Abstract
Background
Computed tomography (CT) and magnetic resonance (MR) enterography are now widely used to diagnose and monitor Crohn’s disease.
Aim
We sought to assess the use of enterography for management of inflammatory bowel disease (IBD) in our medical center.
Methods
We performed a retrospective review of all patients diagnosed with IBD who underwent MR or CT enterography from November 1, 2010 to October 25, 2012 at our institution. We assessed disease complications identified by enterography, agreement between disease activity determined by endoscopy and enterography, association between inflammatory markers and enterography-determined disease activity and recommended changes in medical and surgical management following enterography.
Results
A total of 311 enterography studies (291 MR and 20 CT enterographies) were performed on 270 patients, including 258 (83.0 %) on patients with presumed Crohn’s disease and 53 (17.0 %) with presumed ulcerative colitis. Active small bowel (SB) disease was noted in 73/311 (23.5 %) studies. Complications including strictures, perianal fistulas, abscesses and SB fistulas were noted in 108/311 (34.7 %) studies. Endoscopic and enterography defined active disease had an agreement of κ = 0.36 in the ileum (n = 179). A total of 142/311 (45.7 %) enterographies were associated with recommended medication changes within 90 days while surgery or endoscopic dilation of stricture was recommended following 41/311 (13.2 %) enterographies. Enterography resulted in a change in diagnosis from ulcerative colitis to Crohn’s in 5/311 (1.6 %) studies.
Conclusion
Enterography reveals active disease and complications not evident on endoscopy and should be considered in the initial diagnosis, assessment of disease activity, and monitoring of therapy in patients with IBD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease is a complex chronic inflammatory disease affecting all portions of the gastrointestinal tract [1]. The natural history of Crohn’s disease is variable with most patients having a chronic intermittent disease course. Approximately 10 % of patients with Crohn’s disease have a prolonged remission, while up to two-thirds experience complications such as strictures, fistulas and abscesses and frequently require surgery [2, 3]. Esophagogastroduodenoscopy (EGD) and ileocolonoscopy can only assess a small portion of the small bowel, which is the part of the bowel that is most commonly affected by Crohn’s disease. Historically, radiographic assessment of the small bowel relied on fluoroscopic techniques including small bowel follow through and small bowel enteroclysis, however these techniques have largely been replaced by cross-sectional imaging techniques including computed tomography (CT) and magnetic resonance (MR) imaging [4, 5]. Enterography involves the ingestion of a large amount of contrast resulting in distension of the small bowel. This allows for identification of luminal disease and can distinguish true bowel wall thickening from underdistension [6, 7]. Unlike enteroclysis, which relies on an enteric tube for the administration of contrast, enterography is performed following the oral ingestion contrast. Since cross-sectional techniques using oral contrast agents are reliable and better tolerated than enteroclysis [8, 9], enteroclysis is not as commonly used in clinical practice.
Cross-sectional enterography techniques are playing an increasingly important role in the diagnosis and monitoring of inflammatory bowel disease (IBD) and have several advantages over traditional barium fluoroscopic evaluation of small intestinal disease. CT enterography (CTE) and MR enterography (MRE) provide more complete evaluation of mural disease as well as allowing assessment of extra-luminal complications of Crohn’s disease [10–15]. In addition, cross-sectional enterography may augment diagnostic colonoscopy by identifying Crohn’s disease of the small bowel proximal to the terminal ileum [16]. Enterography techniques are also being studied in ulcerative colitis, as these can be used to evaluate the colon and post-surgical ileal pouch [17] and can identify small bowel inflammation that could change the diagnosis to Crohn’s disease.
Early use of cross-sectional enterography in IBD utilized CT techniques and provided excellent assessment of disease activity and complications [6]. However, concerns about radiation exposure have limited the use of CTE [18]. Patients with IBD are at risk of recurrent imaging studies over time, rendering them susceptible to excessive radiation exposure [19]. The desire to avoid radiation exposure is one factor that has led to the increasing use of MRE, which has been shown to be a cost-effective alternative for radiation-free evaluation of the small bowel, particularly in younger patients [20].
Previous studies have reported similar sensitivity in the detection of small bowel disease using CTE and MRE [12, 21]. Although CTE and MRE have come into widespread clinical practice, there are few large studies discussing how they are actually used in clinical practice. In addition, there is very limited literature describing CTE and MRE findings in a large clinical series of IBD patients and how they may affect clinical decision-making. In this study, we hope to provide additional insights regarding the use of multimodality enterography in clinical practice by reviewing findings from MRE and CTE studies performed on patients at our IBD center. We report how disease activity determined by enterography correlates with endoscopic findings and laboratory markers of inflammation. In addition, we review changes in diagnosis and management based on MRE and CTE findings as well as the utility of serial imaging.
Methods
Study Design and Patient Population
This is a retrospective review of patients who received MRE and/or CTE studies at the UC San Diego (UCSD) Health System IBD Center. Electronic medical records were searched for all patients seen in the gastroenterology clinic between November 1, 2010 and October 25, 2012 carrying an IBD or IBD related ICD-9 diagnosis code. This information was cross-referenced with a registry of UCSD radiology imaging tests to obtain a list of patients who received one or more MRE and/or CTE studies during this time period. Imaging results, endoscopy results, laboratory information and treatment information were reviewed for these patients. The study was approved by the University of California, San Diego institutional review board.
