Abstract
Purpose
Little is known about the causes of central nervous system tumors in children. An inverse association between asthma and brain cancer was found in adults, but there is a dearth of studies in children. The goal of this study was to evaluate the association between asthma and brain cancer in children.
Methods
Two hundred and seventy-two cases of children with brain tumor diagnosed between 0 and 14 years of age in the Province of Québec, Canada, between 1980 and 1999 and 272 incidence density-matched controls were included in the study. The parents of cases and controls were interviewed by phone using structured questionnaires. Besides asthma in children, family history of asthma, the presence of other atopies, and medication intake were also investigated. Conditional logistic regression was used to analyze the data.
Results
Brain tumor risk was decreased in children with asthma (OR, 0.55; CI 95%, 0.33–0.93), with eczema (OR, 0.52; CI 95%, 0.17–1.57), and with both asthma and eczema (OR, 0.76; CI 95%, 0.18–3.2). Maternal or sibling asthma did not modify the effect of asthma on central nervous system (CNS) tumors, while father’s asthma seemed to increase the risk, but numbers were small. Antiasthma medications such as inhaled corticosteroid and beta agonists seemed to increase the risk of CNS tumors (OR for steroids, 2.55; CI 95%, 0.79–8.20 and OR for inhaled beta agonist, 1.62; CI 95%, 0.57–4.63).
Conclusions
This study strengthens the hypothesis of inverse association between asthma and brain cancer in children, but family history and medications for asthma need further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central nervous system (CNS) tumors represent approximately the 22% of all new cases of cancer among Canadian children less than 15 years of age. In this age group, astrocytoma accounts for the 40% of tumors, followed by primitive neuroectodermal tumors (PNET) (22%), other gliomas (12%), other specified intracranial neoplasms (12%), and ependymoma (10%) [1]. Risk factors for CNS studied in adults may be different in children [2]. Current thinking suggests that brain tumors develop in children as a consequence of accumulated genetic alterations that permit cells to evade normal regulatory mechanisms and destruction by the immune system. These alterations in the germ line may be inherited, but neurocarcinogens, agents of a chemical, biological, or physical nature, that damage DNA can lead to somatic mutations [2]. The causes of CNS cancers are largely unknown, but causes are likely to be both genetic and environmental. Some rare family genetic disorders (such as Li-Fraumeni syndrome, neurofibromatosis, Turcot syndrome, tuberous sclerosis, and nevoid basal cell syndrome), as well as other factors such as white race, age, male gender and ionizing radiation exposure, have been associated with CNS tumors in children. Other potential risk factors have been investigated, but the results are inconclusive so far [3]. Among the latter are childhood infections, maternal infections during gestation, parental smoking, maternal dietary intake of N-nitroso compounds (NOC), and drug consumption during pregnancy [4–10].
The role of allergies and asthma on the risk of developing brain tumors in adults has been studied for decades, and the results showing an inverse association between asthma and brain cancer are consistent, even if the underlying mechanism for this finding is still unclear [11–15]. The strongest hypothesis suggested to explain these findings in adults is that the hypersensitive immune system of people affected by asthma is more capable of responding to malignant cells. However, the reverse causality hypothesis, whereby the tumor itself acts as a suppressor of the immune system, has not been excluded. Indeed, it is still unclear, whether allergies protect from brain tumors or whether the immunosuppressive factors secreted by the brain tumor inhibit allergies and asthma [16]. Another hypothesis to explain the inverse association, at least in adults, is, for example, the association of glioma with immunological defects such as abnormal delayed hypersensitivity responses, low numbers of T cells, impaired T-cell cytotoxicity, and decreased antibody response [17].
Despite several studies carried out in adults, only one investigated the association between atopy and brain cancer in children. The findings are consistent with those in adults and show an inverse association between asthma and SNC tumors [18].
The aim of our study is to study the association between brain cancer and asthma in children, considering also parental history of asthma and children’s use of asthma medication.
