Abstract
Stereotactic body radiotherapy (SBRT) has been shown to achieve high local control rates in limited metastatic burden of disease. Few papers reported on the efficacy of SBRT in nodal oligometastases. The primary aim of the present paper was to analyze the treatment outcome in this setting. Data from DESTROY-1 and SRS-DESTROY-2 phase I clinical trials were reviewed and analyzed. These trials were based on a 5 fractions and a single fraction regimens, respectively. End-points of this analysis were toxicity rates, overall response rate (ORR), and local control (LC). Patients treated between December 2003 and January 2018, with any metastatic site, and primary tumor type and histology were included. One hundred-eighty-one patients (M/F: 93/88; median age: 67, range 37–88) treated with SBRT on 253 nodal lesions were analyzed. Initially, the used technique was 3D-CRT (20.9%), while subsequently treatments were delivered by VMAT (79.1%). The total dose to the PTV ranged between 12 Gy/single fraction to 50 Gy/5 fractions. With a median follow-up of 21 months (2–124), no grade 3 acute or late toxicity was recorded. ORR based on functional imaging was 92.5% with a complete response rate of 76%. Two- and three-year actuarial LC were 81.6% and 76.0%, respectively. Our large pooled analysis confirms the efficacy and safety of SBRT/SRS in patients with nodal metastases and identifies clinical and treatment variables able to predict complete response and local control rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The oligometastatic status is considered as a transition zone between local and disseminated cancer disease. A recent consensus recommendation proposed a comprehensive classification of oligometastatic disease on the basis of a decision tree of five binary disease characterization factors [1]. This interest in a more detailed classification of these patients, together with a growing evidence on improved outcome when systemic therapy is combined to local therapies in this setting, suggests an increasing role of the latter in this field.
From the radiation oncologists perspective, the Stereotactic Body Radiotherapy (SBRT) represents nowadays the cutting-edge technology in the oligometastatic setting, being a non-invasive radiotherapy (RT) technique allowing the delivery of high total dose in few fractions, with consequent high Local Control (LC) probability [2,3,4].
The rapid development of high precision RT equipment and image-guided techniques has allowed SBRT application in primary or oligometastatic cancers, including unresectable pancreatic cancer [5], kidney tumors [6], as well as other abdominal-pelvic [7,8,9] and thoracic lesions [10,11,12]. Very recently, a retrospective multicenter Italian study confirmed the activity and safety of SBRT in very large, real-world data set of patients with oligometastatic ovarian cancer identifying clinical and treatment parameters able to predict complete response and LC rates [13].
A promising setting for SBRT is represented by lymph node metastases, with a growing body of evidence although generally of weak level [8, 14,15,16,17,18,19,20,21,22,23,24]. Indeed, nodal involvement represents a sign of spreading disease and therefore is frequently treated by systemic instead of local treatment. In reality, the use of SBRT in these patients could have several goals, such as to treat patients with potentially curative purposes, or to delay the use of systemic therapies, or to delay the transition to subsequent systemic therapy lines.
A literature review suggested that SBRT may be a safe and effective approach to nodal oligometastases, offering excellent in-field LC with a low toxicity profile. However, the majority of reports were retrospective and based on small patients series with heterogeneous primary tumor [25].
At our Institution, two prospective phase I dose-escalation trials (DESTROY-1, DESTROY-2) were designed and carried out in order to define the maximum tolerated dose (MTD) in patients treated with fractionated SBRT or single fraction stereotactic radio-surgery (SRS) [26,27,28,29,30,31]. The aim of this pooled analysis is to report the results recorded in these two studies in terms of toxicity, response, and LC.
Methods and materials
Study design and end-points
This is a monocentric, retrospective pooled analysis of the DESTROY trials aimed at assessing the efficacy and safety of SBRT/SRS in nodal oligometastases [30, 31].
In detail, DESTROY-1 was a multi-arm phase I study on SBRT delivered with fixed non-coplanar conformal fields (3D-CRT) or Volumetric Modulated Arc Therapy (VMAT) in patients with primary or metastatic tumors in various extra-cranial body sites [31]. DESTROY-2 was a radiosurgery trial based on the SRS delivered by VMAT technique in patients with primary or metastatic tumors in various extra-cranial body sites [30].
Both trials were approved by the local Ethics Committee and the Institutional Review Board (Destroy-1: P#594/CE/2003 and Destroy-2: P#988/CE/2010) and all patients signed a written informed consent before treatment.
Primary end-point of Destroy-1 and Destroy-2 trials was the definition of the MTD of SBRT and SRS in different treatment settings, respectively. The co-primary endpoints of the studies were complete response and 2-year actuarial LC (progression of disease inside SBRT field) rates on a “per lesion” basis. The secondary end-points were rate and severity of acute and late toxicities as well as 2-year actuarial late toxicity free survival.
Inclusion criteria were: age > 18 years, histological proven solid tumor, adequate performance status (ECOG 0–3), < 5 nodal lesions, salvage surgery or other local therapies not feasible. Only patients with oligometastatic, oligoprogressive or oligorecurrent nodal lesions (any site) were included in this analysis.