Magnetic Resonance and Computed Tomography Enterography Evaluation
All patients in this study underwent MRE or CTE according to the standard protocols used at UCSD. All patients who underwent MRE ingested approximately 1,750 mL of oral VoLumen (EZ-E-M, Westbury, NY), a low-density barium sulfate contrast agent prior to examination. For MRE, patients were studied in the prone position. Using a 1.5 Tesla MR scanner, multiplanar single shot fat spin echo sequences with and without fat saturation, steady state free precession sequences, and axial dual echo sequences were obtained. Following the administration of MultiHance (Bracco Diagnostics, Princeton, NJ) intravenous contrast, post-contrast dynamic images through the abdomen were obtained. Patients also received a total of 1 mg of Glucagon (Eli Lilly, Indianapolis, IN) during the exam. This MRE technique was consistent with previously described protocols [7].
Patients who underwent a CTE were scanned in the supine position. Multiple helical images were obtained through the abdomen and pelvis following the administration of 100 mL of Omnipaque 350 (GE Healthcare, Princeton, NJ) intravenous contrast. Enteric phase imaging of the abdomen and pelvis was performed as noted in previously described CTE protocols [6].
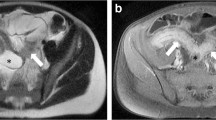
All studies were reviewed by radiologists at UCSD experienced in the evaluation of MRE and CTE. Study quality was assessed to determine whether adequate small bowel distension and minimal motion artifact were achieved. Studies were evaluated for the presence of small and large bowel disease activity as well as complications including strictures, abscesses, sinus tracts, fistulas and perianal disease if pelvic views were obtained. The small bowel was specifically assessed for the presence of mural thickening or stratification, abnormal bowel wall enhancement, vascular engorgement, bowel wall edema and presence of enlarged or reactive lymph nodes, all of which are radiographic signs of active inflammation in Crohn’s disease [22–24]. Disease activity was determined by the radiologist based on these findings. MRE studies of two patients with radiographic evidence of active disease are shown in Figs. 1 and 2.
Magnetic resonance enterography axial single shot fast spin echo fat saturated image of a patient with Crohn’s disease demonstrates increased signal in the wall of the distal ileum (black arrow, a) consistent with edema. Mural thickening and engorgement of the vasa recta is shown on the delayed post-contrast imaging (white arrows, b). These findings suggest a long segment of active inflammation in the distal ileum
Magnetic resonance enterography coronal single shot fast spin echo (SSFSE) image of a patient with Crohn’s disease demonstrates focal wall thickening of the terminal ileum (arrow, a), mural edema as evidence by increased signal on the fat saturated SSFSE image (b), and hyperenhancement following intravenous contrast (c). A focal outpouching along the medial margin of the terminal ileum represents an ulcer. The combination of these findings is consistent with active inflammation
Endoscopic Evaluation
Electronic medical records were reviewed for all endoscopies performed within 60 days of enterography evaluation. These included EGD, colonoscopy, flexible sigmoidoscopy, double balloon enteroscopy as well as pouchoscopy and ileoscopy in patients with prior bowel surgery. Endoscopies were specifically distinguished based on evaluation of the ileum (i.e. colonoscopy with terminal ileum intubation, pouchoscopy with evaluation of the pre-pouch ileum and ileoscopy), attempted but failed evaluation of the ileum (i.e. colonoscopy with unsuccessful terminal ileum intubation) and studies in which evaluation of the ileum was not attempted (i.e. EGD, flexible sigmoidoscopy). Endoscopic and histologic findings were reviewed for the presence and location of disease activity.
Laboratory Evaluation
Laboratory data was reviewed for any studies of the inflammatory markers erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) that were obtained based on provider discretion. ESR and CRP values obtained within 60 days of an enterography study were analyzed.
Clinical Evaluation
Electronic medical records were reviewed for clinic visits prior to and following the enterography study. Diagnosis and indication for ordering the MRE or CTE were obtained. Subsequent clinic visits were reviewed for any change in medical or surgical management recommended within 90 days of the MRE or CTE study. Changes in medical or surgical management included a change in diagnosis, initiation or discontinuation of a medication for treatment of IBD, change in medication dose, or referral for therapeutic procedure or surgery (including endoscopic dilation of stricture, large and small bowel surgery as well as perianal surgery).
Statistical Analysis
The two-sample t test was used for comparison of continuous variables between groups. A two-sided p value < 0.05 was considered statistically significant. Study concordance between enterography and endoscopy was determined using the kappa correlation coefficient for inter-study agreement. Accuracy of inflammatory markers as diagnostic tools was determined using receiver operating characteristic (ROC) methodology. Statistical analysis was performed using SPSS (Somers, NY).