Methods
Study design
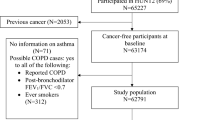
The study is a matched case–control study. As described previously [6], primary malignant brain tumor cases diagnosed in the Province of Québec, Canada, were recruited from tertiary care centers designated by governmental policy to treat childhood cancers. For budgetary reasons, between 1980 and 1993, a random sample of one-third of all brain tumor case diagnosed before 10 years of age was selected from the tertiary centers (n = 130). Between 1995 and 1999, all first primary, malignant brain tumor cases diagnosed in Quebec before 15 years of age were recruited to participate (n = 142). In 1994, no cases were selected due to an interruption of the study. Because brain cancer treatment is covered under the universal Health Care Plan, we believe that a very small number of children, if any, were hospitalized outside the province. The cases were matched to population-based controls (1:1 ratio) for sex and age at diagnosis. Between 1980 and 1993, controls were chosen from family allowance files. Family Allowance is a monthly allowance paid to families with children to help cover the costs of child maintenance; it began in 1945 and was Canada’s first universal welfare program. The term universal is applied to benefits that are awarded solely on the basis of age, residence, or citizenship, without reference to the recipient’s income or assets. The file contains continuously updated information on all children living legally in Canada. From 1995 to 1999, controls were chosen from the continuously updated provincial health insurance agency files where current information on all families living in Québec is maintained to provide universal medical care coverage. These sources of data were the most complete census of children available during the study period. Ten controls per case were randomly chosen from the lists according to the expected distribution of cases. Children who were adopted, who lived in foster families, whose families spoke neither French nor English, who were not Canadian residents, or whose parents were both unavailable for interview were excluded. Response rates were calculated as the number of subjects who participated in the study divided by the total number of eligible subjects, including subjects who were never located or were lost at the follow-up. The response rates for cases from 1980 to 1993 and from 1995 to 1999 were 94.0 and 82.7%, respectively. Among controls, response rates were 83.8 and 90.4%, respectively, during these same periods. Differences in response rates between the study periods are likely due to slightly different methods in recruiting subjects: in the early study period, cases were recruited by the research team, while in the latter study period, cases were first approached by hospital personnel to determine interest in the study. Furthermore, address information provided for control subjects and based on the health insurance files was slightly more accurate than in the family allowance files. The study was approved by each hospital’s institutional review board and the provincial agency regulating access to public databases with nominal information. Soon after sending a letter introducing the general purpose of the study, trained interviewers contacted the parents of cases and controls to schedule an appointment for the interview, which was administered by telephone using a structured questionnaire. It included an explicit question on a diagnosis of asthma for the index child, the child’s siblings, the mother answering for the previous and herself, and for her own family. Although diagnosis “by a physician” was not specified as such, the question was worded to imply it (e.g., “Were you ever diagnosed with asthma?”). Age at diagnosis was also asked. Fathers were interviewed separately with similar questions pertaining to themselves and their own family. There was an open question in the interviewer-administered questionnaire related to other conditions such as eczema and other atopic conditions. Mothers were also asked about their smoking history and vitamin supplementation intake before and during pregnancy. The intake of asthma medication for the index child was studied, including names of the drugs, periods of administration, and doses of the treatment. All reported medications named under immunosuppressive drugs, anti-inflammatory drugs, and any other drugs were reviewed and regrouped into asthma medications categories (long-term control including inhaled corticosteroids, long-acting beta-2 agonists, leukotriene modifiers, cromolyn, theophylline; quick relief medication including short-acting beta-2 agonists, ipratropium, oral or intravenous steroids; and medication for allergy-induced asthma including antihistamines, decongestants, and immunotherapy injections).
Case definition
Cases were clinically and histologically confirmed using international Children’s Oncology Group protocols. We considered as cases the children who had a brain tumor as defined by ICD-O-2 classification: C71.0–71.9, plus cerebral meninges (C70.0), meninges undefined (C 70.9), optic nerve (C72.3) pituitary gland (75.1), craniopharyngeal duct (75.2), and pineal gland (75.3). Brain tumors were classified according to the International Classification of Childhood Cancer: ependymoma, astrocytoma primitive neuroectodermal tumors (PNET), other gliomas, other specified intracranial tumors, and other unspecified intracranial tumors [19].
Statistical analysis
Conditional logistic regression was used and odds ratios (OR) with 95% confidence intervals (CI) estimated. Asthma alone as well as asthma and/or eczema were used as the exposure variable. The ORs were adjusted for mother smoking during the last month of pregnancy, infection of mother during pregnancy, and infection of the child at birth. Although not all previous studies have shown these variables to be risk factors for childhood brain cancer, some have [4–6, 20], justifying the estimation of adjusted measures to be compared with crude measures. Vitamin supplementation during pregnancy was also adjusted for because of the inverse association found between vitamin intake, including folic acid, and reduction in risk of brain cancer in childhood and particularly in PNET [9, 21, 22].
