Abstract
Platelet-rich plasma (PRP) has been widely used in clinical practice for more than 20 years because it causes the release of many growth factors. However, the burst release pattern and short release period of PRP have become obstacles to its application. An optimal controllable release system is an urgent need for researchers. This study investigated whether collagen/PRP (COL/PRP) scaffolds can serve as a vehicle for the controllable release of growth factors. We fabricated a novel scaffold that integrates PRP activated by thrombin or collagen into type I collagen. The mechanical properties, cytotoxicity, and transforming growth factor β1 (TGF-β1), platelet derived growth factor (PDGF), fibroblast growth factor (FGF) and vascular endothelial growth factor (VEGF) content were evaluated. Our results demonstrate that the COL/PRP scaffolds were not cytotoxic to L-929 fibroblasts. The PDGF and FGF content in the thrombin group was at a higher level and lasted for a long period of time. Collagen and thrombin played the same role in the release of TGF-β1 and VEGF. These data suggest that the novel COL/PRP scaffolds provide a carrier for the controllable release of growth factors and may be used in tissue- regenerative therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Platelet-rich plasma (PRP), the plasma part of blood, has gained attention because it can be used not only as an adjunctive therapeutic agent for injuries of the musculoskeletal system but also for the treatment of osteoarthritis. The conventional role of platelets is mainly to promote hemostasis. Most studies have focused on this topic over the past century (Sampson et al. 2008). Many tissue-healing proteins can be released from the α-granules of platelets following activation. Over the last 20 years, these proteins have been called growth factors and have gained much attention from researchers (Werner and Grose 2003). The ease of its preparation and its safe clinical application have made PRP a welcome therapeutic agent.
However, liquid PRP can diffuse into circumambient tissue, resulting in significant loss of the growth factors within the PRP. Determining how to maintain a higher concentration of these cytokines for a longer period of time within damaged tissue has become one of the challenges facing doctors and researchers. Thrombin or calcium chloride has often been used to activate platelets and to gelatinize PRP. Many growth factors, such as transforming growth factor β1 (TGF-β1), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF), are released from the α-granules of platelets following activation. Several publications have reported gelatinizing PRP by using thrombin or calcium chloride and have applied these gelatins at the site of tissue injury, with satisfactory results (Foster et al. 2009; Alsousou et al. 2009; Anitua et al. 2008; Kocaoemer et al. 2007; Sánchez et al. 2009). Nevertheless, approximately 70 % of the growth factors are released in the first 10 min and 100 % are released within an hour (Foster et al. 2009). This burst release pattern makes it difficult for the cytokines to play a role in regenerative therapies for damaged tissue. Recently, to augment efficacy and effect of growth factors, gelatin microspheres, freeze-dried PRP, alginate beads, and chitosan scaffolds have been used as controlled release systems (Bir et al. 2009; Pietramaggiori et al. 2006, 2007, 2008; Sum et al. 2007; Lu et al. 2008; Kutlu et al. 2013; Busilacchi et al. 2013).
Collagen plays a considerable role in many supporting and connective tissues. Type I collagen has attracted the most attention due to its abundance, excellent biocompatibility, and ubiquity. Thus, type I collagen has been widely used as a biomaterial in tissue engineering. In addition, type I collagen can cause clotting of PRP and can stimulate growth factor release from platelets and granulocytes (Fufa et al. 2008).
The aim of this study was to prepare and compare two types of novel collagen/PRP COL/PRP scaffolds, generated by (1) mixing type I collagen with thrombin-activated PRP or (2) mixing type I collagen with PRP, followed by freeze drying. It was hypothesized that the COL/PRP scaffolds would possess certain basic characteristics of bioscaffolds, without cytotoxicity. Moreover, the expected effect of collagen on the growth factor release kinetics was sustained release over an ideal delivery period, with efficacy similar to that of thrombin.
