Abstract
Background
Ileocecal thickening (ICT) on imaging could result from diverse etiologies but may also be clinically insignificant.
Aim
Evaluation of role of combined 2-deoxy-2-fluorine-18-fluoro-d-glucose(18F-FDG)-positron emission tomography and computed tomographic enterography (PET–CTE) for determination of clinical significance of suspected ICT.
Methods
This prospective study enrolled consecutive patients with suspected ICT on ultrasound. Patients were evaluated with PET–CTE and colonoscopy. The patients were divided into: Group A (clinically significant diagnosis) or Group B (clinically insignificant diagnosis) and compared for various clinical and radiological findings. The two groups were compared for maximum standardized uptake values of terminal ileum, ileo-cecal valve, cecum and overall.
Results
Of 34 patients included (23 males, mean age: 40.44 ± 15.40 years), 12 (35.3%) had intestinal tuberculosis, 11 (32.4%) Crohn’s disease, 3 (8.8%) other infections, 1 (2.9%) malignancy, 4 (11.8%) non-specific terminal ileitis while 3 (8.8%) had normal colonoscopy and histology. The maximum standardized uptake value of the ileocecal area overall (SUVmax-ICT-overall) was significantly higher in Group A (7.16 ± 4.38) when compared to Group B (3.62 ± 9.50, P = 0.003). A cut-off of 4.50 for SUVmax-ICT-overall had a sensitivity of 70.37% and a specificity of 100% for prediction of clinically significant diagnosis. Using decision tree model, the SUVmax-ICT with a cut-off of 4.75 was considered appropriate for initial decision followed by the presence of mural thickening in the next node.
Conclusion
PET–CTE can help in discrimination of clinically significant and insignificant diagnosis. It may help guide the need for colonoscopy in patients suspected to have ICT on CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ileocecal thickening (ICT) is a common clinical problem encountered by physicians in general and gastroenterologists and radiologists in particular [1]. The term ileocecum refers to the terminal ileum, ileocecal valve, appendix and the cecum. Any of these regions could be involved in isolation or in a contiguous manner resulting in a diagnostic confusion. Also, the region could be involved by diseases localized to the ileocecum or systemic disorders [1, 2]. Further, previously treated diseases may result in certain sequelae which may be confused with ongoing active disease process, e.g., pulled up cecum in patients previously having intestinal tuberculosis [3]. The region is an area of physiological stasis of the gut contents, thereby increasing the exposure time to various pathogens and antigens and has abundant lymphoid tissue and therefore a frequent site of many diseases like intestinal tuberculosis (ITB) and Crohn’s disease (CD). The differential diagnosis of ICT is diverse and needs multimodality assessment with the use of radiological, endoscopic, histological, microbiological and serological modalities to establish the diagnosis [1, 4]. To add to the problem is the challenge of assessing the bowel wall thickness in situations where the luminal distension is poor [5]. This could result in overreporting of ileocecal thickening necessitating unwarranted colonoscopy. Currently, computed tomography (CT) is the modality of choice for evaluation of ileocecal region. CT Enterography (CTE) uses the distension of the lumen by oral administration of negative contrast to improve the evaluation of bowel wall and lumen [6, 7]. The abnormalities detected or suspected on CT must be evaluated further using colonoscopic examination and sampling.
Combination of 2-deoxy-2-fluorine-18- fluoro- d-glucose (18F-FDG) positron emission tomography (PET) and CTE may help in providing both anatomic data from CTE and metabolic information from PET thereby helping in comprehensive evaluation. To the best of our search, no previous study has reported on prospective evaluation of suspected ICT by using PET–CTE. Therefore, we planned to study the role of PET–CTE as a single modality in determining the significance of its findings in patients suspected to have ICT.
Materials and Methods
Setting
This prospective study was done at the Department of Gastroenterology of a large tertiary care institution. The patients were enrolled from July 2017 to October 2018. The study was conducted as per the Declaration of Helsinki and local guidelines. The study protocol was approved by the Institute Ethics Committee of the institute and the study protocol conforms to the ethical guidance provided as per Helsinki declaration and the Indian Council of Medical Research. Written informed consent was obtained from the patients prior to inclusion in the study and separate written consent was also taken prior to any invasive procedure including PET–CTE and colonoscopy.
