Abstract
Background and Aims
Long-term results on hepatitis B virus (HBV) reactivation in patients with resolved infection during anti-cancer therapy are unknown. This study investigated long-term risk and therapeutic endpoints including hepatitis B surface antigen (HBsAg) seroclearance following antiviral therapy in patients developing reactivation of resolved HBV.
Methods
The study included 528 consecutive HBsAg-negative/hepatitis B core antibody-positive patients who underwent rituximab treatment or hematopoietic stem cell transplantation (HSCT) between 2006 and 2016. Long-term outcomes of patients with reactivation after antiviral therapy were examined in comparison with 37 HBsAg-positive chronic carriers under the same medical settings.
Results
The 7-year cumulative rate of HBV reactivation was 10.8% and 57.9% in patients receiving rituximab treatment and HSCT, respectively. After antiviral initiation, patients with reactivation of resolved HBV showed significantly higher 1-year cumulative rates of hepatitis B e antigen seroconversion (69.2% vs. 22.6%, P = 0.008) and HBsAg seroclearance (61.8% vs. 3.3%, P < 0.001) than chronic HBsAg carriers. Reactivation of resolved HBV was independently predictive of HBsAg seroclearance in a combined group of reactivated patients and chronic HBsAg carriers. Low viral load at reactivation was predictive of HBsAg seroclearance in reactivated patients. The majority of patients with HBsAg seroclearance developed anti-HBs. None of the reactivated patients who achieved HBsAg seroclearance relapsed after cessation of antiviral therapy.
Conclusions
HBsAg seroclearance rapidly occurs following antiviral therapy for reactivation of resolved HBV infection, suggesting distinct clinical phenotypes as well as shorter duration of HBV infection associated with this particular disease setting-HBV reactivation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) reactivation is commonly documented in chronic hepatitis B (CHB) patients who receive immunosuppressive therapy or chemotherapy. Clinical features can be asymptomatic in some patients and fatal in others [1, 2]. Reactivation can also occur in patients with past HBV infection who are negative for hepatitis B surface antigen (HBsAg) and positive for antibody to hepatitis B core antigen (anti-HBc), which indicates either a self-limiting acute HBV infection or occult HBV infection with low viremia. With recent advances in anti-cancer therapies, this unfavorable event is also reported in the setting of hepatocellular carcinoma, antibody against tumor necrosis factor or methotrexate as well as hematological diseases [3,4,5].
HBsAg-negative/anti-HBc-positive patients have a relatively higher risk for HBV reactivation while on rituximab or hematopoietic stem cell transplantation (HSCT), compared to other treatments [1, 6, 7]. The reported incidence rates range 3–30% with rituximab [1, 6, 8] and 3–43% with HSCT [9,10,11]. To prevent serious outcomes from HBV reactivation, recent guidelines for HBV infection recommend that HBsAg-negative/anti-HBc-positive patients receiving rituximab or HSCT should be closely monitored with on-demand antiviral therapy or treated with nucleos(t)ide analog (NUC) if close monitoring is not guaranteed [12, 13].
However, long-term risk of reactivation in hematological patients with resolved hepatitis B still remains unknown, since most previous studies evaluated only a limited number of patients with short-term follow-up. Intermediate or surrogate endpoints to evaluate the efficacy and response to antiviral therapy as prophylaxis or rescue therapy for HBV reactivation have not been adequately studied so far. Thus, it is not clear whether the current initiation, continuation or stopping rule of NUC therapy for CHB patients is still applicable to such patients. Additionally, long-term clinical outcomes following antiviral therapy in this particular patient group remain unknown. To address these issues, we investigated long-term course of reactivation and therapeutic endpoints including HBsAg seroclearance after the commencement of antiviral therapy in previously HBsAg-negative/anti-HBc-positive patients developing HBV reactivation under rituximab treatment or HSCT through long-term follow-up.
