Abstract
Background
Peppermint oil is well known to inhibit smooth muscle contractions, and its topical administration during colonoscopy is reported to reduce colonic spasms.
Aims
We aimed to assess whether oral administration of IBGard™, a sustained-release peppermint oil formulation, before colonoscopy reduces spasms and improves adenoma detection rate (ADR).
Methods
We performed a single-center randomized, double-blinded, placebo-controlled trial. Patients undergoing screening or surveillance colonoscopies were randomized to receive IBGard™ or placebo. The endoscopist graded spasms during insertion, inspection, and polypectomy. Bowel preparation, procedure time, and time of drug administration were documented. Statistical analysis was performed using the Student’s t test and Wilcoxon rank-sum test.
Results
There was no significant difference in baseline characteristics or dose-timing distribution between IBGard™ and placebo groups. Similarly, there was no difference in ADR (IBGard™ = 47.8%, placebo = 43.1%, p = 0.51), intubation spasm score (1.23 vs 1.2, p = 0.9), withdrawal spasm score (1.3 vs 1.23, p = 0.72), or polypectomy spasm score (0.52 vs 0.46, p = 0.69). Limiting the analysis to patients who received the drug more than 60 min prior to the start of the procedure did not produce any significant differences in these endpoints.
Conclusions
This randomized controlled trial failed to show benefit of orally administered IBGard™ prior to colonoscopy on the presence of colonic spasms or ADR. Because of its low barrier to widespread adoption, the use of appropriately formulated and timed oral peppermint oil warrants further study to determine its efficacy in reducing colonic spasms and improving colonoscopy quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Each year, over 100,000 people are diagnosed with colorectal cancer (CRC) leading to over 50,000 CRC-related deaths in the USA alone [1]. It is the third most common malignancy, and approximately 4.2% of people will be diagnosed with colorectal cancer at some point during their lifetime [1, 2]. Worldwide in 2018, 1.8 million new cases of CRC and 881,000 CRC-related deaths were reported and are expected to continue to rise [3, 4].
Colonoscopy is the gold standard for the diagnosis and prevention of colon cancer [5]. Colon cancer prevention is achieved by detection and resection of precancerous polyps. The adenoma detection rate (ADR) is a widely accepted measure of colonoscopy. Inadequate bowel preparation, short withdrawal time, and colonic spasms are factors that can interfere with mucosal inspection and reduce colonoscopy quality [5].
A variety of antispasmodic medications such as hyoscine butylbromide (HBB), glucagon, warm water, and topical lidocaine have been used during colonoscopy to reduce colonic spasms and improve inspection. Unfortunately, the routine use of many of these agents has not gained traction because of their side effects [6].
Peppermint oil is a commonly used flavoring agent that relaxes the gastrointestinal smooth muscles via calcium channel antagonism. It has no significant adverse effects and has been used for irritable bowel syndrome. Several studies evaluating intraluminal administration of peppermint oil during colonoscopy have demonstrated an increase in ADR and a reduction in colonic spasms [7,8,9,10,11]. However, there is a lack of studies evaluating orally administered peppermint oil on colonoscopy quality.
The objective of our study is to determine whether the use of a sustained-release formulation of peppermint oil, IBGard™, administered prior to colonoscopy, improves the quality of colonoscopy. We hypothesized that administration of two capsules of orally administered IBGard™ would be associated with reduced colonic spasms and higher adenoma detection rates compared to administration of placebo. Significant reductions of spasm and improved ADR by convenient administration of an inexpensive and safe peppermint oil preparation would have the potential to gain widespread use.
Materials and Methods
Study Design
This study was a single-center, randomized, double-blind, placebo-controlled trial conducted at the University of California Irvine Comprehensive Digestive Disease Center. The study protocol was approved by the Institutional Review Board (IRB) at the university and followed the SPIRIT guidelines. Patients were randomized to receive either IBGard™ or placebo before colonoscopy using a simple randomization method. There are no prior studies of ADR on colonoscopy with orally administered peppermint oil, but there has been one well-designed study reporting ADR with intraluminally sprayed peppermint oil or l-menthol. Inoue et al. found the ADR to be 60.2% in colonoscopies with intraluminally administered l-menthol compared to 42.6% in the control group, an improvement of 41%. Inoue et al. calculated their sample size using an expected improvement of 20% over baseline ADR of 37.5% [7]. We therefore similarly assumed a control baseline ADR of 40% based on local experience and the expected ADR of the IBGard group to be 48%, a 20% improvement. A sample size of 110 was calculated to detect this difference with 80% power and 95% confidence.
