Abstract
Purpose
This study was conducted in order to investigate the safety and accuracy of percutaneous transluminal forceps biopsy (PTFB) during percutaneous biliary drainage (PTBD) in patients with a suspicion of malignant biliary stricture.
Material and methods
Fifty consecutive patients with obstructive jaundice underwent PTFB during PTBD. Biopsy specimens were obtained using 5.2-F flexible biopsy forceps and these specimens were independently analysed by two pathologists. Consensus was obtained in case of discrepancy. Biopsy was considered as a true positive when tumour cells were retrieved. In the absence of tumour cells, comparison with available surgical findings and/or endoscopic ultrasound fine-needle aspiration (EUS-FNA) and/or percutaneous liver biopsy and/or imaging or clinical follow-up was made to distinguish true and false negatives. Specificity, sensitivity, positive predictive value, negative predictive value and accuracy were calculated. Influence of tumour location and pre-operative imaging findings was evaluated. Adverse events were reported.
Results
Biliary drainage and tissue sampling were achieved in 100% of patients. Sensitivity and specificity were 70 and 100%, respectively, while overall accuracy was 72%. After excluding the first 25 patients, accuracy and sensitivity for tissue sampling reached 80 and 78%, respectively. Sensitivity was better (87%) if stenosis was located at the upper part of the biliary tree, compared to the lower part (55%). In case of cholangiocarcinoma or intraductal invasion suspected on imaging, biopsy was contributive in 84 and 81% of patients, respectively. Four complications occurred consisting of one bile leak, two haemobilia and one pneumoperitoneum.
Conclusion
PTFB combined with PTBD is a safe and effective technique for both histopathological diagnosis and biliary decompression of biliary strictures.
Key Points
Implications for patient care:
• Percutaneous transbiliary forceps biopsy is technically feasible (100% of tissue sampling in our study) and is a safe technique.
• Radiological management combining PTFB plus PTBD may allow diagnosis and treatment of the biliary stricture at the same time.
• Sensitivity and accuracy for PTFB reached 78 and 80%, respectively, with a 100% specificity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Identification of the cause of biliary stricture remains the main challenge. Despite the development of non-invasive imaging techniques [1, 2], indeterminate biliary stricture (IBS), biliary stricture without histopathologic diagnosis, remains high at up to 20% [3]. Different endoscopic techniques are available or under development: endoscopic retrograde cholangiopancreatography (ERCP)-guided brushing, cyto-aspiration or biopsy, endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) or biopsy, and cholangioscopy with direct biopsy, as well as other novel techniques such as intraductal ultrasonography and confocal laser endomicroscopy [4, 5]. ERCP tissue sampling techniques suffer from low sensitivity ranging from 27 to 56% for bile aspirated cytology or forceps biopsy, respectively [6]. EUS-FNA has proven to be superior to ERCP (guided) in suspected malignant biliary obstructions [7,8,9]. In a prospective study comparing EUS-FNA to EUS-core biopsy, accuracy for FNA was 92.3%, compared to 84.6% for biopsy [10]. Nowadays, EUS-FNA is the gold standard for tissue sampling in cases of suspected malignant biliary stricture. However, in some cases, this technique may not be available or feasible (e.g. surgical anastomosis). Its accuracy also relies on the operator’s experience [10]. Lesions located at the proximal part of the biliary tree (hilar strictures) are especially challenging and associated with a lower accuracy for sampling [8].
In 1980, the first case of tissue sampling (brush and forceps biopsy) through a percutaneous access was described [11]. Twenty years later in 2002, a large study of 130 patients reported on the performance of percutaneous transhepatic forceps biopsy (PTFB) [12]. Since the beginning of the twenty-first century, endoscopic techniques, interventional radiology materials and imaging techniques have largely improved.
The objectives of the present study were to evaluate the feasibility, safety and clinical results of tissue sampling during percutaneous biliary drainage (PTBD) in patients with presumed malignant biliary stricture. We evaluated the efficacy of percutaneous biliary drainage and included a radiation dose analysis.
