Abstract
Neuropathic pain (NP) is characterized by persistent pain, tactile allodynia, or hyperalgesia. Peripheral nerve injury contributes to rapid progress of inflammatory response and simultaneously generates neuropathic pain. Hydrogen (H2) has anti-inflammation, anti-apoptosis, and anti-oxidative stress effects. Therefore, we hypothesized that H2 treatment could alleviate allodynic and hyperalgesic behaviors and the release of inflammatory factors in rats with neuropathic pain. Peripheral neuropathic pain was established by chronic constriction injury of sciatic nerve in rats. H2 was given twice through intraperitoneal injection at a daily dose of 10 mL/kg during days 1–7 after the operation. Hyperalgesia and allodynia were tested, pro-inflammatory factors of dorsal root ganglia (DRG) and the spinal cord were measured by enzyme-linked immunosorbent assay (ELISA) during days 1–14 after the operation, and heme oxygenase (HO)-1 messenger RNA (mRNA) and protein expression and activities were measured at day 14 after sciatic nerve injury in rats. After Sn (IV) protoporphyrin IX dihydrochloride (SnPP)-IX, hemin, and carbon monoxide-releasing molecule (CORM)-2 had been given for chronic constriction injury (CCI) in rats, the above indicators were assessed. We found that H2 clearly inhibited hyperalgesia and allodynia in neuropathic pain and also attenuated the pro-inflammatory cytokines TNF-α, IL-1β, and high-mobility group box (HMGB) 1. H2 improved HO-1 mRNA and protein expression and activities in the process of pain. SnPP-IX reversed the inhibitory effect of H2 on hyperalgesia and allodynia and on pro-inflammatory cytokines in DRG and the spinal cord. The antinociceptive and anti-inflammatory effects of H2 were involved in the activation of HO-1/CO signaling during neuropathic pain in rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Chronic pain is a widespread and highly debilitating condition caused by personal and social afflictions and is also a public health problem [1]. Neuropathic pain is the most common category of chronic pain. It may be triggered or initiated in the peripheral or central nervous system by a primary lesion or dysfunction and is characterized by persistent pain, tactile allodynia, or hyperalgesia [2, 3]. Because of its elusive cellular and physiopathologic mechanisms, neuropathic pain is difficult to cure, and the strongest painkillers may not be able to completely relieve the patient’s pain.
Peripheral nerve injury contributes to rapid progress of inflammation response and simultaneously generates neuropathic pain and nerve regeneration [4]. Cytokines play a critical role in the initiation and progress of neuropathic pain stimulated by nerve injury [5–7]. Nadeau et al. attested that the messenger RNA (mRNA) and protein expressions of the cytokines IL-1 and TNF were increased in injured mice sciatic nerve; interestingly, nerve function and nociceptive sensitivity were strengthened in IL-1β-, TNF-α-, and IL-1β/TNF-knockout mice after sciatic nerve injury. IL-10, an endogenous and potent anti-inflammatory and antinociceptive cytokine, exhibits anti-allodynic or anti-hyperalgesic effects by inhibiting or neutralizing the expression of the pro-inflammatory cytokines TNF-α and IL-1β [8]. Heme oxygenase (HO)-1 is a rate-limiting enzyme that catalyzes the oxidative degradation of heme into biliverdin, CO, and iron. The expression of HO-1 can exhibit forceful antinociceptive effects [9–12]. In addition to the positive effect of HO-1 on antinociception, the upregulation of the HO-1/CO pathway can also mediate the anti-inflammatory response of IL-10. A better knowledge of these mechanisms can contribute toward the application of potential targets to treat neuropathic pain without interfering with the nerve repair process [4].
Hydrogen has been reported to play a vital therapeutic role in sepsis, multiple organ dysfunction syndrome (MODS), lipopolysaccharide (LPS)-induced acute lung injury (ALI), and chronic pain, among others, through its anti-apoptosis effect, alleviating excessive inflammatory response and oxidative stress [13–18]. This strongly implies that hydrogen (H2) treatment has beneficial and anti-inflammatory effects. Therefore, we hypothesized that H2 treatment could alleviate allodynic and hyperalgesic behaviors and the release of inflammatory factors through a related mechanism in rats with neuropathic pain.
MATERIALS AND METHODS
Drugs and Reagents
Carbon monoxide-releasing molecule 2 (CORM-2) (Sigma-Aldrich, St. Louis, MO), HO-1 inhibitor Sn (IV) protoporphyrin IX dihydrochloride (SnPP-IX) (Frontier Scientific, Lancashire, UK), and hemin (Sanjay Biological, Amritsar, India) were obtained and given as reported in previous studies [3]. The catheter was purchased from Becton Dickinson (Sparks, MD, USA). β-actin primary antibody, HO-1 primary antibody, and secondary antibody (1:5000) were obtained from Abcam (UK). The HO-1 activity kit was from GenMed Scientifics Inc. (Arlington, MA).
Animals
Male Sprague-Dawley rats (180–220 g) were housed with food and water ad libitum under standard conditions (12:12 light/dark cycle) at the Experimental Animal Center of the Academy of Military Medical Sciences. The animals were acclimatized to laboratory conditions for at least 1 week before the experiments. The experimental protocol conformed to the ethical guidelines of Tianjin Medical University and the local ethics committee.
Intrathecal Catheterization
As in previous studies [19], the rats were deeply anesthetized; a PE-10 i.t. catheter was inserted through an incision in the atlantooccipital membrane, which reached the level of the lumbar enlargement. Hemin was injected through the catheter. After the injection, rats were performed to the neuropathic pain model without locomotion deficits.
