Abstract
Background
Hepatitis B surface antigen (HBsAg)-negative/hepatitis B core antibody (HBcAb)-positive patients with undetectable serum hepatitis B virus (HBV) DNA have experienced and resolved hepatitis B virus (HBV) infection. Lymphoma patients with resolved HBV infection have high risk of HBV reactivation when treated with robust immunosuppressive agents, but the reported rate varies extensively between different studies. This study aims to estimate the risk of HBV reactivation in HBsAg-negative/HBcAb-positive patients receiving rituximab-containing chemotherapy for lymphoma.
Methods
Databases were searched for papers published in English until 8 August 2016. The pooled risk of HBV reactivation was estimated using a random-effects model.
Results
Data from 15 studies were retrieved, including a total of 1312 HBsAg-negative/HBcAb-positive lymphoma patients treated with rituximab-containing chemotherapy. The results revealed HBV reactivation rate of 9.0 % [95 % confidence interval (CI) 0.05–0.15]. In subgroup analysis, the reactivation rates for prospective and retrospective studies were 17 % (I 2 = 87.3 %; 95 % 0.08–0.39, p < 0.001) and 7 % (I 2 = 43.1 %; 95 % CI 0.05–0.11, p = 0.07), respectively.
Conclusions
This meta-analysis confirms a measurable and potentially substantial risk of HBV reactivation in HBsAg-negative/HBcAb-positive patients with rituximab treatment for lymphoma. Prophylactic use of anti-HBV agents should be seriously considered for such patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rituximab (R) is a chimeric anti-CD20 monoclonal antibody that can induce B cell lysis by antibody-dependent cellular cytotoxicity, resulting in apoptosis of B-cell lymphoma cells [1]. Chemotherapy consisting of R, cyclophosphamide, doxorubicin, vincristine, and prednisolone is currently considered the standard chemotherapy for diffuse large B-cell lymphoma [2]. A growing body of evidence suggests that HBV reactivation is associated with use of rituximab [3]. It is well recognized that HBsAg-positive patients who receive immunosuppressive or cytotoxic chemotherapy have a substantial possibility of developing HBV reactivation [4]. Cancer patients with “resolved” HBV infection [HBsAg negative and hepatitis B core antibody (HBcAb) positive] also carry a risk of chemotherapy-induced HBV reactivation [5]. In these patients, HBV may remain in covalently closed circular DNA in hepatocytes without obvious activity after clearance of HBsAg but could be reactivated when the immune system is suppressed by chemotherapy [6]. However, such reactivation rates vary extensively in different studies, ranging from 0 to 41.5 % [3, 7,8,9,10,11,12,13,14,15,16,17,18,19,20].
Therefore, we performed a systematic review of recent literature to estimate the risk of HBV reactivation in HBsAg-negative/HBcAb-positive patients receiving rituximab-based lymphoma therapy.
Materials and methods
Literature search strategy
We conducted searches using PUBMED and EMBASE (from 1996 to 8 August 2016) with the medical subject headlines of “Rituximab” and “Hepatitis B”. Search results were limited to English-language publications.
Study selection and data extraction
We limited studies to those including HBsAg-negative/HBcAb-positive and rituximab-treated patients with lymphoma. Reviews, case reports, and case series with fewer than five patients were excluded. Author Z.T. reviewed the titles and abstracts of all the identified studies. Authors X.L., Y.L., and Y.Q. reviewed the full text of all potentially eligible studies. Author S.W. reviewed the inclusion criteria of the reference list of studies to identify additional studies that met the eligibility criteria. Authors D.X., J.L., and X.L. designed the study and revised the manuscript.
The primary outcome of this meta-analysis was the rate of HBV reactivation in HBsAg-negative/HBcAb-positive patients treated for lymphoma using rituximab. HBV reactivation was defined as increase in alanine aminotransferase (ALT) >40 U/L with an increase in HBV DNA from baseline (including change from undetectable to detectable), and/or HBsAg seroconversion from negative to positive, and absence of clinical or laboratory features of acute infection with hepatitis A virus, hepatitis C virus, or other systemic infections.
Statistical analysis
The probability of HBV reactivation was estimated using a random-effects model. For the meta-analysis, we used the Cochrane heterogeneity chi-square test to determine whether the pooled estimates showed significant statistical heterogeneity, defined to be significant for p value <0.05. The I 2 statistic was used as a measure of heterogeneity in the selected study, with I 2 > 50 % indicating significant heterogeneity.