Materials and methods
Local ethics and National Data Protection committee approval was obtained (reference CPP A15-D30-VOL.26) for this retrospective study.
Recording data
Over a 7-month period (January 2015 to July 2015), all consecutive patients with obstructive jaundice referred for PTBD without histological diagnosis were retrospectively analysed. Indications for radiological treatment and tissue sampling were validated by a pluridisciplinary tumour board. Endoscopic management of the patients was retrospectively analysed.
Clinical history, demographic data, tumour markers, pre- and post-procedure (within 7 days after treatment) liver parameters and C-reactive protein (CRP) were also recorded. Pre-operative imaging findings were also reported. Available imaging was retrospectively reviewed by one of the radiologists involved in the study, blinded of the final diagnosis, and subsequently compared with the initial report. Consensus was obtained for lesion size, suspected intraductal invasion, suspected diagnosis and tumour location (level on the biliary tree). The biliary stricture location on cross-sectional imaging was ranged according to the biliary tree anatomy (right and left intrahepatic bile duct, hilum, common hepatic duct, common bile duct, ampullary segment and gallbladder). The entire extrahepatic bile duct included the bile duct from the hilum to the ampullary segment.
Technical aspects of the procedure were recorded. Procedure-related complications were reported according to the Society of Interventional Radiology (SIR) Standards of Practice Committee classification [13, 14]. Dosimetry parameters were recorded for each procedure.
PTBD and PTFB procedure details
All procedures were performed in an angiography suite Artis zee (Siemens Healthcare) by three interventional radiologists with 15, 8 and 2 years of experience, respectively.
SIR guidelines for PTBD were followed [14]. Broad spectrum antibiotics (amoxicillin and clavulanate potassium or cephalosporin) were administered before intervention. Percutaneous access to the biliary system was always performed using a micropuncture Seldinger technique with a 22-gauge access system (Merit Medical), under US guidance and general anaesthesia. A cholangiography under fluoroscopy allowed the identification of the biliary stricture (Fig. 1). A flexor sheath 7-F, 30 cm long (Cook Medical), with radio-opaque tip was inserted over a 0.035-in. wire (Terumo). If possible, biliary obstruction was crossed using a 4-F catheter. In case of successful stricture crossing, a rigid 0.035-in. wire (Amplatz, Cook Medical) was placed distally in the duodenum. The 4-F catheter was then removed. The flexible biopsy forceps 5.2-F, 60 cm long, 2.25 mm3 cup volume (Cook Medical) was inserted in the sheath, along the stiff wire. Tissue sampling was performed, under fluoroscopy, with the opened cup pushed into the stricture. The cup is then closed to capture the sample. Intraprocedural imaging is covered in Fig. 2. After tissue sampling, an internal drainage catheter was left in place. In case of malignant strictures, a biliary stent (Luminexx, Bard) was placed secondarily (10 mm in diameter and length chosen according to the biliary tree anatomy).
A 60-year-old male patient with jaundice and suspected hilar cholangiocarcinoma on pre-operative cross-sectional imaging. Cholangiography under fluoroscopy performed with a left side approach (white arrow, showing the 4-F catheter) demonstrates enlarged right and left intrahepatic bile ducts (black arrow). Stricture is located at the biliary convergence (star). Percutaneous transbiliary biopsy was contributive, with a final histopathological diagnosis of cholangiocarcinoma
A 65-year-old male patient with suspected hilar cholangiocarcinoma on pre-operative cross-sectional imaging. Cholangiography (a) performed with a right side approach shows the 7-F flexor sheath (small black arrow) with a radio-opaque tip (large black arrow). The stricture (black stars) was successfully crossed and a 0.035-in. rigid wire (white arrow) was placed distally in the common bile duct (white star) and duodenum. The flexible biopsy forceps 5.2-F, 60 cm long, is inserted with closed cup into the sheath (index finger). Intraprocedural imaging shows the opened 2.25-mm3 cup volume pushed into the stricture (b). The cup is then closed to capture the sampling (c) and is removed from the sheath to retrieve the sample. Macroscopic sample is then placed in a formol area (d)
In cases of failed stricture crossing, an external drainage catheter was left in place.