Induction of Neuropathic Pain
Peripheral neuropathic pain was established by chronic constriction injury of sciatic nerve in rats as described in the method of Bennett and Xie [20], with slight modifications. In brief, the rats were anesthetized by using 10 % chloral hydrate (350 mg/kg intraperitoneally). The fur on the mid-thigh up to the right paw was shaved, and the skin layer was immediately sutured with povidone-iodine solution. The common sciatic nerve of the right hind paw was exposed at the level of the mid-thigh by blunt dissection from the biceps femoris. A 7-mm portion of sciatic nerve was freed from the adhering tissue at the sciatic trifurcation, and four ligatures of 4-0 silk were tied loosely at 1-mm intervals. The right leg was sutured layer by layer. In the sham-operated rats, the same process was done without ligation of the nerve.
Preparation of Hydrogen-Rich Saline
Hydrogen-rich saline was produced according to the method described in our previous reports [13]. Briefly, H2 was dissolved in physiologic saline for 4 h under high pressure (0.4 MPa) until a supersaturated level was reached. The saturated H2 physiologic saline was stored under atmospheric pressure at 4 °C in an aluminum bag without dead volume. To achieve a concentration of 0.6 mmol/L, the hydrogen-rich medium had to be freshly prepared every week. A needle-type hydrogen sensor (Unisense A/S, Aarhus, Denmark) was used to confirm the hydrogen content of the medium according to the method reported by Hayashida et al. [21]. The hydrogen-rich saline was given twice through intraperitoneal injection at a daily dose of 10 mL/kg during days 1–7 after the operation; the physiologic saline was injected in the same manner in control mice.
Experimental Protocol
-
Experiment 1:
A total of 208 rats were randomly divided into four groups (n = 30 per group): sham, sham + H2, chronic constriction injury (CCI), and CCI + H2. Neuropathic pain was induced by chronic constriction injury of sciatic nerve. Cold hypersensitivity, thermal hypersensitivity, and mechanical hypersensitivity were determined before sciatic nerve injury and 1, 4, 7, 10, and 14 days thereafter (n = 8 per group). The cytokines TNF-α, IL-1β, and high-mobility group box 1 (HMGB1) were detected 1, 4, 7, 10, and 14 days after sciatic nerve injury (n = 8 per group per time point).
-
Experiment 2:
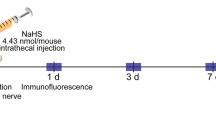
A total of 32 rats were grouped into sham, sham + H2, CCI, and CCI + H2. Another 72 rats were grouped into sham, CCI, CCI + H2, CCI + SnPP, CCI + Hemin, CCI + CORM-2, CCI + H2 + SnPP, CCI + H2 + Hemin, and CCI + H2 + CORM-2. Dorsal root ganglia (DRG) and spinal cord samples were collected for HO-1 mRNA and HO-1 protein expression and activity 14 days after sciatic nerve injury.
-
Experiment 3:
The same nine groups as in experiment 2 were used. Cold hypersensitivity, thermal hypersensitivity, mechanical hypersensitivity, and pro-inflammatory factors were determined 14 days after sciatic nerve injury (n = 8 per group).
Cold Sensitivity
Cold sensitivity of the hind paw was assessed as described in the method of Bennett and Xie [20]. Rats were acclimated for at least 5 min on a copper plate cooled with ice. The number of right hind paw withdrawals from the cold surface over the subsequent 20-min period was quantified.
Mechanical Allodynia
Von Frey filament (Stoelting, North Coast, USA) stimulation and an up-and-down method were used to assess the mechanical allodynia in the hind paw withdrawal response as described in the method of Chaplan et al. [22]. Rats were placed under a wire mesh dome; the filament was presented to the plantar surface until a withdrawal of the foot during or after stimulus.
Thermal Hyperalgesia
Thermal hyperalgesia was measured as previously reported by Bianchi et al. [23]. Each rat was placed on a hot plate to acclimate it to the device, and then the temperature was increased by a heat source under the plantar surface of the hind paw. The time of right hind paw withdrawal latency was regarded as the measurement of thermal hyperalgesia. After the withdrawal latency had been measured, each rat was kept away from the hot plate to prevent tissue damage.
Detection of Inflammatory Cytokines by ELISA
Rats were sacrificed 1, 3, 7, or 14 days after nerve injury for the detection of cytokines. Under deep anesthetization, ipsilateral sciatic nerve and ipsilateral L4–5 spinal cord samples were collected and dissected on ice. These were weighed, homogenized in phosphate-buffered saline (PBS; pH 7.4), and centrifuged at 10,000g at 4 °C for 60 min; the supernatant was collected for subsequent assays. Cytokine detection in sciatic nerve and spinal cord tissue was done by using enzyme-linked immunosorbent assay kits (TNF-α and IL-1β; R&D Systems Inc., Minneapolis, MN; HMGB1; IBL, Hamburg, Germany).
Western Blot
The sciatic nerve and spinal cord samples were homogenized in cold lysis buffer (50 mmol/L Tris-HCl (pH 6.8), 150 mmol/L NaCl, 5 mmol/L EDTA, 0.5 % sodium deoxycholate, 0.5 % NP-40, and protease inhibitor cocktail) and centrifuged at 10,000g for 20 min at 4 °C; the supernatant mixed with the loading buffer was heated at 100 °C for 5 min. The samples were stored at −80 °C until HO-1 assay. The proteins were electrophoresed on 10 % SDS-PAGE gel, transferred to PVDF membranes, blocked in 5 % defatted milk for 1 h, and incubated with HO-1 (1:2000) and β-actin primary antibody (1:4000) at 4 °C overnight. The membranes were then washed and incubated with HRP-conjugate IgG secondary antibody (1:5000) for 1 h at 37 °C. After the membranes had been washed, signals were visualized by ECL and photographed as quantitative in gel by using the Quantity One software (BIO-RAD, Tokyo, Japan). The HO-1 expression was normalized to β-actin.
