supplementation. Diabetes 42:1401–1406. doi:10.2337/diab.42.10.1401
Zakikhani M, Dowling RJ, Sonenberg N, Pollak MN (2008) The effects of adiponectin and metformin on prostate and colon neoplasia involve activation of AMP-activated protein kinase. Cancer Prev Res (Philadelphia, Pa) 1:369–375. doi:10.1158/1940-6207.capr-08-0081
Zangiabadi N, Ahrari MN, Nakhaee N (2007) The effect of omega-3 fatty acids on nerve conduction velocity (NCV) and F-wave latency in patients with diabetic polyneuropathy. Am J Pharmacol Toxicol 2:1–3. doi:10.3844/ajptsp.2007.1.3
Zhang H, Zhang H, Dougherty PM (2013) Dynamic effects of TNF-alpha on synaptic transmission in mice over time following sciatic nerve chronic constriction injury. J Neurophysiol 110:1663–1671. doi:10.1152/jn.01088.2012
Zhou G et al (2001) Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Investig 108:1167–1174. doi:10.1172/jci13505
Zhuo XZ et al (2013) Isoproterenol instigates cardiomyocyte apoptosis and heart failure via AMPK inactivation-mediated endoplasmic reticulum stress. Apoptosis Int J Program Cell Death 18:800–810. doi:10.1007/s10495-013-0843-5
Zimmermann M (1983) Ethical guidelines for investigations of experimental pain in conscious animals. Pain 16:109–110. doi:10.1016/0304-3959(83)90201-4
Acknowledgments
This study was conducted with the support of Tehran University of Medical Sciences with Grant Number of 93-02-103-25681.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in the matter related to this article.
Rights and permissions
About this article
Cite this article
Hasanvand, A., Amini-khoei, H., Hadian, MR. et al. Anti-inflammatory effect of AMPK signaling pathway in rat model of diabetic neuropathy. Inflammopharmacol 24, 207–219 (2016). https://doi.org/10.1007/s10787-016-0275-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-016-0275-2