Evaluation of efficacy and accuracy
Efficacy of PTBD was based on changes of biological parameters. Samples were considered feasible and adequate by the radiologist if the size was macroscopically large enough: 1 mm length (minimum) and consists of solid tissue (no liquid sample or fragmented tissue) (Fig. 2d).
Samples were considered adequate by the pathologists if the samples were quantitatively and qualitatively adequate for a pathologist to formulate a diagnosis.
Percutaneous transbiliary specimens collected at the site of stenosis were fixed, routinely processed and embedded in paraffin. H&E staining on 4-μm sections was used to perform diagnosis. Three cutting levels were performed on each biopsy. If necessary, immunohistochemistry was performed using an automated immunohistochemical staining processor (Autostainer Plus, Dako).
Biopsy sample slides were retrospectively and independently analysed by two pathologists with 10 and 7 years of experience, respectively. Consensus was obtained in case of discrepancy. Performance of PTFB was established on the ability to diagnose malignant tissue and, for malignant tumour, to diagnose the type of tumour and lesion differentiation. Sensitivity, specificity, positive (PPV) and negative (NPV) predictive values and accuracy of PTFB and their 95% CI were calculated.
Where there was consensus of malignant tissue on PTFB specimens, biopsy was considered as a true positive. In the other cases, pathological examination of the surgical specimen and/or EUS-FNA and/or percutaneous liver biopsy and/or imaging follow-up and/or clinical follow-up was used to determine the final diagnosis. The endpoint for clinical and imaging follow-up was 14 months after the initiation of the study. If a progressive disease included the occurrence of metastasis or lymph nodes or progression of tumoural tissue within a long follow-up period (14 months) was observed on follow-up imaging, malignant aetiology was considered as final diagnosis. For clinical follow-up, where death or deterioration of performance status (PS) took place, malignant aetiology was considered as final diagnosis, when no other reason for PS deterioration was found.
Correlations between PTFB accuracy and imaging findings (suspected diagnosis, suspected invasion of biliary duct on cross-sectional imaging, lesion size, location of the stricture on the biliary tree) were calculated.
Statistical analysis
Continuous variables were expressed as mean values/standard deviation and median/range (min–max). Categorical variables were expressed as counts and percentages.
Sensitivity, specificity, and positive and negative predictive values (95% CI) were calculated for the percutaneous biopsy technique. Accuracy (95% CI) for percutaneous transbiliary forceps biopsy was calculated as the sum of true positives and true negatives divided by the sum of all tests and was expressed as percentages. For mean comparison, a paired t test was used.
Correlation between different data (binomial distribution), as described above, was calculated with a correlation test (Pearson). A p value < 0.05 was considered as a significant difference. All calculations were performed with the JMP Pro 12 software.
Results
Fifty patients were included in this study. Characteristics of the population are summarised in Table 1. Pre-operative imaging consisted of 49 CE-CT and 11 hepato-biliary MRI (Table 1). The mean delay between imaging and percutaneous biliary procedure was 26 ± 22 days (SD); median was 21 days (range 7–112). Five patients had a history of non-bilio-pancreatic malignant tumour including one gastric adenocarcinoma, one recto-sigmoidal adenocarcinoma, one lung carcinoma (small cell carcinoma), one breast cancer and one ovarian mucinous tumour. The patient with a history of breast cancer had an increased CA 15-3 (92 U/mL, normal level < 25 U/mL) and the patient with ovarian cancer had a CA 125, near normal level (39 U/mL, normal level < 35). Out of 13 patients with available CEA dosage, only 4 (31%) patients had an abnormal level (> 5 ng/mL). All procedures were performed by interventional radiologists with 15 (n = 19), 8 (n = 22) and 2 (n = 9) years of experience, respectively. Eighty-eight percent (44/50) of the biliary interventions were performed through a right-sided approach. All (100%) stenosis were successfully crossed and tissue sampling was always macroscopically adequate for the radiologist. Concerning PTFB sampling, the mean number of specimens per patient was 3 ± 1 (SD) and median was 3 (range 2–8), because the IR decided to add sampling according to the macroscopic aspect of specimens.