Patients
We screened consecutive patients with complaints like abdominal pain, chronic diarrhea or episodes of intestinal obstruction for possible inclusion. The patients who had suspicion of ileocecal thickening on ultrasound were considered for inclusion. Patients who were allergic to intravenous contrast or polyethylene glycol (PEG), were younger than 18 years, pregnant or lactating females, had uncontrolled diabetes, were claustrophobic or had renal dysfunction or those who refused consent were excluded.
A detailed clinical history of various parameters like pain, fever, loss of weight or appetite, fever, past history of tuberculosis or any relevant past history was obtained and recorded in a preformat. The patients who were included underwent PET–CTE and colonoscopy within a period of 1 week.
PET–CTE and Colonoscopy
The PET–CTE was done prior to colonoscopy and colonoscopy was done within a week of the PET–CTE. The staff involved in F-18 PET–CTE imaging were not provided any clinical information except for suspicion of ICT. The PET–CTE was performed after 4 h of fasting and blood glucose levels were ensured to be less than 150 mg/dl before injection of FDG. An intravenous injection of 150–200 Mbq of F-18 FDG was administered. The patients were asked to drink 1500 ml of water mixed with polyethylene glycol (PEG) during the next 1 h. The regional images of abdomen and pelvis were acquired using a dedicated PET–CT scanner (Discovery STE 16 or 710; GE Medical Systems, Milwaukee, WI, USA) after 60 min of IV injection of FDG. The CT parameters were: voltage 120 kVp, current 250 mA, rotation time of 0.8 s and 27.50 mm3/rotation and FOV of 70 mm. The images were reconstructed using 512 × 512 matrix with 3.75 mm slice thickness. PET images were constructed using 128 × 128 matrix and reconstructed using OSEM algorithm.
The PET–CTE images were analyzed by separately for FDG-PET uptake at ICJ and CTE by two investigators (RB and PG respectively). The investigators were blinded from the clinical and endoscopic findings or the diagnosis and also from each other’s reporting. F18-FDG uptake in the bowel was considered to be increased only if it was greater than adjacent bowel loops. Analysis was made comparing maximum standardized uptake value (SUVmax) activity of ileocecal junction and liver. The SUVmax -ICT-overall, i.e., highest value of terminal ileum, cecum and ileocecal junction) was used as a benchmark for analysis. A normal PET activity was assigned if there was no activity or it was less than liver. In cases the PET activity was similar or higher than liver the PET findings were interpreted as positive. CTE was reported for both luminal and extraluminal findings including caliber of involved bowel and part proximal to it, mural thickening, enhancement and stratification were also recorded. Further any perienteric findings like fat stranding, lymphadenopathy, etc., were also recorded.
Colonoscopy was done after standard 4-l preparation with PEG in two split doses. The structured proforma was used to record the findings from each of the colonic areas, ileocecal valve and ileum. The biopsies were taken from terminal ileum and cecum irrespective of the endoscopic findings.
Diagnosis and Follow-Up
The final diagnosis was based on the basis of a combination of clinical, endoscopic, histopathological, microbiological and serological parameters. In cases where the initial diagnosis was uncertain between Crohn’s disease (CD) and intestinal tuberculosis (ITB), a response to antitubercular therapy (ATT) was used [8, 9]. In all patients, irrespective of findings on colonoscopy, biopsies were obtained from the ileocecal area. The diagnosis of CD was made as per the standard criteria using a combination of clinical, endoscopic and histological findings (with lack of response to ATT) and improvement with treatment with steroids/immunomodulators [10]. Nonspecific terminal ileitis was diagnosed in the presence of a few small ulcers in the terminal ileum and in the absence of any involvement of the colon with no identifiable etiology on evaluation (including history of NSAIDs, negative stool culture, histology, serology) and lack of any worsening on follow-up [11]. For the purpose of analysis, patients were divided into one of two groups, i.e., Group A: Clinically significant diagnosis (Crohn’s disease, intestinal tuberculosis, malignancies, other infections, etc.) and Group B: Clinical insignificant diagnosis (normal colonoscopy or nonspecific terminal ileitis). These groups were compared for baseline clinical parameters, mural thickening on CT and SUVmax of the ileocaecal region on PET scan. These parameters were also analyzed in patients with ITB and CD as an exploratory analysis.
