Summary
Taurolidine, the active agent of Taurolin®, is a broad spectrum anti-biotic that has been used for over 15 years for the treatment of severe surgical infections. Recently, taurolidine has been shown to possess anti-neoplastic properties in vitro and in vivo against a variety of cancers including ovarian, colon and prostate. In this study we assessed the cytotoxic activity of taurolidine against human osteosarcoma (OS) cell lines and normal human bone cells. Treatment with taurolidine inhibited the growth of all ten osteosarcoma cell lines tested and taurolidine was equally potent against cell lines with and without distinct genetic defects (i.e. p53, Rb). Moreover, taurolidine-induced growth inhibition was found to be associated with a dose dependent increase in the number of apoptotic cells and apoptosis was shown to be caspase-dependent. Taurolidine treatment was also found to inhibit adhesion of OS cell lines. Compared to OS cell lines, normal bone cells in primary culture were found to be less sensitive to the cytotoxic and anti-adhesive effects of taurolidine. These data indicate that taurolidine possesses potent anti-neoplastic activity against osteosarcoma cell lines and may have potential as a novel OS chemotherapeutic agent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma (OS) is a highly malignant bone tumor that typically affects children and young adolescents between 10 and 20 years of age. Prior to 1970, surgical amputation was the sole treatment for osteosarcoma and 5 year survival rates were less than 20% [1]. Introduction of multi-agent adjuvant chemotherapy in the early 1980s dramatically improved survival rates and today administration of neo-adjuvant and adjuvant chemotherapy is able to achieve 5 year survival rates up to 70% for patients with non-metastatic disease (reviewed in [2]). Despite this success no further increase in survival has been achieved in over 10 years despite the evaluation of several regimens incorporating various combinations of approved chemotherapeutic agents (i.e. methotrexate, doxorubicin, cisplatin, etoposide, ifosphamide). In addition, patients who relapse following standard chemotherapy have no additional chemotherapeutic options at the present time. The mechanism of action of currently approved chemotherapeutic agents is non-specific and consequently their use is associated with a number of serious side-effects including cardio-toxicity, nephrotoxicity, hearing loss and the development of secondary malignancies. Consequently, the discovery of novel chemotherapeutic agents with lower toxicity and comparable or superior efficacy to current agents is essential for the treatment of OS.
Taurolidine [bis (1,1-dioxoperhydro-1,2,4-thiabiazin-4-yl) methane], the active component of Taurolin®, is a synthetic anti-biotic and anti-fungal agent that has been used for over 15 years for the treatment of severe surgical infections and local wound and bone infections [3–6]. Although the exact mechanism underlying taurolidine’s anti-bacterial and anti-fungal properties has yet to be elucidated, taurolidine’s activity is thought to depend upon the interaction of active methylol breakdown products with cell membrane components [7–9]. In addition to its anti-bacterial, anti-fungal and anti-endotoxin properties taurolidine has also been shown to possess potent anti-neoplastic activity in vitro against a number of tumor cell lines including ovarian, colon, glioma and melanoma [10–13]. Taurolidine treatment was also shown to significantly decrease tumor burden in a murine model of human ovarian carcinoma and in a model of malignant mesothelioma [10, 14]. Intravenous administration of taurolidine in patients with advanced glioblastoma and no further chemotherapeutic options showed partial tumor regression and extended survival time [15]. Taken together, these data suggest that taurolidine has potential as a chemotherapeutic agent for the treatment of patients suffering from diverse types of malignancies. Consequently, we were interested in assessing the potential anti-neoplastic effects of taurolidine on human osteosarcoma cell lines in vitro.