Results
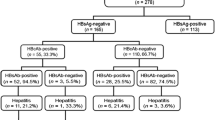
The selection process for trial inclusion is illustrated in Fig. 1. The literature search yielded 964 citations. After screening the titles and abstracts, 78 potentially eligible studies were taken into consideration, 15 of which were ultimately included (Table 1) [3, 7,8,9,10,11,12,13,14,15,16,17,18,19,20]. The selected studies included five prospective cohort studies [3, 7,8,9,10], nine retrospective studies [11,12,13,14,15,16,17,18,19], and one study with mixed prospective and retrospective design [20]. Among all 15 selected studies, 12 studies were completed in Asia (2 from Japan [12, 20], 8 from China [3, 8, 9, 11, 13,14,15,16], 1 from South Korea [19], and 1 from Singapore [7]), 2 from Europe [10, 17] (Italy), and 1 from North America (the USA) [18].
Figure 2 illustrates that the risk estimates for HBV reactivation ranged from 0 to 41.5 %. Using the random-effects model, the pooled standardized HBV reactivation rate (n = 15 studies) was 9.0 % (121 reactivations in 1312 patients; 95 % CI 0.05–0.15). However, significant heterogeneity was present (I 2 = 84 %; p < 0.001).
The source of statistical heterogeneity was explored by analyzing the data by study type (prospective versus retrospective studies). When the analysis was limited to the prospective studies, the HBV reactivation rate was 17 % (Fig. 3; I 2 = 87.3 % p < 0.001; 95 % CI 0.08–0.39). When the analysis was limited to the retrospective studies, the HBV reactivation rate was 7 % (Fig. 4; I 2 = 43.1 %; p = 0.07; 95 % CI 0.05–0.11).
Discussion
Lymphoma patients with “resolved” HBV infection carry a substantial risk of chemotherapy-induced HBV reactivation, but the reactivation rate varies extensively between different studies, ranging from 0 to 41.5 %. Increasing attention has been attracted to whether prophylactic anti-HBV treatment should be administered to patients with resolved HBV infection before rituximab treatment. In this study, we estimated a pooled rate of HBV reactivation rate of 9 % in these patients. The fairly high reactivation rate suggests that antiviral prophylaxis should be taken into consideration for all HBcAb-positive patients regardless of HBsAg status.
It is well recognized that treatment with prophylactic nucleos(t)ide analogs (NAs) should be recommended in chronic hepatitis B (CHB) patients with lymphoma during chemotherapy [5]. Currently, NAs available for clinical intervention include entecavir, adefovir, telbivudine, and tenofovir in addition to lamivudine. In one systematic analysis including 52 articles and 3892 HBsAg-positive participants, Zhang et al. evaluated the prophylactic efficacy of the five oral NAs on chemotherapy-induced HBV reactivation [21]. They found that prophylactic therapy with tenofovir and entecavir may be the most potent interventions for prevention of HBV reactivation. On the other side, after HBV reactivation, entecavir showed good treatment efficacy for suppression of HBV and was highly recommended [22].
The definition of HBV reactivation was not completely identical across the 15 included studies. In this study, we chose a rather loose definition of HBV reactivation, i.e., ALT >1 ULN with HBV DNA increase and/or HBsAg reappearance, in order to include those patients with mild HBV DNA increase but who still had substantial risk of suffering liver damage, liver failure, or even death. A previous meta-analysis reported a 6.3 % HBV reactivation rate [23], lower than the pooled rate (9.0 %) obtained in this study. In comparison with our study, the previous study used a stricter definition of HBV reactivation (ALT >3 ULN with HBV DNA increase and/or HBsAg reappearance), and analyzed fewer patients (578 patients versus 1312 patients in our study). These two factors may account for the difference in the estimated rate of HBV reactivation between the two studies.
HBV genotype is suggested to be a factor associated with the virulence and natural history of HBV, possibly impacting on nucleotide-analog-resistant mutations and the risk of cirrhosis, liver failure, and hepatocellular carcinoma [24]. In this meta-analysis, not all retrieved studies provided HBV genotype information. Therefore, it was hard to judge whether HBV genotype would affect the probability of reactivation during immunosuppression. However, one study reviewed that the HBV reactivation rates did not vary significantly between regions (Asia versus Europe) [23]. Given the fact that the genotype distribution varies by region, i.e., genotypes A and D predominate in Europe while genotypes B and C predominate in Asia, it is very unlikely that genotype is a factor influencing HBV reactivation.
