Abstract
Background
The metabolic syndrome has been suggested as a unifying link between a “western” lifestyle and an increased prostate cancer risk.
Methods
We assessed the associations of components of the metabolic syndrome with prostate cancer in a prospective cohort based on 29,364 Norwegian men followed up for prostate cancer incidence and mortality from 1995–1997 to the end of 2005 in the second Nord Trøndelag Health Study (HUNT 2).
Results
During a mean 9.3 years follow-up, 687 incident prostate cancers were diagnosed, and 110 men died from prostate cancer. There was little evidence that baseline BMI, waist circumference, waist–hip ratio, total or HDL-cholesterol, triglycerides, presence of the metabolic syndrome, diabetes, antihypertensive use, or cardiovascular disease were associated with incident or fatal prostate cancer. There was weak evidence that raised blood pressure was associated with an increased risk: for each SD (12 mm) increase in diastolic blood pressure, there was an 8% (95% CI = 1–17%; p = 0.04) increased risk of incident prostate cancer.
Conclusions
We found little evidence to support the hypothesis that the metabolic syndrome or its components explains higher prostate cancer mortality rates in countries with a “western” diet and lifestyle. The positive association of blood pressure with prostate cancer warrants further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer mortality varies widely across the world, being 26-fold greater in the USA compared with China [1]. Identification of any modifiable environmental risk factors that might underlie these large mortality variations [2–5] could point to potentially effective prevention strategies [1]. Since prostate cancer mortality is high in countries characterized as having “westernized” lifestyles, diet and related behavioral exposures have been implicated as key factors [6]. The metabolic syndrome (a clustering of the metabolic risk factors hyperinsulinemia, hypertension, hypertriglyceridemia, low high-density lipoprotein (HDL) cholesterol, and abdominal adiposity [7, 8]) has been suggested as a unifying link between a “western” lifestyle and hormonal risk factors for prostate cancer [9, 10], perhaps via the IGF-I signaling pathway [11, 12]. The syndrome affects 25% of adults in the USA and is increasing [13], highlighting the potential growing importance of this exposure.
Hyperinsulinemia and measures of general and central adiposity have been positively associated with aggressive and fatal prostate cancer [10, 14–18], but fewer studies have investigated the other features of the metabolic syndrome. Hypertension [14, 19], lower HDL-cholesterol and raised triglycerides [14, 20], and combinations of metabolic syndrome components [21] have been positively associated with prostate cancer. Knowledge of associations of specific metabolic factors with prostate cancer could suggest novel prevention strategies [22, 23] and alternative biological pathways in prostate carcinogenesis [24, 25]. However, there are null or inconsistent findings with blood pressure [24, 26], total- and HDL-cholesterol [27, 28], central adiposity (waist circumference or waist–hip ratio [29, 30]), triglycerides [28], and other markers of insulin resistance [31, 32]. The limited number of positive studies many of which are based on small datasets suggests the possibility that some observed associations may have been due to chance findings or that publication bias has distorted the literature. We investigated the hypothesis that the following components of the metabolic syndrome are prospectively associated with prostate cancer in the second wave of the Nord Trøndelag Health Study (HUNT 2) (http://www.hunt.ntnu.no/): systolic and diastolic blood pressure, triglycerides, total and high-density lipoprotein (HDL) cholesterol, body mass index, and waist circumference. In secondary analyses, we investigated the hypothesis that the metabolic syndrome (defined, with modification, by the National Cholesterol Education Program’s Adult Treatment Panel (ATP) III criteria [33]) is associated with prostate cancer, assessed whether associations differed for advanced and fatal prostate cancer compared with localized disease, and investigated metabolic syndrome components in relation to survival amongst men diagnosed with prostate cancer.
Methods
Study population
Between 1995 and 1997, all residents in Nord-Trøndelag County in Norway aged 20 years or older were invited to participate in the second wave of the Nord-Trøndelag Health Study (HUNT 2). Among 92,936 eligible individuals, 64,943 (69.9%) accepted the invitation, completed questionnaires and attended a clinical examination (30,425 men and 34,518 women). Among the 30,425 men who participated, we excluded 882 men with prevalent cancer at baseline, 126 were excluded due to incomplete information on height or weight, 52 were excluded due to incomplete data on marital status, and one was excluded due to unknown date of participation. This study is therefore based on the follow-up for cancer of 29,364 men. The population in Nord-Trøndelag County (127,000 residents) is stable, with a net out-migration of 0.3% per year (1996–2000) and is ethnically homogenous (less than 3% non-Caucasian).