Materials and methods
PRP preparation and component analysis
A total of 6–8 mL blood was extracted from the heart of adult Sprague-Dawley (SD) rats (at least 6 weeks old, mass 220–260 g, Center of Experimental Animals, People’s Liberation Army, China) under aseptic conditions. Anticoagulant dextrose solution A (ACD-A, BD Vacutainer, Becton Drive, Franklin Lakes, NJ, USA) was used as an anticoagulant agent. The counts of leukocytes, erythrocytes and platelets in 5 whole-blood samples were measured using an automated animal blood counter (Hemavet 950, Drew Scientific, Dallas, TX, USA). PRP was prepared as previously described (Nagae et al. 2007). When the blood samples were centrifuged at 1500 rpm for 10 min, the blood separated into three phases: platelet-poor plasma (top), the PRP, containing leukocytes and platelets (middle), and erythrocytes (bottom). The top and middle layers were transferred to new tubes and centrifuged again at 3000 rpm for 10 min. The supernatant plasma was discarded, and the remaining 500 μL plasma, containing precipitated platelets, was blended evenly and designated as PRP. Five samples of PRP were then analyzed using an automated animal blood counter and stored at −80 °C.
Preparation of type I collagen and COL/PRP scaffolds
Type I collagen was prepared using our previously reported method (Zhang et al. 2014). The freeze-dried collagen films were lysed in 0.5 M ethanoic acid solution and adjusted pH value of 7. Samples of PRP were thawed at room temperature and poured into 48-well microplates (300 μL/well). The mixture of 300 μL PRP + 30 μL thrombin (30 IU, Sigma, USA) was defined as the thrombin-activated group, 300 μL PRP + 300 μL collagen solution was the collagen-activated group, and 600 μL collagen was the blank group. Ten minutes later, 300 μL collagen solution was added to each well of the thrombin group. The mixed solutions were stirred uniformly and freeze dried.
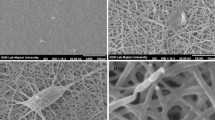
Scanning electron microscopy (SEM) observation
The morphology of the prepared scaffolds was observed by SEM (JSM-6360LV, JEOL, Japan). The matrices were fixed on copper stubs using mutual conductive adhesive tape and were covered with gold using a sputter coater.
Analysis of mechanical properties
Mechanical testing was carried out using a material testing machine (Instron 5540, USA) and by compression in the vertical direction at a deformation rate of 1.5 mm/min and a temperature of 20 °C until failure. The compressive strength was calculated as Q = Fmax/S, where Fmax is the maximum load on the load-deformation curve and S is the cross-sectional area of each sample (n = 5). The blank group was set as the control.
Cultivation of the L-929 cell line
L-929 mouse fibroblast cells were seeded in 25 cm2 cell culture flasks with 5 ml low-glucose Dulbecco’s modified Eagle’s medium (L-DMEM, Hyclone, USA) supplemented with 10 % fetal bovine serum (FBS, Hyclone, USA) and were cultured at 37 °C and 5 vol% CO2. The culture medium was changed once every other day. When cells reached confluency, the passaging was performed.
Cytotoxicity analysis
The cytotoxicity of the samples (n = 5) was assessed by the MTT colorimetric assay. COL/PRP scaffolds were sterilized with ethylene oxide and immersed in L-DMEM at 37 °C for 48 h, after which the conditioned media containing scaffold extracts was collected. L-929 mouse fibroblast cells were seeded in 96-well plates at a density of 4.0 × 103 cells/well in 0.1 mL L-DMEM supplemented with 10 % FBS, and were cultured at 37 °C and 5 vol% CO2 for 24 h, followed by treatment with the leaching liquor from the scaffolds. Cells were treated with L-DMEM as a control group. After 1, 3, and 7 days of culture, the medium was removed and the cells were washed with PBS. Next, 20 μL 0.5 % MTT solution was added to each well, followed by incubation for 4 h at 37 °C and 5 vol% CO2. Subsequently, the MTT solution was removed, and 150 μL DMSO was added to each well. The 96-well plates were then placed on a shaker for 10 min, and the optical density (OD) value of each well was measured at 490 nm using an ELISA reader (Bio-Rad, Model II, USA).
