Abstract
The young age at onset of many cancers in childhood has led to investigations on maternal exposures during pregnancy. Data from a population-based case-control study in Germany (1992–1997) that included 1,867 cases and 2,057 controls was used to investigate this question. Maternal use of vitamin, folate or iron supplementation was associated with a reduced risk of non-Hodgkin lymphoma and tumors and, less clearly, with leukemia, but not with CNS tumors. An increased risk of neuroblastoma was associated most markedly with diuretics and other antihypertensives, but also with vitamin, folate or iron supplementation. No associations were seen with pain relievers, antinauseants or cold medications, nor with delivery by Caesarian section. The strengths of this study are its population base, the large number of cases and the inclusion of different case groups to identify disease specificity of associations. The limitation of this study is an exposure assessment relying on maternal self-reports. In conclusion, these data indicate a potential influence of some maternal medication during pregnancy on the risk of childhood cancer in the offspring; however, no clear picture is seen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is growing evidence that various types of childhood cancers are initiated already in utero [1, 17, 21]. It is biologically plausible that mutations in utero contribute particularly to the development of cancers in infancy, due to the young age of onset for the disease [34]. More recently, with the use of direct molecular tests, it has been shown that many cases of the most common type of childhood cancer, acute lymphoblastic leukemia (ALL), are also initiated in utero [10, 12, 13, 20, 49]. This emphasizes the importance of maternal exposures during pregnancy and their possible role in the etiology of childhood cancer. Maternal medication use during pregnancy is linked to such exposures because drugs may cross the placenta and, potentially, damage the fetus [46]. Congenital malformations are one adverse pregnancy outcome that was demonstrated to be associated with maternal medication use [15]. There are a number of epidemiological studies in which an association between maternal medication use during pregnancy and the risk of childhood cancer has been investigated; however, no clear picture has emerged so far [21]. Among those associations that show some degree of consistency are the relation between maternal use of diuretics and an increased risk of neuroblastoma [18, 39], and a risk reduction for leukemia and CNS tumors with maternal use of folate [6, 28, 29, 44, 48].
During the years 1992 to 1997, a large-scale case-control study on causes of childhood cancer was conducted in Germany, including cases with acute leukemia, non-Hodgkin lymphoma (NHL), CNS tumor, neuroblastoma, Wilms' tumor, bone tumor and soft tissue sarcoma [36]. Questions on maternal drug use were part of the original questionnaire; however, due to the huge amount of information from a total of 1,867 cases and 2,057 controls, this information was not coded and evaluated before now. This is a report of the analyses addressing maternal medication use during pregnancy and the risk of various childhood cancers in the offspring.
Materials and methods
Cases were ascertained from the nationwide German Childhood Cancer Registry (GCCR) at the University of Mainz, which is estimated to be more than 95% complete [11]. Patients aged 14 years or less were eligible if their disease was diagnosed between October 1992 and September 1994, and if the child lived in West Germany at the date of diagnosis. For each case, one control matched by gender, date of birth within at most 1 year and community was selected from the complete files of the local resident registration offices. More details are described elsewhere [36].
Information on potential risk factors was collected by both a self-administered questionnaire and a subsequent telephone interview with both parents. The questions were based on a structured questionnaire developed by the US Children’s Cancer Group [31]. Questionnaires were mailed by the physician responsible for the cancer treatment (cases) or by the study center at the GCCR (controls) and were returned to the study center. The questions on maternal medication use were on the postal questionnaire. A list of medication groups was offered to the mother with three check-boxes per group, representing “yes”, “no” or “unknown”. The listed medication groups included vitamin, folate or iron supplements; antinauseants or antiemetics; diuretics or other antihypertensives; tranquillizers or sleeping pills; pain relievers; cold medications; psychotropics; antiepileptics; and diet pills. In addition to that, each medication group was followed by an open text field to specify the brand names of the respective drugs. All brand names were coded according the “Rote Liste,” a German dictionary of medications, to check the classifications from the questionnaire and to obtain data on specific substances. No information was available on which trimesters the medication was taken. We also asked the mother about episodes of high blood pressure or edema during pregnancy and whether the index child’s delivery was by Caesarean section. Questions concerning the socioeconomic status of a family were based on parental education, on parental occupational training and on the average monthly family net income, and were all part of the telephone interview.