RT-PCR
After 14 days of experiment, the sciatic nerve and spinal cord samples were collected for detection of HO-1 mRNA expression. Total RNA extraction was done with the RNA TRIzol isolation reagent kit (Invitrogen, USA). Amplification reactions were carried out with the SYBR green polymerase chain reaction (PCR) master mix (Applied Biosystems). Samples were amplified by using the Mastercycler ep realplex2 system (Eppendorf, Hamburg, Germany). The primer sequences were 5′-TGC TCG CAT GAA CAC TCT GGA GAT-3′ (HO-1 forward), 5′-ATG GCA TAA ATT CCC ACT GCC ACG-3′ (HO-1 reverse), 5′-TCA TCA CTA TCG GCA ATG AGC GGT-3′ (β-actin forward), and 5′-ACT CCT GCT TGC TGA TCC ACA TCT-3′ (β-actin reverse).
HO-1 Activity
Sciatic nerve and spinal cord tissues were collected for HO-1 activity determination, which was done by using the HO-1 activity kit according to the manufacturer’s instructions (GenMed Scientifics Inc., Genmed Scientifics, Arlington, MA).
Statistical Analysis
All statistical analyses were done with GraphPad Prism 5 (GraphPad Software, La Jolla, CA), and the results were expressed as mean ± SD. Statistical differences between groups were analyzed with one-way ANOVA, followed by least significant difference t tests for multiple comparisons. Significance was determined at the P < 0.05 level.
RESULTS
Effect of H2 Treatment on Behavioral Reflex Sensitization in Rats with Neuropathic Pain
After sciatic nerve ligation, the rats progressively showed the typical signs of hyperalgesia and allodynia. In our research, we measured cold and thermal hyperalgesia and mechanical allodynia before the operation and 1, 4, 7, 10, and 14 days after CCI. Compared with the sham group, the number of paw lifts (cold hyperalgesia) in the CCI group increased significantly from days 4 to 14 (P < 0.05, n = 8, one-way ANOVA) (Fig. 1a) and attained the peak level on day 10. The withdrawal latency and withdrawal threshold decreased from days 4 to 14 and reached their minimum 10 days after sciatic nerve ligation in the CCI group compared with the sham-operated rats (P < 0.05, n = 8, one-way ANOVA) (Fig. 1b, c). H2 treatment largely reversed the behavioral performance of hyperalgesia and allodynia nerve injury in rats (P < 0.05, n = 8, one-way ANOVA) (Fig. 1a–c). Thus, H2 treatment showed a significant regulatory role in cold and thermal hyperalgesia and mechanical allodynia from 4 to 14 days after CCI, with the peak reached 10 days after nerve injury.
Effect of H2 on cold hypersensitivity, thermal hypersensitivity, and mechanical hypersensitivity induced by sciatic nerve injury in rats. Mechanical anti-allodynic (a), thermal anti-hyperalgesic (b), and thermal anti-allodynic (c) effects of H2 before and 1, 4, 7, 10, and 14 days after sciatic nerve injury. Data are expressed as mean ± SD; a P < 0.05 versus sham, b P < 0.05 versus CCI.
H2 Alleviated the Excessive Release of Pro-inflammatory Cytokines in CCI Rats
IL-1β and TNF-α are early cytokines in the inflammatory response process. In this study, the release of IL-1β and TNF-α in the DRG and spinal cord of nerve-injured rats was significantly increased 1, 4, 7, 10, and 14 days after nerve injury compared with that in sham-operated rats (P < 0.05, n = 8, one-way ANOVA) (Fig. 2a–d). The peak releases were 4 days after injury. HMGB1, regarded as a late inflammatory cytokine, was secreted from necrotic cells, immune cells, or nonimmune parenchymal cells in various pathologic processes [24]. Our results showed an increased expression of HMGB1 both in DRG and the spinal cord from days 4 to 14 in the CCI rat model, with a peak at advanced stages (day 14), compared with sham-operated rats (P < 0.05, n = 8, one-way ANOVA) (Fig. 2e, f). However, there was no significant difference in HMGB1 expression between the sham group and the CCI group 1 day after nerve injury (P > 0.05, n = 8, one-way ANOVA). Regardless of the DRG and spinal cord, H2 treatment significantly attenuated the excessive release of early and late cytokines from days 4 to 14 in CCI rats (P < 0.05, n = 8, one-way ANOVA) (Fig. 2e, f).
Expression of the pro-inflammatory cytokines TNF-α, IL-1β, and HMGB1 1, 4, 7, 10, and 14 days after sciatic nerve injury. After nerve injury, H2 treatment was given for 14 days after CCI. TNF-α (a and b), IL-1β (c and d), and HMGB1 (e and f) were detected by ELISA in DRG (a, c, and e) and the spinal cord (b, d, and e). Data are expressed as mean ± SD; a P < 0.05 versus sham, b P < 0.05 versus CCI.
Effect of H2 on HO-1 Expression and Activity of CCI Rats
We detected the HO-1 mRNA and protein expression and activity 14 days after nerve injury. In contrast with control rats, CCI induced an increase in HO-1 mRNA and protein expression and activity in the DRG and spinal cord (P < 0.05, n = 8, one-way ANOVA) (Fig. 3a–f). As shown in Fig. 3g, compared with the sham group, CCI rats showed an increased expression of HO-1 protein in DRG. The administration of H2 further improved the HO-1 mRNA and protein expression and activity in the CCI + H2 group (P < 0.05, n = 8, one-way ANOVA; Fig. 3a–f).