Analysis of growth factor release
The ethylene oxide-sterilized COL/PRP scaffolds (n = 5) in each group were immersed in 2 mL L-DMEM at 37 °C. The release of TGF-β1, PDGF, VEGF and FGF from each scaffold was measured at 1, 4, 7 and 10 days. At each time point, 1 mL medium was aspirated from around each sample and replaced with 1 mL fresh medium. The medium samples were stored in 1.8 mL cryovials in a −80 °C freezer until all samples were collected. The concentrations of rat TGF-β1, PDGF, VEGF and FGF were determined using the commercially available Quantikine colorimetric sandwich ELISA kits (Sangon Biotech, China).
Statistical analyses
Statistical analyses were performed using SPSS software, version 16.0 (SPSS Inc, USA). The data are presented as the mean ± SD, and values were compared by one-way repetitive-measure analysis of variance (ANOVA). p values <0.05 were considered as statistically significant.
Results
PRP component analysis
The platelet content in the PRP was 3.91 ± 0.98 times greater than in whole blood after centrifugation. The leukocyte and erythrocyte content was 1.11 ± 0.40 and 0.31 ± 0.20 times greater, respectively, than in whole blood (Table 1).
Morphological characterization of COL/PRP scaffolds
The scaffolds in the different groups were freeze-dried into cylindrical samples of 10 mm in diameter and 5 mm in height. The color of the freeze-dried COL/PRP scaffolds was pink (Fig. 1). The COL/PRP scaffolds were analyzed by SEM and presented a three-dimensional (3D), interconnected porous structure with a pore size ranging from 50 to 80 μm. The blank collagen scaffolds possessed a pore size that ranged from 100 to 250 μm (Fig. 2).
Mechanical properties
The mechanical properties of the scaffolds were evaluated by compression.
The compressive strength of the different groups was about 10 kPa, and there was no significant difference between the groups (p > 0.05) (Fig. 3).
Cytotoxicity analysis
OD values appeared relatively steady from day 1 to day 7. No significant difference was observed between any of the three groups (p > 0.05) (Fig. 4).
Analysis of growth factor release
The TGF-β1 content was highest at day 4. Although the content decreased at days 7 and 10, an elevated concentration could be maintained in each group. There was no significant difference between the groups (p > 0.05). The FGF and PDGF content gradually decreased over time. The concentrations of the two growth factors in the thrombin group were higher than those in the collagen group at each time point. A significant difference was observed between the groups at all time points (p < 0.01). Regarding VEGF, the content increased from day 1 to day 4 and dropped at day 7. However, at day 10, the content increased once again. The concentrations of VEGF in the two groups were similar at each time point. No significant difference was observed between the groups (p > 0.05) (Fig. 5).
Discussion
In recent years, PRP has attracted significant attention because it can be used as a source of growth factors, not only for tissue regenerative therapies but also for cosmetic and plastic surgery (Intini 2009; Nikolidakis and Jansen 2008; Roukis et al. 2006; Farrior and Ladner 2011). Currently, the major applications of PRP include local injection into damaged tissue (Woo et al. 2014), use in its gelatin form, activated by calcium chloride or thrombin, or formulation as an ideal controllable release system by combining PRP with inductive biomaterials. We integrated type I collagen and activated PRP into a 3D scaffold and evaluated the physical and chemical characteristics of this scaffold. In addition, via quantitative detection of growth factors released from the scaffold, we explored the feasibility of using this scaffold as a biomaterial for tissue engineering.
We first assessed the variation in platelet, leukocyte, and erythrocyte content between whole blood and PRP. After centrifugation, the platelets content clearly increased, and a larger number of erythrocytes were exorcized. Interestingly, the leukocyte content did not undergo any change. Certain authors have found that the leukocyte content in human PRP was higher than in whole blood when using the “Harvest Smart” system. In equine PRP, however, the leukocyte content was the same as in peripheral blood (Schnabel et al. 2007; Weibrich et al. 2003). The different genera of experimental object may have induced these different results.
