Abstract
This study aimed to identify the prognostic value of lymph node metastasis in patients with non-small cell lung cancer (NSCLC) and distant organ metastasis. A total of 42,613 NSCLC patients with distant metastasis from the surveillance, epidemiology, and end results database between 2010 and 2013 were included for analysis. The proportion of N0 stage in M1a patients was significantly higher than that in M1b patients, 34.0% and 22.7% respectively (P < 0.001). Compared with N0 patients, patients had higher odds of experiencing multiorgan metastases (MOM) if they had higher N stage at diagnoses (P < 0.001). The Kaplan–Meier curves suggested both M1a and M1b groups patients at stage N0 had better survival than those at higher N stage (P < 0.001). Further analysis indicated that better survival was observed in N0 stage compared with N2 or N3 stage if patients had bone metastasis, brain metastasis, or MOM (P < 0.001, P < 0.001, and P = 0.002, respectively), but there was no significant difference in survival among each N stage patients with liver metastasis only. Cox regression analysis showed that compared with N0 patients, higher hazard for disease-specific mortality was observed for patients with higher N stage. Among NSCLC patients with distant organ metastasis, lymph node metastasis was associated with higher odds of experiencing MOM and a worse prognosis in terms of longer survival except patients with liver metastasis. Better understandings of the role of lymphatic metastasis in M1 NSCLC could help clinicians with better management of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the second most common cancer among both males and females. The American Cancer Society estimated that 116,990 men and 105,510 women developed new lung and bronchus cancers in 2017, with 84,590 men and 71,280 women dying from them [1]. The estimated numbers of new cases and deaths were comparable to those in 2014 [2]. In addition, Bray et al. have reported that lung cancer was the leading cause of cancer mortality for women in 17 countries and for men in 94 countries [3]. Non-small cell lung cancer (NSCLC) and small cell lung cancer are the two major histological variants that account for 90% of lung cancers, with the major variants of NSCLC being adenocarcinoma (AD) and squamous cell carcinoma (SQCC). Lung cancer patients have a low 5-year survival rate [4] and approximately 40% of new NSCLC cases have distant metastases at diagnosis [5].
The eighth edition of the lung cancer staging system developed by the International Association for the Study of Lung Cancer (IASLC) has significant revisions regarding distant metastasis, while the lymph node (N) descriptors remained unchanged [6]. The 8th edition defines M1a as intrathoracic metastases, M1b as a single extra-thoracic metastasis, and M1c as multiple extra-thoracic metastases. For patients with distant metastasis, tumor, node, and metastasis (TNM) stage is determined only by M stage. IVA stage includes any T, any N, M1a and M1b; IVB stage includes any T, any N, and M1c. Previous studies have also demonstrated that multiorgan metastasis predict inferior survival in M1 NSCLC [7, 8]. It has been revealed that lymph node metastasis might have prognostic value in M1a NSCLC [9], and N2 disease is associated with poor survival in oligometastatic NSCLC [10], but the impact of N status on the outcome of NSCLC patients with specific organ metastasis, especially multiorgan metastases (MOM) remains to be determined. Identifying factors with prognostic value may contribute to management of disease [11], thus determining effective predictors of survival especially in late stage NSCLC is of great importance.
In the present study, we aimed to investigate the relationship between lymph node metastasis and distant organ metastasis and how N stage affects the outcome of M1 disease in NSCLC patients using surveillance, epidemiology, and end results (SEER) database.
Methods
Patients and clinicopathologic data
This retrospective study assessed (1) the association of N stage with distant metastases and (2) the prognostic value of N stage among patients with M1 NSCLC. Data for a large number of NSCLC patients were obtained from the SEER database, which was launched in 1973 by the National Cancer Institute and consists of 18 population-based cancer registries, covering approximately 28% of the total population of the United States.