Concerning the size of the specimens (Fig. 2d), pathologists reported the following findings: 1 mm (n = 26); 1 mm < x ≤ 3 mm (n = 19); 1 mm < x ≤ 4 mm (n = 4); and 1 mm < x ≤ 7 mm (n = 1).
Secondary stent placement was always feasible (100%). Concerning laboratory parameters, results are presented in Table 2.
The mean dose area product (DAP) (n = 49) was 3016 ± 2805 μGy m2 and median was 2148 μGy m2 (range 732–14,783), the mean skin dose SD (n = 44) was 373 ± 468 mGy and median was 184 mGy (range 38–2144) and mean fluoroscopy time (FT) (n = 49) was 18 ± 12 min and median was 13 min (range 5–58).
Safety
Complications occurred in four patients (8%) consisting of three minor (grade A) and one major (grade D) complication. Minor complications included two (4%) haemobilia (resolved spontaneously within 24 h) and one (2%) pneumoperitoneum related to a duodenal perforation (cholangiocarcinoma was suspected on imaging and biliary biopsy was negative), also spontaneously resolved. One biliary injury (2%) was depicted on cholangiography and unenhanced CT after drainage, showing biliary leakage. This leakage was successfully treated with external drainage catheter placement for 1 week (grade D).
Detailed histopathological findings with PTFB are available in the Supplemental data.
In 32 (64%) patients, tissue sampling histology found neoplastic tissue with tumour cells. Among the 18 (36%) patients without evidence of tumour cells on tissue sampling, we used surgical findings or surgical specimens (n = 2), EUS-FNA (n = 3), and clinical and/or imaging follow-up (n = 13) for the determination of final diagnosis. For the three patients with EUS-FNA, histology was not available at the time of percutaneous drainage; therefore, the PTFB was performed. Among those 18 patients, four were finally true negative (no neoplastic pathology): one CDHP, confirmed with surgical biopsy (patient 2 on the Supplemental data); two autoimmune pancreatitis (one Ig-G4-related disease) with normalisation of pancreas aspect on MRI after corticoid treatment (patients 7 and 47 on the Supplemental data); and one chronic cholecystitis, complicated with a cholecystico-colic fistula (patient 44 on the Supplemental data). Among the 14 false negative cases, two corresponded to hepatic pediculitis (secondary to a cholecystitis with adhesions), one from gastric carcinoma and the other from small cell carcinoma. For the 12 others, eight (67%) corresponded to suspected pancreatic adenocarcinoma on imaging.
In eight (8/50; 16%) patients, pathologists reported crushing artefacts. These artefacts are a common finding in histological section and may represent a major pitfall for pathologists to conclude. In two patients, these artefacts prevented a definitive diagnosis. Examples of histopathology findings including immunohistochemistry analysis are represented in Fig. 3.
Performance
For the global population (50 patients), sensitivity, specificity, PPV, PNV and accuracy were 70% (95% CI 0.55–0.81), 100% (95% CI 0.51–1), 100% (95% CI 0.89–1), 22% (95% CI 0.09–0.45) and 72% (95% CI 0.58–0.82), respectively.
Taking into consideration the learning curve of the readers, the last 25 patients were analysed separately. Both groups were similar in terms of difficulty for biliary tree access or for stricture crossing.
Performance increased with reported sensitivity, specificity, PPV, PNV and accuracy of 78% (95% CI 0.58–0.9), 100% (95% CI 0.34–1), 100% (95% CI 0.82–1), 29% (95% CI 0.08–0.64) and 80% (95% CI 0.61–0.91), respectively.
After a 14-month follow-up, among the 46 patients with malignant tumours, 29 (63%) had a PS < 3, 6 (13%) had a PS ≥ 3 and 11 (24%) died.
Sensitivity was lower if the stenosis involved the lower part of the biliary tree (55%; 15/27) (95% CI 0.37–0.72) compared to the upper part (87%; 20/23) (95% CI 0.68–0.95), but the difference was not significant (p = 0.57).