Patients and Methods
Study Population
This study recruited consecutive patients who underwent rituximab-containing chemotherapy or HSCT for their underlying hematological malignancies between January 2006 and May 2016 at a tertiary center in South Korea. Patients were eligible for the study if they were 18 years or older and negative for HBsAg and positive for anti-HBc before therapy. We retrospectively evaluated HBV reactivation in these patients, and HBV reactivation was typically detected during identifying the cause of hepatitis (usually ALT level > two times the upper limit of normal, 40 U/L) or routine testing of HBV serologic markers. To compare virological/serological responses to antiviral therapy in patients with HBV reactivation, distinct clinical manifestation of HBV infection, we also included chronic HBsAg carriers who underwent rituximab treatment or HSCT during the same period and started antiviral therapy. Patients were excluded if they had drug resistance, prior antiviral therapy, intermittent use of antiviral agents and no available follow-up testing for HBV. Patients with HBsAg negativity or undetectable HBV DNA when starting antiviral therapy were also excluded. Until recently, Korean national health insurance system strictly limits the use of antiviral therapy to CHB patients in whom the level of alanine aminotransferase (ALT) is over 80 U/L and the level of HBV DNA is over 20,000 and 2000 IU/mL in hepatitis B e antigen (HBeAg)-positive and -negative patients, respectively. Although antiviral therapy was considered for all patients with reactivation of resolved hepatitis B or preemptively for chronic HBsAg carriers, some patients who refused antivirals due to a discrepancy in the Korean insurance policy were closely followed up with on-demand antiviral therapy upon reactivation. Each patient provided written informed consent for this study. This study was approved by the Ethics Committee of the Catholic University of Korea (IRB KC17RESI0680).
Treatment Protocol
In this study, the chemotherapeutic agents used were diverse and opted according to standard regimens for each hematological malignancy. In the rituximab group, patients received mean 6 ± 3 cycles of rituximab-containing chemotherapy (usually given every 21 days). In the HSCT group, patients generally started chemotherapy and/or immunosuppressive treatment 5 months before receiving HSCT. A considerable number of the patients (52.5%) were diagnosed with AML or ALL, and they received myeloablative or reduced intensity conditioning regimens before performing HSCT. For pretreatment in patients who underwent allogeneic HSCT, a calcineurin inhibitor (tacrolimus or cyclosporine) in combination with methotrexate or mycophenolate mofetil was used for graft-versus-host disease (GVHD) prophylaxis and antithymocyte globulin was given intravenously at various doses during conditioning.
Definitions
HBV reactivation was defined as HBsAg seroreversion or the appearance of detectable HBV DNA levels (≥ 10 IU/mL) in previously HBsAg-negative/anti-HBc-positive patients. The period of time to HBV reactivation was calculated from the first date of HSCT or rituximab-containing chemotherapy, and that of HBsAg seroclearance was calculated from the first date of starting antiviral therapy. Virological response was defined as a decrease in serum HBV DNA to undetectable level by real-time polymerase chain reaction (PCR) assay.
Laboratory Measurements
Routine laboratory tests were done every 1–3 months according to their treatment schedules for hematological malignancies, whereas regular virological assessment was unable to be performed due to the lack of adequate reimbursement by national insurance policy for HBV testing in HBsAg-negative patients with resolved infection. HBV markers were monitored every 1–3 months if HBV reactivation was confirmed. Serum HBsAg, HBeAg and antibodies to HBeAg and HBsAg (anti-HBs) were tested by the Modular E170 assay (Hoffman-La Roche, Switzerland). HBsAg was measured qualitatively or quantitatively using the ARCHITECT assay (detection limits > 0.05 IU/mL; Abbott Park, IL, USA). Serum HBV DNA was quantified by a real-time PCR assay (Abbott Laboratories; detection limits ≥ 10 IU/mL).
Statistical Analyses
The t test or Mann–Whitney U test was used for comparison of continuous variables, and the Chi-squared test or Fisher exact test was used for comparing categorical variables. The cumulative rates of HBV reactivation, virological response, HBeAg seroconversion and HBsAg seroclearance were estimated using the Kaplan–Meier method, and the differences were analyzed using the log-rank test. The following parameters were analyzed to identify predictive factors for HBsAg seroclearance by univariate analysis: age (< 50 vs. ≥ 50 years), gender, HBV DNA (≤ 2.0 × 104 vs. > 2.0 × 104 IU/mL), HBsAb (absence or presence), HBeAg (absence or presence), ALT (< 120 vs. ≥ 120 U/L), treatment modality (HSCT vs. rituximab) and HBV reactivation (absence or presence). Continuous variables of age and ALT were transformed into two-level categorical data based on the median value. For HBV DNA, we used the level of 2.0 × 104 IU/mL, which is the value often suggested as high viremia in practice guidelines. Parameters with P < 0.05 were included in a multivariable Cox proportional hazard model. A two-sided P value < 0.05 was considered statistically significant. Data were analyzed using the SPSS 20.0 (SPSS Inc., Chicago, IL, USA).