Randomization was conducted with a 1:1 ratio using a randomization table generated by a third party and performed at the time of consent. Patients and endoscopists were both blinded to the intervention. Patients were randomly allocated to either intervention or control group based on randomization table that was concealed from endoscopists. Patients undergoing screening colonoscopy, colonoscopy to investigate a positive fecal occult blood test (FOBT) or FIT (fecal immunohistochemical test), and surveillance colonoscopy for prior history of colorectal polyps were eligible for enrollment.
Patients were excluded if they were over age 85 or under 18, had history of colectomy, known current colorectal cancer, known colorectal stenosis, history of inflammatory bowel disease (IBD), familial polyposis, sepsis, use of calcium channel blockers for 24 h prior to colonoscopy, or had a documented or suspected allergy to peppermint oil. Certain patients with coagulopathies—including INR greater than 2.5, platelets less than 20,000, uncorrectable coagulopathy or active bleeding, anemia requiring transfusion to maintain hemoglobin greater than 7, or inherited disorders of hemostasis such as von Willebrand disease and hemophilia were also excluded (Table 1).
Procedure
Patients were given a preparatory bowel cleanse procedure using split-dose of GoLytely, NuLytely, or SUPREP (Braintree Laboratories Inc., Braintree, MA, USA) the day of and the evening prior to procedure.
Prior to the procedure, patients were administered two capsules of IBGard™ (each containing 90 mg of peppermint oil or 41.5 mg l-menthol equivalent) or two placebo capsules containing sucrose. Placebo capsules were compounded to appear identical to retail IBGard™ capsules by a third-party compounding agency (Alvarado Pharmacy Services Inc., San Diego, CA). The timing of administration varied to maintain patient flow but whenever possible was targeted to be performed at least 60 min prior to the colonoscopy.
Procedures included conscious sedation titrated at the discretion of the endoscopist or no sedation. Endoscopy was performed with adult or pediatric colonoscopes (Olympus® PCF-H190L or Olympus® CF-HQ190L). All procedures were performed by one of three colonoscopists (W.K., S.P., and G.A). One endoscopist (W.K.) performed approximately 80% of the procedures. Each colonoscopist had performed more than 1000 colonoscopies.
During each colonoscopy, the endoscopist evaluated the effect of colonic spasm using a 3-grade scale (Table 2) during insertion, withdrawal, and polypectomy for each of the right, middle, and left segments of the colon. Afterward the procedure, the endoscopist graded the ease of colonoscopy and the patient graded his or her toleration level using a single question survey (Table 3).
The baseline demographics, including age and colonoscopy indication, were recorded. Procedure details including time of drug administration, procedure start time and end time, cecal intubation time, and Boston Bowel Preparation Score (BPSS) were also recorded.
Study data were collected using UCICQD database, a prospective electronic data capture tool containing > 10 k colonoscopies hosted securely at the University of California, Irvine (UCI). Data were de-identified and extracted using analytical software (Power BI, Microsoft Corporation). The extracted de-identified dataset is exempt from human subjects research for IRB purposes as determined by the UCI Human Research Protections (HS#2015-2939 [eAPP #8814]) dated 1/13/2016.
Endpoints
Two primary outcomes were evaluated. The first was a difference in the ADR between the IBGard™ and control group. ADR is defined as the proportion of patients undergoing colonoscopy with at least one adenomatous lesion identified (adenoma, tubulovillous adenoma, or villous adenoma) determined by pathology report. The second primary outcome was a difference in spasm scores between the IBGard™ and control group. Differences were evaluated for each phase of the colonoscopy (intubation, withdrawal, and polypectomy) and for each segment of the colon (left, transverse, and right colon). Secondary outcomes included differences in cecal intubation time, endoscopist ease of colonoscopy score, and patient pain score.