Potential effect modification of asthma on brain tumor by parental history of asthma was evaluated. The effect modification was tested with a chi-squared test and a likelihood ratio test. Unconditional regression was also used adjusting for the matching variables when limiting the analysis to cases and controls taking specific asthma medication and while stratifying for parental history of asthma. Analyses were performed with STATA software package (version11, Stata Corporation, College Station, Texas).
Results
The children’s mean age was 5.92 (SD 3.27) years for cases and 5.85 (SD 3.23) years for controls. The majority of brain tumor cases had astrocytoma (44%), followed by PNET (29%) and ependymoma (10%). The prevalence of reported asthma among cases was 10.3 and 16.2% among controls. In the case group, 11% of mothers had a positive history of asthma, 4.8% of fathers, and 16.2% of siblings; in the control group, these figures were 8.1, 6.3, and 12.5%, respectively (Table 1).
The OR for brain tumors was significantly reduced among subjects with asthma (OR, 0.55; CI 95%, 0.33–0.93). The analysis showed a lower risk for every subgroup of tumors, but the inverse association seemed driven by ependymoma tumors (OR 0.15, CI 95% 0.18–1.21) (Table 2).
A strong inverse association with CNS tumors was found for children with eczema (OR, 0.52; CI 95%, 0.17–1.57) and for children with both asthma and eczema (OR, 0.76; 95% CI, 0.18–3.2), but for these results, a chance finding could not be excluded (Table 3).
Maternal and sibling asthma did not modify the effect of asthma on CNS; risk appeared different among subjects by paternal history; however, numbers were very small, and the interaction was not statistically significant (Table 4).
The distribution of medication intake among asthmatic children is reported in Table 5. Intake of antiasthma medications such as inhaled corticosteroids and beta agonists was associated with non-statistically significant, increased ORs for CNS (OR for steroids, 2.55; CI 95%, 0.79–8.20 and OR for inhaled beta agonist, 1.62; CI 95%, 0.57–4.63) (Table 5).
Discussion
In our study, the risk of developing a brain cancer in children was inversely associated with a diagnosis of asthma, and the protective association seemed driven mainly by the ependymoma group despite the small numbers in this group of tumors. Adjusting for maternal smoking during the last month of pregnancy, vitamin supplementation and prenatal as well as infection of child at birth seemed to increase the protective role of asthma. In the subgroup of children with asthma but without eczema, asthma had a protective role, but the effect of both asthma and eczema together was not more protective than that for asthma alone. No evidence of risk modification was detected for maternal, paternal or sibling’ history of asthma, but numbers were too small to carry out a robust analysis. Finally, taking asthma medications, especially inhaled corticosteroids, seemed to increase the risk, but the confidence intervals were large and included the null value.
The role of asthma in developing brain tumor is not clear yet, but some hypotheses have been suggested, especially for adults. The strongest one is based on increased tumor immunosurveillance [24, 25]: The hypersensitive immune system of people affected with asthma and atopy would eliminate abnormal cells before they undergo malignant transformation, playing an important role in tumor prevention. This observation is strengthened by the presence of higher IgE levels among controls compared to glioma patients [26] and by the finding that allergy-associated genetic variants in IL13 and IL4R are inversely related to glioblastoma [27]. Both the studies of Wiemels et al. and Schwatzbaum et al. also argue for a possible reverse causality effect, whereby IgE levels and allergic reactions reported by patients might be influenced by factors secreted by subclinical cancer [17]. However, because an inverse association of asthma/atopy with brain tumors was also observed in several studies when allergies developed at an early age, or when they were present many years before cancer diagnosis [11–13, 28], reverse causation remains an unlikely explanation [29].
To our knowledge, only one previous epidemiologic study [18] has examined the risk of developing brain tumors related to the presence of asthma in children; it reported an association with atopy. Our results regarding asthma are consistent with these findings although our results with eczema cannot eliminate chance as an explanation. A limitation in our study was that the collection of data on eczema was as a secondary open question (other diseases and conditions) as opposed to the asthma information, which was explicit. Therefore, there was a relatively small number of children reporting eczema. Our findings are in keeping also with the published literature on brain tumors in adults [11–15, 28], which has repeatedly shown an inverse relation between asthma and brain cancer.