Results
Patients
A total of 686 HBsAg-negative/anti-HBc-positive patients who were scheduled to undergo rituximab treatment or HSCT were screened for study inclusion. After excluding 158 patients who lacked follow-up results for HBV serum markers, 528 patients (143 and 385 in the rituximab and HSCT groups, respectively) were recruited and evaluated for HBV reactivation during therapy. To compare clinical outcomes after antiviral therapy in patients with HBV reactivation, we selected 37 chronic HBsAg-positive patients who started NUC therapy under the same hematological setting during the same study period (Fig. 1).
HBV Reactivation and Antiviral Therapy
Overall, 61 HBsAg-negative/anti-HBc-positive patients developed HBV reactivation during the mean follow-up period of 23.3 ± 19.9 months. The 7-year cumulative rate of HBV reactivation in the entire population was 31.6%, occurring at a median of 18.8 months (range 2.4–78.6). The rates of reactivation at 1 and 7 years were 7.6% and 10.8% in the rituximab group and 2.5% and 57.9% in the HSCT group, respectively (Fig. 2a). The median level of HBV DNA at reactivation was 5.5 × 106 IU/mL (range 17–7.2 × 108). The median levels of AST and ALT were 93 U/L and 112 U/L, respectively. At reactivation, 5 patients (8.2%) remained HBsAg-negative with positive HBV DNA levels. Forty-nine patients (89.1%) lost anti-HBs even though they had anti-HBs at baseline. The median HBsAg level in 17 available patients was 2.0 × 104 IU/mL (range 0.81–1.2 × 105). One patient died of HBV reactivation. In the other patients, there was no liver-related serious outcome. The clinical characteristics at HBV reactivation of enrolled patients are summarized in Table 1.
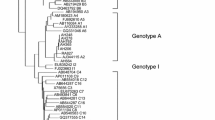
Kaplan–Meier analysis. HBV hepatitis B virus, HBsAg hepatitis B surface antigen, anti-HBc antibody to hepatitis B core antigen, HSCT hematopoietic stem cell transplantation. a The cumulative rates of HBV reactivation among 528 HBsAg-negative and anti-HBc-positive patients (black line), 385 patients who underwent HSCT (green line), and 143 patients who underwent rituximab-containing chemotherapy (blue line). b The cumulative rates of virological response in patients with HBV reactivation and chronic HBsAg carriers. c The cumulative rates of HBeAg seroconversion in patients with HBV reactivation and chronic HBsAg carriers. d The cumulative rates of HBsAg seroclearance in patients with HBV reactivation and chronic HBsAg carriers. HBV hepatitis B virus; HBsAg hepatitis B surface antigen; anti-HBc antibody to hepatitis B core antigen; HSCT, hematopoietic stem cell transplantation
Among the 61 patients with reactivation of resolved infection, 27 were found ineligible for response assessment according to exclusion criteria (Fig. 1), and thus, 34 were evaluable for long-term virological/serological responses to NUC therapy. Among the 37 chronic HBsAg carriers, 32 initiated antivirals preemptively before rituximab or HSCT, and the other 5 started NUCs after recognition of HBV reactivation. Regarding antiviral therapy, all except 4 of the 71 patients with HBV reactivation or chronic HBsAg carriers received tenofovir or entecavir.
Virological and HBeAg Responses
At baseline, HBV DNA levels were not significantly different between the two groups, while AST and ALT levels in the reactivated group were significantly higher than those in chronic HBsAg carriers. Virological response was observed in 82.4% and 86.1% in patients with reactivation of resolved infection and chronic HBsAg carriers, respectively (Fig. 2b). HBeAg at the time of starting antiviral therapy was positive in 29 (85.3%) reactivated patients and in 15 (40.5%) chronic carriers (Table 1). The estimated rates of HBeAg seroconversion at 1 year of NUC therapy were 69.2% and 22.6% in patients with resolved HBV reactivation and chronic HBsAg carriers, respectively (P = 0.008; Fig. 2c).