Data Analysis
The statistical analysis was performed using SPSS version 23, R statistical software version 3.6.1 and Python version 3.6.9. The pROC package was used other than the base package in R [12]. The sklearn package and its dependencies were additionally used other than base packages in python [13]. Mean ± S.D was used for descriptive statistics of continuous data while for categorical data number along with percentages was used. For comparing two groups at a particular time point, independent t test was used for continuous data and Chi-square test was used for categorical data. Welch correction was applied to independent t test in case of unequal variance or unequal sample size. Fisher exact test was used instead of Chi-square if one of the cells expected value is less than 5. In case the P value was found to be significant for a particular comparison, the correction for multiple comparisons (Bonferroni correction) was applied. Further, area under the receiver operating characteristic curve (AUROC) was computed for distinction of clinically insignificant diagnosis with that of clinically significant diagnosis using the SUVmax of PET of the terminal ileum, ileocecal valve, cecum and for ileocaecal region (ICT-Overall) overall. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were determined utilizing the best methodology (cut-off) for each one of them. The decision tree analysis model was constructed to arrive at the diagnosis of clinically significant disease. The features evaluated for inclusion in the model were presence or absence of mural thickening in CT scan and maximum value of SUVmax in PET scan of the terminal ileum, ileocaecal valve and cecum. One hot encoding was done for mural thickening as it was a categorical variable. The data were divided into training and test dataset in the ratio of 0.7:0.3. The entropy was kept as criterion for construction of decision tree model. The maximum depth was kept at 4 and minimum sample leaves was kept at 5. The prediction accuracy of the test dataset was assessed in the constructed model.
Results
Patients and Evaluation
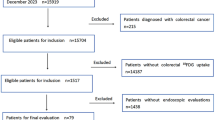
Of the 82 patients with suspected or diagnosed ICT during the study period, we included 34 patients in the final analysis. The reasons for the exclusion are shown in Fig. 1. The mean age of the study population was 40.44 ± 15.40 years. Twenty-three (67.6%) of the patients were males. The clinical presentation included abdominal pain in 29 (85.3%), loss of weight in 20 (58.8%), loss of appetite in 16 (47.1%), fever in 9 (26.5%), diarrhea in 9 (26.5%) and episode(s) of intestinal obstruction in 6 (17.6%). Anemia was present in majority of the patients (24, 70.6%). Elevated C-reactive (> 6 mg/dL) protein levels were found in 19 (55.9%) patients. Elevated fecal calprotectin levels (> 43 mcg/g of stool) were present in 29 (85.3%) patients.
Computed tomography showed lymphadenopathy in 20 (58.8%) patients with mesenteric lymph nodes being the most common involved region. Necrotic lymph nodes were seen in 2 patients while one patient had calcifications. Three patients had pleural effusion and one had ascites. Twenty- seven patients (79.4%) were noted to have ileocecal thickening on computed tomography with mean thickness of 12.76 ± 7.3 mm while perienteric fat changes were noted in 16 (47.1%) patients and mural stratification in 4 (11.8%) patients.
The FDG-PET revealed a mean SUVmax for terminal ileum to be 4.19 ± 2.52, for ileocecal valve to be 4.62 ± 3.00 and for the cecum to be 5.68 ± 4.09. The highest SUVmax from among these three regions, i.e., SUVmax (ICT) was found to be 6.43 ± 4.16. The colonoscopy findings were normal in three patients and biopsies in these patients were deemed to be normal. The major endoscopic findings were transverse ulcers in 25 (80.6%), aphthous ulcers in 16 (51.6%) and linear ulcers in 7 (22.6%) patients. Ileocecal valve was ulcerated in 4 (11.8%) patients, strictured in 8 (23.6%), gaping in 3 (8.8%) and deformed in 2 (5.8%) patients. Ascending colonic involvement was seen in 10 (29.4%) patients while transverse and descending colonic involvement was seen in 6 (17.6%) and 5 (14.7%) patients respectively. None of the patients suffered any adverse events related to PET–CTE.