In case of intraductal invasion or cholangiocarcinoma suspected on pre-procedural imaging, biopsy contributed in 81% (31/38) (95% CI 0.67–0.91) and 84% (21/25) (95% CI 0.65–0.94) of the patients, respectively. Conversely, in case of the absence of intraductal invasion or suspected pancreatic neoplastic lesion, biopsy contributed in only 33% (4/12) (95% CI 0.14–0.61) and 53% (9/17) (95% CI 0.31–0.74), respectively. A significant difference in terms of accuracy was found where there was intraductal invasion on pre-operative imaging (p = 0.014). No difference was found according to the initial suspected diagnosis (pancreatic adenocarcinoma or cholangiocarcinoma) (p = 0.49).
The median value of lesion size on pre-op imaging was 18.5 mm, mean was 25.3 ± 23.6 mm and median was 18.5 mm (range 3–90). No significant difference was found between positive biopsy and lesion size larger than the median value (p = 0.354). Performance of PTFB is summarised in Table 3.
Endoscopic management analysis of the population
Among 50 patients, 17/50 (34%) have not been evaluated using endoscopic examination before interventional radiology treatment and referral to the radiologist. Reasons are summarised in Table 1.
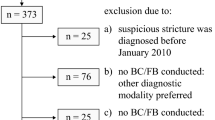
Endoscopic management of the population is summarised in Fig. 4. For 7/33 (21%) patients, EUS-FNA was feasible. Final accuracy was 4/7 (57%) consisting of three positive biopsy (pancreatic adenocarcinoma) and one true negative.
Endoscopic management of the population. Reasons for no endoscopic management are summarised in Table 1. The reasons for failed EUS-FNA were failure to cross the stenosis (n = 6), invisible mass (n = 2), lesion considered to be too small (n = 1) and sampling considered too risky due to the presence of a cavernoma (n = 1)
Material coming from the radiological technique and EUS-FNA is represented on Fig. 5.
Discussion
In our study, radiological management for biliary stricture was proposed in 82% of cases after failure of endoscopic management: failed prosthesis placement (52%), biliary stricture location not accessible for endoscopic route (16%) and endoscopic drainage dysfunction (14%).
Percutaneous biliary drainage was efficient with an improvement of liver parameters including a significant decrease of bilirubin, SGOT and SGPT (Table 2).
Specimens obtained with PTFB were large enough for pathologists to provide tissue characterisation and immunohistochemistry analysis. PTFB accuracy increased up to 80% after a short learning curve, and up to 81 and 84% in case of intraductal invasion or suspected cholangiocarcinoma on pre-op imaging.
If only endoscopic management had been available, only 8% of patients would have histological diagnosis, e.g. 92% with difficult treatment choice, particularly with chemotherapy and surgical indication. Endoscopic techniques face the challenges of difficulty of access, difficulty reaching the target (distal lesion) and the necessity of trained, dedicated and available endoscopists.
To our knowledge, this is the first study that underlines the added value of radiological management for these patients. Other studies only focus on PTFB performance.
In terms of performance for PTFB and biliary stricture location, we found a better sensitivity (87%) for lesions located at the upper part of the biliary tree (hilum or intrahepatic bile duct) for percutaneous access where endoscopic management is more difficult [8]. Jung et al [12] found similar results (sensitivity 100% for hilum), while Ierardi et al [15] underline a very low sensitivity (60%) for hilar lesion.
Exclusion of a malignancy is also challenging for biliary stricture management. With this technique, in our study and in the literature, specificity was always 100% [12, 15,16,17].
Our study also highlights that the most predictive factor for a true positive histology was intraductal invasion on pre-op imaging (p = 0.014), which was not analysed in other published studies [11, 12, 15, 16].
In terms of complications, and in contradiction of other authors, we used the dedicated classification for interventional radiology, which is the most widely accepted [13, 18]. Nevertheless, we had similar complication rates as the largest study (8 vs 6%) [12] and significantly less than Ierardi et al (37.5%) [15].