Statistical methods
Odds ratios (OR) and 95 percent confidence intervals (CI) were computed by conditional logistic regression analysis for matched pairs [43]. To achieve a greater statistical power to detect any association, all analyses were repeated using a post-hoc frequency-matched regression model [4, 24], involving all available cases and controls, irrespective of whether they had a matched partner or not. This model always included the total set of controls. The frequency-matched logistic regression model was stratified by gender, age (groups of 1 year) and year of birth, and additionally adjusted for the degree of urbanization (urban, rural, mixed urban-rural) to compensate for breaking the individual matching. Both conditional logistic regression analyses and frequency-matched conditional logistic analyses were adjusted for socioeconomic status (high; average). In this paper, the results from the frequency-matched analyses are presented by default. Risk estimates from the 1:1-matched model are presented only if there were major differences compared to the frequency-matched approach. We did not apply statistical procedures to adjust for multiple testing, but discuss our findings in respect to their consistency with other studies on this topic, as the adjustment would have substantially decreased the statistical power of our study to detect any association.
Results
The overall response rates were 82.6% among cases and 70.9% among controls (Table 1). The participation rates (the number of families who returned the questionnaire divided by the number of families who were contacted) among control families were lower than among case families (70.9% vs. 84.8%); however, there were only minor differences across the diagnostic groups, with participation rates ranging from 82.3% (bone tumors) to 85.5% (CNS tumors). The overwhelming reason for non-participation was parental refusal. Among families of eligible cases, only 2.6% were not contacted, mainly because of physician preference.
There was a general tendency that control families were more likely to have a higher socioeconomic status (SES) than case families (Table 2). All demographic characteristics were considered as potential confounders and adjusted for in all subsequent analyses.
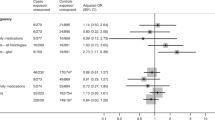
Table 3 displays the most frequent medication groups used by the mother during pregnancy and their associations with the risk of childhood cancer in the offspring. Vitamin, folate and/or iron supplements were associated with reduced risks of ALL, NHL and Wilms' tumor and an increased risk of neuroblastoma. In the individually matched analysis, however, the association with ALL moved towards null (OR 0.96, 95 percent CI: 0.75, 1.22).
Maternal use of diuretics and other antihypertensives during pregnancy was associated with increased risks of ALL and of neuroblastoma. Again, the association with ALL was less apparent from the individually matched approach (OR 1.14, 95 percent CI: 0.50, 2.60). Regarding the risk of CNS tumors, the odds ratios varied with the type of brain tumor: The slight increase in the overall risk of CNS tumors was completely attributable to primitive neuroectodermal tumors (PNET) (OR 4.14, 95 percent CI: 1.30, 13.2), while no mothers of patients with ependymoma or astrocytoma had taken antihypertensives. It has to be noted that the risk increases for neuroblastoma observed with antihypertensives were seen for both low-stage as well as high-stage neuroblastomas.
No associations with any kind of childhood cancer were seen for maternal use of pain relievers, antinauseants or antiemetics, and cold medications.
More mothers of patients than controls reported episodes of high blood pressure or edema during pregnancy. However, the majority of mothers received no treatment for these syndromes. Table 4 presents the childhood cancer risks associated with maternal high blood pressure or edema during pregnancy, divided into groups of mothers who received no treatment and mothers who have reported an intake of antihypertensives such as diuretics. The latter group was associated only with an increased neuroblastoma risk, which was more pronounced for low-stage neuroblastoma (OR 3.44, 95 percent CI: 1.04, 11.44) compared to high-stage (OR 1.54, 95 percent CI: 0.52, 4.51).
Only very few mothers received antiepileptics, psychotropics or diet pills (not presented in the tables). The prevalence among control mothers was 0.1 percent, 0.3 percent and 0.8 percent, respectively. Thus, the risk estimates based on small numbers of subjects were very imprecise and revealed no associations with any risk of childhood cancer. None of the 392 mothers of a child with a CNS tumor reported the use of antiepileptics during pregnancy.