Procedures
All patients underwent planning CT-simulation with the Elekta Stereotactic Body Frame (SBF; Elekta Oncology Systems, Crawley, UK) based on a stereotactic system of coordinates for target position. The Gross Tumor Volume (GTV) was identified by CT and/or CT-PET and/or MRI and the clinical target volume (CTV) was defined as the GTV. An experienced senior radiologist (GS) reviewed all diagnostic and simulation images. Organ motion and set-up analyses were performed for Planning Target Volume (PTV) definition as previously described [30, 31].
Treatment planning
In the aforementioned papers [30, 31], the treatment planning devices, techniques, constraints and quality assurance controls have been reported in details. In particular, the first 53 lesions (20.9%) were treated by 3D Conformal Radiotherapy Technique (3D-CRT) with non-coplanar beams (tetrahedral static beam configuration) [26, 27] while, subsequently, 200 lesions (79.1%) were treated with VMAT technique [28,29,30,31].
In the DESTROY-1 protocol, the total dose, prescribed to the target isocenter (International Commission on Radiation Units and Measurements-ICRU report 62), ranged from 20 to 50 Gy (Biologic Effective Dose, BEDα/β=10 = 28–100 Gy) according to the different study arms and patients cohorts, while the doses per fraction ranged from 4 to 10 Gy along 5 days.
In the DESTROY-2 protocol, for each plan of SRS trial the isodose surface (IDS) was selected as the greatest IDS fulfilling the two following criteria: 95% of the PTV volume reached 100% of the prescription dose and 99% of the PTV reached ≥ 90% of the prescription dose, as per ROSEL study [32]. Tight MLC beam margins (0–1 mm) were used to obtain inhomogeneous dose distributions (especially in the center of the lesion where dose is allowed to reach up to 140% of prescription dose) and to enhance the steepness of dose gradient outside the target volume [33]. The total dose ranged from 12 to 24 Gy (BEDα/β=10 = 26.4–93.6 Gy) according to the different arms and anatomical sites as per DESTROY-2 protocol.
Response assessment
Four-months after treatment, the evaluation of response was carried out by morphological (contrast enhanced CT scan and/or MRI) or by functional imaging modalities (18F-fluorodeoxyglucose (FDG)-PET or choline PET for prostate cancer). RECIST (Response Evaluation Criteria in Solid Tumors) system [34] and EORTC (European Organization for Research and Treatment of Cancer) criteria [35] were used to assess objective tumor response, respectively. Overall Response Rate (ORR) included Complete Response (CR) and Partial Response (PR) while Clinical Benefit (CB) included ORR and Stable Disease (SD).
Actuarial LC was defined as the time interval between the date of SBRT and the date of the in-field relapse/progression of disease or the last seen date. Metastases Free-Survival (MFS) was defined as the time interval between the date of SBRT and the date of out of field progression or the last follow-up visit. PFS was defined as the time between the date of the SBRT and the date of first event (local or distant progression) or the last follow-up visit for censored patients still negative for relapse. Overall Survival (OS) was defined as the time interval between the date of SBRT and the date of death or the last follow-up visit. Acute and late toxicities were evaluated by RTOG/EORTC and CTCAE 4.03 scales, respectively, according to protocols [36, 37].
Analysis of data and statistical methods
Data were collected at the Radiotherapy Unit of Gemelli Molise Hospital, Campobasso, Italy, and entered into an electronic database. The data processing was carried out by GM, FD and SC. Patient characteristics were represented as frequencies and percentages for categorical variables, and medians and ranges for continuous variables. The Pearson χ2 test was used to test differences between subgroups. Statistical significance was defined as p-value < 0.05. Univariate and multivariate analysis of factors predicting clinical CR on “per lesion” basis was carried out by logistic regression. The results of the logistic regression model are expressed as odds ratios with 95% confidence intervals.
Actuarial outcomes were calculated using the Kaplan–Meier method. Differences between subgroups were evaluated by log-rank tests and Cox’s regression model for univariate and multivariate analyses, respectively. Statistical analysis was performed using XLSTAT statistical software (Addinsoft, Paris, France).
Results
One hundred eighty-one (181) patients carrying a total of 253 nodal metastases underwent SBRT (on consecutive weekdays) or SRS between December 2003 and January 2018 and were selected for this analysis. As shown in Table 1, the male/female ratio was 93/88 and the median age was 67 years (range: 37–88). Most patients (92.8%) presented Eastern Cooperative Oncology Group (ECOG) performance status 0–1. The most frequent primary tumor was gynecological cancer (N = 53; 29.3%), followed by prostate (N = 37; 20.4%) and gastrointestinal tumors (N = 25; 13.8%). One hundred and three patients (56.9%) have been already treated by RT before SBRT/SRS (Table 1), in particular 77 (42.5%) of them were re-irradiated on the same site of previous treatment (data not shown). The large majority of patients received chemotherapy (68.0%) and/or hormonal therapy (15.5%) before SBRT, however no more details about schedules or timing are available (Table 1).