Endoscopic management may lead to more complications compared to radiological techniques [19]. Conversely, percutaneous biliary access may lead to tumour seeding along the catheter tract, even if the reported incidence is low [19]. A recent review article stated that PTBD was associated with fewer complications compared to endoscopic biliary drainage as the initial procedure for pre-operative drainage in patients with resectable perihilar cholangiocarcinoma [20].
Biliary interventions are considered as proximal procedure (i.e. procedure during which the operators’ hands are close to the radiation source), with a potential high radiation exposure to the operators’ extremities. Occupational radiation protection should be taken into account for each interventional procedure and follow guidelines [21]. For patients, effective dose may also be high, up to 6.77 mSv according to a study using the Monte Carlo codes [22]. The organ receiving the maximum radiation dose was the lumbar spine [22].
Regarding the dosimetry parameters, mean DAP was 3016 μGy m2 corresponding to 30.16 Gy cm2, and the mean FT was 18 min for PTBD combined with PTFB. These parameters are very close to the already reported dosimetry parameters. For PTBD only, mean FT was 16 min in a recent French study [23]. For bilioplasty, patient’s DAP was 0.7–52.54 Gy cm2 and FT was 1.13–24.47 min in a study published in 2018 [24]. Adding biliary biopsy does not seem to increase radiation dose significantly and may therefore be considered safe with regard to radiation exposure.
EUS-FNA is still considered to be the gold standard for tissue sampling in biliary stricture, particularly for solid pancreatic masses with a high accuracy, ranging from 78 to 95% [25], and lesions in close proximity to the gastrointestinal tract [26, 27]. Nevertheless, a recently published study comparing PTFB and EUS-FNA showed similar sensitivity, negative predictive value and accuracy for proximal biliary stricture [28].
Moreover, there are some controversies associated with the EUS-FNA technique regarding the most suitable diameter for the needle (19, 22 or 25 gauges), the appropriate number of needle passes and the necessity for in-site cyto-pathological evaluation. In a comparative study, EUS-guided FNA and EUS-guided core biopsy showed similar results in terms of accuracy [10].
A comparative study of three intraductal biliary biopsy techniques (cytological brush, clamshell forceps under choledochoscope guidance and under fluoroscopic guidance) was in favour of choledochoscope guidance (sensitivity 44%, specificity 100%) vs fluoroscopic guidance (30, 88%) [29]. Sensitivity was low in this study regardless of the biopsy technique.
Regarding the technique for tissue sampling, brushing cytology has insufficient sensitivity and it allows only cytology analysis, with poor accuracy [30]. Tapping et al compared cytological sampling vs forceps biopsy during PTBD and concluded better sensitivity and negative predictive value for biopsy (78, 30% vs 61, 19%) [31]. PTFB is considered by the authors as the recommended technique for histology during PTBD in patients with inoperable malignant biliary strictures [31]. PTFB clearly has very good performance in the literature [12, 15, 17].
Moreover, interventional radiology materials have largely improved. The first biopsy forceps used by radiologists needed a 10–12-F introducer catheter [11], while we now use a 7-F sheath. Now, radiologists also have dedicated material for the biliary system, whereas the biopsy forceps used in the Jung 1et al study was originally designed for endomyocardial biopsies [12].
The main limitation of this study was that only clinical and imaging follow-up was used for 13 patients out of 18 without tumour cells retrieved on sampling, to conclude final diagnosis. Because we manage a large population of biliary stricture patients in our centre (50 patients were enrolled in 7 months), we could have included more patients. We also may have increased our performance by using the modified method for tissue sampling, provided by Patel et al [17].
Conclusion
Percutaneous radiological access for histology sampling and biliary stricture treatment is a “2-in-1” technique—feasible, safe and efficient. The radiological technique may be the first line in cases of intraductal invasion on pre-procedural imaging, for lesions located at the upper part of the biliary tree and in all cases of failed endoscopic approach.
