Abstract
Background and Aims
Tissue specimen collection represents a cornerstone in diagnosis of proximal biliary tract malignancies offering great specificity, but only limited sensitivity. To improve the tumor detection rate, we developed a new method of forceps biopsy and compared it prospectively with endoscopic transpapillary brush cytology.
Patients and Methods
43 patients with proximal biliary stenoses, which were suspect for malignancy, undergoing endoscopic retrograde cholangiography were prospectively recruited and subjected to both biopsy [using a double-balloon enteroscopy (DBE) forceps under a guidance of a pusher and guiding catheter with guidewire] and transpapillary brush cytology. The cytological/histological findings were compared with the final clinical diagnosis.
Results
35 out of 43 patients had a malignant disease (33 cholangiocarcinomas, 1 hepatocellular carcinoma, 1 gallbladder carcinoma). The sensitivity of cytology and biopsy in these patients was 49 and 69%, respectively. The method with DBE forceps allowed a pinpoint biopsy of the biliary stenoses. Both methods had 100% specificity, and, when combined, 80% of malignant processes were detected. All patients with non-malignant conditions were correctly assigned by both methods. No clinically relevant complications were observed.
Conclusions
The combination of forceps biopsy and transpapillary brush cytology is safe and offers superior detection rates compared to both methods alone, and therefore represents a promising approach in evaluation of proximal biliary tract processes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cholangiocarcinomas (CCCs) are malignant tumors arising from the biliary epithelial cells and represent up to 10–20% of hepatobiliary malignancies [1]. Based on their location, CCCs are divided into intra- and extrahepatic tumors, the latter consisting of a perihilar (termed a Klatskin tumor) and distal subtype [1]. CCCs are among the deadliest gastrointestinal cancers with tumor resection being the only curative treatment option. Accordingly, surgery is the treatment of choice whenever feasible, and, in special cases, liver transplantation is indicated [1, 2]. However, surgery represents an invasive procedure which is associated with considerable mortality, thereby placing a great emphasis on a best possible preoperative evaluation of the candidates [3–5]. This is highlighted by the fact that 5–15% of patients undergoing surgical resection for suspected malignancy in fact have a benign disease [5].
Currently, the diagnosis of CCC is established through a complex approach including clinical context, laboratory analysis, imaging modalities, and tissue sampling [1, 6–8]. The tissue specimen collection is the superior method in terms of specificity and is typically performed through cytologic brushings, biopsy forceps, bile aspiration or endoscopic ultrasonography-guided fine-needle aspiration (EUS-FNA) [4, 9]. Brush cytology represents the most commonly used technique since it is relatively simple, requires little time, but offers an insufficient sensitivity of 30–60% [2, 4, 10, 11]. On the other hand, forceps biopsy is a more challenging procedure, but offers a higher cancer detection rate ranging between 43 and 81% and may allow an evaluation of cancer spread into the subepithelial tissue [4]. Similar to EUS-FNA, the forceps biopsy is especially challenging in proximal biliary lesions [4, 9] and, therefore, is only rarely performed. In general, intraductal biopsies are obtained by the use of a baby endoscope. The disadvantage of this method is the fact that only very small tissue samples are obtained which often do not allow a definite diagnosis. To improve this problem, we describe a new method of biliary biopsy using a double-balloon enteroscopy (DBE) forceps introduced via a pusher used as guiding tube, which enables a safe and reliable tissue specimen collection within the proximal biliary tract. To demonstrate the usefulness of this approach, we prospectively compared its diagnostic yield with cytology brushings in patients with potentially malignant proximal biliary strictures.
Patients and Methods
Human Subjects
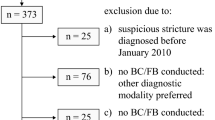
Our prospective study was designed to compare the use of endoscopic transpapillary brush cytology and forceps biopsy in evaluation of proximal biliary strictures and was carried out at the University Medical Centers Heidelberg and Ulm. Patients were included when they presented with a high-grade stricture at or proximal to the hepatic duct bifurcation, which was suspected for malignancy, and were scheduled to undergo endoscopic retrograde cholangiography (ERC) for clinical indication. In some patients, an abdominal CT scan was performed prior to the ERC and was suggestive of a malignant lesion. The cytological/histological finding in ERC specimen was compared with the final diagnosis, which was obtained through surgery and/or prolonged clinical follow-up of at least 12 months. An informed consent was obtained from all patients. This prospective study was registered at ClinicalTrials.gov (NCT 01145248) and was approved by the Human Subjects Committees of both medical centers.