To our knowledge, this is the first study to take family history of asthma into account. Harding et al. [18] found no evidence to suggest an association between parental history of asthma and CNS tumors in children, but they did not distinguish between maternal and paternal history. Considering that parental history of asthma is one of the major determinants of childhood asthma [30, 31], we investigated the association with asthma stratifying by family history. We found no statistically significant heterogeneity, but the sample sizes were small.
To our knowledge, no study has analyzed the association between brain cancer and asthma medication neither in adults nor in children. The main drugs used for asthma are relievers (short-acting β2 agonist) or controllers (inhaled or oral glucocorticosteroids). Relievers are generally used on demand, when a child becomes more symptomatic, and hence, it is more difficult to evaluate the actual extent of drug use, while inhaled glucocorticosteroids are used daily to keep the asthma symptoms controlled and to prevent the attacks [32]. The use of and the compliance for inhaled glucocorticosteroids are hence easier to evaluate and likely reported with more precision than for the β2 agonist. In our study, use of these medications, especially inhaled corticosteroids, was associated with a non-statistically significant increased risk, but the number of asthmatic children using drugs is small for both medications. The anti-inflammatory and immunosuppressive role of steroids is well known [33]; even when inhaled, corticosteroids have several systemic effects [34] and could play a role in the immune system over-stimulated by asthma, invalidating the finding of the protective role for asthma. A few studies examined the role of medication in the development of brain cancer, but never in children. Wigertz et al. [15] found an inverse association between glioma and use of eye drops and nasal spray in adult subjects with allergy; the same result was found by Shoemaker et al. [13] for glioma and nasal spray, but neither of these reports mention the active pharmaceutical ingredient.
Previous studies reported vitamin intake, including folic acid, as potential risk factors for childhood brain cancer in particular PNET [9, 21, 22]. The role of folate in the protection against neural tube defect is well known, and lack of folic acid intake could determine some common mechanism of altered development leading to both neural tube defects and PNET in particular [22, 23].
There are some limitations to our study: the first is the risk of misclassification when reporting a diagnosis of asthma. The diagnosis of asthma obtained by questionnaire could be slightly different from that based on other methods [35]. However, there is a copious literature showing the validity of self-reporting asthma when the gold standard is clinical evaluation. On the other hand, the severity of asthma could bias the reporting [36–39]. The fact that some children were reported as taking asthma medication but not as having asthma could suggest over reporting of medication use or the use of these medications for other related diagnoses [40].
The prevalence of asthma in our control population (16.2%) was slightly higher than that found in 1994 and in 1999 in Canada in a population of children 0–11 years old (11.1% in 1994; 12.9% in 1999) [32], but lower than the prevalence reported by Asher et al. [41] in United States (22.3% in 1992 and 22.9% in 2003). The prevalence of asthma, in fact, varies with age and calendar period [41], and the period spanning this study is, in fact, from 1970 to 1999 where fluctuations have been reported in asthma prevalence in Canada [32, 42]. A second limitation is that eczema was a secondary item in the questionnaire and was not investigated in-depth; this could have resulted in some misclassification.
In conclusion, there were some indications of decreased risk of childhood brain tumors with asthma exposure. The role of asthma medication needs to be further investigated because it could play an important role in the asthma–brain tumor association in children.