Diagnosis and Follow-Up
The final diagnosis was intestinal tuberculosis in 12 (35.3%) patients (Fig. 2), Crohn’s disease in 11(32.4%) (Fig. 3), other infections (amebiasis and histoplasmosis) in 3 (8.8%), malignancy in 1 (2.9%), nonspecific terminal ileitis in 4 (11.8%) (Fig. 4) and normal colonoscopy and histology in 3 (8.8%) patients. Therefore Group A had 27 cases while group B had 7 cases. Of the patients with ITB, 3 patients (25%) had a microbiologically confirmed diagnosis. Two patients had GeneXpert positivity from intestinal tissue biopsy and one from lymph node aspirate. In the rest of nine cases of probable ITB, early mucosal healing of ulcers was demonstrated by colonoscopy at 2 months. The patients with nonspecific terminal ileitis underwent repeat colonoscopy at least 6 months after initial diagnosis and did not demonstrate any progression of lesions. One of these patients had also undergone capsule endoscopy without evidence of any other area of involvement except terminal ileum.
Axial CT and Fused PET/CT images (a and b) revealed FDG avid thickening at the ICJ (SUVmax), Cecum (arrow) and descending colon (arrow-head). Additionally paracolic stranding is also noted along the descending colon. Colonoscopy showing diffuse ulceration in cecum and histology showing focal crypt abscess (arrow) and submucosal noncaseating granuloma (asterisk) in a case of Crohn’s disease
Trans-axial CT and Fused PET/CT images (A and B) revealed no abnormal FDG uptake or thickening at the ICJ and Cecum. Colonoscopy showed small ulcer in terminal ileum and histology showed ulcerated mucosa (arrow) over lymphoid aggregate. At 9 months of follow-up the patient remained well and showed no progression of the lesion and a diagnosis of nonspecific terminal ileitis was made
Comparison Between the Clinically Significant and Clinically Insignificant Diagnosis
Of the 27 patients with clinically significant diagnosis (Group A), 25 had mural thickening whereas two out of seven with clinically insignificant diagnosis (Group B) had mural thickening (P = 0.008). Therefore, of the seven patients without any mural thickening, five had a clinically insignificant diagnosis. The two groups had significant differences for the hemoglobin values, C-reactive protein levels and fecal calprotectin levels. The SUVmax (ICT-overall) between the two groups and was found to be significantly higher in Group A (7.16 ± 4.38) when compared to Group B (3.62 ± 9.50, P < 0.003). The SUVmax for all three sites was significantly higher in the Group A (Table 1).
The area under the receiver operating characteristic (ROC) curve for SUVmax (ICT-overall) for prediction of clinically significant diagnosis was 0.741 (95% CI 0.579–0.903), for terminal ileum was 0.804 (95% CI 0.657–0.951), cecum was 0.698 (95% CI 0.528–0.868) and ileocecal valve was 0.714 (95% CI 0.537–0.892) (Fig. 5). The cut-off calculated by best methodology for Terminal ileum, IC Valve and cecum were 2.65 (Sensitivity 77.77% and Specificity 100%), 4.15 (55.55% and 100%) and 4.55 (62.96% and 100%). For SUVmax (ICT-overall), the cut-off of 4.50 had sensitivity of 70.37% and a specificity of 100% for prediction of final diagnosis. The final developed decision tree is shown in Fig. 6. The maximum value of SUVmax among terminal ileum, ileocaecal valve and cecum with a cut-off of 4.75 was considered for the initial decision followed by the mural thickening in the CT scan in the next node. The accuracy of the developed model on the test dataset was 100%.
Graphical representation of the Decision Tree model. The value corresponds to the classification of clinically insignificant and clinically significant respectively. The orange color represents true and blue color represents false. The intensity of the orange and blue colors corresponds to the purity of the classification based on entropy with larger intensity representing more purity (less entropy)
Intestinal Tuberculosis Versus Crohn’s Disease
The comparison between the ITB and CD groups has been shown in Table 2. Although fever, absence of diarrhea and lymphadenopathy was found with higher frequency in ITB group, none of these reached statistical significance. The mean SUVmax (ICT) was not statistically different between the patients with ITB and CD (6.15 ± 2.87 and 6.56 ± 2.87).