Materials and methods
Cell lines and reagents
Human SAOS-2 (HTB-85), U2OS (HTB-96), HOS and 143B cells were obtained from the American Type Culture Collection (ATCC, Rockville, MD). LM5 cells were provided by E.S. Kleinerman (M.D. Anderson Cancer Center, Houston, TX). Hu09 WT, Hu09 H3 and Hu09 L13 cells were provided by Dr. M. Tani (National Cancer Center Hospital, Tokyo, Japan), MG-63 cells were provided Dr. G. Sarkar (Mayo Clinic, Rochester, MN, USA) and MG-63 M8 cells were provided by Dr. W.T. Zhu (Tongji Hospital, Huazhong University of Science and Technology, Wuhan, China). Normal fibroblasts were obtained from Coriell Cell Repositories (Camden, NJ, USA). All cell lines, with the exception of Hu09 WT, Hu09 H3 and Hu09 L13, were cultured in Dulbecco’s Modified Eagle Medium (4.5 g/l glucose)/Ham F12 (1:1) (Invitrogen, Carlsbad, CA) supplemented with 10% FCS, 1 unit/ml penicillin G, and 1 μg/ml streptomycin. Hu09 WT, Hu09 H3 and Hu09 L13 cells were maintained in RPMI supplemented with 10% FCS, 1 unit/ml penicillin G, and 1 μg/ml streptomycin. All cells were cultured at 37°C in a humidified atmosphere of 5% CO2. The pan caspase inhibitor, Z-VAD-FMK, was purchased from BD Pharmingen (San Diego, CA). Taurolidine was generously provided by Geistlich Pharma, Switzerland. Rat tail collagen type 1 was obtained from Sigma (St. Louis, MO, USA) and DAPI was obtained from Molecular Probes (Eugene, OR, USA).
Normal human bone cell culture
Trabecular bone pieces (0.2–0.5 cm edge length), obtained from surgical waste of patients undergoing total knee arthroplasty, were washed several times with cell culture medium supplemented with penicillin/streptomycin/amphotericin (PSA;1:100, Invitrogen, Carlsbad, CA) until the supernatant was clear and free of fat. Ten to twenty pieces were then plated in a 10 cm dish and medium was changed every second day to remove newly appearing fat for 1 week. After further culture for 1–2 weeks a confluent monolayer of outgrowing cells was obtained (E1). After harvesting by trypsinization cells were expanded and passaged yielding E1P1 and E1P2 cells. A second round of explant (E2) of the same bone pieces yielded E2P1 and E2P2 cells. P1 or P2 cells from E1 or E2 were used for the experiments.
Cytotoxicity assays
Cells were plated in 96-well plates (3,000 cells/well) and allowed to adhere overnight. Various concentrations of taurolidine were added the following day and cells were incubated with taurolidine for either 24 or 72 h. Cytotoxicity was measured by adding 10 μl of WST-1 reagent (Roche, Mannheim, Germany) and incubating for 3 h. WST-1 reagent is a membrane permeable tetrazolium salt that undergoes cleavage via cellular enzymes in intact living cells. The resulting cleavage product is formazan. Thus, a change in the number of viable cells results in a corresponding change in the amount of formazan dye produced. Quantification of formazan dye was determined by measuring dye absorbance with a scanning multiwell spectrophotometer (Bio-Rad, Basel, Switzerland) at 415 nm. Percentage growth inhibition was determined by dividing the absorbance of taurolidine treated cell results by that of control (untreated) cells and multiplying by 100. Statistical differences were determined using the Student’s T-test.
Detection of apoptosis
Apoptosis was assessed using an annexin V-FITC apoptosis detection kit and necrotic cells were determined by Propidium Iodide (PI) staining (BD Pharmingen San Diego, CA). 150,000 cells were plated in each well of a 6-well plate. Cells were allowed to adhere overnight and indicated taurolidine concentrations were added the following day. Twenty-four hours later the cell culture medium was removed and cells were washed 1× with PBS and 1× with annexin binding buffer. Cells were then incubated for 15 min with annexin binding buffer containing annexin-V-FITC and PI. The cells were then washed 1× and visualized using a Nikon Eclipse E600 microscope (Egg, Switzerland) equipped with a 10× objective, a Nikon Y-FL fluorescence illumination with appropriate filters and a Kappa DX20 camera (Kappa opto-electronics GmbH, Gleichen, Germany).
Immunoblotting
Cells (1 × 106) were lysed on ice with lysis buffer containing 50 mM Tris pH 7.5, 150 mM NaCl, 1% NP-40, 0.5% DOC, 0.1% SDS. Lysates were cleared of insoluble material by centrifugation at 14,000 rpm for 10 min. Protein quantification was determined using a standard Bradford assay and 80 μg of total protein was resolved by SDS-PAGE. Resolved proteins were then transferred to Immobilon-P membranes for immunoblotting. Poly-ADP-ribose polymerase (PARP) and actin were detected using a PARP antibody (Cell Signaling Technology, Beverly, MA) and an actin antibody, respectively, (Chemicon, Dietikon, Switzerland) and HRP secondary antibodies (Cell Signaling Technology, Beverly, MA).