The present study included NSCLC patients with M1 disease who were diagnosed between 2010 and 2013 and had complete information. We initially identified 90,817 cases of lung cancer, 20,576 cases with two or more primary sites, 6918 with incomplete information on organs metastases, 55 cases with no information on survival, 17,845 cases with small cell lung cancer, and 2810 patients with incomplete N stage and histological information. Thus, a total of 42,613 NSCLC patients were eligible analyses, with 26,457 AD cases and 8637 SQCC cases. All patients had distant metastasis at diagnosis and complete information regarding N stage. TNM stage information in the present SEER database was based on the 7th TNM staging system. N stage is defined as follows: N0 stage as no regional lymph node metastasis, N1 stage as metastasis in the ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension, N2 stage as metastasis in the ipsilateral mediastinal and/or subcarinal lymph node(s), and N3 stage as metastasis in the contralateral mediastinal, contralateral hilar, ipsilateral, contralateral scalene, or supraclavicular lymph node(s). M1 is classified as two stages, M1a: presence of a malignant pleural or pericardial effusion, pleural dissemination, or pericardial disease, and metastasis in opposite lung; M1b: extrathoracic metastases. Multiorgan metastases refers to patients with two or more metastatic organs among lung, liver, brain and bone as previously described [7]. The endpoint of the present study was lung cancer specific survival, which was defined as the interval from diagnosis until death due to lung cancer or until the last follow-up.
Statistical analyses
Patient characteristics were statistically described. Pearson’s Chi square test was used to detect differences for categorical variables. Differences in NSCLC-specific survival time were compared among patients of different N stage using Kaplan–Meier analysis and the log-rank test. Cox regression analysis was used to investigate the predictors of survival, and binary logistic regression analysis was performed to calculate the odds ratios (ORs) of experiencing various organ metastases. Differences were considered statistically significant at two-tailed p-values of less than 0.05. All analyses were performed using IBM SPSS software (version18.0; IBM Corp., Armonk, NY).
Results
Patient characteristics
Table 1 shows the clinical characteristics of total populations and subtypes, respectively. A total of 42,613 NSCLC patients (23,642 male and 18,971 female) were analyzed. The histological type AD had 26,475 cases and SQCC had 8637 cases. The median age for the overall population was 67 years [interquartile range (IQR): 59–76 years] and the median follow-up time was 4 months (IQR 1–10 months). There were 25.9% (11,057 cases) patients diagnosed at N0 stage, 8.1% (3443 cases) at N1 stage, 46.0% for N2 stage (19,609 cases), and 20.0% for N3 stage (8504 cases). The primary tumors were more common on the right side (54.9% overall, with 28.4% on the right upper lobe) and less common on the left side (39.1% overall) (Table 2).
Association between N stage and M stage in M1 NSCLC patients
Table 3 shows that in NSCLC patients, the proportion of N0 in M1a was significantly higher than that in M1b, 34.0% and 22.7% respectively (P < 0.001). Interestingly, the proportions of patients with N1, N2 and N3 were all lower in M1a NSCLC patients than that in M1b (P < 0.001). In the subgroup analysis, similar results were obtained in AD patients, with N0 rate as high as 36.8% in M1a disease. While in SQCC patients, N0 rate was also higher in M1a group although the difference between M1a and M1b was relatively smaller compared with AD patients, and the N2 proportion between M1a and M1b group failed to reach statistical difference.
Association between N stage and MOM
The proportion of patients diagnosed at stage N0, N1, N2, and N3 who developed MOM was 18.7%, 25.0%, 29.3%, and 33.6%, respectively (Table 4). Compared with the N0 group, the odds of having MOM were higher for patients diagnosed at stage N1 (OR 1.45 [1.33–1.59], P < 0.001), N2 (OR 1.80 [1.70–1.90], P < 0.001), and N3 (OR 2.19 [2.06–2.34], P < 0.001). After adjusting for age, sex, and tumor size, the ORs remained significant in N1 group (OR 1.30 [1.17–1.44]), N2 group (OR 1.70 [1.59–1.81]), and N3 group (OR 1.96 [1.81–2.11]) (all P < 0.001). Similar results were observed in the AD and SQCC subgroups (Table 4).
Association between N stage and disease-specific survival
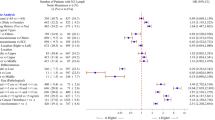
The effects of N stage on disease-specific survival among overall NSCLC patients and two histological subtypes are shown in Figs. 1, 2 and 3. Survival decreased with increasing N stage (P < 0.001), with the best survival observed in the N0 group, intermediate survival observed in N1 group, and similarly poor survival observed in both N2 and N3 groups (N3 vs. N2, P = 0.511) (Fig. 1). Similar results were observed when conducting analyses in AD and SQCC subgroups (Fig. 2).