HBsAg Seroclearance
Overall, 24 of the patients with reactivation of resolved infection achieved HBsAg seroclearance after median 6.2 months (range 0.5–28.3) of NUC therapy. The cumulative rates were 35.3%, 61.8% and 89.8% at 6 months, 1 and 4 years, respectively. Anti-HBs developed in 19 (79.2%) of the 24 patients with HBV reactivation by 34.6 months. Sixteen (66.7%) of the reactivated patients with HBsAg seroclearance stopped NUCs. Apart from two patients without follow-up HBV testing, none of the 14 evaluable patients relapsed during median 25.0 months (range 5.1–42.5) after cessation of antiviral therapy. On the contrary, the other 8 patients with HBsAg seroclearance still continued NUCs against HBV reactivation because they developed post-HSCT GVHD and were treated with steroid-containing immunosuppressants. In chronic HBsAg carriers, only 3 of the 37 (8.1%) patients receiving NUCs during rituximab or HSCT displayed HBsAg seroclearance, which occurred at 10, 34 and 44 months (Fig. 2d). Two of the 3 chronic HBsAg carriers who achieved HBsAg seroclearance started antivirals after experiencing HBV reactivation. Their HBV DNA level increased from almost undetectable values to over 7.0 × 105 IU/mL, and ALT flares were accompanied. The remaining one started NUC preemptively.
Factors for HBsAg Seroclearance
For the entire population, male sex, positive HBeAg, high ALT levels, HSCT and HBV reactivation group were significantly associated with HBsAg seroclearance. On multivariate analysis, male sex [P =0.007, hazard ratio (HR) = 4.4, 95% confidence interval (CI) 1.5–12.7] and HBV reactivation group (P < 0.001, HR = 23.6, 95% CI 6.6–84.5) remained independently predictive of HBsAg seroclearance. For patients with reactivation of resolved hepatitis B, male and HBV DNA levels appeared associated with HBsAg seroclearance. On multivariate analysis, male sex (P = 0.008, HR = 4.3, 95% CI 1.5–12.6) and HBV DNA level < 2.0 × 104 IU/mL (P < 0.001, HR = 27.7, 95% CI 6.1–124.7) at reactivation were identified to be independent factors for HBsAg seroclearance (Table 2). HBsAg levels were more likely to drop earlier in patients achieving HBsAg seroclearance, when compared to those not (Fig. 3). The median values of the slopes of HBsAg levels were 0.43 (0.23–0.75) and 0.06 (0.02–0.17) in patients with or without HBsAg seroclearance, respectively (P = 0.017).
Changes in HBsAg levels in individual patients with reactivation of resolve HBV following antiviral therapy. The measurements of baseline and follow-up HBsAg levels were available in 10 patients. Each line represents a change in HBsAg level in each patient. HBsAg, hepatitis B surface antigen. Solid lines represent the HBsAg levels of patients with HBsAg seroclearance. Dotted lines represent the HBsAg levels of patients without HBsAg seroclearance
Discussion
Despite a multitude of prior reports on HBV reactivation in previously HBsAg-negative/anti-HBc-positive patients on chemotherapy, very little is known about patient outcome after the commencement of antiviral therapy. The actual long-term risk of reactivation is also not well known in such settings. In this long-term follow-up study involving a large number of patients, we observed that HBsAg-negative patients with resolved hepatitis are at considerable risk for HBV reactivation during rituximab or HSCT, with cumulative risk of 10.8% and 57.9% at 7 years, respectively. However, early antiviral intervention is associated with a higher probability of achieving therapeutic or surrogate endpoints in patients with reactivation of resolved infection as compared to chronic HBsAg carriers undergoing the same anti-cancer therapies. In particular, HBsAg seroclearance occurred significantly earlier with a high cumulative rate of 61.8% at 1 year in HBsAg-negative/anti-HBc-positive patients developing reactivation than in chronic HBsAg carriers. Anti-HBs also developed in the majority of patients with HBsAg seroclearance, and none of them relapsed after cessation of antiviral therapy.