H2 treatment resulted in increased protein expression and activity changes in DRG and spinal cord 14 days after sciatic nerve injury. HO-1 mRNA was detected by RT-PCR in DRG (a) and spinal cord (b) 14 days after CCI. HO-1 protein expression in DRG (c) and the spinal cord (d) was measured by Western blot and immunofluorescence 14 days after CCI; HO-1 activity was measured in DRG (e) and the spinal cord (f) 14 days after CCI. The immunofluorescence labeling of HO-1 (red) and nuclei (blue) in DRG (g) and the spinal cord (h) is indicated by yellow arrows. Data are expressed as mean ± SD; a P < 0.05 versus sham, b P < 0.05 versus CCI.
To further understand the role of HO-1 in the process of neuropathic pain, we used SnPP-IX, hemin, and CORM-2 in the following experiment. As shown in Fig. 4, SnPP-IX, the active inhibitor of HO-1, inhibited a further increase in HO-1 mRNA and protein expression and activity in the DRG and spinal cord in the CCI + H2 group compared with the CCI + H2 group (P < 0.05; Fig. 4a–d). Hemin (which induces the expression and activity of HO) and CORM-2 (CO-releasing molecule) improved the HO-1 mRNA and protein expression and activity in H2-treated nerve-injured rats. The results showed that SnPP-IX apparently inhibited the effect of H2 on HO-1, whereas hemin and CORM-2 had a synergetic effect on HO-1 in CCI rats.
H2 treatment resulted in increased protein expression and activity changes in DRG and spinal cord at 14 days after sciatic nerve injury. HO-1 mRNA (a), protein expression (b), and HO-1 activity (c) were measured by RT-PCR, Western blot, and HO-1 activity assay kits 14 days after CCI. Data are expressed as mean ± SD; a P < 0.05 versus sham, b P < 0.05 versus CCI, c P < 0.05 versus CCI + H2, d P < 0.05 versus CCI + H2.
SnPP-IX, Hemin, and CORM-2 Attenuated Hyperalgesia and Allodynia in H2-treated CCI Rats
In contrast to the CCI group, the CCI + SnPP group showed an increased number of paw lifts 14 days after nerve ligation (P < 0.05; Fig. 5a); hemin and CORM-2 decreased the number of paw lifts in the CCI + hemin and CCI + CORM-2 groups (P < 0.05, n = 8, one-way ANOVA) (Fig. 5a). Compared with the CCI + H2 group, the CCI + H2 + SnPP group showed an increased number of paw lifts (P < 0.05, n = 8, one-way ANOVA) (Fig. 5a); hemin and CORM-2 enhanced the inhibitory effect of H2 on the number of paw lifts in the CCI + H2 + hemin and CCI + H2 + CORM-2 groups (P < 0.05, n = 8, one-way ANOVA) (Fig. 5a).
Effect of HO-1 on cold hypersensitivity, thermal hypersensitivity, and mechanical hypersensitivity 14 days after H2 treatment of neuropathic pain. Cold hypersensitivity (a), thermal hypersensitivity (b), and mechanical hypersensitivity (c) were measured 14 days after CCI. Data are expressed as mean ± SD; a P < 0.05 versus sham, b P < 0.05 versus CCI, c P < 0.05 versus CCI + H2, d P < 0.05 versus CCI + H2.
SnPP, hemin, and CORM-2 reduced the withdrawal latency and improved the withdrawal threshold of CCI rats (P < 0.05, n = 8, one-way ANOVA) (Fig. 5b, c). SnPP narrowed the withdrawal latency and decreased the withdrawal threshold in the CCI + H2 group compared with the CCI + H2 group (P < 0.05, n = 8, one-way ANOVA) (Fig. 5b, c). Hemin and CORM-2 prolonged the withdrawal latency and increased the withdrawal threshold in the CCI + H2 + hemin and CCI + H2 + CORM-2 groups compared with the CCI + hemin and CCI + CORM-2 groups (P < 0.05, n = 8, one-way ANOVA).
The Regulatory Effect of HO Inhibitor or Inducer on Cytokines in H2-treated CCI Rats
Compared with the CCI group, the release of IL-1β, TNF-α, and HMGB1 in DRG and the spinal cord 14 days after nerve ligation was upregulated in CCI + SnPP rats (P < 0.05, n = 8, one-way ANOVA) (Fig. 6a–f) and downregulated in the CCI + hemin and CCI + CORM-2 groups (P < 0.05 n = 8, one-way ANOVA) (Fig. 6a–f). Regarding the CCI + H2 group, SnPP-IX reversed the inhibitory effect of H2 on the pro-inflammatory cytokines IL-1β, TNF-α, and HMGB1 in DRG and the spinal cord in the CCI + H2 + SnPP group (P < 0.05, n = 8, one-way ANOVA) (Fig. 6a–f); hemin and CORM-2 further boosted the release of IL-1β, TNF-α, and HMGB1 in DRG and the spinal cord in the CCI + H2 + hemin and CCI + H2 + CORM-2 groups (P < 0.05, n = 8, one-way ANOVA) (Fig. 6a–f).