Discussion
In this study where the role of PET CTE in patients with suspected ICT was evaluated, we found that PET–CTE could help in discrimination of clinically significant diagnoses from clinically insignificant diagnosis. Our study also indicates that the values of the uptake, do not help in discrimination of ITB and CD, the two most common conditions seen in the study group. These findings have clinical relevance because ICT is a common finding on computed tomography which may be misleading because of possible overdiagnosis due to multiple reasons like nonspecific thickening or lack of proper distension of the bowel. This could lead to unwarranted colonoscopy which is an invasive procedure requiring sedation and associated with complications like pain, colonic perforation apart from the associated costs. In this regard, a discriminative modality which could guide the need of colonoscopy in such doubtful cases is needed. Further, colonoscopy is often needed to demonstrate mucosal healing in patients initiated on ATT for suspected ITB and even in patients with CD who are on treatment [8]. In such cases repeat PET–CT may provide information on mucosal healing and may avoid repeated colonoscopy. The addition of metabolic information, as provided by PET scan, may help in avoiding unnecessary colonoscopy especially in patients who are at a high risk from such a procedure.
Multiple imaging modalities have previously been used for evaluation of ITB and CD [14,15,16]. While CT remains the initial modality used at most centers and provides information on luminal and extraluminal involvement, contrast MRI with use of diffusion weighted imaging is particularly useful for assessment of disease activity in Crohn’s disease [14, 16]. Only limited studies have previously reported about the role of PET in evaluation of ileocecal lesions. Most previous reports have dealt with use of PET–CTE in estimation of disease activity in Crohn’s disease [17,18,19]. One previous report on 17 patients has addressed the use of PET–CT enteroclysis for evaluation of small bowel inflammatory diseases and found it to be better than barium studies and colonoscopy combined together [20]. However, enteroclysis is associated with patient discomfort and additional radiation exposure related to naso-enteral tube placement. Enterography, in contrast, provides almost similar bowel distension without the need of a naso-enteral tube [7]. PET CTE has been used in patients with inflammatory bowel disease. In a study of 43 patients with Crohn’ disease, PET CT was reported to show a high sensitivity and specificity (90 and 90.2%) for picking up inflamed disease segments [21]. While PET CTE has been found to be very sensitive for detection of moderate to severe disease activity, the sensitivity is reduced in patients with milder endoscopic disease [22]. The study suggested that SUVmax could be an objective criterion for detection of active inflammation. The role of PET CTE in discriminating inflammatory and fibrotic strictures in CD has, however, been less satisfactory [23].
The most important causes of ICT in our setting were CD and ITB. These two conditions are extremely difficult to discriminate because of overlapping clinical, endoscopic, radiological and histological findings. The clinician often has to embark on presumptive trial of antitubercular therapy to look for healing of ulcers to discriminate the two conditions [9, 10]. None of the previous reports have compared the findings on PET–CTE in ITB and CD. Unfortunately, our data indicates the lack of discriminative value of SUV on PET CTE for differentiating these two conditions. Further, our results indicate that the PET Uptake between a normal colon and those with nonspecific terminal ileitis is similar. However, even in patients with normal colon some uptake was noted on PET CT. Low-level uptake in intestine is well-recognized to be present and is possibly related to peristalsis and low-grade inflammation in response to huge antigenic load to which the bowel is continuously exposed [24].
Many previous reports have suggested that some of the ulcers detected in the terminal ileum during an ileocolonoscopy may not have clinical implications and the course is benign and progression to CD is rare. The patients who were diagnosed to have nonspecific terminal ileitis asymptomatic on > 6 months of follow-up [11, 25]. The decision tree constructed in the study combines the SUVMax and the mural thickening on PET–CTE. Although, decision tree is recognized to underperform in external data, still its intuitivity and clinical applicability in decision making may make it a useful tool. The presence of unequal sample sizes between the predicted classes might push the developed model toward detection of the dominant class, but we did not correct for it by employing correction techniques such as resampling as we do not want to miss a clinically significant lesion.