Results
Patient Demographics
Between November 1, 2010 and October 25, 2012, 911 patients were evaluated in the gastroenterology clinic carrying a diagnosis code related to IBD. Amongst these, 270 patients had at least one MRE or CTE study performed at UCSD. The average age of patients (±standard deviation) was 41.1 (±16.4) and 45.9 % were male (Table 1). A total of 217 patients (80.4 %) carried a diagnosis of Crohn’s disease while 53 (19.6 %) carried a diagnosis of ulcerative colitis. Most patients (87.0 %) had only one enterography study during the study time period; however, 11.1 % had two enterography studies and 1.9 % had three to five studies during this time period. A total of 311 enterographies were performed, including 291 MRE studies and 20 CTE studies. Amongst these, 258 (83.0 %) were performed in patients diagnosed with Crohn’s disease and 53 (17.0 %) were performed in patients diagnosed with ulcerative colitis.
Magnetic Resonance and Computed Tomography Enterography Disease Activity
Amongst 311 enterography studies, 134 (43.1 %) showed radiographic evidence of small bowel disease including 131 (42.1 %) with disease noted in the ileum and 8 (2.6 %) with disease noted in the jejunum (Table 2). Seventy-three of these (23.5 %) had MRE or CTE findings consistent with active small bowel disease including 71 (22.9 %) with active disease of the ileum and 5 (1.6 %) with active disease of the jejunum. Active colonic disease was noted in 68 studies, or 24.2 % of the 281 studies performed in patients without a prior colectomy. Complications of IBD were noted in 108 studies (34.7 %) and included 62 patients (19.9 %) with small bowel or colon strictures, 25 (8.0 %) with perianal fistulas, 25 (8.0 %) with small bowel fistulas or sinus tracts and 15 (4.8 %) with abscess formation.
MR enterography and CT enterography studies were evaluated for several radiographic characteristics of small bowel disease activity. All 73 studies with active small bowel disease noted on enterography had abnormal mural enhancement. Of those studies with active small bowel disease, 71 (97.2 %) had mural thickening or stratification, 41 (56.2 %) had bowel wall edema, 32 (43.8 %) had enlarged lymph nodes and 26 (35.6 %) had vascular engorgement (Fig. 3).
Thirty-five patients had multiple enterographies during the study period ranging from two to five per patient. In 42 follow-up MREs, 16 (38.1 %) showed predominantly improved findings, 15 (35.7 %) showed predominantly stable findings, and 11 (26.2 %) showed predominantly worsening findings.
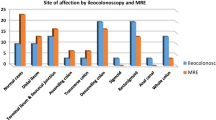
Endoscopic Disease Activity
Endoscopy was performed within 60 days of enterography in 216 cases and included 179 cases with evaluation of the ileum (Fig. 4). Evaluation of ileum was not attempted in 28 cases in which patients received EGD and/or flexible sigmoidoscopy. In addition, evaluation of the ileum was attempted and was unsuccessful in nine cases due to colonoscopy with impassable stricture or inability to intubate the terminal ileum. Endoscopy studies with adequate evaluation of the ileum included colonoscopy with terminal ileum intubation, ileoscopy in patients with prior ileostomy, and pouchoscopy in patients with prior ileoanal pouch. Active ileal disease was noted in 70 of 179 (39.1 %) endoscopy studies with evaluation of the ileum and in 38 of 179 (21.2 %) of the corresponding enterography studies (Table 3). The kappa agreement between endoscopy and enterography ileal disease activity amongst 179 cases with endoscopy evaluation of the ileum (i.e. efficacy analysis) was 0.36 (95 % confidence interval 0.23–0.49). Nine enterography studies demonstrated signs of active ileal disease that were not noted on endoscopic evaluation. Additionally, an effectiveness analysis was performed including the 179 cases with endoscopy evaluation of the ileum and nine additional cases with failed endoscopic ileal evaluation that were treated as negative values (no active ileal disease on endoscopy). The kappa agreement between endoscopy and enterography ileal disease activity (i.e. effectiveness analysis) was 0.33 (95 % confidence interval 0.20–0.47) (Table 3). Four of nine patients with failed endoscopic ileal evaluation had active disease of the ileum noted on enterography.
A total of 198 patients received endoscopic evaluation of the colon within 60 days of their enterography study, which included either colonoscopy or flexible sigmoidoscopy. The kappa agreement between large bowel active disease noted on endoscopy and enterography is provided in Table 4 in the online supplement. It should be noted that enterography was not optimized for evaluation of the colon, as rectal contrast was not administered.
Laboratory Evaluation
Amongst 311 enterography studies, ESR was evaluated within 60 days of enterography in 120 studies (38.6 %) and CRP was evaluated within 60 days of enterography in 126 studies (40.5 %). As shown in Fig. 5, ESR was higher in 59 patients with active disease noted on enterography (22.5 ± 20.7 mm/h) than in 61 patients without evidence of active disease on enterography (16.3 ± 17.9 mm/h); however, the difference was not significant (p = 0.08, ref range = 0–20 mm/h). CRP was significantly higher in 59 patients with active disease on enterography (0.94 ± 1.15 mg/dL) than in 67 patients without active disease on enterography (0.47 ± 0.82 mg/dL, p < 0.05, ref range 0–0.5 mg/dL). The area under the receiver operating characteristic curves were estimate as 0.62 for ESR (95 % confidence interval 0.51–0.73) and 0.65 for CRP (95 % confidence interval 0.55–0.76), respectively.