SBRT treatment on “per lesion” basis
Table 2 shows characteristics of lesions (N = 253), and treatment details. The most frequent anatomical sites were thorax (36.4%) followed by pelvis (34.8%) and abdomen (24.1%). One hundred thirty-five patients presented only 1 lesion (74.6%) and received a single SBRT course, while concurrent or sequential SBRT treatments were carried out in 46 patients bearing > 1 lesion. The median Planning Target Volume (PTV) was 24.4 cc (range 1.4–144.5). SBRT was administered using a standard linear accelerator (ELEKTA Precise) and a VMAT (N = 200, 79.1%), or 3D-CRT (N = 53, 20.9%) technique.
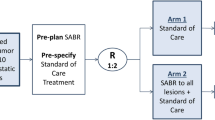
All patients completed the SBRT/SRS as planned. Overall, the prescribed median total dose was 35 Gy (range 12–50 Gy) given in 1–5 fractions, with a median dose per fraction of 8 Gy (range 4–24 Gy). A variety of schedules in terms of dose and fractionation schemes was used, according to the trials design (Fig. 1). The biologically effective dose (BED) was calculated considering two different α/β ratio values (10 and 3 Gy) to account for both early and late responding tissues (BEDα/β10, BEDα/β3). The median BEDα/β10 was 59.5 Gy (range 26.4–100.0 Gy) and the median BEDα/β3 was 93.3 Gy (range 16.0–133.3 Gy) in the whole series. Two hundred and two lesions (79.8%) were treated by SBRT (multiple fractions), and 51 (20.2%) lesions were treated by single fraction (radiotherapy, SRS). Treatment fractionations were chosen on the basis of the study protocol.
In details, the most frequent schedules for SBRT were 6 Gy × 5 fractions, 7 Gy × 5 fractions, and 8 Gy × 5 fractions (Fig. 1a). The median dose delivered by SBRT was 35 Gy (range: 20–50 Gy) with a median BEDα/β10 of 59.5 Gy (range: 28–100 Gy) and a median BEDα/β3 of 116.7 Gy (range: 46.7–216.7 Gy).
As per SRS, the most frequently adopted schedule was 20 Gy × 1 fraction, as reported in Fig. 1b. The median dose delivered by SRS was 18 Gy (range 12–24); in terms of BEDα/β10 and BEDα/β3, the median BEDα/β10 was 50.4 Gy (range 26.4–81.6 Gy) and the median BEDα/β3 was 126 Gy (range 60–216 Gy) (individual data not shown). Five lesions were treated by 12 Gy as a retreatment after 45 Gy: this relatively low dose was constrained by healthy tissues tolerance.
Efficacy
As shown in Table S1 (Supplementary Material), the 4 months-clinical response was evaluated in 239 of 253 lesions (94.5%) by morphological imaging (CT scan and/or MRI examinations). The ORR of target lesions was 60.7%, including 101 CR (42.3%) and 44 PR (18.4%). Moreover, SD was observed in 88 (36.8%) lesions, while SBRT/SRS in-field progression was documented in 6 (2.5%) lesions (Table S1).
The 4 months-clinical response was evaluated in 200 of 253 lesions (79.1%) also by functional imaging (PET-CT). The ORR of target lesions was 92.5% including: 152 CR (76%), 33 PR (16.5%), 12 SD (6.0%), and 3 SBRT/SRS in-field progression (1.5%) (Table S1).
As shown in Table 3, univariate analysis of variables predicting CR per lesion showed that female gender, ECOG 0–1 and planning target volume (PTV) ≥ 24.4 cc were significantly associated with higher CR rates. Multivariate analysis confirmed the statistically significant independent role of the same variables in predicting clinical CR (Table 3).
An easy tool aimed at CR prediction on per lesion basis, according to different combinations of the variables included in the final multivariate model, except from the ECOG performance status, due to the small number of subjects with worse values (ECOG 2–3), is shown in Fig. S1 (Supplementary Material). For instance, lymph node lesions with PTV ≤ 24.4 cc, in female patients showed the highest CR rate (85.7%). In contrast, large lesions with PTV > 24.4 cc in male patients had the lowest percentage of CR (57.6%). Notably, the CR could be evaluated at morphological or functional imaging.
Clinical outcomes
With a median follow-up of 21 months (range 2–124), we recorded progressive disease in 46 of 253 irradiated lesions (18.2%). The 2- and 3-year actuarial LC rates were 81.6%, and 76.0%, respectively (Fig. 2a).
Univariate analysis of variables predicting “per lesion” LC rate showed that ECOG 0–1 and achievement of CR were significantly associated with a higher probability of LC rate. In the multivariate analysis, only the achievement of CR resulted significantly associated with improved LC rate (Table 4).