Baseline data
The study has been described in detail elsewhere (www.hunt.ntnu.no/forskning/metodeartikkel.pdf). Briefly, information was collected on a range of lifestyle and health-related factors, including past medical history, measures of physical activity, smoking, alcohol consumption, marital status, and education. At the clinical examination, standardized anthropometric measurements were conducted by the trained nurses: height was measured to the nearest centimeter; weight to the nearest half kilogram; and waist and hip circumference to the nearest centimeter. Additionally, blood pressure was measured automatically three times at 2-min intervals using a Dinamap 845XT (Critikon). The mean of the second and third reading was used in the analysis of diastolic, systolic, and mean arterial pressure. Finally, a blood sample (non-fasting) was drawn from all the participants, centrifuged at the research clinic, and sent in a cooler to the laboratory, usually on the same day. Serum samples were analyzed for glucose, total cholesterol, HDL-cholesterol, and triglycerides on a Hitachi 911 Auto-analyzer, applying reagents from Boehringer Mannheim. The data were used to derive a binary variable for the presence or absence of the metabolic syndrome in each man, as defined by the ATP III criteria, i.e., men who were above the threshold value for three or more of the following components were classified as having the metabolic syndrome: waist circumference (≥103 cm), triglycerides [≥150 mg/dl (≥1.7 mmol/l)], HDL-cholesterol [<40 mg/dl (<1.04 mmol/l)], and blood pressure (systolic ≥ 130 mmHg and/or diastolic ≥ 85 mmHg) [33]. Since we did not have fasting glucose levels, we replaced the glucose criteria (fasting glucose ≥ 110 mg/dl) with a non-fasting (random) glucose threshold of ≥200 mg/dl (≥11.1 mmol/l), which was defined as a positive screen in the health survey. This cut-off for random glucose has also been used in previous studies [34]. Obesity was defined as BMI ≥ 30 kg/m2.
Follow up
The unique 11-digit identity number of Norwegian citizens was used to link individuals from the HUNT Study to information on cancer incidence at the Cancer Registry of Norway. Prostate cancer was registered according to the International Classification of Diseases, seventh edition (ICD-7, code 177). We also used information from the Cancer Registry on metastasis at the time of diagnosis to classify men, who presented with either localized prostate cancer (defined as no invasion to surrounding tissues/organs, lymph nodes, or distant organs) or advanced prostate cancer (defined as regional or distant metastases) at diagnosis.
Information on deaths, where prostate cancer was registered as the underlying cause, was obtained by linkage to the Cause of Death Registry at Statistics Norway (ICD-9 code: 185; and ICD-10 code: C61).
For the analyses of prostate cancer incidence, each participant contributed person-time from the date of clinical examination until the date of any cancer diagnosis (of any site, not just prostate cancer), death, emigration, or to the end of follow-up till December 31, 2005, whichever occurred first. For the analysis of prostate cancer mortality, participants contributed person-years until death, emigration, or to the end of December 31, 2004. The use of different dates to define the end of follow-up for incidence (2005) and mortality (2004) is because the Cause of Death Registry linkage was not updated as recently as the Cancer Registry linkage at the time of obtaining the linked data for this study.
The study was approved by the Norwegian Data Inspectorate, the Norwegian Board of Health, and by the Regional Committee for Ethics in Medical Research.
Statistical analysis
We used Cox proportional hazards models to compute hazard ratios (HRs) with 95% confidence intervals (CI) for prostate cancer incidence and mortality, where men within quartiles 2–4 of each exposure variable were compared to the reference group of men in the lowest quartile (quartile cut-points were based on the distribution among all men in the study who had available data on a specific variable). Additionally, we calculated standard deviation (SD) scores for the exposure variables and estimated the HR associated with an increase in one SD. Since age is a strong determinant of prostate cancer risk, and individuals entered the study at different ages, we very closely controlled for current age in all models using age as the follow-up time scale in the Cox model [35]. In addition, we adjusted for height in quintiles (since height is independently associated with prostate cancer [36]), smoking status (never, former, current, and unknown), marital status (married, unmarried, widower, and divorced/separated), education (<10, 10–12, and ≥13 years), a recreational physical activity variable [37] (based on responses to questions on hours spent on light and hard activity during 1 week (averaged over a year): no activity; <3 h light activity; 3+ h light or <1 h hard activity; ≥1 h hard activity; unknown), and the International Prostate Symptom Score (no, mild, moderate, severe, and unknown lower urinary tract symptoms). Results for blood pressure were also controlled for the concurrent use of blood pressure medication, although this adjustment made little difference to affect estimates. Trend tests across quartiles of exposure level were calculated using the median value within each category in the Cox model. We examined the associations of the metabolic syndrome and its components with the following outcomes: all incident prostate cancers; whether prostate cancers were localized or advanced at diagnosis; and prostate cancer mortality. We also undertook an analysis restricted to those with incident prostate cancer to assess the associations of the metabolic syndrome and its components with survival (deaths from all causes).