Enterography disease activity association with ESR and CRP. ESR erythrocyte sedimentation rate (ref range 0–20 mm/h), CRP c-reactive protein (ref range 0–0.5 mg/dL). Active disease refers to enterography studies with evidence of active small or large bowel disease. Mean values shown with p value based on two-tailed t test
Clinical Evaluation
A total of 142 of 311 (45.7 %) CTE and MRE studies yielded findings that resulted in a recommended medication change within 90 days (Fig. 6). These included 37 patients who were started on an anti-tumor necrosis factor (anti-TNF) medication, 40 patients who were started on combination therapy with an anti-TNF and immunomodulator (thiopurine or methotrexate), 14 patients who were started on corticosteroids, 13 patients who were started on a thiopurine alone, eight patients who were started on antibiotics, 14 patients who required a dose increase in their anti-TNF medication and 16 patients who had various other medication changes (Fig. 6, footnote).
Clinical management and diagnosis changes associated with enterography. anti-TNF anti-tumor necrosis factor, UC ulcerative colitis. Percentages are based on 311 enterography studies. Combination treatment refers to anti-TNF and thiopurine or anti-TNF and methotrexate. Colon surgery refers to partial or total colectomy. Small bowel surgery refers to small bowel resection or stricturoplasty. *Other medication change refers to four patients started on 5-aminosalicylic acid, three started on bile acid sequestrants, three started on a combination of systemic steroids, antibiotics and anti-TNF, two started on systemic steroids and antibiotics, two patients in which anti-TNF was discontinued and two patients in which thiopurine was discontinued. **Other surgery refers to two patients referred for exploratory laparotomy and lysis-of-adhesions and one referred for ileostomy takedown
In addition, enterography was associated with a referral for endoscopic dilation of strictures in 11 of 311 studies (3.5 %) and referral for surgery in 30 of 311 (9.6 %) studies. These included 11 patients referred for small bowel resection or stricturoplasty, seven referred for colonic resection, six referred for surgical treatment of perianal fistulas, three referred for ileocecal resection and three referred for other surgeries. Enterography findings also resulted in a change in diagnosis from ulcerative colitis to Crohn’s disease in five patients (1.6 %).
Discussion
The major advantages of CTE or MRE over traditional cross sectional or small bowel series imaging techniques are their ability to evaluate for multiple different signs of Crohn’s disease beyond the reach of traditional endoscopes including transmural disease or extra-luminal disease complications. Evaluation of mural enhancement, edema and thickening as well as vascular engorgement and surrounding reactive lymphadenopathy provide an assessment of transmural disease activity that is not provided by fluoroscopic techniques or endoscopy alone. This assessment may be valuable when trying to differentiate inflammatory from fibrostenotic strictures, as the treatment differs for these entities.
In this retrospective review of MRE and CTE studies at our center, we demonstrate that active small bowel disease and luminal and transmural complications are commonly identified in patients with Crohn’s disease undergoing enterography. In our study, transmural and extra-luminal complications were frequently identified, a fair agreement between disease activity identified on endoscopy and enterography was noted, and elevation in inflammatory markers was associated with enterography disease activity. This study confirms that findings on enterography are associated with changes in treatment, surgical intervention and diagnosis of IBD.
In our study, 23.2 % of patients were identified to have penetrating complications, including 18.3 % with fistulas or sinus tracts and 4.8 % with abscesses. Prior studies have shown similar findings, with penetrating complications in approximately 20 % of patients with known or suspected Crohn’s disease undergoing CT or MR enterography [25, 26]. A major concern regarding the use of CT and MR enterography is whether these studies are sufficiently accurate to determine disease activity. One way to assess this is to correlate enterography findings with disease activity identified on endoscopy as well as histology, which are considered the gold standard for monitoring disease activity in IBD. Previous studies have also shown a significant correlation between disease activity on enterography and histology from surgically resected bowel [27–29] as well as Crohn’s disease activity index (CDAI) score [30]. Prior studies have shown a strong association between disease activity identified on endoscopy and enterography, suggesting that enterography may be a reasonable tool for monitoring disease activity in IBD. A retrospective review of patients with Crohn’s disease by Colombel et al. [31] found that CT enterography findings of active ileal disease correlated with endoscopic and histologic severity scores (r 2 = 0.33–0.39), with CT findings of bowel enhancement having the strongest correlation with histologic inflammation. Gallego et al. [32] performed a prospective study on 61 patient with Crohn’s disease in 2011 and found good agreement between endoscopy and MRE in identifying inactive, mild, or moderate to severe ileal disease (κ = 0.60). Similarly, a retrospective study by Grand et al. [33] showed high sensitivity (85 %) and specificity (80 %) for MRE (κ = 0.65) when comparing to endoscopy as the gold standard in 310 patients with known or suspected Crohn’s who underwent endoscopy within 90 days of MRE. In our study, agreement between active disease of the ileum identified on endoscopy and enterography was slightly lower than in the previously described literature (κ = 0.36). This may be explained by the time interval of up to 60 days between enterography and endoscopy studies, which allows for possible treatment changes to affect disease activity in this time interval. Active ileal disease was noted on enterography in nine cases without evidence of active disease on endoscopy. Since ileal inflammation can spare the distal terminal ileum [16], this disease activity may not have been identified on ileocolonoscopy. This would further emphasize the importance of enterography studies in complementing endoscopy in the diagnosis and staging of Crohn’s disease. In addition, enterography was necessary in our study to identify active ileal disease in four of nine cases in which colonoscopy with ileal intubation was unsuccessful.