Only 1.3 percent of control mothers reported the use of tranquillizers or sleeping pills. Mothers of patients reported the use of tranquillizers or sleeping pills more often (almost 3 percent), but the higher prevalence compared to controls was entirely attributable to the use of homeopathic sleeping pills (of which some have no pharmacological effect, according to conventional medicine). This kind of medication was virtually never reported by control mothers, so we suggest that the difference between case and control mothers was likely to be attributable to a different understanding of the respective question, due to the way it was phrased in the German original.
The low prevalences of most medications precludes age-specific analyses for most diagnoses. For ALL and maternal exposure to vitamin, folate and/or iron supplements, we found a stronger protective effect in older children (age 5 years or more) than in younger children, with an odds ratio of 0.67 (95 percent CI: 0.50, 0.90) compared to 0.98 (95 percent CI: 0.76, 1.25). This, however, was not a general tendency across all diagnoses for this exposure, as for all solid tumors combined the odds ratio for older children was 0.95 and hereby similar to that for younger children (1.01).
Finally, there was no association between the risk of childhood cancer and delivery of the index child by Caesarean section (Table 5).
Discussion
One strength of the German study is its population base. Cases were ascertained from a complete nationwide cancer registry, covering a population of some 13 million children in the age range 0 to 14 years [11]. Controls were randomly selected from the study base from which the cases arose. As population registration is compulsory in Germany, these registries offer an optimal sampling frame for population-based controls.
The major limitation of this study was that maternal medication use was solely based on self-reported information, raising concern about recall bias [38]. Although all interviews were performed within 3 years after diagnosis, it was still challenging for the mother to recall periods of medication use and, in particular, brand names of medications used during pregnancy. Especially for mothers of older children this was more than a decade ago (with a maximum of 17 years). As about half of the control mothers ticked the main medication group, but provided no more details on brands, it was not possible to go beyond the main medication group in the analysis. This is a particular limitation for vitamins, folate and iron supplementation as well as the group of antihypertensives, for which other studies (that will be discussed later) provided more specific associations, which hampers a direct comparison of results. In addition to that, we had no further information on the amount of use or the timing of exposure. If effects are only related to an intake of medication during the first trimester of pregnancy or only above a certain threshold, associations may have been diluted in our study. However, the inclusion of several case groups allowed the investigation of disease specificity of the observed associations. Similar effects for heterogeneous case groups may be an indicator for some general recall bias, while disease-specific results may argue against it.
An ambiguous finding of this study is the reduced ALL risk in children whose mothers reported a vitamin, folate or iron supplementation during pregnancy. On the one hand, our findings confirm two recent studies. One was an Australian study that found a strong risk reduction [44] (but based on a small number of subjects), while the other was a large US study (n=1,800 children) that found a modest, but significant 20% reduction in risk [48]. On the other hand, the protective association disappeared in the current study when leukemia cases were compared with their original matched controls only. No protection at all, however, was also seen in a recent Canadian study [40]. Shu et al. found no association comparing two case groups of childhood ALL with different ras mutations [41]. Beneficial effects with regard to the prevention of cancer are under discussion for all three substances. A well-known benefit of folate supplementation is in the prevention of congenital malformations, particularly neural tube defects [2]. The role of folate in cancer risk is supposed to be due to impaired DNA synthesis and repair as a result of folate deficiency [16]. Through their role as antioxidants, vitamins have been found to reduce the risk of various cancers in adults [47]. A recent study in California showed a strong protective association against ALL with a maternal diet rich in vitamins during the index pregnancy, but it was the first study to report this and relied on self-reports on maternal diet [14]. Iron supplementation during pregnancy is used to prevent anemia, and studies in the UK and in Greece have showed a higher leukemia risk in children whose mothers were anemic during pregnancy [27, 32]. In a second larger UK study, this risk, however, was only confirmed for AML, but not ALL [33]. A reduced risk in our study was also seen for NHL and for Wilms' tumor, but not CNS tumors. For CNS tumors this is not consistent with previous studies as several studies have shown reduced risks with maternal vitamin use during pregnancy [35]. The strength of the association, however, was always largest in US studies, and most pronounced in mothers who also had a high intake of cured meats, so it may well be that differences in the diet between the US and Germany explains the different findings. In contrast to the various protective effects, vitamin, folate or iron supplementation leads to a higher risk of neuroblastoma. This is the opposite finding compared to two large US studies in which strong protective associations of maternal vitamin use have been observed (30–70% risk reduction) [22, 26]. Flavonoids (formerly known as vitamin P) are known as topoisomerase II inhibitors, and it has been hypothesized that the maternal intake of flavonoids during pregnancy is associated with an increased risk of leukemia in the offspring [21]. However, for flavonoids, no specific galenic is available in Germany, and, hence, we were not able to address this question.