We tested whether age at baseline could modify the association of exposure level with prostate cancer risk by constructing product terms between the exposure categories and age and testing for interaction using the likelihood ratio test. A cut-off value of 70 years of age was chosen to maximize numbers in each stratum. We also checked that the associations were similar in those with and without a history of cardiovascular disease or diabetes at baseline using the likelihood ratio test. In addition, we examined the association of the metabolic syndrome with prostate cancer risk across tertiles of BMI, given the findings of Pischon et al., who observed stronger associations of abdominal adiposity with prostate cancer in men with the lowest BMI tertile [18].
Departure from the proportional hazards assumption was evaluated by Schoenfeld residuals. All statistical tests were two-sided and all analyses were performed using Stata for Windows (Version 10© StataCorp LP, 1985–2007).
Results
The characteristics of the study participants at baseline are presented in Table 1. During a median follow-up of 9.3 years (258,359 person-years), 687 prostate cancers were diagnosed among the 29,364 studied men. We were able to classify 217 of these prostate cancer cases as localized and 136 as advanced at the time of diagnosis (334 were classified as unknown stage). Overall, 2,898 men died during the follow-up period, and of these, 110 (3.8%) men were registered with prostate cancer as the underlying cause of death. There was no evidence of departure from the proportional hazards assumption in the analyses described below.
There was no evidence that BMI, waist circumference, waist–hip ratio, total or HDL-cholesterol, triglyceride levels, random glucose levels, presence of the metabolic syndrome, number of metabolic factors present, or related factors (diabetes, being on blood pressure medication, or a history of cardiovascular disease) were associated with incident prostate cancer (Table 2). There was evidence that raised blood pressure levels were associated with an increased risk of prostate cancer. For example, for each SD increase in diastolic blood pressure (i.e., per 12 mmHg), there was an 8% (95% CI = 1–17%) increased risk of incident prostate cancer. Stratifying the outcomes by localized or advanced cancers (Table 3), also suggested largely null associations with prostate cancer by stage. However, there was evidence that for an SD increase in waist circumference (i.e., per 9.4 cm) there was a 16% increased risk of localized prostate cancer (95% CI = 1–32%), whereas there was no association of waist circumference with advanced cancers.
Table 4 suggested little evidence of associations of metabolic risk factors with death from prostate cancer and only a history of previous cardiovascular disease was associated with all-cause mortality in men with prostate cancer (Table 5).
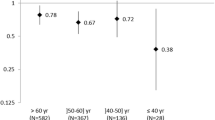
There was no evidence of interaction by age at baseline (<70 or ≥70 years) of associations of components of the metabolic syndrome with prostate cancer risk (e.g., for systolic blood pressure, p for interaction = 0.33; BMI, p = 0.98; and for total cholesterol, p = 0.55). Associations were similar in those with and without a history of cardiovascular disease at baseline (e.g., for systolic blood pressure, p for interaction = 0.74; BMI, p = 0.56; and for total cholesterol, p = 0.59). Sensitivity analyses excluding men with baseline diabetes did not materially alter the results, and there was no evidence for interaction with baseline diabetes (e.g., for metabolic syndrome, p for interaction = 0.31; systolic blood pressure, p = 0.86; and for total cholesterol, p = 0.81). However, there was some evidence of an interaction of metabolic syndrome with thirds of BMI (p = 0.03) [i.e., there was no association of metabolic syndrome with prostate cancer in the lowest third of BMI (HR = 1.03; 95% CI = 0.65–1.64), a positive association in the middle third (HR = 1.32; 95% CI = 0.98–1.77), and an inverse association in the highest third (HR = 0.77; 95% CI = 0.59–0.99)].