With the increasing concerns of cumulative radiation exposure in patients with IBD, MRE is replacing CTE as the optimal enterography technique [20, 34, 35]. Our institution performed far more MRE studies than CTE studies (291 vs. 20) in the time period reviewed, due to both the lack of radiation associated with MRE as well as local expertise in reading MRE. Most prior studies have shown similar sensitivities in detecting small bowel disease using these two techniques, but concerns remain regarding reduced image quality and lower inter-observer agreement using MRE as compared to CTE [21, 36, 37]. One prospective study by Fiorina et al. [38] showed improved detection of small bowel strictures and inflammation with MRE compared to CTE. One of the most important operating characteristics of small bowel imaging studies for small bowel Crohn’s disease is the ability to assess the chronicity and functionality of a stricture. This can be best assessed using MRE and is not feasible using CTE due to the large amounts of radiation that would be required to perform dynamic imaging. Our study was not powered to assess differences in sensitivity or specificity of findings between techniques. However, both techniques identified findings that assisted in decision-making. To minimize radiation exposure to our patients with IBD, we have adopted a practice of performing MRE as opposed to CTE (in the absence of contraindications to MR) on patients undergoing an enterography study. In patients over 50, we perform either CTE or MRE, depending on the clinical scenario, but the vast majority of patients choose MRE in order to avoid radiation exposure.
The inflammatory markers ESR and CRP are often evaluated and monitored in patients with IBD. In the present study, receiver operator curves showed that ESR and CRP are modest predictors of disease activity noted on enterography. The association between inflammatory markers and disease activity as measured on enterography varies from study to study. Colombel et al. [31] showed that CRP concentrations in patients with Crohn’s disease were associated with CTE evidence of peri-enteric inflammation, but not with bowel enhancement. A retrospective study of patients with IBD by Solem et al. [39] showed that CRP concentrations correlated with endoscopy and histologic disease activity, however did not correlate with radiographic disease activity noted on small bowel follow through and CTE. Conversely, Sauer et al. [40] showed that CRP is significantly higher in pediatric Crohn’s disease patients with active disease on MRE. Overall, these findings further characterize the relatively low sensitivity and specificity of these laboratory values.
Our study suggests that enterography should play an integral role in the assessment of disease activity and complications in patients with Crohn’s disease. Furthermore, our observations suggest that findings of disease activity and complications such as strictures, fistulas, and abscesses identified on MRE and CTE are commonly associated with changes in medical and surgical management. In our cohort, disease activity on enterography was linked to initiation of anti-TNF therapy and combination therapy in many patients as well as initiation of other therapeutics. Identification of active disease, strictures and other complications was also linked to referral for small bowel resection, stricturoplasty, endoscopic dilation and other procedures.
MR has been shown to be useful in patients with ulcerative colitis to assess disease activity and extent of disease [41]. A total of 5–13 % of patients who have presumed ulcerative colitis are later diagnosed with Crohn’s disease after colectomy [42–46]. Enterography has a potential role to look for signs of small bowel disease that could help categorize a patient into Crohn’s disease, which would affect a patient’s subsequent medical and surgical management. In our practice, we ordered 53 MR enterographies in patients with ulcerative colitis and in five patients small bowel findings on enterography led to a change in diagnosis from ulcerative colitis to Crohn’s disease. The reasons for ordering an MR enterography varied from patient to patient. However, Crohn’s disease was suspected in many of them, due to persistent abdominal pain or diarrhea after colectomy, history of small bowel obstructions, persistent pouchitis or pouch fistulas.
Enterography provided valuable information regarding the worsening or improvement of disease activity in patients who received serial studies. In our study, serial enterography was valuable in monitoring changes in disease activity in patients undergoing treatment. A prior study by Bruining et al. used serial CTE studies to identify responders, partial responders and non-responders to treatment [47]. Enterography findings did not agree strongly with clinical or endoscopic evaluation of disease activity, suggesting that serial enterography may provide additional information regarding mural inflammation and healing that is not provided by other methods. Indeed, for patients in whom the location of disease is not within reach of a standard endoscope, MRE could potentially be used as the primary modality for monitoring that patient’s disease. Several other studies have reviewed the utility of enterography in the clinical setting. A retrospective review of 120 patients with Crohn’s by Messaris et al. [28] illustrated that disease activity assessed by MRE correlated with the need for medical or surgical intervention. A similar retrospective review by Ha et al. showed that MRE assisted in directing changes in clinical management, including escalation of medical therapy and surgical management, in 119 patients with Crohn’s disease [29]. This was particularly true in patients presenting with obstructive symptoms. CT and MR enterography may also provide new evidence of stricture formation when such findings are not expected based on clinical assessment alone [48] and significantly impact practitioner confidence regarding the presence or absence of small bowel disease [49]. In addition, a study by Booya et al. [50] showed that enterography may result in a change in medical or surgical management by identifying occult fistulas and abscesses.