Further analysis showed that in M1a patients, N0 stage was associated with better outcome compared with higher N stage, with 1- and 3-year survival rates as high as 42.3% and 19.3%, respectively (P < 0.001) (Table 5) (Fig. 3a). Similar results were obtained in M1b disease (Table 5) (Fig. 3b). M1a patients had better survival than M1b patients, but the difference between N3M1a and N0M1b was not significant (P = 0.574) (Table 5). In the subgroup analysis for the M1b group, better survival was observed in N0 stage compared with N2 or N3 stage if patients had bone metastasis only, brain metastasis only, or MOM (P < 0.001, P < 0.001, and P = 0.002, respectively), but there was no significant difference in survival among each N stage patients with liver metastasis only (Fig. 4).
Cox regression analysis was performed to investigate the effect of N stage on disease-specific mortality risk of M1 NSCLC patients. Compared with patients diagnosed at N0 stage, patients diagnosed at N1 stage had higher hazard for crude mortality (HR 1.12 [1.07–1.17], P < 0.001) and for age, sex, M stage, and tumor size adjusted mortality (HR 1.13 [1.07–1.19], P < 0.001). For crude mortality, higher hazards were also observed for patients diagnosed at N2 stage (HR 1.23 [1.20–1.27], P < 0.001) and N3 stage (HR 1.23 [1.19–1.27], P < 0.001). Furthermore, for age, sex, M stage, and tumor size adjusted mortality, N2 group (HR 1.26 [1.22–1.30], P < 0.001) and N3 group (HR 1.29 [1.23–1.34], P < 0.001) had higher hazards compared to N0 group. Similar results were observed for the AD and SQCC subgroups (Table 6).
Discussion
In the newly developed 8th edition American Joint Committee on Cancer (AJCC) TNM staging manual for NSCLC, T descriptor and M descriptor were both revised, while N descriptors remained unchanged. Lymph node involvement is an important demarcation criterion for the staging of M0 patients, whereas stage IV is classified as IVA and IVB only based on the M stage, without concern of N status. It is well accepted that lymph node metastasis is a key predictor of outcome in M0 NSCLC [12], but few studies have focused on whether N status plays an important role in M1 patients [9, 10]. This study evaluated the relationships between lymph node metastasis and distant metastasis in NSCLC patients and further identified the prognostic value of N stage in M1 patients.
Our primary finding is that patients with M1a (intra-thoracic metastasis) NSCLC trends to have lower N stage compared with M1b (distant metastasis) patients, as N1, N2, and N3 rates in M1b were all significantly higher than those in M1a (Table 3). We observed that nearly 34% of M1a and 22.7% of M1b patients had no lymph node involvement in our study, which could be explained by that blood vessel dissemination is responsible for distant metastasis of cancer [13]. Nevertheless, we observed that lymph node metastasis is associated with higher risk of MOM in NSCLC patients. It has been a subject of considerable debate whether cancer cells in lymph nodes can seed distant organs. It is possible that primary tumors may remain noninvasive until somehow triggered to metastasize via both lymphatics and blood vessels simultaneously [14]. As lymph nodes are often the first site of metastasis, it is also possible that lymphatics serve as part of pathway contributing to the subsequent dissemination to distant organs [15]. Experimental evidence has demonstrated that inhibiting lymphatic dissemination could be a promising method for preventing distant metastases [16,17,18]. The exact mechanism of how lymphatic spread leads to systematic metastasis remains unclear, most likely through the left lymphatic duct (thoracic duct) or the right lymphatic duct and subsequently into the subclavian veins [14]. Recent studies revealed that lymph node metastases can disseminate by invading lymph node blood vessels rather than by transiting through efferent lymphatic vessels in a mouse model, but whether this form of tumor cell spreading occurs in cancer patients remains to be determined [19, 20]. Our findings also shed light on the important role of lymphatic route in distant metastasis.