A common concern in all of these case-control studies is a higher participation rate among more affluent families [19]. In the current study, the prevalence of vitamin, folate or iron supplementation in mothers with the highest educational level was some 15 percent higher than among mothers of the lowest educational level, suggesting a possible overestimation of the protective effect of this supplementation due to selection bias (Fig. 1). Another concern is that the prevalence of use in the current study is lower than the average prevalence of 90% (range 21–100%) reported by Bonati et al. [3], who presented an overview of epidemiological studies in 1990.
Maternal use of antihypertensives during pregnancy was associated with a three-fold increased risk of neuroblastoma in the current study. This observation was strengthened by another finding, namely that among the various case groups only mothers of children with neuroblastoma reported a treatment of pregnancy-related high blood pressure or edema more frequently than controls. Two earlier small studies found strong associations between diuretics and neuroblastoma risk [18, 39]; however, this was not confirmed by both another small study from Germany [23] and a large study from the US [8]. In the latter study, among 504 matched case-control pairs, only three case mothers and none of the control mothers had reported the use of diuretics during pregnancy. Thus, it is rather surprising that in all the smaller studies (with about 100 cases) the numbers of exposed were higher. A possible mechanism for the association between diuretics and antihypertensives might be the toxic presence of n-nitroso precursors. N-nitroso is a strong transplancental nervous system carcinogen [25, 39] and is known to be an ingredient in some diuretics, e.g., furosemide and hydrochlorothiazid and also antihypertensives such as propanolol [7]. It might also be that, in case of a cancer of the fetus, catecholamine production might be responsible for maternal hypertension followed by the accordant medication [39]. However, hydrochlorothiazide is contradicted during pregnancy, and furosemide has been given mainly in case of emergency. The first-choice antihypertensive drug is α-methyldopa, and cardioselective betablockers are only the second choice.
The prevalence of hypertension during pregnancy in both German and US studies has been reported to be between 5 and 7% [30], and the prevalence of preeclampsia between 6 and 8%, respectively [9, 42]. Although the role of diuretics in the treatment of hypertension is inferior during pregnancy, there is a broad spectrum of established drugs like α-methydopa, beta-blockers, calcium-channel blockers and others [51]. Taking all this into account, the intake of antihypertensive drugs might have been underestimated in our study, while the intake of diuretics was overestimated. However, we were not able to subdivide the two medication groups in the analysis.
In all, there is some evidence that most associations between any maternal medication and a risk of childhood cancer in the offspring are attributable to neuroblastoma [21]. It is noticeable within this context that the neuroblastoma cases represent the youngest case group, which may strengthen the biological plausibility and may also be related to a more precise recall as the time period between pregnancy and the interview was the shortest [37]. It is reassuring that the comparison of neuroblastoma cases only with its original individually matched controls resulted in the same estimated odds ratios as those derived from the main analytical model.
The results for diuretics and antihypertensives and childhood ALL were somewhat ambiguous. Firstly, the type of the analysis had an impact on the results. Secondly, no association was seen between ALL risk and maternal high blood pressure or edema during pregnancy, indicating that most of the case mothers gave no reason for the use of diuretics. No evidence of an association between diuretics and ALL risk appeared in previous studies [21].
For pain relievers, antinauseants and cold medications, all odds ratios were close to unity. While these data suggest that there are at least no strong associations, it was not possible to confirm findings from studies with more specific data as in the neuroblastoma study showing an association between codeine and tumor risk [8]. The prevalence of pain reliever use during pregnancy in the current study was lower than the average presented in a review [3].