As far as the outside field actuarial recurrence rate is concerned, the 2- and 3-year actuarial MFS rates were 40.9% and 31.3%, respectively (Fig. 2b). The 2- and 3- year actuarial PFS rates were 34.9% and 25.7%, respectively (Fig. 2b), while the 2- and 3-year actuarial OS rates were 78.2%, and 66.9%, respectively (Fig. 2d).
Safety
All patients received the prescribed SBRT/SRS treatment and were included in the safety analysis. Details concerning the time of onset, type and severity of complications are provided in Table S2 (Supplementary Material).
Of 181 patients, 68 patients (37.6%) experienced mild acute toxicity, totalling 78 side effects of which 62 were grade 1, and 16 grade 2 (Table S2).
Only 23 patients (12.7%) presented late toxicity accounting for 27 side effects of which 19 were grade 1, and 8 grade 2. The most represented late adverse effect was the radiologic findings of asymptomatic pneumonia in 13 patients, while the most severe were pulmonary and subcutaneous ones, with 4 and 3 grade 2 toxicities, respectively. The 2- and 3-year late toxicity free survival rates were 87.8%, and 82.3%, respectively.
Discussion
Isolated lymph node metastases are a common route of cancer spread and can be found at the time of diagnosis as well as during follow-up, with variable incidence according to primary tumor, stage, histology and grading.
In the treatment of nodal metastases, SBRT seems to be a potentially effective and safe option due to the high biological equivalent deliverable dose and reduced irradiation of healthy tissues, with the possibility to avoid the not negligible complications caused by lymph node dissection. The majority of published studies are retrospective and inhomogeneous in terms of patient characteristics, assessment modalities, treatment planning and delivery techniques [8, 14,15,16,17,18,19,20,21,22,23,24,25]. Moreover, in most cases the available analyses have a small sample size.
To the best of our knowledge, this is the largest series on SBRT/SRS treatments of nodal metastases. In fact, the present study included 253 nodal recurrences from 181 patients undergone stereotactic irradiation over a period of 15 years. Our findings are in line with the available literature, particularly in terms of long-lasting local control (2-year LC: 81.6%), and PFS (2-year PFS: 34.9%). Most recorded side effects were mild and more than half of patients did not experience any toxicity.
The PET-CT overall and complete response rate reached 92.5% and 76%, respectively. These findings are slightly higher than those registered with morphological imaging and those reported in other series [8, 13]. Different imaging modalities have different diagnostic sensitivity which could influence the results. For example, Trippa and colleagues in their paper on SBRT for lymph node relapse in ovarian cancer reported the highest rate of CR (100.0%) using 18F-FDG PET-CT [21], while Scorsetti and colleagues recorded the lowest CR (0.0%) using CT [38].
Among clinical and treatment parameters, only female gender, ECOG 0–1 and PTV ≤ 24.4 cc resulted as independent predictors of CR. Indeed, different predictive models and nomograms have been published in different scenarios in order to help clinical decisions [13, 39,40,41,42]. In this trial, an easy tool aimed to predict the rate of complete response was provided as a result of data analysis (Fig. S1). The independent favourable role of lower tumor volume in predicting CR has been already reported by other studies [8, 43]. Moreover, it should be noted that our target volumes were slightly smaller compared to Jereczek-Fossa et al. series (median PTV: 29.1 cc) [8] or Alongi et al. series (median PTV: 56.7 cc) [43] and this could explain the higher response rates recorded in our analysis.
As far as the LC rate is concerned, the favorable performance status (ECOG 0–1), probably related to the possibility to perform other subsequent systemic treatments, seems to act as a major driver in LC, as well as the achievement of a complete response that impacts on LC rate, as showed in univariate and multivariate analyses. In the present series, SBRT treatment provided a high and durable LC rate (2-year and 3-year rate: 81.6% and 76.0%, respectively) in line with other studies: in fact, we were able to find 11 studies [9, 12, 14,15,16,17,18,19,20,21,22] reporting two-year LC with a median of 77.8% and a range of 63.1–90.6% and only 4 studies reporting three-year LC, with a median of 77.5% and a range of 64.3–90.6% [8, 15, 22, 23, 43, 44]. In particular, in a series of 25 patients with nodal recurrences from prostate cancer treated with SBRT, Casamassima et al. reported a 3-year LC rate of 90% [15], while, in the largest published series on SBRT treatment of solitary lymph node metastasis from different primary tumors, Jereczek-Fossa et al. found a 3 years—LC rate of 64% [8] suggesting that long-term results are affected by histology and other systemic therapies. In contrast to other more recent published studies investigating the SBRT in parenchymal metastasis [45, 46], our findings in nodal disease show that LC is not influenced by BED. This is probably due to the reported high local control that could be explained by the histological nature of lesions treated. In fact, it is known that lymph node and parenchymal metastases show different response rates [13].