Statistical Analysis
All variables analyzed exhibited right-skewed distributions. Generalized estimating equations with a Poisson distribution were used to examine the differences in treatment groups (placebo vs IBGard™). Subgroup analysis of subjects with dose times of < 60 and > 60 min was performed using the same statistical methods. A two-sided p value of 0.05 was used in all analyses.
Ethical Considerations
This study was approved by the IRB at the University of California, Irvine, and was conducted in compliance with ethical standards of the University of California on human subjects and with the 1964 Declaration of Helsinki. The trial was exempt from registration with Clinicaltrials.gov because IBGard™ is regarded as a medical food that is not FDA regulated.
Results
Two hundred patients met eligibility criteria and were enrolled between January 2019 and September 2019. They were randomized to receive IBGard™ and placebo equally. Eight patients had incomplete data recorded and were excluded. Therefore, 192 patients were included in the final analysis (IBGard™ n = 102, placebo n = 90) (Fig. 1).
There were no significant differences in baseline data between the two groups (Table 4). Average insertion and withdrawal times were slightly shorter in the placebo group (10.9 and 14.5 min) compared to the IBGard™ group (12.5 and 16.5 min), but this difference was not significant.
The dose timing of the capsules before colonoscopy ranged from 26 to 164 min. 55.7% (107/192) of patients received their capsules greater than 60 min, while 44.3% (85/192) of patients received their capsules less than 60 min before their procedure. Mean time of dose was 67.94 min before colonoscopy with a standard deviation of 27.29. The distribution of dose timing between the placebo and IBGard™ groups did not differ significantly (Fig. 2).
There were no significant differences in adenoma detection rate (IBGard™ = 47.8%, placebo = 43.1%, p = 0.51), intubation spasm score (1.23 vs 1.2, p = 0.9), withdrawal spasm score (1.3 vs 1.23, p = 0.72), or polypectomy spasm score (0.52 vs 0.46, p = 0.69). Full results are presented in Table 5. After stratifying the results by timing of doses > 60 min and < 60 min, there remained no significant differences. Full results stratified by dose timing are presented in Table 6. No adverse events were reported in either the experimental or control groups.
Discussion
The quality of colonoscopy is dependent on the endoscopist’s ability to detect and remove colonic lesions. Technologies to enhance visibility and improve colonoscopy quality such as high-definition white light, chromoendoscopy, narrow-band imaging, and Endocuff/AmplifEYE rely on adequate bowel preparation and a well-distended colon [12]. Colonic spasms affect colonoscopy quality by preventing adequate colonic distention, impeding visualization of the mucosa, and interfering with resection of polyps.
Several methods have been proposed to reduce colonic spasms. Intravenous HBB and glucagon have been used, though routine use of these agents has been limited by cost and side effects. HBB, while shown to improve polyp detection when administered at the cecum, can cause miosis, palpitations, dry mouth, and urinary retention and is contraindicated in patients with heart disease. Glucagon can cause hyperglycemia, reactive hypoglycemia, and rebound spasm. Both can cause anaphylaxis [13, 14]. Warm water infusion has been shown to enhance patient comfort but has not been shown to suppress spasms [15]. Topical lidocaine was shown to reduce colonic spasms in one study but did not improve ADR [16].
Peppermint oil is well known to inhibit colonic peristalsis. The primary active component of peppermint oil is l-menthol, which has a variety of effects as an anti-inflammatory, antispasmodic, and analgesic [17, 18]. l-menthol works via antagonism of calcium channels in smooth muscles to inhibit contraction which has been demonstrated in vitro on the human colon [18]. The antispasmodic effect appears to be dependent on the direct uptake by the gastrointestinal mucosa [19]. Once absorbed, l-menthol is metabolized in the liver by the cytochrome P450 system, producing inactive metabolites that are then excreted via bile and urine [6]. Orally administered peppermint oil has been shown to be safe with no serious adverse effects [17, 20].