HBsAg seroclearance rarely occurs until up to 5 years in patients with CHB, even with the use of potent antivirals such as entecavir or tenofovir [14]. Previous studies calculated HBsAg seroclearance in CHB patients treated with NUCs as taking a median of 36–52.2 years [15, 16]. By contrast, our study showed a remarkably high rate of HBsAg seroclearance, occurring in 89.8% of the patient with HBV reactivation up to 4 years of NUC therapy. These suggest unique clinical features of reactivation in patients with resolved HBV distinct from reactivation in chronic HBV carriers.
In our results, lower levels of HBV DNA (≤ 2.0 × 105 IU/mL) were independently associated with rapid HBsAg seroclearance. Although this should be further validated, this finding implies that early antiviral initiation at low-level viremia before it begins to significantly increase is essential to achieve HBsAg seroclearance in patients developing reactivation if preemptive NUCs are not administered. Consistently, low baseline levels or the rapid decline of HBsAg following antiviral therapy was predictive of HBsAg seroclearance in CHB patients [17,18,19]. The lower baseline HBV DNA observed in our patients achieving HBsAg seroclearance supports the potential role of HBsAg in predicting HBsAg seroclearance, since HBsAg level is reportedly correlated with HBV DNA level in the early phase of hepatitis B [20, 21]. Indeed, most of our patients showing a rapid HBsAg decline following antiviral therapy eventually achieved HBsAg seroclearance.
Male was also a significant predictor for HBsAg seroclearance in this study. Although there are controversies, some studies showed that males tended to achieve the higher rate of HBsAg seroclearance than females [22, 23]. One possible hypothesis is the difference in immunity between males and females. While IL-6 is able to suppress HBV replication [24], overproduction of IL-6 is associated with the development of HCC [25]. A previous study demonstrated that estrogen inhibits IL-6 production, which could partly contribute to male predominance in HCC [26]. Based on these, we hypothesize that differential intensity of immune activity could lead to gender difference in the incidence of HBsAg seroclearance as well as HCC. Further study is needed to delineate the association between gender and HBsAg seroclearance.
The phenomenon of early HBsAg seroclearance that occurred in patients with reactivation of resolved hepatitis B is clearly distinct from that in CHB patients. In acute HBV infection, virus-specific T cells have a crucial role in viral clearance, whereas these cells are functionally impaired and exhausted in CHB, permitting viral persistence [27]. A previous study showed that host-induced ALT flare followed by a decrease in HBV DNA led to HBsAg seroclearance in 42% of CHB patients, whereas no HBsAg seroclearance was noted in virus-induced flare [28]. Thus, host immunity against HBV in patients with resolved infection would be fairly preserved, resembling that in acute infection rather than chronic infection and eventually contributed to HBsAg seroclearance following antiviral therapy. Additionally, low levels of intrahepatic covalently closed circular DNA (cccDNA) and total DNA coupled with the shorter duration of HBV infection in patients with resolved HBV versus CHB patients will further help facilitate a successful clearance of HBsAg, as in patients with acute hepatitis B [29]. Taken together, our observations of early HBsAg seroclearance in previously HBsAg-negative/anti-HBc-positive patients reflect the preserved immune response to HBV and low levels of intrahepatic HBV, indicating distinct clinical phenotypes of reactivation of resolved HBV. In any case, early recognition and initiation of antivirals prior to a significant increase in HBV load is crucial for the prevention of serious hepatic morbidities as well as the achievement of HBsAg seroclearance.
Although HBsAg seroclearance is accepted as the ideal endpoint of therapy, HBsAg can be produced from transcriptionally active cccDNA or integrated HBV DNA even in patients who lost serum HBsAg [21]. Given the shorter duration of HBV infection, the likelihood of off-therapy relapse after HBsAg seroclearance in resolved hepatitis B is lower when compared to chronic HBV infection, because of presumably low levels of intrahepatic cccDNA and integration. Indeed, none of our patients who discontinued antivirals developed relapse post-treatment. More studies will be needed to determine whether antiviral therapy can be safely discontinued in this setting.