Despite the encouraging LC rate, in our series the PFS remains low (2-year and 3-year actuarial PFS rates: 34.9% and 25.7%, respectively). In literature, eight [9, 12, 14,15,16,17, 19, 24] and two studies [12, 15] reported 2-year (median 34.4%; range: 17.0%–72.7%) and 3-year (17.0% and 22.5%) PFS analyzed with an actuarial method, respectively. The worst result (median PFS: 9 months, 2-year PFS: 17%,) was reported by Franceschini and coll. who treated thoracic nodal metastases using SBRT (30–60 Gy in 5–8 fractions) [24]. The best result (2-year PFS: 72.7%) was recorded by Franzese et al. who treated abdominal-pelvic nodal metastases with SBRT (45 Gy in 6 fractions) [16]. This large variability suggests to combine SBRT with systemic therapies in order to improve outcomes. Therefore, prospective studies about the optimal combination between therapies in different settings (primary tumor, number of lesions, previous treatments and outcome) are required. Moreover, mostly when micro-metastasis in neighbouring lymph nodes are suspected, the association of ablative high dose radiotherapy and extended nodal irradiation with conventional fractionation could be an option to take into account.
A quite favourable toxicity profile was recorded in our series, allowing us to consider SBRT technique as cost effective. In fact, even if all SBRT treatments were delivered with a “consecutive days” schedule, which elsewhere was reported to be more toxic than an “every other day” treatment [44], in our series no grade 3 acute toxicity was registered, and more than half of patients did not experience any toxicity at all. Moreover, no late severe toxicity was observed, notwithstanding previous medical and surgical cancer treatments, as per patients’ characteristics. This finding is a further confirmation of the safety of this technique, also in unfit settings, likely due to the large use of intensity modulated radiotherapy techniques and to the small target volumes both likely explaining the high tolerability registered in our series.
The strengths of our analysis included the large numbers of treated lesions with lengthy patient’s follow-up, while the weaknesses include the inhomogeneous patient population in terms of primary tumors, being some histological types probably more amenable to oligometastases radical treatment than others [3]. Also, as we selected the patients from two different dose escalation protocols started in 2003, the specific patient cohorts (i.e., gynecologic cancer patients, prostate cancer patients, gastrointestinal cancer patients, etc.) represent smaller subgroups that did not provide us with the statistical power to perform sub-analysis. Furthermore, the change in baseline imaging throughout the long accrual period has to be acknowledged; indeed, CT and MRI were more used in the early years of the study, while PET-CT imaging became available in our center only later. Finally, another weakness is represented by the range of doses utilized in our trial, sometimes providing a relatively lower biologically effective dose compared with other studies [8]. Therefore, we are unable to draw firm conclusions about the best fractionation or the total dose to be preferred. Surely, according to a very recent paper on ovarian cancer, lymph node lesions show a higher responsiveness compared with parenchymal disease, and this behaviour has been mentioned in the literature [13], but a comprehensive evaluation of this issue is still lacking. In conclusion, our large pooled analysis confirms the efficacy and safety of SBRT/SRS in patients with nodal metastases and identifies clinical and treatment variables able to predict complete response and local control rate. Due to the lack of optimal SBRT/SRS schedules as well as standard criteria to identify the patients who can benefit most from this treatment, the development of predictive models seems today more than ever useful and justified.
Abbreviations
- SBRT:
-
Stereotactic body radiotherapy
- RT:
-
Radiotherapy
- LC:
-
Local control
- MTD:
-
Maximum tolerated dose
- SRS:
-
Stereotactic radio-surgery
- 3D-CRT:
-
3-Dimensional conformal radiotherapy
- VMAT:
-
Volumetric modulated arc therapy
- ECOG:
-
Eastern cooperative oncology group
- SBF:
-
Stereotactic body frame
- GTV:
-
Gross tumor volume
- CT:
-
Computer tomography
- PET:
-
Positron emission tomography
- MRI:
-
Magnetic resonance imaging
- CTV:
-
Clinical target volume
- PTV:
-
Planning target volume
- BED:
-
Biologic effective dose
- ORR:
-
Overall response rate
- CR:
-
Complete response
- PR:
-
Partial response
- CB:
-
Clinical benefit
- SD:
-
Stable disease
- MFS:
-
Metastases free-survival
- PFS:
-
Progression free-survival
- OS:
-
Overall survival
References
Guckenberger M, Lievens Y, Bouma AB, Colette L, Dekker A, deSouza NM et al (2020) Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol 21:e18–e28. https://doi.org/10.1016/S1470-2045(19)30718-1
Tree AC, Khoo VS, Eeles RA, Ahmed M, Dearnaley DP, Hawkins MA et al (2013) Stereotactic body radiotherapy for oligometastases. Lancet Oncol 14:e28–37. https://doi.org/10.1016/S1470-2045(12)70510-7
Milano MT, Katz AW, Zhang H, Okunieff P (2012) Oligometastases treated with stereotactic body radiotherapy: long-term follow-up of prospective study. Int J Radiat Oncol Biol Phys 83:878–886. https://doi.org/10.1016/j.ijrobp.2011.08.036
de Vin T, Engels B, Gevaert T et al (2014) Stereotactic radiotherapy for oligometastatic cancer: a prognostic model for survival. Ann Oncol 25:467–471. https://doi.org/10.1093/annonc/mdt537
Chang DT, Schellenberg D, Shen J, Kim J, Goodman KA, Fisher GA et al (2009) Stereotactic radiotherapy for unresectable adenocarcinoma of the pancreas. Cancer 115:665–672. https://doi.org/10.1002/cncr.24059
Wersall PJ, Blomgren H, Lax I, Kälkner KM, Linder C, Lundell G et al (2005) Extracranial stereotactic radiotherapy in primary and metastatic renal cell carcinoma. Radiother Oncol 77:88–95. https://doi.org/10.1016/j.radonc.2005.03.022
Wulf J, Hadinger U, Oppitz U, Thiele W, Flentje M (2004) Stereotactic boost irradiation for targets in abdomen and pelvis. Radiother Oncol 70:31–36. https://doi.org/10.1016/j.radonc.2003.10.013
Jereczek-Fossa BA, Piperno G, Ronchi S, Catalano G, Fodor C, Cambria R et al (2014) Linac-based stereotactic body radiotherapy for oligometastatic patients with single abdominal lymph node recurrent cancer. Am J Clin Oncol 37:227–233. https://doi.org/10.1097/COC.0b013e3182610878
Zeng XL, Wang HH, Meng MB, Wu ZQ, Song YC, Zhuang HQ et al (2016) Stereotactic body radiation therapy for patients with recurrent pancreatic adenocarcinoma at the abdominal lymph nodes or postoperative stump including pancreatic stump and other stump. Onco Targets Ther 9:3985–3992. https://doi.org/10.2147/OTT.S102784
Nagata Y, Matsuo Y, Takayama K, Norihisa Y, Mizowaki T, Mitsumori M et al (2007) Current status of stereotactic radiotherapy for lung cancer. Int J Clin Oncol 12:3–7. https://doi.org/10.1007/s10147-006-0646-6
Ricardi U, Badellino S, Filippi AR (2015) Stereotactic body radiotherapy for early stage lung cancer: history and updated role. Lung Cancer 90:388–396. https://doi.org/10.1016/j.lungcan.2015.10.016
Horne ZD, Richman AH, Dohopolski MJ, Clump DA, Burton SA, Heron DE (2018) Stereotactic body radiation therapy for isolated hilar and mediastinal non-small cell lung cancers. Lung Cancer 115:1–4. https://doi.org/10.1016/j.lungcan.2017.10.014
Macchia G, Lazzari R, Colombo N, Laliscia C, Capelli G, D'Agostino GR et al (2019) A large, multicenter, retrospective study on efficacy and safety of stereotactic body radiotherapy (SBRT) in oligometastatic ovarian cancer (MITO RT1 study): a collaboration of MITO, AIRO GYN, and MaNGO groups. Oncologist. https://doi.org/10.1634/theoncologist.2019-0309
Bignardi M, Navarria P, Mancosu P, Cozzi L, Fogliata A, Tozzi A et al (2011) Clinical outcome of hypofractionated stereotactic radiotherapy for abdominal lymph node metastases. Int J Radiat Oncol Biol Phys 81:831–838. https://doi.org/10.1016/j.ijrobp.2010.05.032
Casamassima F, Masi L, Menichelli C, Bonucci I, Casamassima E, Lazzeri M et al (2011) Efficacy of eradicative radiotherapy for limited nodal metastases detected with choline PET scan in prostate cancer patients. Tumori 97:49–55
Franzese C, Cozzi L, Franceschini D, D'Agostino G, Comito T, De Rose F et al (2016) Role of stereotactic body radiation therapy with volumetric-modulated arcs and high-intensity photon beams for the treatment of abdomino- pelvic lymph-node metastases. Cancer Invest 34:348–354. https://doi.org/10.1080/07357907.2016.1197235
Franzese C, Lopci E, Di Brina L, D'Agostino GR, Navarria P, Mancosu P et al (2017) 11C-choline-pet guided stereotactic body radiation therapy for lymph node metastases in oligometastatic prostate cancer. Cancer Invest 35:586–593. https://doi.org/10.1080/07357907.2017.1375116
Jereczek-Fossa BA, Fanetti G, Fodor C, Ciardo D, Santoro L, Francia CM et al (2017) Salvage stereotactic body radiotherapy for isolated lymph node recurrent prostate cancer: single institution series of 94 consecutive patients and 124 lymph nodes. Clin Genitourin Cancer 15:e623–e632. https://doi.org/10.1016/j.clgc.2017.01.004