Effect of HO-1 on TNF-α, IL-1β, and HMGB1 expression in DRG and spinal cord 14 days after sciatic nerve injury. After nerve injury, H2, hemin, SnPP, and CORM-2 were given as treatment for 14 days after CCI. TNF-α (a and b), IL-1β (c and d), and HMGB1 (e and f) were detected in DRG (a, c, and e) and the spinal cord (b, d, and e) by ELISA. Data are expressed as mean ± SD; a P < 0.05 versus sham, b P < 0.05 versus CCI, c P < 0.05 versus CCI + H2, d P < 0.05 versus CCI + H2.
DISCUSSION
In the present study, we focused on the effect of HO-1/CO on hyperalgesia and allodynia and on the release of inflammatory cytokines in rats with neuropathic pain treated by H2. First, we showed that H2 suppressed hyperalgesia by thermal hyperalgesia and allodynia through mechanical allodynia, by attenuating the release of the cytokines TNF-α, IL-1β, and HMGB1 in rats with nerve injury. Second, our data indicated that sciatic nerve injury induced an increase in HO-1 mRNA and protein expression and activity and that H2 treatment further promoted a change in HO-1. In addition, H2, hemin, and CORM-2 had a synergistic effect on HO-1 in the process of neuropathic pain. Furthermore, the beneficial effects of H2 on hyperalgesia, allodynia, and inflammatory factors were dependent on the HO-1/CO pathway in rats with neuropathic pain induced by sciatic nerve injury.
Hydrogen has been reported to act as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals in ischemia-reperfusion injury of the brain [14]. Growing research and our previous studies have also shown the protective and preventive effects of H2 in sepsis, MODS, LPS-induced acute lung injury, neuropathic pain, etc., without remarkable side effects, by reducing inflammation response, apoptosis, and oxidative stress [13–18].
In this study, neuropathic pain was induced by chronic constriction of sciatic nerve, which contributed to the development of both hyperalgesia and allodynia. CCI induced mechanical and thermal hypersensitivity, which coincided with pain behaviors. These findings were in agreement with other previously described results [25–27]. Treatment with antioxidants has been reported to significantly alleviate thermal hyperalgesia [28]. In view of the anti-oxidative effect of H2, we also showed that H2 treatment could attenuate mechanical allodynia and hyperalgesia in rats with neuropathic pain.
Growing evidence has suggested that central neuro-immune and neuro-inflammation activation plays a vital role in the generation and maintenance of chronic pain. In the process of chronic neuropathic pain, a nerve injury activates microglia and astrocytes; these cells may be associated with the cascade of neuropathologic events, which initiates at the nerve injury site and proceeds to involve DRG and the spinal cord dorsal horn. Once a nerve is injured, Schwann cells and local macrophages initiate an immune response, releasing pro-inflammatory cytokines and algesic mediators in the spinal cord, such as TNF-α, IL-1β, and IL-6, and thus propagating the inflammatory response over time, which further aggravates central sensitization, hyperalgesia, and allodynia [29–31]. TNF-α appears early in the cytokine cascade; it is an early-stage prototype pro-inflammatory factor that has been well verified in peripheral and central sensitization of neuropathic pain and is sufficient to trigger pro-inflammatory events that lead to the development of pain [32, 33]. The sciatic nerve and DRG activation of TNF coincides well with that of pain behaviors, such as hyperalgesia and allodynia [33]. TNF has been reported to be excessively released at 1 day after injury and to remain at a high level until 3 days later. However, in fact, TNF overexpression is delayed and lasts longer [34–36], and the presence of activation has been shown to start from the periphery and then move toward the center [32]. IL-1β, a major pro-inflammatory cytokine, has been found to be upregulated in the injured sciatic nerve, DRG, and spinal cord in various models of neuropathic pain [37–41]. Considerable evidence has verified that IL-1β has an important role in the pain sensitization condition. Inhibition of spinal IL-1β signaling has been found to contribute to alleviating inflammatory pain, neuropathic pain, and cancer pain [42, 43]. Our results showed that sciatic nerve injury induced excessive expression of the pro-inflammatory cytokines TNF-α and IL-1β in DRG and the spinal cord 1 to 14 days after nerve injury. Because TNF-α and IL-1β are considered as early cytokines, we found that the release of TNF-α and IL-1β peaked at day 4 and remained at a high level until 14 days after nerve injury. H2 treatment clearly inhibited the upregulation of TNF-α and IL-1β in the DRG and spinal cord of CCI rats. High-mobility group box 1 (HMGB1) has been identified as a potent inflammatory mediator. Shibasaki et al. showed that nerve injury induced HMGB1 release in the peripheral nerve, which led to the process of pain hypersensitivity [44]. HMGB1 was responsible for pain hypersensitivity in DRG, which contributed to the IL-1β expression in the spinal cord, thereby modulating spinal excitatory synaptic transmission and pain responses [45]; HMGB1 has also been found to activate immunocytes and the release of inflammatory cytokines, such as TNF-α, IL-1β, IL-6, and IL-8, which were associated with hyperalgesia and allodynia in CCI rats [46]. Further, HMGB1 has been indicated to have cross talk with other inflammatory mediators, which may affect the development and maintenance of neuropathic pain. In accordance with these data, our results showed that HMGB1 was expressed at 1 day after nerve injury and was maintained until day 14 of neuropathic pain induced by sciatic nerve injury. H2 treatment clearly inhibited the upregulation of HMGB1 in the DRG and spinal cord of CCI rats.
Heme oxygenase (HO) is a rate-limiting enzyme that can decompose heme into equimolecular quantities of carbon monoxide, iron, and biliverdin. HO includes two genetically distinct isozymes: the inducible HO-1 and the constitutive HO-2. HO-1 upregulation has been associated with an anti-inflammatory and antinociceptive effect in the formalin test [10]. CO, which is produced by HO, has also been found to inhibit inflammatory hyperalgesia in the paw [47]. CORM-2 may be selected to release carbon monoxide [48]. Hervera et al. showed that the administration of CORM-2 attenuated mechanical and thermal hypersensitivity in neuropathic pain stimulated by chronic constriction of sciatic nerve in mice [25]. Also, CORMs generated antinociceptive and anti-inflammatory effects in inflammatory diseases [49].