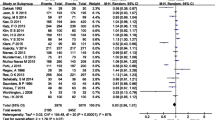
The use of peppermint oil and its active component l-menthol in both upper and lower endoscopy to reduce peristalsis has been studied. Yamamoto et al. and Hiki et al. found that peppermint oil administered intraluminally to the pylorus and duodenum significantly reduces gastrointestinal spasms during ERCP and upper endoscopy, respectively, with no significant side effects [21, 22]. Asao et al. applied a topical peppermint oil mixture (8 mL of peppermint oil with 1 L of water and 0.2 mL of polysorbate 80) intraluminally during colonoscopy to 409 patients. In this unblinded study, 88.5% of treated patients had a satisfactory spasmolytic effect compared to 33.3% in the control group (p < 0.001) [8]. Inoue et al. randomized 226 patients to receive either a preparation of 1.6% l-menthol or saline sprayed intraluminally during cecal intubation and withdrawal. The study, which was also unblinded, found significantly increased ADR for the l-menthol group compared with placebo (60.2% vs 42.6%, p = 0.01), and the proportion of patients with no peristalsis to be higher in the l-menthol group (71.2% vs 30.9%, p < 0.01) [7].
More recently, Dhillon et al. performed a similar double-blinded randomized trial comparing l-menthol to simethicone applied to the cecum. The l-menthol group had a significantly higher proportion of patients with no peristalsis (44.3% l-menthol vs 21.3% control, p = 0.002), but there was no significant difference in ADR [10].
While these studies demonstrated that intraluminal application of l-menthol or peppermint oil can reduce colonic spasms and potentially improve ADR, the practicality and cost of preparing topical l-menthol and applying it during a colonoscopy have hindered widespread adoption. Oral administration of peppermint oil or l-menthol would be both easier and more cost-effective to use in clinical practice.
Only two studies have evaluated the effect of oral peppermint oil on colonic spasms. Both studies used Colpermin (Tillotts Pharma, Ziefen, Switzerland), a formulation of peppermint oil that has been enteric-coated to minimize the risk of worsening reflux symptoms. Shavakhi et al. randomized 65 patients to one capsule of orally administered Colpermin (187 mg peppermint oil) or placebo 4 h prior to colonoscopy. They found a significant reduction in cecal intubation time (6.87-min Colpermin vs 10.6-min placebo, p < 0.001) and total procedure time (12.2 min vs 15.9 min, p < 0.001). Moreover, colonic spasm scores and pain scores were significantly lower in the Colpermin group. Patients in the Colpermin group were also much more likely to be amenable to repeat colonoscopy. The study, however, did not evaluate ADR as an endpoint [23]. Al Moussawi et al. similarly randomized 78 patients to receive placebo or two capsules of Colpermin (374 mg peppermint oil). They did not find any significant differences between cecal intubation time, colonic spasms, endoscopist satisfaction, or patient pain scores [24].
Cash et al. described a novel triple-coated microsphere formulation of purified l-menthol designed for sustained release in the small intestine. Industry-sponsored studies of this formulation, marketed as IBGard™, have shown it to be effective at reducing symptoms associated with IBS with minimal side effects [17]. To the best of our knowledge, our study is the first to evaluate the use of this specific formulation of peppermint oil in endoscopy. It is also the largest double-blinded randomized controlled trial to date that examines the effect of oral administration on colonoscopy. We did not find any differences in ADR, spasm scores, or cecal intubation time between patients who received IBGard™ versus placebo. These findings were unchanged when patients were stratified into two cohorts—those who received their capsules < 60 min before their procedure and those who received their capsules > 60 min before their procedure.
Our findings are consistent with those by Al Moussawi et al. but stand in contrast to the improvement in ADR found by Asao et al. and reduction in cecal intubation time and colonic spasms found by Shavakhi et al.
There are several differences between our study and the aforementioned ones that can explain discrepancies in results. Compared to oral administration, the application of peppermint oil or l-menthol intraluminally leads to a quicker onset of action due to immediate absorption by the colonic mucosa. In the study by Asao, the mean time to onset was 21.6 s and the effect continued for at least 20 min [8]. As these studies have suggested, the antispasmodic effect appears to be dependent on the direct uptake by the gastrointestinal mucosa. Thus, orally administered formulations should be given enough time to allow for gastric emptying and absorption to take place. In their study, Shahvakhi et al. administered oral enteric-coated peppermint oil 4 h before colonoscopy. In contrast, we aimed to administer IBGard™ at least 60 min before the procedure. Although there are no published data on the pharmacodynamics, our target time of 60 min was selected based on data from the IBS Adherence and Compliance Trial (IBSACT) study that showed a reduction in IBS symptoms of 33.7% at 1 h, 41.9% at 1–2 h, and 14.4% at 3–8 h with minimal side effects, suggesting a therapeutic effect as soon as within 1 h of ingestion [25]. However, there was significant variability in the dose timing due to uncontrollable factors such as the arrival time of patients and procedure room turnover, and nearly half of our patients received IBGard™ less than 60 min before their procedure. Analysis of the > 60 min cohort versus the < 60 min cohort did not show significant differences, which may further reflect the design of IBGard™ as triple-coated microspheres for slow sustained release in the small bowel.