Ideal tissue engineering scaffolds must possess high porosity, with a large surface area/volume ratio to provide suitable space for cell adhesion and proliferation and to allow the exchange of nutrients and waste. In the current study, the COL/PRP scaffolds presented a 3D, interconnected porous structure with a pore sizes ranging from 50 to 80 μm. Compared with those structures with a large pore size that are used for tissue engineering, a small pore size may help to capture nanodimensional growth factors. The other basic requirements for tissue engineering scaffolds are distinguished biocompatibility and low cytotoxicity. Our results were consistent with a recent report (Diaz-Gomez et al. 2014) and demonstrate that COL/PRP were not cytotoxic to L-929 fibroblasts.
Once a platelet is activated, many growth factors, such as TGF-β1, PDGF, VEGF and FGF, are released from the α-granules of the platelet. These cytokines play an important part in tissue regeneration. It is difficult to maintain a suitable cytokine concentration for a prolonged duration, and the burst release pattern of cytokines is an obstacle to regenerative therapies for damaged tissue. Therefore, an optimal delivery system is needed for the application of PRP. To evaluate whether COL/PRP scaffolds could be used as materials for tissue regeneration, we investigated the concentration of growth factors released from COL/PRP scaffolds and the persistence of the released cytokines in vitro. Our data showed that different growth factors showed different time-dependent release patterns in each Group. During the 10 days, for example, the thrombin and collagen groups did not differ in TGF-β1 and VEGF release (p > 0.05). But did differ in PDGF and FGF release (p < 0.01). Prior studies have reported that almost complete release of growth factors from thrombin-activated PRP within the first few hours of activation (Roussy et al. 2007; Su et al. 2008). Our results in the TGF-β1 and VEGF group, however, did not parallel this observation. This may relate to retention properties of the COL/PRP scaffolds and the molecular characteristics of TGF-β1 and VEGF. Anitua reported that the PRP fibrin matrix maintained almost 30 % of the total amount of growth factors for longer than 1 week (Anitua et al. 2013). Maybe our freeze-dried COL/PRP scaffolds play the same role in the retention of the growth factors. TGF-β1 is released from platelets in a latent form and later becomes activated by any number of molecules (Murray et al. 2006). The latent and activated forms of TGF-β1 simultaneously exist in the mammal body. Due to the limitations of our techniques, we could not distinguish between these two forms in rat plasma. The shorter activated time in vitro maybe resulted in the discrepancy of data with other researchers. As far as VEGF, some researchers demonstrated that VEGF had a high affinity to fibrinogen and fibrin (Sahni and Francis 2000), perhaps this could explain the lack of time-dependent changes in VEGF concentrations.
TGF-β1 and PDGF are thought to play a crucial role in the modulation of extracellular matrix deposition and fibrosis in a wide range of tissues (Lee et al. 1998). The latent and activated forms of TGF-β1 simultaneously exist in the human body. Due to the limitations of our techniques, we could not distinguish between these two forms in rat plasma. The results of certain studies have shown that enhancing the normal plasma value of active TGF-β1 by twofold to threefold will cause renal fibrosis in mice (Sanderson et al. 1995). This elevated value also increases cell influx into and matrix deposition onto subcutaneous sponges (Shah et al. 1999). In humans, elevated levels are closely associated with coronary artery disease (Wang et al. 1997). Although the active TGF-β1 content changes slightly, it can have important biological effects on multiple tissues. Our data indicated that a relatively higher concentration of TGF-β1 was found in the collagen-activated group and that both groups could sustain the concentration. The greatest concentration of TGF-β1, or 18 ng/L, was observed from day 1 to day 4, so the adverse effect was minimal. At each time point, the PDGF content in the thrombin-activated group was higher than in the collagen-activated group. The PDGF content in both groups gradually decreased over time. Between the consecutive time points, decreases of 6 and 3 ng/L were detected in the thrombin-activated group and the collagen-activated group, respectively. A similar situation occurred in the detection of FGF. The minor fluctuation of the released cytokines was not consistent with a burst release pattern. Interestingly, the VEGF content in both groups did not gradually decrease over time: it increased from day 1 to day 4 and dropped at day 7. However, at day 10, the content increased once again. Although this wave-like release cannot be explained, the fact remains that the VEGF content can be maintained at a higher level for 10 days.