Endoscopic Treatment
ERC was performed with a duodenoscope Olympus TFJ 160-R (Olympus., Tokyo, Japan) under analgosedation (midazolam, propofol, and/or short acting opiates) by two experienced endoscopists (H.K., A.S.). Endoscopic sphincterotomy was performed with an Olympus papillotome (Olympus) introduced over a guide wire (Jagwire, 0.035 inch; Boston-Scientific, Natick, MA, USA). The strictures were identified under a radiographic guidance and dilated up to 10 Fr with a gradually dilating catheter (Soehendra Biliary Dilatation Catheter; Wilson Cook, Winston-Salem, NC, USA). After that, the region of interest was brushed five times in both directions to obtain cytology specimens. Then, the cannulation of the bile duct was performed by a pusher using a guidewire. The guidewire was removed and two histology samples were taken via a DBE forceps (BF1725DF; Fujinon, Willich, Germany), which was placed under the guidance of the pusher. In some instances, the cannulation of the bile duct was performed with a help of guiding catheter (Figs. 1, 2), if the cannulation was not feasible with the pusher and guidewire alone. The obtained biopsy size was on average 2 mm.
The technique of bioptic sampling. a To reach the biliary stricture, a guiding wire and pusher was introduced via the duodenoscope Olympus TFJ 160-R. In some instances, a guiding catheter was also used. b The histology samples were taken with a DBE-forceps, which was placed under a guidance of a pusher after guiding wire and catheter were removed
ERC findings and retrieval of the specimen. Patients presenting with a potentially malignant perihilar (arrows in a) or intrahepatic stenosis (arrows in c). Position of the hepatic bifurcation is highlighted by an arrowhead. Strictures at ERC were subjected to both transpapillary brush cytology and forceps biopsy (as shown in b and d) at the same time
Pathologic Assessment and Data Analysis
For histological evaluation, biopsy specimen were fixed in 10% buffered formalin and embedded in paraffin. Tissue sections were stained with hematoxylin and eosin (H&E) and Periodic Acid Schiff (PAS). The cytology specimens were transferred to a glass slide by smearing the cellular material directly from the brush. After fixation with ethanol, standard cytological stains (H&E, Papanicolau, May-Grunwald-Giemsa, PAS) were performed. The slides were evaluated by dedicated pathologists (T.B., I.E., P.Sch.) in both centers.
The patient data were collected and statistically analyzed with Excel software, version 2003 (Microsoft). The sensitivity of both methods was defined as the primary endpoint of the study.
Figures were assembled with Adobe Photoshop (Version 10.0) and Illustrator software (Version 13.0.0; both Adobe Systems, San Jose, CA).
Results
In the period from January 2007 to March 2009, the study recruited 43 patients presenting with proximal biliary strictures (26 males, 17 females) and an average age of 64 ± 17 years (Table 1). An extensive evaluation revealed a malignant disease in 35 of them, while 8 had a benign cause of biliary strictures, including 7 patients with primary sclerosing cholangitis and 1 with a nonspecified inflammatory stenosis. Among the malignant processes, 33 patients had a cholangiocarcinoma (including 18 Klatskin tumours), 1 patient had a hepatocellular, and 1 had a gallbladder carcinoma. All patients were subjected to ERC with both cytology brushing and forceps biopsy in the same session (Fig. 2). The method with DBE forceps allowed a pinpoint biopsy of the biliary stenoses. In contrast to studies with unguided biopsying, by the use of a guiding tube an exact biopsying of the stenosis was made possible in each case. Moreover, intraductal biopsy of intrahepatic biliary stenoses were possible by this new method (Fig. 2c, d). The biopsy specimens were larger, on average 2 mm, than biopsies taken by a cholangioscopy (see Fig. 3 for characteristic examples of histologic/cytologic findings). In some instances, the cannulation of the bile duct was difficult with the pusher and guidewire alone. In these cases, the help of guiding catheter was utilized.