In line with these results, our findings showed that nerve injury induced HO-1 mRNA and protein expression and activity in rats and that H2 could further increase the HO-1 mRNA and protein expression and activity. SnPP-IX, an HO-1 inhibitor, reversed the facilitation of H2 in HO-1 in pain induced by sciatic nerve injury. CORM-2 and hemin could improve the promoting effect of H2 on HO-1 in rats with neuropathic pain stimulated by chronic constriction of sciatic nerve. SnPP-IX, hemin, and CORM-2 were used to verify the specific mechanism of H2 on behavioristic and inflammatory response during neuropathic pain. Our results revealed that the administration of SnPP-IX blocked the inhibitory effects of H2 on hyperalgesia, allodynia, and the pro-inflammatory factors TNF-α, IL-1β, and HMGB1 in rats with neuropathic pain. H2 could assist hemin or CORM-2 (hemin- or CORM-2-assisted H2) to produce anti-allodynic, anti-hyperalgesic, and anti-inflammatory effects in rats with neuropathic pain induced by sciatic nerve injury.
Our results verified that H2 has an anti-inflammatory effect on neuropathic pain through the HO-1/CO pathway. However, the present study has its limitations. In the research, we discussed only the effect of male rats and measured the HO-1 expression only in DRG and the spinal cord. In future studies, we intend, first, to investigate the effect of H2 on neuropathic pain by using both male and female rats so as to determine any difference between them and the influence of estrogen on neuropathic pain. Second, we will look further into the HO-1 expression in the gliocytes and neurons of CCI rats to study the upstream and downstream of HO-1 so as to clarify how hydrogen exerts anti-inflammatory effects on neuropathic pain through the HO-1/CO pathway. Third, we will investigate cultured gliocytes and neurons to find the underlying mechanisms of H2 in vitro in neuropathic pain.
Our data indicated that H2 treatment clearly inhibited hyperalgesia and allodynia in neuropathic pain and also attenuated the pro-inflammatory cytokines TNF-α, IL-1β, and HMGB1. Similarly to hemin and CORM-2, H2 may be an inducer of HO-1 in the process of pain and could work in synergy with them. The antinociceptive and anti-inflammatory effects of H2 were produced through the activation of HO-1/CO signaling during neuropathic pain in rats. These molecules are potential targets in developing hydrogen treatment for pain.
REFERENCES
Da, S.K., A.F. Paszcuk, G.F. Passos, E.S. Silva, A.F. Bento, and F.C. Meotti. 2011. Activation of cannabinoid receptors by the pentacyclic triterpene alpha, beta-amyrin inhibits inflammatory and neuropathic persistent pain in mice. Pain 152: 1872–87.
Lavertu, G., S.L. Cote, and Y. de Koninck. 2014. Enhancing K-Cl co-transport restores normal spinothalamic sensory coding in a neuropathic pain model. Brain 137: 724–38.
Bijjem, K.R., S.S. Padi, and S.P. Lal. 2013. Pharmacological activation of heme oxygenase (HO)-1/carbon monoxide pathway prevents the development of peripheral neuropathic pain in Wistar rats. Naunyn-Schmiedeberg’s Archives of Pharmacology 386: 79–90.
Nadeau, S., M. Filali, J. Zhang, B.J. Kerr, S. Rivest, D. Soulet, Y. Iwakura, J.P. de Rivero Vaccari, R.W. Keane, and S. Lacroix. 2011. Functional recovery after peripheral nerve injury is dependent on the pro-inflammatory cytokines IL-1beta and TNF: implications for neuropathic pain. Journal of Neuroscience 31: 12533–42.
Watkins, L.R., M.R. Hutchinson, E.D. Milligan, and S.F. Maier. 2007. “Listening” and “talking” to neurons: implications of immune activation for pain control and increasing the efficacy of opioids. Brain Research Reviews 56: 148–69.
Verri, W.J., T.M. Cunha, C.A. Parada, S. Poole, F.Q. Cunha, and S.H. Ferreira. 2006. Hypernociceptive role of cytokines and chemokines: targets for analgesic drug development? Pharmacology and Therapeutics 112: 116–38.
Scholz, J., and C.J. Woolf. 2007. The neuropathic pain triad: neurons, immune cells and glia. Nature Neuroscience 10: 1361–8.
Vale, M.L., J.B. Marques, C.A. Moreira, F.A. Rocha, S.H. Ferreira, S. Poole, F.Q. Cunha, and R.A. Ribeiro. 2003. Antinociceptive effects of interleukin-4, -10, and -13 on the writhing response in mice and zymosan-induced knee joint incapacitation in rats. Journal of Pharmacology and Experimental Therapeutics 304: 102–8.
Fan, W., F. Huang, Z. Wu, X. Zhu, D. Li, and H. He. 2011. Carbon monoxide: a gas that modulates nociception. Journal of Neuroscience Research 89: 802–7.
Rosa, A.O., J. Egea, S. Lorrio, A.I. Rojo, A. Cuadrado, and M.G. Lopez. 2008. Nrf2-mediated haeme oxygenase-1 up-regulation induced by cobalt protoporphyrin has antinociceptive effects against inflammatory pain in the formalin test in mice. Pain 137: 332–9.