Enterography complements endoscopy in evaluating disease activity and is the best method for assessing for disease-related complications. Enterography may also result in identification of incidental findings that can lead to increased patient morbidity from additional testing of benign conditions [51].
Implications for Future Studies
Further studies are needed to better characterize the impact of enterography on clinical practice and review how enterography may play a role in physician decision making independent of endoscopy and clinical findings. In addition, future studies will likely evaluate new techniques and applications for enterography. These include the study of terminal ileum motility on enterography as a marker of disease activity [52], the use of positron emission tomography (PET) in conjunction with enterography to identify disease activity [53] as well as new MRI sequences and techniques [54, 55]. Additionally, the use of objective markers of disease activity based on quantitative assessment of the imaging is critical for accurate assessment of new therapeutics in clinical trials [56].
Historically, clinical trials in this area relied primarily on endoscopic disease activity and clinical assessment tools, such as the CDAI score. However, enterography may also play a role in assessing the efficacy of new therapeutics. Enterographies can also be considered for post-operative assessment of Crohn’s disease when making decisions about future medical therapy to prevent disease recurrence, especially when the region of interest is not within reach of the standard endoscope.
Strengths and Limitations
A major strength of this study is the large number of enterography studies evaluated for significant findings, correlation with endoscopy and impact on clinical decision making. Unlike prior studies, this study evaluated both CT and MR enterography and reviewed detailed changes in clinical management associated with enterography findings. This study was also conducted at a large IBD referral center with standardized protocol for CT and MR enterography and radiologists experienced in the interpretation of these studies. Appropriate use of MRE in particular requires a standardized radiographic protocol and a radiologist experienced with this technique [57].
Despite this, there are several limitations to consider. These include the retrospective design of our study and the use of a time interval of up to 60 days between these studies, potentially allowing for changes in disease activity, and changes in medication that can affect disease activity. It is also impossible to determine whether the changes in management that occurred in patient management within 90 days of the enterography may be due to multiple factors other than or in addition to the imaging studies. In addition, we did not prospectively use a validated endoscopic scoring system for measuring disease activity such as the Crohn’s disease endoscopic index of severity (CDEIS) or the simple endoscopic score for Crohn’s disease (SES-CD) to measure activity. Also, in our practice, we primarily employ enterography studies rather than video capsule endoscopy for small bowel imaging. Thus, our data may not be generalizable to practices which employ video capsule endoscopy as a primary modality for small bowel imaging in patients with inflammatory bowel disease. Finally, in our practice we primarily employ MRE rather than CTE, and thus we had only 20 CTE studies versus 290 MRE studies. Thus, our data may not be generalizable to practices in which a larger proportion of patients undergo CTE for small bowel imaging.
Conclusion
CT and MR enterography play an important role in the assessment and management of IBD. This study confirms that enterography studies reveal complications of Crohn’s disease including strictures, fistulas and abscesses not evident on endoscopy. In addition, disease activity assessed by enterography correlates with endoscopic findings of active disease and elevated inflammatory markers. The results of enterography studies guide clinical decision making with regard to medical therapy and surgical intervention. We suggest that MR enterography be considered in the initial diagnosis, assessment of disease activity and monitoring of therapy in patients with IBD in clinical practice.
References
Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012;380:1590–1605.
Louis E. Epidemiology of the transition from early to late Crohn’s disease. Dig Dis. 2012;30:376–379.
Loftus EV Jr, Schoenfeld P, Sandborn WJ. The epidemiology and natural history of Crohn’s disease in population-based patient cohorts from North America: a systematic review. Aliment Pharmacol Ther. 2002;16:51–60.
Saibeni S, Rondonotti E, Iozzelli A, et al. Imaging of the small bowel in Crohn’s disease: a review of old and new techniques. World J Gastroenterol. 2007;13:3279–3287.
Grand DJ, Harris A, Loftus EV Jr. Imaging for luminal disease and complications: CT enterography, MR enterography, small-bowel follow-through, and ultrasound. Gastroenterol Clin North Am. 2012;41:497–512.
Raptopoulos V, Schwartz RK, McNicholas MM, et al. Multiplanar helical CT enterography in patients with Crohn’s disease. AJR Am J Roentgenol. 1997;169:1545–1550.
Sinha R, Verma R, Verma S, et al. MR enterography of Crohn disease: part 1, rationale, technique, and pitfalls. AJR Am J Roentgenol. 2011;197:76–79.
Negaard A, Paulsen V, Sandvik L, et al. A prospective randomized comparison between two MRI studies of the small bowel in Crohn’s disease, the oral contrast method and MR enteroclysis. Eur Radiol. 2007;17:2294–2301.
Masselli G, Casciani E, Polettini E, et al. Comparison of MR enteroclysis with MR enterography and conventional enteroclysis in patients with Crohn’s disease. Eur Radiol. 2008;18:438–447.
Wold PB, Fletcher JG, Johnson CD, et al. Assessment of small bowel Crohn disease: noninvasive peroral CT enterography compared with other imaging methods and endoscopy—feasibility study. Radiology. 2003;229:275–281.