Adhesion
Cells were detached with PBS, 0.05% EDTA, transferred to cell culture medium and counted in a Neubauer chamber. After adjustment of cell number to 50,000 cells per ml, 1 ml was added to a 6-well plate containing 1 ml of freshly prepared 2-fold concentrated taurolidine, and coated overnight with 20 μg (1 ml) per well with rat tail collagen type 1. Cells were then allowed to adhere for 15 min at 37°C, washed twice with cell culture medium and once with PBS. After fixation with 10% formalin for 15 min cell nuclei were stained with 300 nM DAPI (Molecular Probes) and random pictures (4–8 per well) were taken with a Nikon Eclipse E600 microscope equipped with a Kappa camera using a 10× objective corresponding to an area of 1.8 mm2. Nuclei counting was performed with the freely available ImageJ software (http://rsb.info.nih.gov/ij/).
Results
Taurolidine inhibits the growth of osteosarcoma cell lines
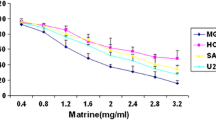
In initial experiments we examined whether taurolidine exerted a growth inhibitory effect on osteosarcoma cell lines. Incubation with taurolidine for 72 h resulted in growth inhibition of all ten OS cell lines tested and the half-maximal inhibitory concentration (IC50) of taurolidine ranged from 29 to 64 μM (Fig. 1a). Although certain OS cell lines are known to possess distinct genetic defects [i.e. (SAOS-2-p53 deficient, truncated Rb) [16]], inhibition of the OS cell lines was found to be independent of the presence or absence of these defects. Moreover, cell lines possessing greater in vivo metastatic potential (Hu09 H3, LM5, MG-63 M8, 143B) than their parental cell lines (Hu09 WT, SAOS-2, MG-63 WT, HOS, respectively) were also found to be taurolidine sensitive. Of note, although 143B and MG-63 M8 cells were found to be taurolidine sensitive the IC50 was found to be higher than their parental cell lines. Based on the fact that Rodak et al (2005) [12] demonstrated that taurolidine can exert cytotoxic effects on glioma cells as early as 24 h following exposure, we also assessed the cytotoxic effect of taurolidine on OS cell lines after 24 h (Fig. 1a). The half-maximal inhibitory concentration of taurolidine following a 24 h treatment ranged from 28 to 95 μM.
Taurolidine inhibits the growth of OS cell lines and induces apoptosis. a Taurolidine IC50 values of all cells tested. Cells were treated with increasing concentrations of taurolidine. Twenty-four or seventy-two hours later cells were subjected to a WST-1 assay in order to determine the total viable cells. Values represent mean ± SEM (n ≥ 3). Double asterisks signify not tested. b Taurolidine dose response curve of the OS cell line U2OS (black line), normal bone cells (blue line) and normal fibroblasts (green line). c U2OS cells were treated with increasing concentrations of taurolidine. Twenty-four hours later cells were stained with annexin-V-FITC and PI and visualized for apoptotic cells. Figures are representative of three independent experiments. d Normal bone cells were treated with 100 μM taurolidine. Twenty-four hours later cells were stained for annexinV/PI and visualized for apoptotic cells
Given the potent cytotoxic and anti-adhesive effects of taurolidine on osteosarcoma cells we also wanted to determine if taurolidine would have similar effects on cells obtained from bone explants or normal human bone cells and normal fibroblasts. Indeed, taurolidine inhibited the growth of normal bone cells and normal fibroblasts. However, the IC50 of taurolidine for normal bone cells and normal fibroblasts was approximately three times higher than those for OS cell lines suggesting that these cells are less sensitive to the growth inhibitory effects of taurolidine (Fig. 1a). The dose-response curves for the osteosarcoma cell line U2OS, normal bone cells and normal fibroblasts are shown in Fig. 1b. Due to the fact that the effect of taurolidine appeared to be similar among all OS cell lines tested, U2OS cells were used as a representative cell line for all further experiments examining the effects of taurolidine on OS cell lines.