Summary statement
The data suggests that PTFB and PTBD are safe with a relatively high overall accuracy for diagnosis in the setting of biliary stricture.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CDHP:
-
Cystic dystrophy in heterotopic pancreas
- CE-CT:
-
Contrast-enhanced computed tomography
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- DAP:
-
Dose area product
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- EUS-FNA:
-
Endoscopic ultrasound-guided fine-needle aspiration
- GGT:
-
Gamma-glutamyltransferase
- H&E:
-
Haematoxylin and eosin
- IBS:
-
Indeterminate biliary stricture
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- PTBD:
-
Percutaneous biliary drainage
- PTFB:
-
Percutaneous transhepatic forceps biopsy
- SD:
-
Skin dose
- SIR:
-
Society of Interventional Radiology
References
Katabathina VS, Dasyam AK, Dasyam N, Hosseinzadeh K (2014) Adult bile duct strictures: role of MR imaging and MR cholangiopancreatography in characterization. Radiographics 34:565–586
Arrivé L, Hodoul M, Arbache A, Slavikova-Boucher L, Menu Y, El Mouhadi S (2015) Magnetic resonance cholangiography: current and future perspectives. Clin Res Hepatol Gastroenterol 39:659–664
Singh A, Gelrud A, Agarwal B (2014) Biliary strictures: diagnostic considerations and approach. Gastroenterol Rep (Oxf) 3:22–31
Tabibian JH, Visrodia KH, Levy MJ, Gostout CJ (2015) Advanced endoscopic imaging of indeterminate biliary strictures. World J Gastrointest Endosc 7:1268–1278
Tringali A, Lemmers A, Meves V et al (2015) Intraductal biliopancreatic imaging: European Society of Gastrointestinal Endoscopy (ESGE) technology review. Endoscopy 47:739–753
de Bellis M, Sherman S, Fogel EL et al (2002) Tissue sampling at ERCP in suspected malignant biliary strictures (part 2). Gastrointest Endosc 56:720–730
Rösch T, Hofrichter K, Frimberger E et al (2004) ERCP or EUS for tissue diagnosis of biliary strictures? A prospective comparative study. Gastrointest Endosc 60:390–396
Weilert F, Bhat YM, Binmoeller KF et al (2014) EUS-FNA is superior to ERCP-based tissue sampling in suspected malignant biliary obstruction: results of a prospective, single-blind, comparative study. Gastrointest Endosc 80:97–104
De Moura DTH, Moura EGH, Bernardo WM et al (2016) Endoscopic retrograde cholangiopancreatography versus endoscopic ultrasound for tissue diagnosis of malignant biliary stricture: systematic review and meta-analysis. Endosc Ultrasound 7:10–19
Lin M, Hair CD, Green LK et al (2014) Endoscopic ultrasound-guided fine-needle aspiration with on-site cytopathology versus core biopsy: a comparison of both techniques performed at the same endoscopic session. Endosc Int Open 2:220–223
Elyaderani MK, Gabriele OF (1980) Brush and forceps biopsy of biliary ducts via percutaneous transhepatic catheterization. Radiology 135:777–778
Jung GS, Huh JD, Lee SU, Han BH, Chang HK, Cho YD (2002) Bile duct: analysis of percutaneous transluminal forceps biopsy in 130 patients. Radiology 7:725–730
Omary RA, Bettmann MA, Cardella JF et al (2003) Quality improvement guidelines for the reporting and archiving of interventional radiology procedures. J Vasc Interv Radiol 14:S293–S295
Saad WE, Wallace MJ, Wojak JC, Kundu S, Cardella JF (2010) Quality improvement guidelines for percutaneous transhepatic cholangiography, biliary drainage, and percutaneous cholecystostomy. J Vasc Interv Radiol 21:789–795
Ierardi AM, Mangini M, Fontana F et al (2013) Usefulness and safety of biliary percutaneous transluminal forceps biopsy (PTFB): our experience. Minim Invasive Ther Allied Technol 3:1–6
Li TF, Ren KW, Han XW (2014) Percutaneous transhepatic cholangiobiopsy to determine the pathological cause of anastomotic stenosis after cholangiojejunostomy for malignant obstructive jaundice. Clin Radiol 69:13–17