There are a few limitations for the present study: the numbers were small and overall numbers in the various etiologic groups were few for any meaningful comparisons. The small number was primarily because we excluded patients who presented to us with a prior computed tomography so as to avoid additional radiation exposure. There are also additional limitations of the technique as some patients may not tolerate bowel preparation, the procedure cannot be done in cases with deranged blood glucose and an obvious increase in the costs. The strength combines the benefits of luminal distension achieved by CTE and metabolic activity assessed by PET. Also, the best gold standard of complete histological assessment of the bowel wall and mesentery was not possible as this would have required surgical resection. Further, we did not evaluate the interobserver agreement for the findings reported. However, previous studies have shown that CTE for IBD has perfect interobserver agreement of CT [26, 27]. Considering the evolving role of PET–CT enterography, a similar data is not available for the FDG uptake in the bowel and therefore constitutes a limitation for our study.
However, the prospective nature of the study, masking of the personnel involved in conduct and reporting of PET–CTE, well-characterization of the diagnosis and complete follow-up and assessment of response to therapy are the strengths of the study. Further, it is the first prospective study of PET–CTE in patients with suspected ICT.
In conclusion, PET CTE could help identify the group of patients having clinically significant conditions as the cause of ileocecal thickening.
References
Agarwala R, Singh AV, Shah J, Mandavdhare HS, Sharma V. Ileocecal thickening: clinical approach to a common problem. JGH Open. 2019;3:456–463.
Kumar A, Rana SS, Nada R, et al. Significance of ileal and/or cecal wall thickening on abdominal computed tomography in a tropical country. JGH Open. 2018;3:46–51.
Goyal P, Shah J, Gupta S, Gupta P, Sharma V. Imaging in discriminating intestinal tuberculosis and Crohn’s disease: past, present and the future. Expert Rev Gastroenterol Hepatol. 2019;13:995–1007.
Toshniwal J, Chawlani R, Thawrani A, et al. All ileo-cecal ulcers are not Crohn’s: changing perspectives of symptomatic ileocecal ulcers. World J Gastrointest Endosc. 2017;9:327–333.
Fernandes T, Oliveira MI, Castro R, et al. Bowel wall thickening at CT: simplifying the diagnosis. Insights Imag. 2014;5:195–208.
Sheedy SP, Kolbe AB, Fletcher JG, Fidler JL. Computed tomography enterography. Radiol Clin North Am. 2018;56:649–670.
Minordi LM, Vecchioli A, Mirk P, Bonomo L. CT enterography with polyethylene glycol solution vs CT enteroclysis in small bowel disease. Br J Radiol. 2011;84:112–119.
Sharma V, Mandavdhare HS, Dutta U. Letter: mucosal response in discriminating intestinal tuberculosis from Crohn’s disease-when to look for it? Aliment Pharmacol Ther. 2018;47:859–860.
Sharma V, Mandavdhare HS, Lamoria S, Singh H, Kumar A. Serial C-reactive protein measurements in patients treated for suspected abdominal tuberculosis. Dig Liver Dis. 2018;50:559–562.
Magro F, Gionchetti P, Eliakim R, et al. European Crohn’s and Colitis Organisation [ECCO]. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J Crohns Colitis. 2017;11:649–670.
Chang HS, Lee D, Kim JC, et al. Isolated terminal ileal ulcerations in asymptomatic individuals: natural course and clinical significance. Gastrointest Endosc. 2010;72:1226–1232.
Robin X, Turck N, Hainard A, et al. pROC: an open-source package for R and S + to analyze and compare ROC curves. BMC Bioinf. 2011;12:77.
Pedregosa F, Varoquaux G, Gramfort A, et al. Scikit-learn: machine learning in python. J Mach Learn Res. 2011;12:2825–2830.
Rajendran H, Razek AAKA, Abubacker S. Multimodal imaging of fibrosing mesenteric tuberculosis. Radiol Case Rep. 2019;14:920–925.