Taurolidine induces apoptosis of OS cell lines
Translocation of phosphatidylserine (PS) to the cell surface is an early indicator of apoptosis and annexin-V binds to PS with high affinity [17]. To address whether taurolidine was inducing apoptosis of OS cell lines we treated U2OS cells with increasing concentrations of taurolidine for 24 h and then stained PS on the surface of cells with annexin-V-FIT-C. Necrotic cells were detected by PI staining. As shown in Fig. 1c, exposure of U2OS cells to increasing concentrations of taurolidine resulted in morphological changes including cell rounding and detachment. Annexin-V-FITC/PI staining of OS cells following taurolidine exposure revealed a dose-dependent increase in the number of apoptotic cells. Similar results were found with HOS cells (data not shown). Given that normal bone cells are not as sensitive to the effects of taurolidine, we also observed that a 24 h treatment of normal bone cells with 100 μM taurolidine did not induce significant numbers of apoptotic cells (Fig. 1d).
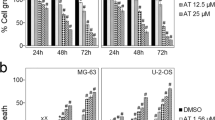
Taurolidine-induced cytotoxic effects, apoptosis and PARP are inhibited by the general caspase inhibitor Z-VAD-FMK
PARP cleavage occurs through the activation of caspases, a family of cysteine acid proteases. Treatment of U2OS cells with 50, 100 and 200 μM taurolidine resulted in a dose-dependent increase in PARP cleavage (Fig. 2a). Similar results were found with HOS cells (data not shown). In order to determine whether caspase activation is involved in PARP cleavage, taurolidine-induced cytotoxicity, apoptosis and PARP cleavage, U2OS cells were pre-treated for 2 h with 50 μM of the pan-caspase inhibitor Z-VAD-FMK prior to taurolidine addition. Twenty-four hours later cell lysates were subjected to immunoblot analysis and cells were either subjected to a WST-1 assay or were stained for annexin-V-FITC/PI to determine apoptotic and necrotic cells. Pre-treatment with 50 μM Z-VAD-FMK prior to taurolidine addition significantly inhibited PARP cleavage (Fig. 2b), decreased taurolidine-induced growth inhibition of U2OS cells (Fig. 2c) and decreased the number of annexin-V-FITC positive cells (Fig. 2d).
Caspase inhibitor prevents taurolidine-induced apoptosis. a U2OS cells were treated with 0, 50, 100 or 200 μM taurolidine and resulting cell lysates were subjected to immunoblot analysis for PARP cleavage and actin. In figures b–d U2OS cells were pre-treated for 2 h with 50 μM of the general caspase inhibitor Z-VAD-FMK prior to taurolidine addition. b Twenty-four hours following taurolidine treatment cell lysates were harvested and subjected to western blot analysis. c Twenty-four hours later cells were subjected to a WST-1 assay to determine total viable cells. Values represent mean ± SEM (n = 3). d Twenty-four hours later cells were stained with annexin-V-FITC and PI and visualized for apoptopic cells. Figures are representative of three independent experiments
Taurolidine inhibits adhesion of osteosarcoma cells in a dose-dependent manner
Taurolidine has been shown to possess anti-adherent properties and a substantial portion of its anti-bacterial capability is thought to occur through the inhibition of micro-organism adhesion [8, 9]. Nestler et al. (2005) [18] have shown that taurolidine treatment reduces the adhesion of colon carcinoma cells. In order to determine if taurolidine could decrease the adhesion of osteosarcoma cell lines U2OS cells were treated with various concentrations of taurolidine and subjected to an adhesion assay. As shown in Fig. 3a, treatment with taurolidine significantly decreased the number of adherent U2OS cells and similar results were found with HOS cells (data not shown). Taurolidine treatment also inhibited the adhesion of normal bone cells (Fig. 3a). However, anti-adherent effects were only observed when cells were treated with concentrations of taurolidine higher than those used for U2OS or HOS cells. Thus, normal bone cells appear to be less sensitive to the anti-adherent effects of taurolidine.
Effect of taurolidine on adhesion and in combination with Doxorubicin. a U2OS cells (filled square) and normal bone cells (filled triangle) were treated with increasing concentrations of taurolidine and subjected to an adhesion assay. Values represent mean ± SEM (n = 3). b U2OS cells were treated with either increasing concentrations of doxorubicin alone (filled square) or in combination with 15 μM taurolidine (filled triangle). Seventy-two hours later cells were subjected to a WST-1 assay in order to determine the total viable cells. Values represent mean ± SEM (n = 3)
Taurolidine can be used in combination with doxorubicin
In order to determine whether taurolidine could be used in combination with a current chemotherapeutic agent used for the treatment of osteosarcoma, U2OS cells were simultaneously incubated with increasing concentrations of doxorubicin and with a concentration of taurolidine that produces a 10% growth inhibition following a 72 h incubation (15 μM for U2OS) (Fig. 3b). The combined treatment of taurolidine and doxorubicin resulted in an additive effect compared to treatment with either drug alone. Similar results were found with HOS cells (data not shown).