Histological/cytological findings with intraepithelial neoplasia and cholangiocarcinoma. a Forceps biopsy showing bile duct epithelium with architectural distortion, nuclear crowding, pseudostratification, and hyperchromasia. No invasion of the underlying stroma is evident (intraepithelial neoplasia). H&E staining, scale bar 300 μm. b Higher magnification of (a) shows papillary structures with hyperchromatic, irregular nuclei. Large nucleoli are visible in some cells (arrows). H&E staining, scale bar 200 μm. c Bile duct brushings of the same lesion depicted in (a, b) showing a small group of malignant cells with hyperchromatic, pleomorphic nuclei. PAS staining, scale bar 100 μm. d–e Histology and cytology of a carcinoma of the choledochus (simultaneously taken scratch cytology and biopsy of the same lesion). d Biopsy reveals carcinoma cells infiltrating the desmoplastic stroma; H&E staining. e Cytology: neoplastic cells show varying sizes and polymorphic nuclei. Carcinoma cells are twice the diameter as compared to the biopsy due to different fixation procedures (May-Grünwald-giemsa staining). Scale bar (e) 50 μm. d and e are the same magnification
No clinically relevant complications such as significant bleeding, perforation, or pancreatitis were observed. During the brush cytology, sufficient material was obtained in 40 cases, while in 3 cases, the material was only of limited informative value. Using the DBE forceps, a satisfactory sampling succeeded in 38 patients, while 3 and 2 samples were of limited and no informative value, respectively.
The procedure of brush cytology took 2–3 min and the forceps biopsy 5–7 min. Both methods reached 100% specificity for prediction of malignancies. When all patients were considered, the sensitivity of cytology and biopsy in detecting malignant processes were 49 and 69%, respectively. When including only patients with material of at least limited informative value, the sensitivity of biopsy in detecting malignancies improved to 73%, while the cytology results remained unaltered. Considering only high quality samples, the sensitivity of cytology and biopsy further increased to 53 and 80%, respectively. When both methods were combined, they reached a sensitivity of 80% in detecting malignant diseases and this sensitivity further improved to 86% in patients, where both methods yielded samples of good informative value. Of note, all patients with non-malignant conditions were correctly evaluated by both methods.
Discussion
While proximal biliary strictures are often caused by malignant processes, it is not always possible to confirm the diagnosis through specimen collection, and, in these instances, the further management of these patients has to be based on less specific criteria such as clinical context or imaging modalities [1]. A combination of biliary forceps biopsy with a transpapillary brush cytology may represent an useful approach to increase the diagnostic yield [12–14]. To the best of our knowledge, only one retrospective study has assessed the utility of both methods in parallel in patients with hilar CCC, and it showed a moderate increase in diagnostic yield when biliary forceps biopsy and a transpapillary brush cytology were combined (sensitivities of 60.3, 41.4 and 53.4 for a combined approach, brush cytology and forceps biopsy, respectively; [15]). To verify these data, our study prospectively evaluated both methods in parallel in patients with proximal biliary strictures. To further improve the diagnostic yield of tissue specimen collection, we established a new method of biliary biopsy using a relatively large forceps introduced via a tube which still enables an intraductal biopsying of even intrahepatic biliary stenoses. This approach addresses the three major problems associated with previous biopsy techniques, i.e. the difficulty of cannulation of the bile duct with a standard biopsy forceps, the imprecise sampling from the surrounding tissue/wall which happens when forceps is introduced without the use of a guiding tube under the x-ray control only, and the retrieval of very small specimen, which is a common obstacle when using a baby-endoscope.
We reached the combined sensitivity of 80%, which is well above the sensitivity published in the previous report [15]. The sensitivity of cytology brushing (49%) and forceps biopsy alone (69%) was also slightly above the ones reported by Weber et al. [15], but well within the previously reported range (30–60% for cytology, 43–81% for biopsy; [4]).
With this new method of forceps biopsy, we obtained high quality biopsy samples in most cases. But in 5 of 43 cases the obtained material had suboptimal quality or was not sufficient for histological evaluation. However, all these 5 cases were in the first half of the study and may represent a suboptimal biopsy technique at the beginning of the study.
Comparison of costs show that the more challenging procedure of forceps biopsy with the DBE forceps is more expensive (80 Euros) than the method of brush cytology (52 Euros). But our results yielded a higher sensitivity for the forceps biopsy which relativize these costs.
Further studies are needed to clarify whether the higher diagnostic yield seen in our cohort is indeed due to the novel endoscopic techniques employed or due to statistical variability or different patient cohorts examined (i.e. proximal biliary stenoses analyzed in our paper vs hilar CCC only studied by Weber et al. [15]).