The grading system for colonic spasms also varied between studies. As there is no consensus standard for grading colonic spasms, each study used a proprietary grading system subject to endoscopist interpretation. We designed a grading scale that aimed to minimize endoscopist bias by having most procedures performed by a single endoscopist and focusing on whether spasms impeded procedural tasks such as polypectomy. However, while having most procedures performed by single endoscopist decreases interobserver variability for subjective measures, it can be a limitation for objective measures such as ADR, which is measured per endoscopist. It is important to note that our endoscopists had a high average ADR of 43%, which could may be close to the general incidence of adenoma and thus potentially limit the degree of benefit from additional interventions such as IBGard™.
The strengths of our study included the double-blind and randomized design and the large number of subjects. We used a formulation of peppermint oil that is available over-the-counter, meaning that our study can be easily replicated and validated.
The largest limitation of our study was the significant variability in the dose timing of administration of IBGard™ that likely affected our results. The use of a sustained-release formulation of peppermint oil may have a delayed response that our study was unable to detect. Furthermore, like grading scales used in previous studies, our colonic spasm scale is subjective. For future studies, these issues can be resolved by simplifying the colonic spasm scale (i.e., present or not present) to reduce subjective observation variability, targeting a strict time of administration (i.e., 4 h before colonoscopy), and possibly using a non-sustained-release formulation of peppermint oil.
Conclusion
Our study of orally administered IBGard™ administered at arrival time for colonoscopy does not show any significant impact on colonic spasms, procedure time, or ADR. Earlier administration of IBGard™ prior to colonoscopy may have revealed significant results as suggested by prior studies. The use of oral peppermint oil to reduce colonic spasms and improve colonoscopy quality warrants further exploration given its low cost, safety, and low barrier to widespread adoption. Larger, double-blinded randomized controlled trials are needed to compare different methods of peppermint oil administration to assess its true benefit and efficacy for colonoscopy.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683–691.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Araghi M, Soerjomataram I, Jenkins M, et al. Global trends in colorectal cancer mortality: projections to the year 2035. Int J Cancer. 2019;144:2992–3000.
Joseph DA, Meester RGS, Zauber AG, et al. Colorectal cancer screening: Estimated future colonoscopy need and current volume and capacity. Cancer. 2016;122:2479–2486.
Sanagapalli S, Agnihotri K, Leong R, Corte CJ. Antispasmodic drugs in colonoscopy: a review of their pharmacology, safety and efficacy in improving polyp detection and related outcomes. Ther Adv Gastroenterol. 2017;10:101–113.
Inoue K, Dohi O, Gen Y, et al. l-menthol improves adenoma detection rate during colonoscopy: a randomized trial. Endoscopy. 2014;46:196–202.
Asao T, Mochiki E, Suzuki H, et al. An easy method for the intraluminal administration of peppermint oil before colonoscopy and its effectiveness in reducing colonic spasm. Gastrointest Endosc. 2001;53:172–177.
Yoshida N, Naito Y, Hirose R, et al. Prevention of colonic spasm using l-menthol in colonoscopic examination. Int J Colorectal Dis. 2014;29:579–583.
Dhillon AS, Alshankiti S, Khorasani-zadeh A, et al. A247 l-menthol during colonoscopy for adenoma detection in an intermediate risk patient population: a double-blind, randomized controlled trial. J Can Assoc Gastroenterol. 2018;1:360–361.
Chumpitazi BP, Kearns GL, Shulman RJ. Review article: the physiological effects and safety of peppermint oil and its efficacy in irritable bowel syndrome and other functional disorders. Aliment Pharmacol Ther. 2018;47:738–752.