Lymph node status is a powerful prognostic predictor as many studies have demonstrated that lymphatic metastasis is an independent prognostic factor for NSCLC [21, 22]. Lymphatic metastasis after surgical resection of NSCLC has been shown to be the most important determinant of long-term outcome [21], and even lymphatic micrometastasis could predict poor prognosis [23]. In the present study, earlier N stage was associated with better disease-specific survival, based on the result of Kaplan–Meier analysis that N0 patients had the best survival while N2 and N3 was associated with worse survival. Analyses of the current N descriptors at clinical and pathological staging in the IASLC database showed that they clearly separate lung cancers of significantly different prognosis [6]. In this cohort of patients, the 3-year survival rates were significantly lower than AJCC guidelines estimates due to the research design that our study only included patients with M1 disease at diagnosis. Despite the difference and limitation, our findings did highlight a similar trend to AJCC guidelines’ estimates, that the survival was best for patients diagnosed at N0 stage and poorest at N2 or N3 stage. Similar trends were noticed in the sub-group analysis of M1a and M1b disease. In addition, our results showed that although M1a disease was associated with better survival compared with M1b, N3M1a had equal survival as N0M1b. To exclude the impact of other prognostic factors, Cox regression analysis was employed to confirm the effect of N status in NSCLC and its two pathological subtypes AD and SQCC, showing that increasing N status was associated with higher risk of mortality after adjusted for age, sex, tumor size and M stage. These findings provide evidence for the prognostic value of lymph node metastasis in M1 NSCLC, and may be relevant for the next version of TNM staging system.
Interestingly, in the subgroup analysis we found that the effect of lymph node metastasis was significantly attenuated in liver metastasis only group, which might be related to the strong negative effect of liver metastasis as previous studies have reported [8, 24, 25]. The exact mechanism why liver metastasis is associated with poorer survival is still not clear. More research will be necessary to study the molecular mechanisms of liver metastasis in lung cancer in order to devise effective treatment strategies. In the bone metastasis only group, brain metastasis only group, and MOM group, the best survival was observed in N0 patients, and N2–3 was associated with worse survival, while the difference between N0 and N1 group did not reach statistical significance. Although bone metastasis, brain metastasis, and MOM were associated with poor survival, our results showed that lymph node metastasis still had prognostic value and should be considered in the management of disease.
This study has several limitations. Firstly, metastases were identified based on the 7th edition of the AJCC guidelines, which did not provide information on the number of metastasis in the metastatic organ. Secondly, metastasis information was only available for the four common metastatic organs (lung, bone, brain, and liver) starting from 2010. This limited the data and population that could be included and omitted the influence of patients with metastases to other organs. In addition, the SEER database did not provide details regarding the methods used to determine N stage, and information such as comorbidities, treatment details, and gene mutations were also not available, which prevented us from further stratification analysis. Therefore, more research will be needed to confirm our findings.
Conclusion
In conclusion, these results reveal lymph node metastasis is associated with higher risk of MOM in M1 NSCLC. Our study also provides evidence that lymph node status has important prognostic value in patients with M1 NSCLC and may help guide the next TNM staging system. Knowledge of these findings may be helpful when making precise prognostic evaluation and treatment decisions for NSCLC patients.