Many growth factors can be released by platelets following activation. However, a great deal of factors may influence this biological process. For example, the method of collection of plasma, the source of plasma, the variety of activators studied, the temperature, and the pH value may have important effects on the results. Thus, little consensus has been reached regarding how these cytokines affect the regenerative process of damaged tissue. To explore the secrets of this process, further studies should be performed.
Conclusion
This study analyzed the morphology, characterization, mechanical properties, and cytotoxicity of COL/PRP scaffolds. We evaluated whether these scaffolds could be used as carrier systems that provide controlled release of TGF-β1, PDGF, VEGF, and FGF. Higher delivered doses of PDGF and FGF were observed in the thrombin-activated group. Regarding TGF-β1 and VEGF, the collagen and thrombin played the same role in these cytokines’ release. Maybe the molecular characteristics of TGF-β1 and VEGF resulted in this release discrepancy. Our study has demonstrated that COL/PRP scaffolds can serve as an efficient vehicle for growth factors for tissue-regenerative therapies.
References
Alsousou J, Thompson M, Hulley P, Noble A, Willett K (2009) The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg Br 91:987–996
Anitua E, Sanchez M, Orive G, Andia I (2008) Delivering growth factors for therapeutics. Trends Pharmacol Sci 29:37–41
Anitua E, Zalduendo MM, Alkhraisat MH, Orive G (2013) Release kinetics of platelet-derived and plasma-derived growth factors from autologous plasma rich in growth factors. Ann Anat 195:461–466
Bir SC, Esaki J, Marui A, Yamahara K, Tsubota H et al (2009) Angiogenic properties of sustained release platelet-rich plasma: characterization in vitro and in the ischemic hind limb of the mouse. J Vasc Surg 50:870–872
Busilacchi A, Gigante A, Mattioli-Belmonte M, Manzotti S, Muzzarelli RA (2013) Chitosan stabilizes platelet growth factors and modulates stem cell differentiation toward tissue regeneration. Carbohydr Polym 98:665–676
Diaz-Gomez L, Alvarez-Lorenzo C, Concheiro A, Silva M, Dominguez F et al (2014) Biodegradable electrospun nanofibers coated with platelet-rich plasma for cell adhesion and proliferation. Mater Sci Eng C Mater Biol Appl 40:180–188
Farrior E, Ladner K (2011) Platelet gels and hemostasis in facial plastic surgery. Facial Plast Surg 27:308–314
Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA (2009) Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med 37:2259–2272
Fufa D, Shealy B, Jacobson M, Kevy S, Murray MM (2008) Activation of platelet-rich plasma using soluble type I collagen. J Oral Maxillofac Surg 66:684–690
Intini G (2009) The use of platelet-rich plasma in bone reconstruction therapy. Biomaterials 30:4956–4966
Kocaoemer A, Kern S, Klüter H, Bieback K (2007) Human AB serum and thrombin-activated platelet-rich plasma are suitable alternatives to fetal calf serum for the expansionof mesenchymal stem cells from adipose tissue. Stem Cells 25:1270–1278
Kutlu B, Tiğl Aydın RS, Akman AC (2013) Platelet-rich plasma-loaded chitosan scaffolds: preparation and growth factor release kinetics. J Biomed Mater Res B Appl Biomater 101:28–35
Lee J, Harwood FL, Akeson WH, Amiel D (1998) Growth factor expression in healing rabbit medial collateral and anterior cruciate ligaments. Iowa Orthop J 18:19–25
Lu HH, Vo JM, Chin HS, Lin J, Cozin M et al (2008) Controlled delivery of plateletrich plasma-derived growth factors for bone formation. J Biomed Mater Res 15(86):1128–1136
Murray MM, Forsythe B, Chen F, Lee SJ, Yoo JJ et al (2006) The effect of thrombin on ACL fibroblast interactions with collagen hydrogels. J Orthop Res 24(3):508–515