This study has some limitations. Measurement of HBV markers was not regularly done in a considerable proportion of patients before recognition of HBV reactivation. This might have led to the underestimation of actual HBV reactivation rates. The reason for the higher reactivation rates observed in patients undergoing HSCT versus rituximab-based therapy remains unclear. Unlike settings of rituximab-based therapy, there might be additional contributable factors for HBV reactivation such as other chemotherapies or more frequent use of steroids for GVHD, especially in patients who underwent HSCT. The starting points of antiviral therapy differed among the enrolled patients, making it difficult to evaluate factors associated with early achievement of response or HBsAg seroclearance after rescue antiviral therapy for reactivation. Elucidating these associations in future studies will be challenging because recent therapeutic strategy more strictly pursues inhibiting the development of HBV reactivation.
In conclusion, HSCT or rituximab treatment can pose a significant risk of HBV reactivation in previously HBsAg-negative/anti-HBc-positive patients. For these patients, close monitoring and early intervention with antiviral drugs before HBV load significantly increases is of paramount importance in reducing the mortality related to this complication. That will also lead to early achievement of therapeutic endpoints such as HBsAg seroclearance. The unexpectedly early clearance of HBsAg in patients with reactivation of resolved infection suggests its distinct phenotype, indicating a lower level of HBV pool associated with the shorter duration of HBV infection and preserved immunity against HBV. Further studies will be needed to revisit the optimal antiviral strategy, especially the initiation and duration of antiviral therapy in this particular setting.
References
Yeo W, Chan TC, Leung NW, et al. Hepatitis B virus reactivation in lymphoma patients with prior resolved hepatitis B undergoing anticancer therapy with or without rituximab. J Clin Oncol. 2009;27:605–611.
Hsu C, Tsou HH, Lin SJ, et al. Chemotherapy-induced hepatitis B reactivation in lymphoma patients with resolved HBV infection: a prospective study. Hepatology. 2014;59:2092–2100.
Han JW, Yang H, Lee HL, et al. Risk factors and outcomes of hepatitis B virus reactivation in hepatitis B surface antigen negative patients with hematological malignancies. Hepatol Res. 2015;46:657–668.
Jang JW, Kim YW, Lee SW, et al. Reactivation of hepatitis B virus in HBsAg-negative patients with hepatocellular carcinoma. PLoS ONE. 2015;10:e0122041.
Seto WK. Hepatitis B virus reactivation during immunosuppressive therapy: appropriate risk stratification. World J Hepatol. 2015;7:825–830.
Hui CK, Cheung WW, Zhang HY, et al. Kinetics and risk of de novo hepatitis B infection in HBsAg-negative patients undergoing cytotoxic chemotherapy. Gastroenterology. 2006;131:59–68.
Pattullo V. Prevention of hepatitis B reactivation in the setting of immunosuppression. Clin Mol Hepatol. 2016;22:219–237.
Seto WK, Chan TS, Hwang YY, et al. Hepatitis B reactivation in patients with previous hepatitis B virus exposure undergoing rituximab-containing chemotherapy for lymphoma: a prospective study. J Clin Oncol. 2014;32:3736–3743.
Vigano M, Vener C, Lampertico P, et al. Risk of hepatitis B surface antigen seroreversion after allogeneic hematopoietic SCT. Bone Marrow Transpl. 2011;46:125–131.
Park S, Kim K, Kim DH, et al. Changes of hepatitis B virus serologic status after allogeneic hematopoietic stem cell transplantation and impact of donor immunity on hepatitis B virus. Biol Blood Marrow Transpl. 2011;17:1630–1637.
Seto WK, Chan TS, Hwang YY, et al. Hepatitis B reactivation in occult viral carriers undergoing hematopoietic stem cell transplantation: a prospective study. Hepatology. 2017;65:1451–1461.
Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10:1–98.
Hwang JP, Somerfield MR, Alston-Johnson DE, et al. Hepatitis B virus screening for patients with cancer before therapy: American society of clinical oncology provisional clinical opinion update. J Clin Oncol. 2015;33:2212–2220.
Chang TT, Lai CL, Kew Yoon S, et al. Entecavir treatment for up to 5 years in patients with hepatitis B e antigen-positive chronic hepatitis B. Hepatology. 2010;51:422–430.