No associations were observed between delivery by Caesarean section and the risk of various childhood cancers. As a Caesarean section is related to the use of narcotics during labor, it may represent another aspect of medication use during pregnancy. One study on childhood brain tumors found an elevated odds ratio of 1.8 for astrocytoma [5], but this was not confirmed in the current study. However, the odds ratio for neuroblastoma was slightly elevated (odds ratio of 1.36), corresponding to a small risk excess observed in the largest neuroblastoma study to date (odds ratio 1.4, 95 percent CI: 1.0, 1.9) [7].
It has to be taken into account that the different tumor groups are heterogenous in pathogenesis and biology. However, additional subdivision of the groups would result in very small numbers.
In conclusion, this study only weakly supports the hypothesis that maternal use of vitamin, folate or iron supplementation during pregnancy is associated with a reduced risk of childhood ALL in the offspring. A stronger risk reduction, albeit not reported in previous studies [21], was seen for NHL and Wilms' tumor. A risk increase of neuroblastoma was associated with several maternal medications during pregnancy. The validity of the exposure assessment, however, remains somewhat uncertain. A large-scale ongoing study in the UK with access to medical records will hopefully provide more insight, including into the agreement between self-reported data and the practitioners’ notes, but also no objective data will be available on the use of over-the-counter medications [45]. The establishment of medication prescription registries in some of the Nordic countries (Denmark and Finland) will be a very valuable basis for future research in this area [50].
Abbreviations
- ALL:
-
acute lymphoblastic leukemia
- AML:
-
acute myeloblastic leukemia
- CNS:
-
central nervous system
- NHL:
-
non-Hodgkin lymphoma
- OR:
-
odds ratio
- CI:
-
confidence interval
- SES:
-
socioeconomic status
References
Anderson LM, Diwan BA, Fear NT, Roman E (2000) Critical windows of exposure for children's health: cancer in human epidemiological studies and neoplasms in experimental animal models. Environ Health Perspect 108:573–594
Berry RJ, Li Z, Erickson JD, Li S, Moore CA, Wang H, Munlinare J, Zhao P, Wong LY, Gindler J, Hong SX, Correa A (1999) Prevention of neural-tube defects with folic acid in China. China-U.S. Collaborative Project for Neural Tube Defect Prevention. N Engl J Med 341:1485–1490
Bonati M, Bortelus R, Marchetti F, Romero M, Rognoni G (1990) Drug use in pregnancy: an overview of epidemiological (drug utilization) studies. Eur J Clin Pharmacol 38:325–328
Brookmeyer R, Liang KY, Linet M (1986) Matched case-control designs and overmatched analyses. Am J Epidemiol 124:693–701
Bunin GR, Kuijten RR, Buckley JD, Rorke LB, Meadows AT (1993) Relation between maternal diet and subsequent primitive neuroectodermal brain tumors in young children. N Engl J Med 329:536–541
Bunin GR, Buckley JD, Boesel CP, Rorke LB, Meadows AT (1994) Risk factors for astrocytic glioma and primitive neuroectodermal tumor of the brain in young children: a report from the Children's Cancer Group. Cancer Epidemiol Biomarkers Prev 3:197–204
Carozza SE, Olshan AF, Faustman EM, Gula MJ, Kolonel LN, Austin DF, West ED, Weiss NS, Swanson GM, Lyon LK, Hedley-Whyte T, Gilles FH, Aschenbrenner C, Leviton A (1995) Maternal exposure to N-nitrosatable drugs as a risk factor for childhood brain tumours. Int J Epidemiol 24:308–312
Cook MN, Olshan AF, Guess HA, Savitz DA, Poole C, Blatt J, Bondy ML, Pollock BH (2004) Maternal medication use and neuroblastoma in offspring. Am J Epidemiol 159:721–731
Feuring M, Melchert F, Wehling M (1999) Pharmacotherapy for hypertonia in pregnancy. Gynäkologe 32:443–449