Patel P, Rangarajan B, Mangat K (2015) Improved accuracy of percutaneous biopsy using “cross and push” technique for patients suspected with malignant biliary strictures. Cardiovasc Intervent Radiol 38:1005–1010
Brown DB, Nikolic B, Covey AM et al (2012) Quality improvement guidelines for transhepatic arterial chemoembolization, embolization, and chemotherapeutic infusion for hepatic malignancy. J Vasc Interv Radiol 23:287–294
Kim KM, Park JW, Lee JK, Lee KH, Lee KT, Shim SG (2015) A comparison of preoperative biliary drainage methods for perihilar cholangiocarcinoma: endoscopic versus percutaneous transhepatic biliary drainage. Gut Liver 9:791–799
Al Mahjoub A, Menahem B, Fohlen A et al (2017) Preoperative biliary drainage in patients with resectable perihilar cholangiocarcinoma: is percutaneous transhepatic biliary drainage safer and more effective than endoscopic biliary drainage? A meta-analysis. J Vasc Interv Radiol 28:576–582
Miller DL, Vañó E, Bartal G et al (2010) Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. J Vasc Interv Radiol 21:607–615
Karavasilis E, Dimitriadis A, Gonis H, Pappas P, Georgiou E, Yakoumakis E (2014) Effective dose in percutaneous transhepatic biliary drainage examination using PCXMC2.0 and MCNP5 Monte Carlo codes. Phys Med 30:432–436
Etard C, Bigand E, Salvat C et al (2017) Patient dose in interventional radiology: a multicentre study of the most frequent procedures in France. Eur Radiol 27:4281–4290
Degiorgio S, Gerasia R, Liotta F et al (2018) Radiation doses to operators in hepatobiliary interventional procedures. Cardiovasc Intervent Radiol 41:772–780
Yoshinaga S, Suzuki H, Oda I, Saito Y (2011) Role of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) for diagnosis of solid pancreatic masses. Dig Endosc 23(Suppl 1):29–33
Vander Noot MR 3rd, Eloubeidi M, Chen VK et al (2004) Diagnosis of gastrointestinal tract lesions by endoscopic ultrasound-guided fine-needle aspiration biopsy. Cancer 102:157–163
Chen VK, Eloubeidi MA (2005) Endoscopic ultrasound-guided fine-needle aspiration of intramural and extraintestinal mass lesions: diagnostic accuracy, complication assessment, and impact on management. Endoscopy 37:984–989
Mohkam K, Malik Y, Derosas C et al (2017) Percutaneous transhepatic cholangiographic endobiliary forceps biopsy versus endoscopic ultrasound fine needle aspiration for proximal biliary strictures: a single-centre experience. HPB (Oxford) 19:530–537
Savader SJ, Prescott CA, Lund GB, Osterman FA (1996) Intraductal biliary biopsy: comparison of three techniques. J Vasc Interv Radiol 7:743–750
Navaneethan U, Njei B, Lourdusamy V, Konjeti R, Vargo JJ, Parsi MA (2015) Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: a systematic review and meta-analysis. Gastrointest Endosc 81:168–176
Tapping CR, Byass OR, Cast JE (2012) Cytological sampling versus forceps biopsy during percutaneous transhepatic biliary drainage and analysis of factors predicting success. Cardiovasc Intervent Radiol 35:883–889
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Jean Pierre Pelage.
Conflict of interest
The authors declare that they have no conflict of interest.
Statistics and biometry
One of the authors has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because it was a retrospective study, based on acquired data.
Ethical approval
Institutional Review Board approval was obtained.
CPP Nord Ouest-France, reference: CPP A15-D30-VOL.26.
Methodology
• Retrospective
• Observational
• Performed at one institution
Electronic supplementary material
ESM 1
(DOCX 23 kb)
Rights and permissions
About this article
Cite this article
Fohlen, A., Bazille, C., Menahem, B. et al. Transhepatic forceps biopsy combined with biliary drainage in obstructive jaundice: safety and accuracy. Eur Radiol 29, 2426–2435 (2019). https://doi.org/10.1007/s00330-018-5852-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5852-x