Discussion
Identification of novel chemotherapeutic agents to improve the survival rates of osteosarcoma patients are of the utmost importance. The discovery of novel chemotherapeutic agents can be an ominous process, as even though a drug may show activity in vitro, it may face challenges in vivo due to lack of stability, metabolism or delivery. However, novel chemotherapeutic agents can occasionally be identified when a compound established for one application is subsequently examined for anti-neoplastic activity. For example, taurolidine has been safely used clinically for over 15 years for the treatment of various surgical infections and can be safely administered through a number of routes including intravenous, intrapleural, intraperitoneal instillation and direct application to wound and bone cavities [19–21]. For infection, taurolidine is clinically effective at low mM concentrations and extensive tolerance investigations have not reported any clinically significant side effects. When taurolidine was examined for anti-neoplastic properties it was shown to have efficacy against a variety of cancer cell lines and several tumor models (reviewed in [22]). Based on these findings and taurolidine’s previously established clinical safety profile, we were interested in determining whether taurolidine may have potential as a novel chemotherapeutic treatment for patients with osteosarcoma.
In initial studies we examined the effect of taurolidine on the growth of ten osteosarcoma cell lines possessing various genetic defects (i.e. mutant p53, defective Rb) and differing in vivo metastatic potential. All cell lines tested were shown to be remarkably sensitive to the effects of taurolidine. The IC50 obtained for OS cell lines are within the range of previously reported IC50 for ovarian, colon, prostate and mesothelioma cell lines [10, 14, 18]. Interestingly, all of these values are approximately 100 times lower than the concentrations used clinically for the treatment of infection.
A number of reports have stated that the effect of taurolidine is tumor cell specific and that normal cell lines and stem cells are not affected by taurolidine treatment [10, 14]. However, few reports have directly examined or demonstrated the effect of taurolidine on normal cells. In 2001, Calabresi et al. reported that taurolidine inhibited the growth of NIH-3T3 (mouse) fibroblasts but did not induce apoptosis of these cells [10]. The inhibitory effect of taurolidine on NIH-3T3 was also found to be reversible since proliferation resumed following removal of the compound. In the current study we found that taurolidine had cytotoxic effects on both normal human fibroblasts and normal human bone cells. However, compared to OS cell lines, these cells were far less taurolidine sensitive. These data suggest that the cytotoxic effect of taurolidine is tumor specific, which is consistent with previous reports [10, 14]. Consequently, the in vitro effects of taurolidine on osteosarcoma cells should be achievable in vivo and/or in a clinical setting with only minor damage to normal bone cells or fibroblasts.
The effect of anti-cancer agents on tumor cells can be either cytostatic (i.e. cell growth suppression) or cytotoxic (i.e. direct toxic effect). The effect of taurolidine on various other tumor cell lines has previously been shown to be cytotoxic and associated with a dose-dependent increase in apoptotic cells [10, 23]. Annexin-V-FITC/PI staining of osteosarcoma cells after treatment with increasing concentrations of taurolidine resulted in a dose-dependent increase in AnnexinV positive cells, and an increase in PI positive cells at higher concentrations. In addition, taurolidine treated osteosarcoma cells displayed dose-dependent cleavage of PARP. These results confirm that taurolidine induces apoptosis of osteosarcoma cell lines.
The mechanism by which taurolidine induces apoptosis of tumor cells has yet to be elucidated despite the fact that numerous publications have described taurolidine’s apoptotic-inducing effect [10, 13, 14]. Detailed studies regarding the structure, activity and cellular targets of taurolidine that are involved in initiating apoptosis have been hindered by the fact that taurolidine rapidly undergoes hydrolysation in aqueous environments. Furthermore, isolation and quantification of the relevant intermediate metabolites has proven to be difficult [10]. Hydrosylation of taurolidine results in the production of the metabolites possessing reactive methylol groups [22]. Previous studies have reported that the methylol groups interact with bacteria cell wall components such as lipopolysaccharides (LPS) to induce taurolidine’s anti-bacterial effects including loss of pathogenecity, inability to undergo mitosis and reduced adherence. Consequently, it has been hypothesized that taurolidine may interact with components of the cell membrane such as cell surface receptors in order to initiate apoptosis. Yet, these receptors remain to be identified. However, it is known that taurolidine-induced apoptosis involves activation of the caspase cascade [23]. Likewise, in the current study we demonstrated that pre-treatment with the general caspase inhibitor Z-VAD-FMK inhibited the effects of taurolidine on cell growth and morphology and prevented taurolidine-induced apoptosis and PARP cleavage. These findings confirm that taurolidine-induced apoptosis of osteosarcoma cells is also caspase mediated.