Abdel Razek AA, Abu Zeid MM, Bilal M, Abdel Wahab NM. Virtual CT colonoscopy versus conventional colonoscopy: a prospective study. Hepatogastroenterology. 2005;52:1698–1702.
Abd-El Khalek A, Abd-ALRazek A, Fahmy DM. Diagnostic value of diffusion-weighted imaging and apparent diffusion coefficient in assessment of the activity of crohn disease: 1.5 or 3 T. J Comput Assist Tomogr. 2018;42:688–696.
Shyn PB, Mortele KJ, Britz-Cunningham SH, et al. Low-dose 18F-FDG PET/CT enterography: improving on CT enterography assessment of patients with Crohn disease. J Nucl Med. 2010;51:1841–1848.
Groshar D, Bernstine H, Stern D, et al. PET/CT enterography in Crohn disease: correlation of disease activity on CT enterography with 18F-FDG uptake. J Nucl Med. 2010;51:1009–1014.
Ahmadi A, Li Q, Muller K, et al. Diagnostic value of noninvasive combined fluorine-18 labeled fluoro-2-deoxy-d-glucose positron emission tomography and computed tomography enterography in active Crohn’s disease. Inflamm Bowel Dis. 2010;16:974–981.
Das CJ, Makharia G, Kumar R, et al. PET-CT enteroclysis: a new technique for evaluation of inflammatory diseases of the intestine. Eur J Nucl Med Mol Imag. 2007;34:2106–2114.
Holtmann MH, Uenzen M, Helisch A, et al. 18F-Fluorodeoxyglucose positron-emission tomography (PET) can be used to assess inflammation non-invasively in Crohn’s disease. Dig Dis Sci. 2012;57:2658–2668. https://doi.org/10.1007/s10620-012-2190-8.
Louis E, Ancion G, Colard A, et al. Noninvasive assessment of Crohn’s disease intestinal lesions with (18)F-FDG PET/CT. J Nucl Med. 2007;48:1053–1059.
Lenze F, Wessling J, Bremer J, et al. Detection and differentiation of inflammatory versus fibromatous Crohn’s disease strictures: prospective comparison of 18F-FDG-PET/CT, MR-enteroclysis, and transabdominal ultrasound versus endoscopic/histologic evaluation. Inflamm Bowel Dis. 2012;18:2252–2260.
Das CJ, Manchanda S, Panda A, Sharma A, Gupta AK. Recent advances in imaging of small and large bowel. PET Clin. 2016;11:21–37.
Tse CS, Deepak P, Smyrk TC, Raffals LE. Isolated acute terminal ileitis without preexisting inflammatory bowel disease rarely progresses to crohn’s disease. Dig Dis Sci. 2017;62:3557–3562. https://doi.org/10.1007/s10620-017-4803-8.
Booya F, Fletcher JG, Huprich JE, et al. Active Crohn disease: cT findings and interobserver agreement for enteric phase CT enterography. Radiology. 2006;241:787–795.
Horvat N, Tavares CC, Andrade AR, et al. Inter- and intraobserver agreement in computed tomography enterography in inflammatory bowel disease. World J Gastroenterol. 2016;22:10002–10008.
Funding
None
Author information
Authors and Affiliations
Contributions
AKS was involved in data collection and analysis and manuscript approval. RKB was involved in data interpretation, revision and approval of manuscript. PG involved in data interpretation, revision and approval of manuscript. PKM involved in statistical analysis and revision and approval of manuscript. SM involved in manuscript writing, revision and approval of manuscript. HSM involved in provision of study material, revision and approval of manuscript. Harjeet Singh involved in provision of study material, revision and approval of manuscript. Kaushal K Prasad involved in data interpretation, revision and approval of manuscript. Usha Dutta involved in provision of study material, revision and approval of manuscript. VS involved in conception, data collection, provision of study material, manuscript draft, revision and approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, A.K., Kumar, R., Gupta, P. et al. FDG-PET–CT Enterography Helps Determine Clinical Significance of Suspected Ileocecal Thickening: A Prospective Study. Dig Dis Sci 66, 1620–1630 (2021). https://doi.org/10.1007/s10620-020-06361-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06361-9