The most important source of heterogeneity in this study was likely to be study design. Prospective studies normally use a more accurate definition of HBV reactivation with closer and systematic surveillance for HBV reactivation. As a result, it is likely that the prospective studies provide an estimate of the risk of HBV reactivation that is closer to the true risk. We supplemented recent studies and pooled nine retrospective and five prospective studies that met the inclusion criteria. The results showed that prospective studies tended to report higher rates of HBV reactivation compared with retrospective studies (17 versus 7 %). Besides, studies varied with regard to how long patients were monitored for HBV reactivation. Recent data suggest that the risk of HBV reactivation persists for months after rituximab therapy [25], thus studies that followed up patients for a longer time may be more likely to recognize HBV reactivation. In this review, the follow-up duration for the included studies ranged from 1.1 to 116.3 months.
There are two major limitations to our meta-analysis. One is the high heterogeneity among the retrieved studies, which might influence precise evaluation of the estimated rate of HBV reactivation. Another is that comparison of HBsAg-negative/HBcAb-positive/hepatitis B surface antibody (HBsAb)-negative patients with HBsAg-negative/HBcAb-positive/HBsAb-positive patients was not performed due to the lack of HBsAb information in some retrieved studies. Nevertheless, HBsAb positivity was recently reported to be associated with decreased risk of reactivation in patients with resolved HBV receiving rituximab chemotherapy for lymphoma without antiviral prophylaxis [26].
In summary, our meta-analysis confirms a measurable and potentially substantial risk of HBV reactivation in HBsAg-negative/HBcAb-positive patients with rituximab treatment for lymphoma. This study furthers knowledge on prophylactic use of anti-HBV agents in such patients.
References
Smith MR. Rituximab (monoclonal anti-CD20 antibody): mechanisms of action and resistance. Oncogene 2003;22:359–368
Feugier P, Van Hoof A, Sebban C, Solal-Celigny P, Bouabdallah R, Fermé C, et al. Long-term results of the R-CHOP study in the treatment of elderly patients with diffuse large B-cell lymphoma: a study by the Groupe d’Etude des Lymphomes del’Adulte. J Clin Oncol 2005;23:4117–4126
Yeo W, Chan TC, Leung NW, Lam WY, Mo FK, Chu MT, et al. Hepatitis B virus reactivation in lymphoma patients with prior resolved hepatitis B undergoing anticancer therapy with or without rituximab. J Clin Oncol 2009;27:605–611
Loomba R, Liang TJ. Hepatitis B reactivation associated with immune suppressive and biological modifier therapies: current concepts, management strategies, and future directions. Gastroenterology 2017;152:1297–1309
Merli M, Rattotti S, Gotti M, Arcaini L. Antiviral therapies for managing viral hepatitis in lymphoma patients. Expert Opin Pharmacother 2017;18:363–376
Yuen MF, Wong DK, Fung J, Ip P, But D, Hung I, et al. HBsAg seroclearance in chronic hepatitis B in Asian patients: replicative level and risk of hepatocellular carcinoma. Gastroenterology 2008;135:1192–1199
Koo YX, Tay M, Teh YE, Teng D, Tan DS, Tan IB, et al. Risk of hepatitis B virus (HBV) reactivation in hepatitis B surface antigen negative/hepatitis B core antibody positive patients receiving rituximab-containing combination chemotherapy without routine antiviral prophylaxis. Ann Hematol 2011;90:1219–1223
Seto WK, Chan TS, Hwang YY, Wong DK, Fung J, Liu KS, et al. Hepatitis B reactivation in patients with previous hepatitis B virus exposure undergoing rituximab-containing chemotherapy for lymphoma: a prospective study. J Clin Oncol 2014;32:3736–3743
Hsu C, Tsou HH, Lin SJ, Wang MC, Yao M, Hwang WL, et al. Chemotherapy-induced hepatitis B reactivation in lymphoma patients with resolved HBV infection: a prospective study. Hepatology 2014;59:2092–2100
Persico E, De Renzo A, La Mura V, Bruno S, Masarone M, Torella R, et al. Occult hepatitis B virus infection in patients with non Hodgkin lymphoma: the need for early diagnosis in anti-Hbc positive patients. Gut 2007;56:1470–1471
Ji D, Cao J, Hong X, Li J, Wang J, Chen F, et al. Low rate of hepatitis B virus reactivation during chemotherapy among diffuse large B-cell lymphoma patients who are HBsAg-negative/HBcAb-positive: a multicenter retrospective study. Eur J Haematol 2010;85:243–250