Gale KB, Ford AM, Repp R, Borkhardt A, Keller C, Eden OB (1997) Backtracking leukemia to birth: identification of clonotypic gene fusion sequences in neonatal blood spots. Proc Natl Acad Sci USA 94:13950–13954
German Childhood Cancer Registry: Annual Report 2004 (1980–2003) Technical report, Institute of Medical Biostatistics, Epidemiology and Informatics, 2005 (http://www.kinderkrebsregister.de)
Greaves MF (2002) Childhood leukaemia. BMJ 324:283–287
Hjalgrim LL, Madsen HO, Melbye M, Jorgensen P, Christiansen M, Andersen P, Pallisgaat N, Hokland P, Clausen N, Ryder LP, Schmiegelow K, Hjalgrim H (2002) Presence of clone-specific markers at birth in children with acute lymphoblastic leukaemia. Br J Cancer 87:994–999
Jensen CD, Block G, Buffler P, Ma X, Selvin S, Month S (2004) Maternal dietary risk factors in childhood acute lymphoblastic leukemia (United States). Cancer Causes Control 15:559–570
Khera KS (1987) Maternal toxicity of drugs and metabolic disorders-a possible etiologic factor in the intrauterine death and congenital malformation: a critique on human data. Crit Rev Toxicol 17:345–375
Kim YI (1999) Folate and carcinogenesis: evidence, mechanisms, and implications. J Nutr Biochem 10:66–68
Knudson AG Jr (1971) Mutation and cancer: statistical study of retinoblastoma. Proc Natl Acad Sci USA 68:820–823
Kramer S, Ward E, Meadows AT, Malone KE (1987) Medical and drug risk factors associated with neuroblastoma: a case-control study. J Natl Cancer Inst 78:797–804
Law GR, Smith AG, Roman E; United Kingdom Childhood Cancer Study Investigators (2002) The importance of full participation: lessons from a national case-control study. Br J Cancer 86:350–355
Lightfoot TJ, Roman E (2004) Causes of childhood leukaemia and lymphoma. Toxicol Appl Pharmacol 199:104–117
Little J (1999) Epidemiology of childhood cancer. IARC Scientific Publications No 149. Lyon, France
Michalek AM, Buck GM, Nasca PC, Freedman AN, Baptiste MS, Mahoney MC (1996) Gravid health status, medication use, and risk of neuroblastoma. Am J Epidemiol 143:996–1001
Michaelis J, Haaf HG, Zöllner J, Kaatsch P, Krummenauer F, Berthold F (1996) Case-control study of neuroblastoma in West Germany after the Chernobyl accident. Klin Padiatr 208:172–178
Neuhäuser M, Becher H (1997) Improved odds ratio estimation by post hoc stratification of case-control data. Stat Med 16:993–1004
Olshan AF, Faustman EM (1989) Nitrosable drug exposure during pregnancy and adverse outcome. Int J Epidemiol 18:891–899
Olshan AF, Smith JC, Bondy ML, Neglia JP, Pollock BH (2002) Maternal vitamin use and reduced risk of neuroblastoma. Epidemiology 13:575–580
Petridou E, Trichopoulos D, Kalapothaki V, Pourtsidis A, Kogevinas M, Kalmanti M, Kouliouskas D, Kosmidis H, Panagiotou JP, Piperopoulou F, Tzortzatou F (1997) The risk profile of childhood leukaemia in Greece: a nationwide case-control study. Br J Cancer 76:1241–1247
Preston-Martin S, Pogoda JM, Mueller BA, Holly EA, Lijinsky W, Davis RL (1996) Maternal consumption of cured meats and vitamins in relation to pediatric brain tumors. Cancer Epidemiol Biomarkers Prev 5:599–605
Preston-Martin S, Pogoda JM, Mueller BA, Lubin F, Modan B, Holly EA, Fillippini G, Cordier S, Peris-Bonet R, Choi W, Little J, Arslan A (1998) Results from an international case-control study of childhood brain tumors: the role of prenatal vitamin supplementation. Environ Health Perspect 106:887–892
Rath W (1999) Hypertensive diseases in pregnancy. Gynäkologe 32:432–442
Robison LL, Buckley JD, Bunin G (1995) Assessment of environmental and genetic factors in the biology of childhood cancers: the Children‘s Cancer Group epidemiology program. Environ Health Perspect 6:111–116
Roman E, Ansell P, Bull D (1997) Leukaemia and non-Hodgkin’s lymphoma in children and young adults: are prenatal and neonatal factors important determinants of disease? Br J Cancer 76:406–415