Egea, J., A.O. Rosa, S. Lorrio, B.L. Del, A. Cuadrado, and M.G. Lopez. 2009. Haeme oxygenase-1 overexpression via nAChRs and the transcription factor Nrf2 has antinociceptive effects in the formalin test. Pain 146: 75–83.
Maicas, N., M.L. Ferrándiz, I. Devesa, R. Motterlini, M.I. Koenders, W.B. van den Berg, and M.J. Alcaraz. 2010. The CO-releasing molecule CORM-3 protects against articular degradation in the K/BxN serum transfer arthritis model. European Journal of Pharmacology 634: 184–91.
Chen, H.G., K.L. Xie, H.Z. Han, W.N. Wang, D.Q. Liu, G.L. Wang, and Y.H. Yu. 2013. Heme oxygenase-1 mediates the anti-inflammatory effect of molecular hydrogen in LPS-stimulated RAW 264.7 macrophages. International Journal of Surgery 11: 1060–6.
Ohsawa, I., M. Ishikawa, K. Takahashi, M. Watanabe, K. Nishimaki, K. Yamagata, K. Katsura, Y. Katayama, S. Asoh, and S. Ohta. 2007. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nature Medicine 13: 688–94.
Xie, K., W. Fu, W. Xing, A. Li, H. Chen, H. Han, Y. Yu, and G. Wang. 2012. Combination therapy with molecular hydrogen and hyperoxia in a murine model of polymicrobial sepsis. Shock 38: 656–63.
Xie, K., Y. Yu, Y. Pei, L. Hou, S. Chen, L. Xiong, and G. Wang. 2010. Protective effects of hydrogen gas on murine polymicrobial sepsis via reducing oxidative stress and HMGB1 release. Shock 34: 90–7.
Xie, K., Y. Yu, Z. Zhang, W. Liu, Y. Pei, L. Xiong, L. Hou, and G. Wang. 2010. Hydrogen gas improves survival rate and organ damage in zymosan-induced generalized inflammation model. Shock 34: 495–501.
Chen, Q., P. Chen, S. Zhou, X. Yan, J. Zhang, X. Sun, H. Yuan, and W. Yu. 2013. Hydrogen-rich saline attenuated neuropathic pain by reducing oxidative stress. Canadian Journal of Neurological Sciences 40: 857–63.
Bao, Y.H., Q.H. Zhou, R. Chen, H. Xu, L.L. Zeng, X. Zhang, W. Jiang, and D.P. Du. 2014. Gabapentin enhances the morphine anti-nociceptive effect in neuropathic pain via the interleukin-10-heme oxygenase-1 signalling pathway in rats. Journal of Molecular Neuroscience 54: 137–46.
Bennett, G.J., and Y.K. Xie. 1998. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 33: 87–107.
Hayashida, K., M. Sano, I. Ohsawa, K. Shinmura, K. Tamaki, K. Kimura, J. Endo, T. Katayama, A. Kawamura, S. Kohsaka, S. Makino, S. Ohta, S. Ogawa, and K. Fukuda. 2008. Inhalation of hydrogen gas reduces infarct size in the rat model of myocardial ischemia-reperfusion injury. Biochemical and Biophysical Research Communications 373: 30–5.
Chaplan, S.R., F.W. Bach, J.W. Pogrel, J.M. Chung, and T.L. Yaksh. 1994. Quantitative assessment of tactile allodynia in the rat paw. Journal of Neuroscience Methods 53: 55–63.
Bianchi, M., P. Sacerdote, P. Ricciardi-Castagnoli, P. Mantegazza, and A.E. Panerai. 1992. Central effects of tumor necrosis factor alpha and interleukin-1 alpha on nociceptive thresholds and spontaneous locomotor activity. Neuroscience Letters 148: 76–80.
Andersson, U., and K.J. Tracey. 2011. HMGB1 is a therapeutic target for sterile inflammation and infection. Annual Review of Immunology 29: 139–62.
Hervera, A., S. Leanez, R. Motterlini, and O. Pol. 2013. Treatment with carbon monoxide-releasing molecules and an HO-1 inducer enhances the effects and expression of micro-opioid receptors during neuropathic pain. Anesthesiology 118: 1180–97.
Su, L., C. Wang, Y.H. Yu, Y.Y. Ren, K.L. Xie, and G.L. Wang. 2011. Role of TRPM8 in dorsal root ganglion in nerve injury-induced chronic pain. BMC Neuroscience 12: 120.
Kawaguchi, M., Y. Satoh, Y. Otsubo, and T. Kazama. 2014. Molecular hydrogen attenuates neuropathic pain in mice. PLoS One 9: e100352.
Khalil, Z., T. Liu, and R.D. Helme. 1999. Free radicals contribute to the reduction in peripheral vascular responses and the maintenance of thermal hyperalgesia in rats with chronic constriction injury. Pain 79: 31–7.
Zhang, F., X. Feng, R. Dong, H. Wang, J. Liu, W. Li, J. Xu, and B. Yu. 2011. Effects of clonidine on bilateral pain behaviors and inflammatory response in rats under the state of neuropathic pain. Neuroscience Letters 505: 254–9.
DeLeo, J.A., and R.P. Yezierski. 2001. The role of neuroinflammation and neuroimmune activation in persistent pain. Pain 90: 1–6.
Grace, P.M., P.E. Rolan, and M.R. Hutchinson. 2011. Peripheral immune contributions to the maintenance of central glial activation underlying neuropathic pain. Brain, Behavior, and Immunity 25: 1322–32.
Sacerdote, P., S. Franchi, S. Moretti, M. Castelli, P. Procacci, V. Magnaghi, and A.E. Panerai. 2013. Cytokine modulation is necessary for efficacious treatment of experimental neuropathic pain. Journal of Neuroimmune Pharmacology 8: 202–11.