Siddiki H, Fidler J. MR imaging of the small bowel in Crohn’s disease. Eur J Radiol. 2009;69:409–417.
Lee SS, Kim AY, Yang SK, et al. Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology. 2009;251:751–761.
Schreyer AG, Geissler A, Albrich H, et al. Abdominal MRI after enteroclysis or with oral contrast in patients with suspected or proven Crohn’s disease. Clin Gastroenterol Hepatol. 2004;2:491–497.
Minordi LM, Vecchioli A, Guidi L, et al. Multidetector CT enteroclysis versus barium enteroclysis with methylcellulose in patients with suspected small bowel disease. Eur Radiol. 2006;16:1527–1536.
Sailer J, Peloschek P, Schober E, et al. Diagnostic value of CT enteroclysis compared with conventional enteroclysis in patients with Crohn’s disease. AJR Am J Roentgenol. 2005;185:1575–1581.
Samuel S, Bruining DH, Loftus EV Jr, et al. Endoscopic skipping of the distal terminal ileum in Crohn’s disease can lead to negative results from ileocolonoscopy. Clin Gastroenterol Hepatol. 2012;10:1253–1259.
Tang L, Cai H, Moore L, et al. Evaluation of endoscopic and imaging modalities in the diagnosis of structural disorders of the ileal pouch. Inflamm Bowel Dis. 2010;16:1526–1531.
Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284.
Desmond AN, O’Regan K, Curran C, et al. Crohn’s disease: factors associated with exposure to high levels of diagnostic radiation. Gut. 2008;57:1524–1529.
Cipriano LE, Levesque BG, Zaric GS, et al. Cost-effectiveness of imaging strategies to reduce radiation-induced cancer risk in Crohn’s disease. Inflamm Bowel Dis. 2012;18:1240–1248.
Siddiki HA, Fidler JL, Fletcher JG, et al. Prospective comparison of state-of-the-art MR enterography and CT enterography in small-bowel Crohn’s disease. AJR Am J Roentgenol. 2009;193:113–121.
Sinha R, Verma R, Verma S, et al. MR enterography of Crohn disease: part 2, imaging and pathologic findings. AJR Am J Roentgenol. 2011;197:80–85.
Koh DM, Miao Y, Chinn RJ, et al. MR imaging evaluation of the activity of Crohn’s disease. AJR Am J Roentgenol. 2001;177:1325–1332.
Meyers MA, McGuire PV. Spiral CT demonstration of hypervascularity in Crohn disease: “vascular jejunization of the ileum” or the “comb sign”. Abdom Imaging. 1995;20:327–332.
Bruining DH, Siddiki HA, Fletcher JG, et al. Prevalence of penetrating disease and extraintestinal manifestations of Crohn’s disease detected with CT enterography. Inflamm Bowel Dis. 2008;14:1701–1706.
Paparo F, Bacigalupo L, Garello I, et al. Crohn’s disease: prevalence of intestinal and extraintestinal manifestations detected by computed tomography enterography with water enema. Abdom Imaging. 2012;37:326–337.
Zappa M, Stefanescu C, Cazals-Hatem D, et al. Which magnetic resonance imaging findings accurately evaluate inflammation in small bowel Crohn’s disease? A retrospective comparison with surgical pathologic analysis. Inflamm Bowel Dis. 2011;17:984–993.
Messaris E, Chandolias N, Grand D, et al. Role of magnetic resonance enterography in the management of Crohn disease. Arch Surg. 2010;145:471–475.
Ha CY, Kumar N, Raptis CA, et al. Magnetic resonance enterography: safe and effective imaging for stricturing Crohn’s disease. Dig Dis Sci. 2011;56:2906–2913.
Grieser C, Denecke T, Steffen IG, et al. Magnetic resonance enteroclysis in patients with Crohn’s disease: fat saturated T2-weighted sequences for evaluation of inflammatory activity. J Crohns Colitis. 2012;6:294–301.
Colombel JF, Solem CA, Sandborn WJ, et al. Quantitative measurement and visual assessment of ileal Crohn’s disease activity by computed tomography enterography: correlation with endoscopic severity and C reactive protein. Gut. 2006;55:1561–1567.
Gallego JC, Echarri AI, Porta A, et al. Ileal Crohn’s disease: MRI with endoscopic correlation. Eur J Radiol. 2011;80:e8–e12.
Grand DJ, Kampalath V, Harris A, et al. MR enterography correlates highly with colonoscopy and histology for both distal ileal and colonic Crohn’s disease in 310 patients. Eur J Radiol. 2012;81:e763–e769.
Gee MS, Harisinghani MG. MRI in patients with inflammatory bowel disease. J Magn Reson Imaging. 2011;33:527–534.
Kroeker KI, Lam S, Birchall I, et al. Patients with IBD are exposed to high levels of ionizing radiation through CT scan diagnostic imaging: a five-year study. J Clin Gastroenterol. 2011;45:34–39.
Jensen MD, Ormstrup T, Vagn-Hansen C, et al. Interobserver and intermodality agreement for detection of small bowel Crohn’s disease with MR enterography and CT enterography. Inflamm Bowel Dis. 2011;17:1081–1088.