Given that the combination of both methods was safe (i.e. no significant clinical complications were observed), this approach is promising and should be further evaluated in a larger patient cohort. In addition, sample examination with more advanced analysis methods such as fluorescence in situ hybridization or digital image analysis [1, 4] should be sought, since this may further increase the sensitivity of the described approach.
Abbreviations
- CCC:
-
Cholangiocarcinoma
- DBE:
-
Double-balloon enteroscopy
- ERC:
-
Endoscopic retrograde cholangiography
- EUS-FNA:
-
Endoscopic ultrasonography-guided fine-needle aspiration
- HCC:
-
Hepatocellular carcinoma
- H&E:
-
Hematoxylin and eosin
- PAS:
-
Periodic Acid Schiff
- PSC:
-
Primary sclerosing cholangitis
References
Blechacz B, Gores GJ. Cholangiocarcinoma: advances in pathogenesis, diagnosis, and treatment. Hepatology. 2008;48:308–321.
Boberg KM, Jebsen P, Clausen OP, Foss A, Aabakken L, Schrumpf E. Diagnostic benefit of biliary brush cytology in cholangiocarcinoma in primary sclerosing cholangitis. J Hepatol. 2006;45:568–574.
Bergquist A, Glaumann H, Persson B, Broomé U. Risk factors and clinical presentation of hepatobiliary carcinoma in patients with primary sclerosing cholangitis: a case-control study. Hepatology. 1998;27:311–316.
Weber A, Schmid RM, Prinz C. Diagnostic approaches for cholangiocarcinoma. World J Gastroenterol. 2008;14:4131–4136.
Bennett JJ, Green RH. Malignant masquerade: dilemmas in diagnosing biliary obstruction. Surg Oncol Clin N Am. 2009;18:207–214.
Angulo P, Lindor KD. Primary sclerosing cholangitis. Hepatology. 1999;30:325–332.
Fleming KA, Boberg KM, Glaumann H, Bergquist A, Smith D, Clausen OPF. Biliary dysplasia as a marker of cholangiocarcinoma in primary sclerosing cholangitis. J Hepatol. 2001;34:360–365.
Boberg KM, Schrumpf E. Diagnosis and treatment of cholangiocarcinoma. Curr Gastroenterol Rep. 2004;6:52–59.
Harewood GC. Endoscopic tissue diagnosis of cholangiocarcinoma. Curr Opin Gastroenterol. 2008;24:627–630.
Selvaggi SM. Biliary brushing cytology. Cytopathology. 2004;15:74–79.
Gress TM. Molecular diagnosis of pancreaticobiliary malignancies in brush cytologies of biliary strictures. Gut. 2004;53:1727–1729.
Ponchon T, Gagnon P, Berger F, et al. Value of endobiliary brush cytology and biopsies for the diagnosis of malignant bile duct stenosis: results of a prospective study. Gastrointest Endosc. 1995;42:565–572.
Pugliese V, Conio M, Nicolo G, Saccomanno S, Gatteschi B. Endoscopic retrograde forceps biopsy and brush cytology of biliary strictures: a prospective study. Gastrointest Endosc. 1995;42:520–526.
Schoefl R, Haefner M, Wrba F, et al. Forceps biopsy and brush cytology during endoscopic retrograde cholangiopancreatography for the diagnosis of biliary stenosis. Scand J Gastroenterol. 1997;32:363–368.
Weber A, von Weyhern C, Fend F, et al. Endoscopic transpapillary brush cytology and forceps biopsy in patients with hilar cholangiocarcinoma. World J Gastroenterol. 2008;14:1097–1101.
Acknowledgments
We would like to thank all the participating patients for making this study possible. Our work was supported by German Research Foundation grants KU 1253/5-3 (H.K.) and STR 1095/2-1 (P.Str.). The technical assistance of Annemarie Schmid is greatly acknowledged.
Conflict of interest
The authors declare that they do not have anything to disclose regarding funding from industries or conflict of interest with respect to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kulaksiz, H., Strnad, P., Römpp, A. et al. A Novel Method of Forceps Biopsy Improves the Diagnosis of Proximal Biliary Malignancies. Dig Dis Sci 56, 596–601 (2011). https://doi.org/10.1007/s10620-010-1535-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1535-4