Roman E, Simpson J, Ansell P, Lightfoot T, Mitchell C, Eden TO (2005) Perinatal and reproductive factors: a report on haematological malignancies from the UKCCS. Eur J Cancer 41:749–759
Ross JA, Swensen AR (2000) Prenatal epidemiology of pediatric tumors. Curr Oncol Rep 2:234–241
Schüz J, Kaatsch P (2002) Epidemiology of pediatric tumors of the central nervous system. Exp Rev Neurotherapeutics 2:469–480
Schüz J, Kaatsch P, Kaletsch U, Meinert R, Michaelis J (1999) Association of childhood cancer with factors related to pregnancy and birth. Int J Epidemiol 28:631–639
Schüz J, Kaletsch U, Meinert R, Kaatsch P, Spix C, Michaelis J (2001) Risk factors for neuroblastoma at different stages of disease. Results from a population-based case-control study in Germany. J Clin Epidemiol 54:702–709
Schüz J, Spector LF, Ross JA (2003) Bias in studies of parental self-reported occupational exposures and childhood cancer. Am J Epidemiol 158:710–716
Schwartzbaum JA (1992) Influence of the mother's prenatal drug consumption on risk of neuroblastoma in the child. Am J Epidemiol 135:1358–1367
Shaw AK, Infante-Rivard C, Morrison HI (2004) Use of medication during pregnancy and risk of childhood leukemia (Canada). Cancer Causes Control 15:931–937
Shu XO, Perentesis JP, Wen W, Buckley JD, Boyle E, Ross JA, Robison LL (2004) Parental exposure to medications and hydrocarbons and ras mutations in children with acute lymphoblastic leukemia: a report from the Children's Oncology Group. Cancer Epidemiol Biomarkers Prev 13:1230–1235
Sibai BM (2003) Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol 102:181–192
Stokes ME, Davis CS, Koch GG (1995) Categorical data analysis using the SAS System. SAS Institute Inc., Cary, NC, USA
Thompson JR, Gerald PF, Willoughby ML, Armstrong BK (2001) Maternal folate supplementation in pregnancy and protection against acute lymphoblastic leukaemia in childhood: a case-control study. Lancet 358:1935–1940
UK Childhood Cancer Study Investigators (2000). The United Kingdom Childhood Cancer Study: objectives, materials and methods. UK Childhood Cancer Study Investigators. Br J Cancer 82:1073–1102
Unadkat JD, Dahlin A, Vijay S (2004) Placental drug transporters. Curr Drug Metab 5:125–131
van Poppel G, van den Berg H (1997) Vitamins and cancer. Cancer Lett 114:195–202
Wen W, Shu XO, Potter JD, Severson RK, Buckley JD, Reaman GH, Robison LL (2002) Parental medication use and risk of childhood acute lymphoblastic leukemia. Cancer 95:1786–1794
Wiemels JL, Cazzaniga G, Daniotti M, Eden OB, Addison GM, Masera G, Saha V, Biondi A, Greaves MF (1999) Prenatal origin of acute lymphoblastic leukaemia in children. Lancet 354:1499–1503
Wogelius P, Poulsen S, Sorensen HT (2005) Validity of parental-reported questionnaire data on Danish children's use of asthma-drugs: a comparison with a population-based prescription database. Eur J Epidemiol 20:17–22
Yankowitz J (2004) Pharmacologic treatment of hypertensive disorders during pregnancy. J Perinat Neonat Nurs 18:230–240
Acknowledgements
We would especially like to thank Dr. Ina Reiß for her skillful work on the data set and for the preparation of preliminary analyses. We would like to thank Monika Decher-Neff and Ilona Kerenyi for their assistance in coding the medications. We would also like to thank Drs. Rolf Meinert, Uwe Kaletsch and Jörg Michaelis for their work during the conducting of the original study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sponsored by the Federal Ministry for the Environment, Nuclear Safety, and Nature Protection.
Rights and permissions
About this article
Cite this article
Schüz, J., Weihkopf, T. & Kaatsch, P. Medication use during pregnancy and the risk of childhood cancer in the offspring. Eur J Pediatr 166, 433–441 (2007). https://doi.org/10.1007/s00431-006-0401-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-006-0401-z