Jensen MD, Nathan T, Rafaelsen SR, et al. Diagnostic accuracy of capsule endoscopy for small bowel Crohn’s disease is superior to that of MR enterography or CT enterography. Clin Gastroenterol Hepatol. 2011;9:124–129.
Fiorino G, Bonifacio C, Peyrin-Biroulet L, et al. Prospective comparison of computed tomography enterography and magnetic resonance enterography for assessment of disease activity and complications in ileocolonic Crohn’s disease. Inflamm Bowel Dis. 2011;17:1073–1080.
Solem CA, Loftus EV Jr, Tremaine WJ, et al. Correlation of C-reactive protein with clinical, endoscopic, histologic, and radiographic activity in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11:707–712.
Sauer CG, Middleton JP, Alazraki A, et al. Comparison of magnetic resonance enterography with endoscopy, histopathology, and laboratory evaluation in pediatric Crohn disease. J Pediatr Gastroenterol Nutr. 2012;55:178–184.
Ordas I, Rimola J, Garcia-Bosch O, et al. Diagnostic accuracy of magnetic resonance colonography for the evaluation of disease activity and severity in ulcerative colitis: a prospective study. Gut. 2013;62:1566–1572.
Hartley JE, Fazio VW, Remzi FH, et al. Analysis of the outcome of ileal pouch-anal anastomosis in patients with Crohn’s disease. Dis Colon Rectum. 2004;47:1808–1815.
Braveman JM, Schoetz DJ Jr, Marcello PW, et al. The fate of the ileal pouch in patients developing Crohn’s disease. Dis Colon Rectum. 2004;47:1613–1619.
Brown CJ, Maclean AR, Cohen Z, et al. Crohn’s disease and indeterminate colitis and the ileal pouch-anal anastomosis: outcomes and patterns of failure. Dis Colon Rectum. 2005;48:1542–1549.
Hahnloser D, Pemberton JH, Wolff BG, et al. Results at up to 20 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Br J Surg. 2007;94:333–340.
de Oca J, Sanchez-Santos R, Rague JM, et al. Long-term results of ileal pouch-anal anastomosis in Crohn’s disease. Inflamm Bowel Dis. 2003;9:171–175.
Bruining DH, Loftus EV Jr, Ehman EC, et al. Computed tomography enterography detects intestinal wall changes and effects of treatment in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2011;9(679–683):e1.
Higgins PD, Caoili E, Zimmermann M, et al. Computed tomographic enterography adds information to clinical management in small bowel Crohn’s disease. Inflamm Bowel Dis. 2007;13:262–268.
Hafeez R, Punwani S, Boulos P, et al. Diagnostic and therapeutic impact of MR enterography in Crohn’s disease. Clin Radiol. 2011;66:1148–1158.
Booya F, Akram S, Fletcher JG, et al. CT enterography and fistulizing Crohn’s disease: clinical benefit and radiographic findings. Abdom Imaging. 2009;34:467–475.
Jensen MD, Nathan T, Kjeldsen J, et al. Incidental findings at MRI-enterography in patients with suspected or known Crohn’s disease. World J Gastroenterol. 2010;16:76–82.
Menys A, Atkinson D, Odille F, et al. Quantified terminal ileal motility during MR enterography as a potential biomarker of Crohn’s disease activity: a preliminary study. Eur Radiol. 2012;22:2494–2501.
Shyn PB, Mortele KJ, Britz-Cunningham SH, et al. Low-dose 18F-FDG PET/CT enterography: improving on CT enterography assessment of patients with Crohn disease. J Nucl Med. 2010;51:1841–1848.
Al-Hawary M, Zimmermann EM. A new look at Crohn’s disease: novel imaging techniques. Curr Opin Gastroenterol. 2012;28:334–340.
Oto A, Kayhan A, Williams JT, et al. Active Crohn’s disease in the small bowel: evaluation by diffusion weighted imaging and quantitative dynamic contrast enhanced MR imaging. J Magn Reson Imaging. 2011;33:615–624.
D’Haens G, Feagan B, Colombel JF, et al. Challenges to the design, execution, and analysis of randomized controlled trials for inflammatory bowel disease. Gastroenterology. 2012;143:1461–1469.
Leyendecker JR, Bloomfeld RS, DiSantis DJ, et al. MR enterography in the management of patients with Crohn disease. Radiographics. 2009;29:1827–1846.
Conflict of interest
Cynthia Santillan—Consulting at Robarts Clinical Research. Barrett Levesque—Consulting at Santarus, Prometheus Labs, Castlight Health as well as speaking and teaching at Warner Chilcott, Salix, UCB Pharma, Abbott Labs. William Sandborn has no conflicts relevant to this study. Suresh Pola, Niraj S. Patel, Ramya Muralimohan, Guangyong Zou, and Derek Patel have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Niraj S. Patel and Suresh Pola are co first-authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Patel, N.S., Pola, S., Muralimohan, R. et al. Outcomes of Computed Tomography and Magnetic Resonance Enterography in Clinical Practice of Inflammatory Bowel Disease. Dig Dis Sci 59, 838–849 (2014). https://doi.org/10.1007/s10620-013-2964-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2964-7