Abbreviations
- AD:
-
Adenocarcinoma
- AJCC:
-
American Joint Committee on Cancer
- HRs:
-
Hazard ratios
- IASLC:
-
International Association for the Study of Lung Cancer
- IQR:
-
Interquartile range
- MOM:
-
Multiorgan metastases
- NSCLC:
-
Non-small cell lung cancer
- ORs:
-
Odds ratios
- SEER:
-
Surveillance, epidemiology and end results
- SQCC:
-
Squamous cell carcinoma
- TNM:
-
Tumor, node, and metastasis
References
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67(1):7–30. https://doi.org/10.3322/caac.21387
Siegel R, Desantis C, Jemal A (2014) Colorectal cancer statistics, 2014. CA Cancer J Clin 64(2):104–117. https://doi.org/10.3322/caac.21220
Bray F, Jemal A, Grey N, Ferlay J, Forman D (2012) Global cancer transitions according to the Human Development Index (2008–2030): a population-based study. Lancet Oncol 13(8):790–801. https://doi.org/10.1016/S1470-2045(12)70211-5
Detterbeck FC, Boffa DJ, Kim AW, Tanoue LT (2017) The eighth edition lung cancer stage classification. Chest 151(1):193–203. https://doi.org/10.1016/j.chest.2016.10.010
Morgensztern D, Ng SH, Gao F, Govindan R (2010) Trends in stage distribution for patients with non-small cell lung cancer: a National Cancer Database survey. J Thorac Oncol 5(1):29–33. https://doi.org/10.1097/JTO.0b013e3181c5920c
Rami-Porta R, Asamura H, Travis WD, Rusch VW (2017) Lung cancer—major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 67(2):138–155. https://doi.org/10.3322/caac.21390
Yang J, Zhang Y, Sun X, Gusdon AM, Song N, Chen L, Jiang G, Huang Y (2018) The prognostic value of multiorgan metastases in patients with non-small cell lung cancer and its variants: a SEER-based study. J Cancer Res Clin Oncol 144(9):1835–1842. https://doi.org/10.1007/s00432-018-2702-9
Ren Y, Dai C, Zheng H, Zhou F, She Y, Jiang G, Fei K, Yang P, Xie D, Chen C (2016) Prognostic effect of liver metastasis in lung cancer patients with distant metastasis. Oncotarget 7(33):53245–53253. https://doi.org/10.18632/oncotarget.10644
Dai C, Ren Y, Xie D, Zheng H, She Y, Fei K, Jiang G, Chen C (2016) Does lymph node metastasis have a negative prognostic impact in patients with NSCLC and M1a disease? J Thorac Oncol 11(10):1745–1754. https://doi.org/10.1016/j.jtho.2016.06.030
Johnson KK, Rosen JE, Salazar MC, Boffa DJ (2016) Outcomes of a highly selective surgical approach to oligometastatic lung cancer. Ann Thorac Surg 102(4):1166–1171. https://doi.org/10.1016/j.athoracsur.2016.04.086
Ettinger DS, Wood DE, Akerley W, Bazhenova LA, Borghaei H, Camidge DR, Cheney RT, Chirieac LR, D’Amico TA, Demmy TL, Dilling TJ, Dobelbower MC, Govindan R, Grannis FW Jr, Horn L, Jahan TM, Komaki R, Krug LM, Lackner RP, Lanuti M, Lilenbaum R, Lin J, Loo BW Jr, Martins R, Otterson GA, Patel JD, Pisters KM, Reckamp K, Riely GJ, Rohren E, Schild SE, Shapiro TA, Swanson SJ, Tauer K, Yang SC, Gregory K, Hughes M, National Comprehensive Cancer Network (2015) Non-small cell lung cancer, Version 6.2015. J Natl Compr Cancer Netw 13(5):515–524
Asamura H, Chansky K, Crowley J, Goldstraw P, Rusch VW, Vansteenkiste JF, Watanabe H, Wu YL, Zielinski M, Ball D, Rami-Porta R, International Association for the Study of Lung Cancer S, Prognostic Factors Committee ABM, Participating I (2015) The International Association for the Study of Lung Cancer Lung Cancer Staging Project: proposals for the revision of the N descriptors in the forthcoming 8th edition of the TNM classification for lung cancer. J Thorac Oncol 10(12):1675–1684. https://doi.org/10.1097/jto.0000000000000678
Leung E, Xue A, Wang Y, Rougerie P, Sharma VP, Eddy R, Cox D, Condeelis J (2017) Blood vessel endothelium-directed tumor cell streaming in breast tumors requires the HGF/C-Met signaling pathway. Oncogene 36(19):2680–2692. https://doi.org/10.1038/onc.2016.421
Wong SY, Hynes RO (2006) Lymphatic or hematogenous dissemination: how does a metastatic tumor cell decide? Cell Cycle 5(8):812–817. https://doi.org/10.4161/cc.5.8.2646