Loi M, Frelinghuysen M, Klass ND, Oomen-De Hoop E, Granton PV, Aerts J et al (2018) Locoregional control and survival after lymph node SBRT in oligometastatic disease. Clin Exp Metastasis 35:625–633. https://doi.org/10.1007/s10585-018-9922-x
Napieralska A, Miszczyk L, Stąpór-Fudzińska M (2016) CyberKnife stereotactic ablative radiotherapy as an option of treatment for patients with prostate cancer having oligometastatic lymph nodes: single-center study outcome evaluation. Technol Cancer Res Treat 15:661–673. https://doi.org/10.1177/1533034615595945
Trippa F, Casale M, Draghini L, Anselmo P, Arcidiacono F, Maranzano E (2016) Stereotactic body radiotherapy for lymph node relapse in ovarian cancer. Clin Oncol 1:1038
Wang Z, Wang J, Zhuang H, Wang P, Yuan Z (2016) Stereotactic body radiation therapy induces fast tumor control and symptom relief in patients with iliac lymph node metastasis. Sci Rep 6:37987. https://doi.org/10.1038/srep37987
Bae SH, Kim MS, Cho CK, Kang JK, Kang HJ, Kim YH et al (2012) High dose stereotactic body radiotherapy using three fractions for colorectal oligometastases. J Surg Oncol 106:138–143. https://doi.org/10.1002/jso.23058
Franceschini D, De Rose F, Fogliata A, Navarria P, Ascolese AM, Franzese C et al (2016) Volumetric modulated arc therapy for thoracic node metastases: a safe and effective treatment for a neglected disease. Oncotarget 7:53321–53329
Jereczek-Fossa BA, Ronchi S, Orecchia R (2015) Is stereotactic body radiotherapy (SBRT) in lymph node oligometastatic patients feasible and effective? Rep Pract Oncol Radiother 20:472–483. https://doi.org/10.1016/j.rpor.2014.10.004
Deodato F, Macchia G, Grimaldi L et al (2009) Stereotactic radiotherapy in recurrent gynecological cancer: a case series. Oncol Rep 22:415–419
Macchia G, Morganti AG, Cilla S et al (2012) Quality of life and toxicity of stereotactic radiotherapy in pancreatic tumors: a case series. Cancer Invest 30:149–155. https://doi.org/10.3109/07357907.2011.640649
Deodato F, Cilla S, Macchia G et al (2013) Extracranial radiosurgery with volumetric modulated arc therapy: Feasibility evaluation of a phase I trial. Oncol Lett 5:1889–1896. https://doi.org/10.3892/ol.2013.1276
Macchia G, Deodato F, Cilla S, Torre G, Corrado G, Legge F et al (2014) Volumetric intensity modulated arc therapy for stereotactic body radiosurgery in oligometastatic breast and gynecological cancers: feasibility and clinical results. Oncol Rep 32(5):2237–2243. https://doi.org/10.3892/or.2014.3412
Deodato F, Cilla S, Macchia G, Torre G, Caravatta L, Mariano G, Mignogna S, Ferro M, Mattiucci GC, Balducci M, Frascino V, Piermattei A, Ferrandina G, Valentini V, Morganti AG (2014) Stereotactic radiosurgery (SRS) with volumetric modulated arc therapy (VMAT): interim results of a multi-arm phase I trial (DESTROY-2). Clin Oncol (R Coll Radiol) 26(12):748–756. https://doi.org/10.1016/j.clon.2014.08.005
Deodato F, Macchia G, Cilla S, Ianiro A, Sallustio G, Cammelli S, Buwenge M, Mattiucci GC, Valentini V, Morganti AG (2019) Dose escalation in extracranial stereotactic ablative radiotherapy (DESTROY-1): a multiarm phase I trial. Br J Radiol 92:1094. https://doi.org/10.1259/bjr.20180422
Hurkmans CW, Cuijpers JP, Lagerwaard FJ et al (2009) Recommendations for implementing stereotactic radiotherapy in peripheral stage IA non-small cell lung cancer: report from the Quality Assurance Working Party of the randomised phase III ROSEL study. Radiat Oncol 4:1
Cilla S, Ianiro A, Deodato F, Macchia G, Digesù C, Valentini V, Morganti AG (2018) Optimal beam margins in linac-based VMAT stereotactic ablative body radiotherapy: a Pareto front analysis for liver metastases. Med Dosim 43(3):291–301
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L et al (2000) New guidelines to evaluate the response to treatment in solid tumors (RECIST guidelines). J Natl Cancer Inst 92:205–216. https://doi.org/10.1093/jnci/92.3.205
Young H, Baum R, Cremerius U, Herholz K, Hoekstra O, Lammertsma AA et al (1999) Measurement of clinical and subclinical response using [18 20 F]-fluorodeoxiglucose and positron emission tomography: review and 1999 EORTC recommendations. Eur J Cancer 35:1773–1782. https://doi.org/10.1016/s0959-8049(99)00229-4
Cox JD, Stetz J, Pajak TF (1995) Toxicity criteria of the radiation therapy oncology group (RTOG) and the Eropean organization for research and treatment of cancer (EORTC). Int J Radiat Oncol Biol Phys 31:1341–1346. https://doi.org/10.1016/0360-3016(95)00060-C