Matsue K, Kimura S, Takanashi Y, Iwama K, Fujiwara H, Yamakura M, et al. Reactivation of hepatitis B virus after rituximab-containing treatment in patients with CD20-positive B-cell lymphoma. Cancer 2010;116:4769–4776
Lu S, Xu Y, Mu Q, Cao L, Chen J, Zhu Z, et al. The risk of hepatitis B virus reactivation and the role of antiviral prophylaxis in hepatitis B surface antigen negative/hepatitis B core antibody positive patients with diffuse large B-cell lymphoma receiving rituximab-based chemotherapy. Leuk Lymphoma 2015;56:1027–1032
Wu CY, Hsiao LT, Chiou TJ, Gau JP, Liu JH, Yu YB, et al. Lymphocyte/monocyte ratio and cycles of rituximab-containing therapy are risk factors for hepatitis B virus reactivation in patients with diffuse large B-cell lymphoma and resolved hepatitis B. Leuk Lymphoma 2014;56:2357–2364
Chen KL, Chen J, Rao HL, Guo Y, Huang HQ, Zhang L, et al. Hepatitis B virus reactivation and hepatitis in diffuse large B-cell lymphoma patients with resolved hepatitis B receiving rituximab-containing chemotherapy: risk factors and survival. Chin J Cancer 2015;34:225–236
Hsiao LT, Chiou TJ, Gau JP, Yang CF, Yu YB, Liu CY, et al. Risk of reverse seroconversion of hepatitis B virus surface antigen in rituximab-treated non-Hodgkin lymphoma patients: a large cohort retrospective study. Medicine (Baltimore) 2015; 94:e1321
Targhetta C, Cabras MG, Mamusa AM, Mascia G, Angelucci E. Hepatitis B virus-related liver disease in isolated anti-hepatitis B-core positive lymphoma patients receiving chemo- or chemo-immune therapy. Haematologica 2008;93:951–952
Méndez-Navarro J, Corey KE, Zheng H, Barlow LL, Jang JY, Lin W et al. Hepatitis B screening, prophylaxis and re-activation in the era of rituximab-based chemotherapy. Liver Int 2011;31:330–339
Oh MJ, Lee HJ. A study of hepatitis B virus reactivation associated with rituximab therapy in real-world clinical practice: a single-center experience. Clin Mol Hepatol 2013;19:51–59
Fukushima N, Mizuta T, Tanaka M, Yokoo M, Ide M, Hisatomi T, et al. Retrospective and prospective studies of hepatitis B virus reactivation in malignant lymphoma with occult HBV carrier. Ann Oncol 2009;20:2013–2017
Zhang MY, Zhu GQ, Zheng JN, Cheng Z, Van Poucke S, Shi KQ, et al. Nucleos(t)ide analogues for preventing HBV reactivation in immunosuppressed patients with hematological malignancies: a network meta-analysis. Expert Rev Anti-infective Ther 2017;15:503–513
Huang H, Li X, Zhu J, Ye S, Zhang H, Wang W, et al. Entecavir vs lamivudine for prevention of hepatitis B virus reactivation among patients with untreated diffuse large B-cell lymphoma receiving R-CHOP chemotherapy: a randomized clinical trial. JAMA 2014; 312:2521–2530
Mozessohn L, Chan KK, Feld JJ, et al. Hepatitis B reactivation in HBsAg-negative/HBcAb-positive patients receiving rituximab for lymphoma: a meta-analysis. J Viral Hepat 2015; 22(10):842
Tian Q, Jia J. Hepatitis B virus genotypes: epidemiological and clinical relevance in Asia. Hepatol Int 2016;10:854–860
Huang YH, Lin HC, Lee SD. Reply to S. Kusumoto et al. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology 2013; 31(35):4481
Paul S, Dickstein A, Saxena A, et al. Role of surface antibody in hepatitis B reactivation in patients with resolved infection and hematologic malignancy: a meta-analysis. Hepatology 2017. doi:10.1002/hep.29082
Acknowledgements
This work was supported by the National Natural Science Foundation (81373136, 81572010), Application Research of Capital Clinical Characteristic and Promotion of Achievements (Z151100004015011), and the Capital Health Development Research Special Independent Innovation Project (2016-2-5032).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Zilin Tang, Xiaodong Li, Shunquan Wu, Yan Liu, Qiao Yan, Dongping Xu, and Jin Li declare that there are no conflicts of interest.
Human and animal rights statement
This study was approved by the ethics committee of Beijing 302 Hospital. This article does not contain any studies with human or animal subjects.
Rights and permissions
About this article
Cite this article
Tang, Z., Li, X., Wu, S. et al. Risk of hepatitis B reactivation in HBsAg-negative/HBcAb-positive patients with undetectable serum HBV DNA after treatment with rituximab for lymphoma: a meta-analysis. Hepatol Int 11, 429–433 (2017). https://doi.org/10.1007/s12072-017-9817-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-017-9817-y