Chevaliez S, Hezode C, Bahrami S, Grare M, Pawlotsky JM. Long-term hepatitis B surface antigen (HBsAg) kinetics during nucleoside/nucleotide analogue therapy: finite treatment duration unlikely. J Hepatol. 2013;58:676–683.
Zoutendijk R, Hansen BE, van Vuuren AJ, Boucher CA, Janssen HL. Serum HBsAg decline during long-term potent nucleos(t)ide analogue therapy for chronic hepatitis B and prediction of HBsAg loss. J Infect Dis. 2011;204:415–418.
Wursthorn K, Jung M, Riva A, et al. Kinetics of hepatitis B surface antigen decline during 3 years of telbivudine treatment in hepatitis B e antigen-positive patients. Hepatology. 2010;52:1611–1620.
Zoutendijk R, Zaaijer HL, de Vries-Sluijs TE, et al. Hepatitis B surface antigen declines and clearance during long-term tenofovir therapy in patients coinfected with HBV and HIV. J Infect Dis. 2012;206:974–980.
Seto WK, Wong DK, Fung J, Huang FY, Lai CL, Yuen MF. Reduction of hepatitis B surface antigen levels and hepatitis B surface antigen seroclearance in chronic hepatitis B patients receiving 10 years of nucleoside analogue therapy. Hepatology. 2013;58:923–931.
Jang JW, Yoo SH, Kwon JH, et al. Serum hepatitis B surface antigen levels in the natural history of chronic hepatitis B infection. Aliment Pharmacol Ther. 2011;34:1337–1346.
Cornberg M, Wong VW, Locarnini S, Brunetto M, Janssen HLA, Chan HL. The role of quantitative hepatitis B surface antigen revisited. J Hepatol. 2017;66:398–411.
Fung J, Cheung KS, Wong DK, et al. Long-term outcomes and predictive scores for hepatocellular carcinoma and hepatitis B surface antigen seroclearance after hepatitis B e-antigen seroclearance. Hepatology. 2018;68:462–472.
Park YM, Lee SG. Clinical features of HBsAg seroclearance in hepatitis B virus carriers in South Korea: a retrospective longitudinal study. World J Gastroenterol. 2016;22:9836–9843.
Kuo TM, Hu CP, Chen YL, et al. HBV replication is significantly reduced by IL-6. J Biomed Sci. 2009;16:41.
Jang JW, Oh BS, Kwon JH, et al. Serum interleukin-6 and C-reactive protein as a prognostic indicator in hepatocellular carcinoma. Cytokine. 2012;60:686–693.
Prieto J. Inflammation, HCC and sex: IL-6 in the centre of the triangle. J Hepatol. 2008;48:380–381.
Shin EC, Sung PS, Park SH. Immune responses and immunopathology in acute and chronic viral hepatitis. Nat Rev Immunol. 2016;16:509–523.
Sonneveld MJ, Zoutendijk R, Flink HJ, Zwang L, Hansen BE, Janssen HL. Close monitoring of hepatitis B surface antigen levels helps classify flares during peginterferon therapy and predicts treatment response. Clin Infect Dis. 2013;56:100–105.
Li W, Zhao J, Zou Z, et al. Analysis of hepatitis B virus intrahepatic covalently closed circular DNA and serum viral markers in treatment-naive patients with acute and chronic HBV infection. PLoS ONE. 2014;9:e89046.
Funding
This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2016R1D1A1B03930457). Study sponsor has no role in study design, in the collection, analysis and interpretation of data.
Author information
Authors and Affiliations
Contributions
JWJ and HLL were involved in study concept and design, collecting and interpreting data, JWJ, HLL, JWH, SWL, SHB, JYC, NIH, SKY, H-JK, SL, S-GC, C-KM, D-WK and JWL contributed to reagents/materials/analysis tools, and JWJ and HLL wrote the paper. All authors have approved this final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no financial conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, H.L., Jang, J.W., Han, J.W. et al. Early Hepatitis B Surface Antigen Seroclearance Following Antiviral Treatment in Patients with Reactivation of Resolved Hepatitis B. Dig Dis Sci 64, 2992–3000 (2019). https://doi.org/10.1007/s10620-019-05614-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05614-6