The formation of metastatic lesions is a complex process that involves a series of sequential steps that include intravasation of cells into the circulation, cell survival in the circulation, arrest of cells in a new organ, cell adherence, extravasation of cells into the surrounding tissue, the initiation of growth and vascularization of the metastatic lesion [24]. Approximately 10–20% of osteosarcoma patients have detectable metastatic lesions at the time of diagnosis while 80% have micrometastasis [25, 26]. Death from osteosarcoma typically results from respiratory failure due to progressive pulmonary metastases. Inhibition of any of the steps involved in metastases obviously would be of great benefit to osteosarcoma patients. Taurolidine has previously been demonstrated to possess anti-adherent properties. Classically, taurolidine was known to inhibit the adherence of bacteria and fungi microorganisms [8, 9], which aids in its ability to treat infections. More recently taurolidine has been shown to decrease the adherence of colon carcinoma cells [18]. Similarly, we were able to demonstrate that treatment with taurolidine results in decreased adhesion of osteosarcoma cells. The effect of taurolidine on osteosarcoma patients could potentially be two-fold, by decreasing primary tumor burden and metastatic lesions through direct cytotoxic effects and by reducing metastatic tumor cell seeding via the prevention of adherence. Based on the fact that taurolidine has previously been safely applied to bone for treatment of infection, direct application of taurolidine following surgical resection of osteosarcoma tumors may also be considered as a route of administration in order to decrease adherence of any cells that have escaped resection and to prevent primary site recurrence.
Current EURAMOS chemotherapeutic treatment regimens for osteosarcoma patients begin with ten weeks of pre-surgical treatment with doxorubicin, cisplatin and methotrexate. Following surgery patients are randomized for post-surgical treatment according to their histological response to pre-surgical chemotherapy treatment. Post-surgical treatment for good responders typically involves doxorubicin, cisplatin and methotrexate with or without interferon-alpha maintenance therapy while poor responders receive doxorubicin, cisplatin and methotrexate with or without inclusion of etoposide, ifosfamide and interferon-alpha cycles. New treatment options must either replace existing therapies or must be shown to be compatible with previously established regimens. In this study we examined the compatibility of taurolidine in combination with doxorubicin. The effects of taurolidine were shown to be additive with doxorubicin and thus, in vitro taurolidine appears to be relatively compatible with one of the main agents used for treatment of osteosarcoma and promotes clinical attractiveness for use in the treatment of osteosarcoma. However, the clinical effects of taurolidine when used either alone or in combination with current regimens will have to be established clinically with particular attention focused on synergistic and subadditive effects when used in combination.
The results of the current study suggest that taurolidine possesses potent anti-neoplastic activity against osteosarcoma cell lines and may have potential as a novel OS chemotherapeutic agent. As such, in vivo studies investigating the ability of taurolidine to reduce primary tumor burden and metastases in an osteosarcoma mouse model are underway.