National Cancer Institute (2020) Common Terminology Criteria for Adverse Events v.4.03 (CTCAE v.4.03). https://ctep.cancer.gov/protocolDevelopment
Scorsetti M, Bignardi M, Alongi F, Fogliata A, Mancosu P, Navarria P et al (2011) Stereotactic body radiation therapy for abdominal targets using volumetric intensity modulated arc therapy with RapidArc: feasibility and clinical preliminary results. Acta Oncol 50:528–538. https://doi.org/10.3109/0284186X.2011.558522
Tanadini-Lang S, Rieber J, Filippi AR, Fode MM, Streblow J, Adebahr S, Andratschke N, Blanck O, Boda-Heggemann J, Duma M, Eble MJ, Ernst I, Flentje M, Gerum S, Hass P, Henkenberens C, Hildebrandt G, Imhoff D, Kahl H, Klass ND, Krempien R, Lohaus F, Petersen C, Schrade E, Wendt TG, Wittig A, Høyer M, Ricardi U, Sterzing F, Guckenberger M (2017) Nomogram based overall survival prediction in stereotactic body radiotherapy for oligo-metastatic lung disease. Radiother Oncol 123(2):182–188. https://doi.org/10.1016/j.radonc.2017.01.003
Klement RJ, Abbasi-Senger N, Adebahr S, Alheid H, Allgaeuer M, Becker G, Blanck O, Boda-Heggemann J, Brunner T, Duma M, Eble MJ, Ernst I, Gerum S, Habermehl D, Hass P, Henkenberens C, Hildebrandt G, Imhoff D, Kahl H, Klass ND, Krempien R, Lewitzki V, Lohaus F, Ostheimer C, Papachristofilou A, Petersen C, Rieber J, Schneider T, Schrade E, Semrau R, Wachter S, Wittig A, Guckenberger M, Andratschke N (2019) The impact of local control on overall survival after stereotactic body radiotherapy for liver and lung metastases from colorectal cancer: a combined analysis of 388 patients with 500 metastases. BMC Cancer 19(1):173. https://doi.org/10.1186/s12885-019-5362-5
Franceschini D, De Rose F, Franzese C, Comito T, Di Brina L, Radicioni G, Evangelista A, D'Agostino GR, Navarria P, Scorsetti M (2019) Predictive factors for response and survival in a cohort of oligometastatic patients treated with stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys 104(1):111–121. https://doi.org/10.1016/j.ijrobp.2018.12.049
Valentini V, van Stiphout RG, Lammering G, Gambacorta MA, Barba MC, Bebenek M, Bonnetain F, Bosset JF, Bujko K, Cionini L, Gerard JP, Rödel C, Sainato A, Sauer R, Minsky BD, Collette L, Lambin P (2011) Nomograms for predicting local recurrence, distant metastases, and overall survival for patients with locally advanced rectal cancer on the basis of European randomized clinical trials. J Clin Oncol 29(23):3163–3172. https://doi.org/10.1200/JCO.2010.33.1595
Alongi F, Fogliata A, Clerici E, Navarria P, Tozzi A, Comito T et al (2012) Volumetric modulated arc therapy with flattening filter free beams for isolated abdominal/pelvic lymph nodes: report of dosimetric and early clinical results in oligometastatic patients. Radiat Oncol 7:204. https://doi.org/10.1186/1748-717X-7-204
King CR, Brooks JD, Gill H, Presti JC Jr (2012) Long-term outcomes from a prospective trial of stereotactic body radiotherapy for low-risk prostate cancer. Int J Radiat Oncol Biol Phys 82:877–882. https://doi.org/10.1016/j.ijrobp.2010.11.054
Rieber J, Streblow J, Uhlmann L, Flentje M, Duma M, Ernst I, Blanck O, Wittig A, Boda-Heggemann J, Krempien R, Lohaus F, Klass ND, Eble MJ, Imhoff D, Kahl H, Petersen C, Gerum S, Henkenberens C, Adebahr S, Hass P, Schrade E, Wendt TG, Hildebrandt G, Andratschke N, Sterzing F, Guckenberger M (2016) Stereotactic body radiotherapy (SBRT) for medically inoperable lung metastases-a pooled analysis of the German working group "stereotactic radiotherapy". Lung Cancer 97:51–58. https://doi.org/10.1016/j.lungcan.2016.04.012
Andratschke N, Alheid H, Allgäuer M, Becker G, Blanck O, Boda-Heggemann J, Brunner T, Duma M, Gerum S, Guckenberger M, Hildebrandt G, Klement RJ, Lewitzki V, Ostheimer C, Papachristofilou A, Petersen C, Schneider T, Semrau R, Wachter S, Habermehl D (2018) The SBRT database initiative of the German Society for Radiation Oncology (DEGRO): patterns of care and outcome analysis of stereotactic body radiotherapy (SBRT) for liver oligometastases in 474 patients with 623 metastases. BMC Cancer 18(1):283. https://doi.org/10.1186/s12885-018-4191-2
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Deodato, F., Ferro, M., Cilla, S. et al. Stereobody radiotherapy for nodal recurrences in oligometastatic patients: a pooled analysis from two phase I clinical trials. Clin Exp Metastasis 37, 519–529 (2020). https://doi.org/10.1007/s10585-020-10039-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-020-10039-x