Podgrabinska S, Skobe M (2014) Role of lymphatic vasculature in regional and distant metastases. Microvasc Res 95:46–52. https://doi.org/10.1016/j.mvr.2014.07.004
Brakenhielm E, Burton JB, Johnson M, Chavarria N, Morizono K, Chen I, Alitalo K, Wu L (2007) Modulating metastasis by a lymphangiogenic switch in prostate cancer. Int J Cancer 121(10):2153–2161. https://doi.org/10.1002/ijc.22900
Burton JB, Priceman SJ, Sung JL, Brakenhielm E, An DS, Pytowski B, Alitalo K, Wu L (2008) Suppression of prostate cancer nodal and systemic metastasis by blockade of the lymphangiogenic axis. Cancer Res 68(19):7828–7837. https://doi.org/10.1158/0008-5472.CAN-08-1488
Roberts N, Kloos B, Cassella M, Podgrabinska S, Persaud K, Wu Y, Pytowski B, Skobe M (2006) Inhibition of VEGFR-3 activation with the antagonistic antibody more potently suppresses lymph node and distant metastases than inactivation of VEGFR-2. Cancer Res 66(5):2650–2657. https://doi.org/10.1158/0008-5472.CAN-05-1843
Brown M, Assen FP, Leithner A, Abe J, Schachner H, Asfour G, Bago-Horvath Z, Stein JV, Uhrin P, Sixt M, Kerjaschki D (2018) Lymph node blood vessels provide exit routes for metastatic tumor cell dissemination in mice. Science 359(6382):1408–1411. https://doi.org/10.1126/science.aal3662
Pereira ER, Kedrin D, Seano G, Gautier O, Meijer EFJ, Jones D, Chin SM, Kitahara S, Bouta EM, Chang J, Beech E, Jeong HS, Carroll MC, Taghian AG, Padera TP (2018) Lymph node metastases can invade local blood vessels, exit the node, and colonize distant organs in mice. Science 359(6382):1403–1407. https://doi.org/10.1126/science.aal3622
Osarogiagbon RU, Allen JW, Farooq A, Berry A, Spencer D, O’Brien T (2010) Outcome of surgical resection for pathologic N0 and Nx non-small cell lung cancer. J Thorac Oncol 5(2):191–196. https://doi.org/10.1097/JTO.0b013e3181c8cc32
Osarogiagbon RU, Allen JW, Farooq A, Berry A, O’Brien T (2011) Pathologic lymph node staging practice and stage-predicted survival after resection of lung cancer. Ann Thorac Surg 91(5):1486–1492. https://doi.org/10.1016/j.athoracsur.2010.11.065
Ohta Y, Oda M, Wu J, Tsunezuka Y, Hiroshi M, Nonomura A, Watanabe G (2001) Can tumor size be a guide for limited surgical intervention in patients with peripheral non-small cell lung cancer? Assessment from the point of view of nodal micrometastasis. J Thorac Cardiovasc Surg 122(5):900–906. https://doi.org/10.1067/mtc.2001.117626
Tamura T, Kurishima K, Nakazawa K, Kagohashi K, Ishikawa H, Satoh H, Hizawa N (2015) Specific organ metastases and survival in metastatic non-small-cell lung cancer. Mol Clin Oncol 3(1):217–221. https://doi.org/10.3892/mco.2014.410
Riihimaki M, Hemminki A, Fallah M, Thomsen H, Sundquist K, Sundquist J, Hemminki K (2014) Metastatic sites and survival in lung cancer. Lung Cancer 86(1):78–84. https://doi.org/10.1016/j.lungcan.2014.07.020
Acknowledgements
We would like to thank all the staff of National Cancer Institute for their effort to the SEER program.
Funding
This work was supported by National Natural Science Foundation of China No. 81600052 (J. Y.) and the Fundamental Research Funds for the Central Universities No. 22120180022 (J. Y.).
Author information
Authors and Affiliations
Contributions
Conception and design: J.Y., G.J., and P.Z.; Acquisition, statistical analysis or interpretation of the data: All authors; Drafting of the manuscript: J.Y., A.P., and B.W.; All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors disclose no potential conflicts of interest related to this study.
Ethical approval
Our study was approved by the ethical committee board of Shanghai Pulmonary Hospital and complied with 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, J., Peng, A., Wang, B. et al. The prognostic impact of lymph node metastasis in patients with non-small cell lung cancer and distant organ metastasis. Clin Exp Metastasis 36, 457–466 (2019). https://doi.org/10.1007/s10585-019-09985-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-019-09985-y