References
Friedman MA, Cater S (1972) The therapy of osteogenic sarcoma: current status and thoughts for the future. J Surg Oncol 4:482–510
Marina N, Gebhardt M, Teot L, Gorlick R (2004) Biology and therapeutic advances for pediatric osteosarcoma. Oncologist 9:422–441
Browne MK, MacKenzie M, Doyle PJ (1978) Controlled trial of taurolidine in established bacterial peritonitis. Surg Gynecol Obstet 146:721–724
Billing A, Frohlick D, Ruckdeschel G (1992) Der Einfluss von Taurolidine aud die korpereigene Abwehr und die Keimelimination bei der menschlichen Peritonitis. Langenbecks Arch Chir 377:180–185
Bohm B, Schwenk W, Muller JM (1998) Long-term results after laparoscopic resection of colorectal carcinoma. Chirurg 70:453–455
Knight BI, Skellern GG, Browne MK, Pfirrmann RW (1981) Peritoneal absorption of the antibacterial and antiendotoxin taurolidine in peritonitis. Br J Clin Pharmacol 12:695–699
Gidley MJ, Sanders JK, Myers ER, Allwood MC (1981) The mode of antibacterial action of some “masked” formaldehyde compounds. FEBS Lett 127:225–227
Gorman SP, McCafferty DF, Woolfson AD, Jones DS (1987) Electron and light microscope observations of bacterial cell surface effects due to taurolidine treatment. Lett Appl Microbiol 4:103–109
Gorman SP, McCafferty DF, Woolfson AD, Jones DS (1987) Reduced adherence of micro-organisms to human epithelial cells following treatment with Taurolidine, a novel antimicrobial agent. J Appl Bacteriol 62:315–320
Calabresi P, Goulette FA, Darnowski JW (2001) Taurolidine: cytotoxic and mechanistic evaluation of a novel anti-neoplastic agent. Cancer Res 61:6816–6821
McCourt M, Wang JH, Sookhai S, Redmond HP (2000) Taurolidine inhibits tumor cell growth in vitro and in vivo. Ann Surg Oncol 7:685–691
Rodak R, Kubota H, Ishihara H, Eugster HP, Konu D, Mohler H, Yonekawa Y, Frei K (2005) Induction of reactive oxygen intermediates-dependent programmed cell death in human malignant ex vivo glioma cells and inhibition of the vacular endothelial growth factor production by taurolidine. J Neurosurg 102:1055–1068
Shrayer DP, Lukoff H, King T, Calabresi P (2003) The effect of Taurolidine on adherent and floating subpopulations of melanoma cells. Anti-cancer Drugs 14:295–303
Nici L, Monfils B, Calabresi P (2004) The effects of Taurolidine, a novel antineoplastic agent, on human malignant mesothelioma. Clin Cancer Res 10:7655–7661
Stendel R, Picht T, Schilling A, Heidenreich J, Loddenkemper C, Janisch W, Brock M (2004) Treatment of glioblastoma with intravenous taurolidine. First clinical experience. Anticancer Res 24:1143–1147
Hellwinkel OJ, Muller J, Pollmann A, Kabisch H (2005) Osteosarcoma cell lines display variable individual reactions on wildtype p53 and Rb tumour-suppressor transgenes. J Gene Med 7:407–419
Boersma HH, Kietselaer B, Stolk L, Bennaghmouch A, Hofstra L, Narula J, Heidendal G, Reutelingsperger C (2005) Past, present, and future of Annexin A5: from protein discovery to clinical applications. J Nucl Med 46:2035–2050
Nestler G, Schulz U, Schubert D, Krüger S, Lippert H, Pross M (2005) Impact of taurolidine on the growth of CC531 coloncarcinoma cells in vitro and in a laparoscopic animal model in rats. Surg Endosc 19:280–284
Conlan AA, Abramor E, Delikaris P, Hurwitz SS (1983) Taurolidine instillation as therapy for empyema thoracis. A prospective study of 50 patients. S Afr Med J 64:653–655
Browne MK (1981) The treatment of peritonitis by an antiseptic—taurolin. Pharmatherapeutica 2:517–522
Buhler HU, Mikic S, Wicki O (1978) A new surgical lavage. Helv Chir Acta 45:143–145
Jacobi CA, Menenakos C, Braumann C (2005) Taurolidine—a new drug with anti-tumor and anti-angiogenic effects. Anti-cancer Drugs 16:917–921
Darnowski J, Goulette FA, Cousens LP, Chatterjee D, Calabresi P (2004) Mechanistic and antineoplastic evaluation of taurolidine in the DU145 model of human prostate cancer. Cancer Chemother Pharmacol 54:249–258
Chambers AF, Groom AC, MacDonald IC (2002) Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer 2:563–572
Link MP, Eilber F (1989) Pediatric oncology: osteosarcoma. In: Pizzo PS, Poplack DG (eds) Principles and practice of pediatric oncology. Lippincott, Philadelphia, pp 689–711
Meyers PA, Gorlick R (1997) Osteosarcoma. Pediatr Clin N Am 44:973–989
Acknowledgements
This study was supported by a grant from the Walter L. and Johanna Wolf Foundation, Zurich, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walters, D.K., Muff, R., Langsam, B. et al. Taurolidine: a novel anti-neoplastic agent induces apoptosis of osteosarcoma cell lines. Invest New Drugs 25, 305–312 (2007). https://doi.org/10.1007/s10637-007-9052-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-007-9052-9