Nagae M, Ikeda T, Mikami Y, Hase H, Ozawa H et al (2007) Intervertebral disc regeneration using platelet-rich plasma and biodegradable gelatin hydrogel microspheres. Tissue Eng 13:147–158
Nikolidakis D, Jansen JA (2008) The biology of platelet-rich plasma and its application in oral surgery: literature review. Tissue Eng B 14:249–258
Pietramaggiori G, Kaipainen A, Czeczuga JM, Wagner CT, Orgill DP (2006) Freeze-dried platelet-rich plasma shows beneficial healing properties in chronic wounds. Wound Repair Regen 14:573–580
Pietramaggiori G, Kaipainen A, Ho D, Orser C, Pebley W et al (2007) Trehalose lyophilized platelets for wound healing. Wound Repair Regen 15:213–220
Pietramaggiori G, Scherer SS, Mathews JC, Alperovich M, Yang HJ et al (2008) Healing modulation induced by freeze-dried platelet-rich plasma and micronized allogenic dermis in a diabetic wound model. Wound Repair Regen 16:218–225
Roukis TS, Zgonis T, Tiernan B (2006) Autologous platelet-rich plasma for wound and osseous healing: a review of the literature and commercially available products. Adv Ther 23:218–237
Roussy Y, Bertrand Duchesne MP, Gagnon G (2007) Activation of human platelet-rich plasmas: effect on growth factors release, cell division and in vivo bone formation. Clin Oral Implants Res 18(5):639–648
Sahni A, Francis CW (2000) Vascular endothelial growth factor binds to fibrinogen and fibrin and stimulates endothelial cell proliferation. Blood 6:3772–3778
Sampson S, Gerhardt M, Mandelbaum B (2008) Platelet rich plasma injection grafts for musculoskeletal injuries: a review. Curr Rev Musculoskelet Med 1:165–174
Sánchez M, Anitua E, Orive G, Mujika I, Andia I (2009) Platelet-rich therapies in the treatment of orthopaedic sport injuries. Sports Med 39:345–354
Sanderson N, Factor V, Nagy P, Kopp J, Kondaiah P et al (1995) Hepatic expression of mature transforming growth factor beta 1 in transgenic mice results in multiple tissue lesions. Proc Natl Acad Sci USA 92:2572–2576
Schnabel LV, Mohammed HO, Miller BJ, McDermott WG, Jacobson MS et al (2007) Platelet rich plasma (PRP) enhances anabolic gene expression patterns in flexor digitorum superficialis tendons. J Orthop Res 2:230–240
Shah M, Revis D, Herrick S, Baillie R, Thorgeirson S et al (1999) Role of elevated plasma transforming growth factor-beta1 levels in wound healing. Am J Pathol 154:1115–1124
Su CY, Kuo YP, Nieh HL, Tseng YH, Burnouf T (2008) Quantitative assessment of the kinetics of growth factors release from platelet gel. Transfusion 8(11):2414–2420
Sum R, Hager S, Pietramaggiori G, Orgill DP, Dee J et al (2007) Wound-healing properties of trehalose-stabilized freezedried outdated platelets. Transfusion 47:672–679
Wang XL, Liu SX, Wilcken DE (1997) Circulating transforming growth factor beta 1 and coronary artery disease. Cardiovasc Res 34:404–410
Weibrich G, Kleis WK, Buch R, Hitzler WE, Hafner G (2003) The harvest smart PRePTM system versus the Friadent-Schütze platelet-rich plasma kit. Clin Oral Implants Res 2:233–239
Werner S, Grose R (2003) Regulation of wound healing by growth factors and cytokines. Physiol Rev 83:835–870
Woo SH, Jeong HS, Kim JP, Koh EH, Lee SU et al (2014) Favorable vocal fold wound healing induced by platelet-rich plasma injection. Clin Exp Otorhinolaryngol 7:47–52
Zhang X, Chen X, Yang T, Zhang N, Dong L et al (2014) The effects of different crossing-linking conditions of genipin on type I collagen scaffolds: an in vitro evaluation. Cell Tissue Bank 15:531–541
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, X., Wang, J., Ren, M. et al. A novel collagen/platelet-rich plasma (COL/PRP) scaffold: preparation and growth factor release analysis. Cell Tissue Bank 17, 327–334 (2016). https://doi.org/10.1007/s10561-016-9551-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-016-9551-z