References
Anonymous (2003) Diagnosis and initial treatment of cancer in Canadian children 0 to 14 years, 1995–2000. Health, Canada, Ottawa
McKinney P (2005) Central nervous system tumours in children: epidemiology and risk factors. Bioelectromagnetics Suppl 7:S60–S68
Linet M, Wacholder S, Zahm S (2003) Interpreting epidemiologic research: lessons from studies of childhood cancer. Pediatrics 112(1 Pt 2):218–232
Filippini G, Maisonneuve P, McCredie M, Peris-Bonet R, Modan B, Preston-Martin S, Mueller B, Holly E, Cordier S, Choi N, Little J, Arslan A, Boyle P (2002) Relation of childhood brain tumors to exposure of parents and children to tobacco smoke: the search international case-control study. Int J Cancer 100(2):206–213
Fear N, Roman E, Ansell P, Bull D (2001) Malignant neoplasms of the brain during childhood: the role of prenatal and neonatal factors (United Kingdom). Cancer Causes Control 12(5):443–449
Shaw A, Li P, Infante-Rivard C (2006) Early infection and risk of childhood brain tumors (Canada). Cancer Causes Control 17(10):1267–1274
Huncharek M, Kupelnick B, Klassen H (2002) Maternal smoking during pregnancy and the risk of childhood brain tumors: a meta-analysis of 6566 subjects from twelve epidemiological studies. J Neurooncol 57(1):51–57
Pogoda J, Preston-Martin S, Howe G, Lubin F, Mueller B, Holly E, Filippini G, Peris-Bonet R, McCredie M, Cordier S, Choi W (2009) An international case-control study of maternal diet during pregnancy and childhood brain tumor risk: a histology-specific analysis by food group. Ann Epidemiol 19(3):148–160
Preston-Martin S, Pogoda J, Mueller B, Lubin F, Modan B, Holly E, Filippini G, Cordier S, Peris-Bonet R, Won C, Little J, Arslan A (1998) Results from an international case-control study of childhood brain tumors: the role of prenatal vitamin supplementation. Environ Health Perspect 106:887–892
Stalberg K, Haglund B, Stromberg B, Kieler H (2010) Prenatal exposure to medicines and the risk of childhood brain tumor. Cancer Epidemiol 34(4):400–404
Schlehofer B, Blettner M, Preston-Martin S, Niehoff D, Wahrendorf J, Arslan A, Ahlbom A, Choi W, Giles G, Howe G, Little J, Ménégoz F, Ryan P (1999) Role of medical history in brain tumour development. Results from the international adult brain tumour study. Int J Cancer 82(2):155–160
Brenner A, Linet M, Fine H, Shapiro W, Selker R, Black P, Inskip P (2002) History of allergies and autoimmune diseases and risk of brain tumors in adults. Int J Cancer 99(2):252–259
Schoemaker M, Swerdlow A, Hepworth S, McKinney P, van Tongeren M, Muir K (2006) History of allergies and risk of glioma in adults. Int J Cancer 119(9):2165–2172
Berg-Beckhoff G, Schüz J, Blettner M, Münster E, Schlaefer K, Wahrendorf J, Schlehofer B (2009) History of allergic disease and epilepsy and risk of glioma and meningioma (INTERPHONE study group, Germany). Eur J Epidemiol 24(8):433–440
Wigertz A, Lonn S, Schwartzbaum J, Hall P, Auvinen A, Christensen H, Johansen C, Klaeboe L, Salminen T, Schoemaker M, Swerdlow A, Tynes T, Feychting M (2007) Allergic conditions and brain tumor risk. Am J Epidemiol 166(8):941–950
Bondy M, Scheurer M, Malmer B, Barnholtz-Sloan J, Davis F, Il’yasova D, Kruchko C, McCarthy B, Rajaraman P, Schwartzbaum J, Sadetzki S, Schlehofer B, Tihan T, Wiemels J, Wrensch M, Buffler P (2008) Brain tumor epidemiology: consensus from the Brain Tumor Epidemiology Consortium. Cancer 113(S7):1953–1968
Dix A, Brooks W, Roszman T, Morford L (1999) Immune defects observed in patients with primary malignant brain tumors. J Neuroimmunol 100(1–2):216–232
Harding N, Birch J, Hepworth S, McKinney P (2008) Atopic dysfunction and risk of central nervous system tumours in children. Eur J Cancer 44(1):92–99
Kramarova E, Stiller CA, Ferlay J, Parkin DM (1996) International classification of childhood cancer. IARC technical report. IARC, Lyon
Brooks DR, Mucci LA, Hatch EE, Cnattingius S (2004) Maternal smoking during pregnancy and risk of brain tumors in the offspring. A prospective study of 1.4 million Swedish births. Cancer Causes Control 15(10):997–1005