Sacerdote, P., S. Franchi, A.E. Trovato, A.E. Valsecchi, A.E. Panerai, and M. Colleoni. 2008. Transient early expression of TNF-alpha in sciatic nerve and dorsal root ganglia in a mouse model of painful peripheral neuropathy. Neuroscience Letters 436: 210–3.
Muthuraman, A., and N. Singh. 2012. Neuroprotective effect of saponin rich extract of Acorus calamus L. in rat model of chronic constriction injury (CCI) of sciatic nerve-induced neuropathic pain. Journal of Ethnopharmacology 142: 723–31.
Jaggi, A.S., and N. Singh. 2010. Differential effect of spironolactone in chronic constriction injury and vincristine-induced neuropathic pain in rats. European Journal of Pharmacology 648: 102–9.
Kukkar, A., N. Singh, and A.S. Jaggi. 2013. Neuropathic pain-attenuating potential of aliskiren in chronic constriction injury model in rats. Journal of the Renin-Angiotensin-Aldosterone System 14: 116–23.
Kawasaki, Y., Z.Z. Xu, X. Wang, J.Y. Park, Z.Y. Zhuang, P.H. Tan, Y.J. Gao, K. Roy, G. Corfas, E.H. Lo, and R.R. Ji. 2008. Distinct roles of matrix metalloproteases in the early- and late-phase development of neuropathic pain. Nature Medicine 14: 331–6.
Uceyler, N., A. Tscharke, and C. Sommer. 2007. Early cytokine expression in mouse sciatic nerve after chronic constriction nerve injury depends on calpain. Brain, Behavior, and Immunity 21: 553–60.
Perrin, F.E., S. Lacroix, M. Aviles-Trigueros, and S. David. 2005. Involvement of monocyte chemoattractant protein-1, macrophage inflammatory protein-1alpha and interleukin-1beta in Wallerian degeneration. Brain 128: 854–66.
Ruohonen, S., M. Khademi, M. Jagodic, H.S. Taskinen, T. Olsson, and M. Roytta. 2005. Cytokine responses during chronic denervation. Journal of Neuroinflammation 2: 26.
Kawasaki, Y., L. Zhang, J.K. Cheng, and R.R. Ji. 2008. Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. Journal of Neuroscience 28: 5189–94.
Zhang, R.X., A. Li, B. Liu, L. Wang, K. Ren, H. Zhang, B.M. Berman, and L. Lao. 2008. IL-1ra alleviates inflammatory hyperalgesia through preventing phosphorylation of NMDA receptor NR-1 subunit in rats. Pain 135: 232–239.
Milligan, E.D., C. Twining, M. Chacur, J. Biedenkapp, K. O’Connor, S. Poole, K. Tracey, D. Martin, S.F. Maier, and L.R. Watkins. 2003. Spinal glia and proinflammatory cytokines mediate mirror-image neuropathic pain in rats. Journal of Neuroscience 23: 1026–40.
Shibasaki, M., M. Sasaki, M. Miura, K. Mizukoshi, H. Ueno, S. Hashimoto, Y. Tanaka, and F. Amaya. 2010. Induction of high mobility group box-1 in dorsal root ganglion contributes to pain hypersensitivity after peripheral nerve injury. Pain 149: 514–21.
Tong, W., W. Wang, J. Huang, N. Ren, S.X. Wu, and Y.Q. Li. 2010. Spinal high-mobility group box 1 contributes to mechanical allodynia in a rat model of bone cancer pain. Biochemical and Biophysical Research Communications 395: 572–6.
Lawrence, S., L. Willmott, E. Milligan, S. Winch, B. White, and M. Parker. 2012. Autonomy versus futility? Barriers to good clinical practice in end-of-life care: a Queensland case. Medical Journal of Australia 196: 404–5.
Steiner, A.A., L.G. Branco, F.Q. Cunha, and S.H. Ferreira. 2001. Role of the haeme oxygenase/carbon monoxide pathway in mechanical nociceptor hypersensitivity. British Journal of Pharmacology 132: 1673–82.
Motterlini, R., J.E. Clark, R. Foresti, P. Sarathchandra, B.E. Mann, and C.J. Green. 2002. Carbon monoxide-releasing molecules: characterization of biochemical and vascular activities. Circulation Research 90: E17–E24.
Guillen, M.I., J. Megias, V. Clerigues, F. Gomar, and M.J. Alcaraz. 2008. The CO-releasing molecule CORM-2 is a novel regulator of the inflammatory process in osteoarthritic chondrocytes. Rheumatology (Oxford) 47: 1323–8.
ACKNOWLEDGMENTS
This work was supported by the National Natural Science Foundation of China (Nos. 81372033 to Yonghao Yu; 81101409 and 81471842 to KeliangXie) and the Natural Science Foundation of the Tianjin Science Committee (Nos. 13JCQNJC11400 to KeliangXie).
Conflict of Interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yajun Chen, Hongguang Chen and Keliang Xie contributed equally to this work.
ELECTRONIC SUPPLEMENTARY MATERIAL
Below is the link to the electronic supplementary material.
ESM 1
(JPEG 6631 kb)
Rights and permissions
About this article
Cite this article
Chen, Y., Chen, H., Xie, K. et al. H2Treatment Attenuated Pain Behavior and Cytokine Release Through the HO-1/CO Pathway in a Rat Model of Neuropathic Pain. Inflammation 38, 1835–1846 (2015). https://doi.org/10.1007/s10753-015-0161-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-015-0161-x