Dik VK, Moons LM, Siersema PD. Endoscopic innovations to increase the adenoma detection rate during colonoscopy. World J Gastroenterol. 2014;20:2200–2211.
Byun TJ, Han DS, Ahn SB, et al. Role of intravenous hyoscine N-butyl bromide at the time of colonoscopic withdrawal for polyp detection rates: a randomized, double-blinded, placebo-controlled trial. Gastrointest Endosc. 2009;69:AB229. https://doi.org/10.1016/j.gie.2009.03.555.
Yoshikawa I, Yamasaki M, Taguchi M, et al. Comparison of glucagon and scopolamine butylbromide as premedication for colonoscopy in unsedated patients. Dis Colon Rectum. 2006;49:1393–1398.
Church JM. Warm water irrigation for dealing with spasm during colonoscopy: simple, inexpensive, and effective. Gastrointest Endosc. 2002;56:672–674.
Nemoto D, Suzuki S, Mori H, et al. Inhibitory effect of lidocaine on colonic spasm during colonoscopy: a multicenter double-blind, randomized controlled trial. Dig Endosc. 2019;31:173–179. https://doi.org/10.1111/den.13272.
Cash BD, Epstein MS, Shah SM. A novel delivery system of peppermint oil is an effective therapy for irritable bowel syndrome symptoms. Dig Dis Sci. 2016;61:560–571. https://doi.org/10.1007/s10620-015-3858-7.
Amato A, Liotta R, Mulè F. Effects of menthol on circular smooth muscle of human colon: analysis of the mechanism of action. Eur J Pharmacol. 2014;740:295–301.
Micklefield GH, Greving I, May B. Effects of peppermint oil and caraway oil on gastroduodenal motility. Phytother Res. 2000;14:20–23.
Khanna R, MacDonald JK, Levesque BG. Peppermint oil for the treatment of irritable bowel syndrome: a systematic review and meta-analysis. J Clin Gastroenterol. 2014;48:505–512.
Yamamoto N, Nakai Y, Sasahira N, et al. Efficacy of peppermint oil as an antispasmodic during endoscopic retrograde cholangiopancreatography. J Gastroenterol Hepatol. 2006;21:1394–1398.
Hiki N, Kurosaka H, Tatsutomi Y, et al. Peppermint oil reduces gastric spasm during upper endoscopy: a randomized, double-blind, double-dummy controlled trial. Gastrointest Endosc. 2003;57:475–482.
Shavakhi A, Ardestani SK, Taki M, Goli M, Keshteli AH. Premedication with peppermint oil capsules in colonoscopy: a double blind placebo-controlled randomized trial study. Acta Gastroenterol Belg. 2012;75:349–353.
Al Moussawi H, Al Khatib M, El Ahmar M, et al. The effect of premedication with peppermint oil capsules (Colpermin) prior to colonoscopy: a double blind randomized placebo-controlled trial. Arab J Gastroenterol. 2017;18:220–223.
Bd C, Cash BD, Epstein MS. Patient satisfaction with IBS symptom relief using a novel peppermint oil delivery system in a randomized clinical trial and in the general population. Int J Dig Dis. 2016;. https://doi.org/10.4172/2472-1891.100027.
Acknowledgments
We thank Mary B. Roberts for her statistical expertise and Vicky Cao for her expertise in data acquisition.
Funding
Funding was provided by Dr. Jason B. Samarasena, Associate Clinical Professor of Medicine, Division of Gastroenterology, at the University of California Irvine Medical Center.
Author information
Authors and Affiliations
Contributions
JH and WK conceived and designed the study; ZM, JH, and WK contributed to the acquisition, analysis, and interpretation of data; ZM, JH, and ED drafted the manuscript; ZM, JH, ED, and WK critically revised the manuscript; JS supported financially; and WK is the article guarantor.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Han, J.Y., Moosvi, Z., Duh, E. et al. Oral IBGard™ Before Colonoscopy: A Single-Center Double-Blinded, Randomized, Placebo-Controlled Trial. Dig Dis Sci 66, 1611–1619 (2021). https://doi.org/10.1007/s10620-020-06383-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06383-3