Bunin G, Kuijten R, Buckley J, Rorke L, Meadows A (1993) Relation between maternal diet and subsequent primitive neuroectodermal brain tumors in young children. N Engl J Med 329(8):536–541
Schuz J, Weihkopf T, Kaatsch P (2007) Medication use during pregnancy and the risk of childhood cancer in the offspring. Eur J Pediatr 166(5):433–441
Gurney J, Smith M, Olshan A, Hecht S, Kasum C (2001) Clues to the etiology of childhood brain cancer: N-nitroso compounds, polyomaviruses, and other factors of interest. Cancer Invest 19(6):630–640
Burnet M (1957) Cancer: a biological approach. III. Viruses associated with neoplastic conditions. IV. Practical applications. Br Med J 1(5023):841–847
Dunn G, Bruce A, Ikeda H, Old L, Schreiber R (2002) Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol 3(11):991–998
Wiemels J, Wiencke J, Patoka J, Moghadassi M, Chew T, McMillan A, Miike R, Barger G, Wrensch M (2004) Reduced immunoglobulin E and allergy among adults with glioma compared with controls. Cancer Res 64(22):8468–8473
Schwartzbaum J, Ahlbom A, Malmer B, Lönn S, Brookes A, Doss H, Debinski W, Henriksson R, Feychting M (2005) Polymorphisms associated with asthma are inversely related to glioblastoma multiforme. Cancer Res 65(14):6459–6465
Wiemels J, Wiencke J, Sison J, Miike R, McMillan A, Wrensch M (2002) History of allergies among adults with glioma and controls. Int J Cancer 98(4):609–615
Linos E, Raine T, Alonso A, Michaud D (2007) Atopy and risk of brain tumors: a meta-analysis. J Natl Cancer Inst 99(20):1544–1550
Castro-Rodriguez J (2010) The asthma predictive index: a very useful tool for predicting asthma in young children. J Allergy Clin Immunol 126(2):212–216
Burke W, Fesinmeyer M, Reed K, Hampson L, Carlsten C (2003) Family history as a predictor of asthma risk. Am J Prev Med 24(2):160–169
Garner R, Cohen D (2008) Changes in the prevalence of asthma among Canadian children. Health Rep 19(2):45–50
Wilckens T, De Rijk R (1997) Glucocorticoids and immune function: unknown dimensions and new frontiers. Immunol Today 18(9):418–424
Lipworth B (1999) Systemic adverse effects of inhaled corticosteroid therapy: a systematic review and meta-analysis. Arch Intern Med 159(9):941–955
Pekkanen J, Pearce N (1999) Defining asthma in epidemiological studies. Eur Resp J 14(4):951–957
Toren K, Brisman J, Jarvholm B (1993) Asthma and asthma-like symptoms in adults assessed by questionnaires—a literature review. Chest 104(2):600–608
Toren K, Palmqvist M, Lowhagen O, Balder B, Tunsater A (2006) Self-reported asthma was biased in relation to disease severity while reported year of asthma onset was accurate. J Clin Epidemiol 59(1):90–93
Remes ST, Pekkanen J, Remes K, Salonen RO, Korppi M (2002) In search of childhood asthma: questionnaire, tests of bronchial hyperresponsiveness, and clinical evaluation. Thorax 57(2):120–126
De Marco R, Cerveri I, Bugiani M, Ferrari M, Verlato G (1998) An undetected burden of asthma in Italy: the relationship between clinical and epidemiological diagnosis of asthma. Eur Resp J 11(3):599–605
Zuidgeest MG, van Dijk L, Smit HA, van der Wouden JC, Brunekreef B, Leufkens HG, Bracke M (2008) Prescription of respiratory medication without an asthma diagnosis in children: a population based study. BMC Health Serv Res 8:16
Asher M, Montefort S, Bjorksten B, Lai C, Strachan D, Weiland S, Williams H (2006) Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 368(9537):733–743
Millar W, Hill G (1998) Childhood asthma. Health Rep Winter 10(3):9–21
Acknowledgments
The project was supported in part by The Brain Tumor Foundation of Canada. The authors wish to thank M. Alexandre Cusson for programming assistance. FR is a postdoctoral fellow in the Department of Epidemiology, Biostatistics and Occupational Health, McGill University and was supported by the Associazione Italiana lotta contro le Leucemie, Linfomi e Mielomi, sede Torino. CIR is a James McGill Professorship (Canada Research Chair).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roncarolo, F., Infante-Rivard, C. Asthma and risk of brain cancer in children. Cancer Causes Control 23, 617–623 (2012). https://doi.org/10.1007/s10552-012-9928-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-012-9928-7