Discussion
Major findings
In this large population-based cohort study, we found little evidence that BMI, obesity, waist circumference, waist–hip ratio, total or HDL-cholesterol, triglycerides, presence of the metabolic syndrome, or related factors (diabetes, antihypertensives, or a history of cardiovascular disease) were associated with the development of incident, advanced, or fatal prostate cancer. There was weak evidence that increasing blood pressure levels may be positively associated with incident prostate cancer.
Strengths and limitations
This analysis has several strengths, including its defined county-wide population base, prospective design, cohort size of almost 30,000 men, follow-up of nearly 10 years, large number of incident prostate cancers, and almost 100% ascertainment of outcomes amongst those with exposure information at baseline.
In many countries, the underlying cause of death is assigned by the national cause of death registries on the basis of physician-completed death certificates, which are known to be unreliable, particularly for long-latency diseases in the elderly such as prostate cancer [38–40]. In Norway, however, the unique 11-digit identity number allows close collaboration between the Cancer Registry and the Cause of Death Registry, such that the underlying cause of death is assigned on the basis of information transferred from the Cancer Registry (year of diagnosis, histology, basis for and certainty of the diagnosis, and extent of disease at time of diagnosis), as well as death certificates, autopsy reports, and queries to physicians [41]. Validation of the prostate cancer data reported to the Cancer Registry has shown over 99% completeness [42] and that there was less than a 1% discrepancy between an underlying cause of death being assigned as prostate cancer from the official mortality statistics and, based on the same information, the underlying causes of death assigned by independent expert review [41]. In this study, only three of the 687 prostate cancers had not been morphologically verified.
Another strength was the ability to undertake analyses by whether cancers were localized or advanced at diagnosis based on whether cases presented with regional or distant metastasis. Since PSA screening is not routine in Norway, the cancers are likely to be largely clinically relevant and associations will not be distorted by the detection due to screening of biologically indolent cancers, which may be etiologically distinct [43].
Limitations of the study include the fact that the numbers of advanced and fatal prostate cancers were small, so we did not obtain precise effect estimates. As in all observational studies, the possible role of uncontrolled or residual confounding must be considered, but only negative confounding could explain our null results. It seems unlikely, however, that lack of control for ethnicity or family history, the major known risk factors for prostate cancer, would produce observed effect-estimates toward the null because the cohort was ethnically homogeneous and family history of prostate cancer is not known to be associated with insulin resistance. It also seems doubtful that residual confounding by dietary, behavioral, or other factors related to a “western” lifestyle would produce negative confounding, since these variables are likely to be positively associated with both our exposures and (if anything) prostate cancer. Some prostate cancers may not have become clinically evident, given the long-latency natural history of prostate cancer [44]. In the Cancer Registry, 334 (49%) of 687 cancers had unknown metastatic status at the time of diagnosis, and we were thus unable to classify these cases as advanced or localized. However, because there was little evidence of any substantial differences across the three outcome categories compared in Table 3, it is unlikely that complete information on stage would have made much difference to our conclusions. Only non-fasting glucose measures were available, limiting the secondary analysis of the association of our binary classification of the metabolic syndrome with prostate cancer.
Comparison with existing literature
The broadly null findings are in line with several studies, showing a lack of any consistent association of prostate cancer with levels of insulin [45–47], markers of hyperinsulinemia [31] or with gene variants associated with raised insulin levels [32]. Others have found inverse relationships of insulin resistance measures [48] or metabolic syndrome and its components [49, 50] with incident prostate cancer. This is in conflict with the hypothesis that insulin resistance explains the higher prostate cancer risk in westernized versus the non-westernized countries. It has been suggested that insulin resistance may be inversely associated with prostate cancer initiation and positively associated with aggressive prostate cancer, but the evidence for this hypothesis is weak [48] and our findings are not supportive. A positive association of metabolic syndrome with prostate cancer was observed in a prospective cohort study, but the results were based on only 56 prostate cancers [51], raising the possibility of a chance finding. Another cohort study with 507 prostate cancer cases reported a 56% increased risk of prostate cancer amongst men with three metabolic factors [21], but a recent review indicates that prospective data are limited [45].
Visceral fat is metabolically more active than subcutaneous or peripheral fat and abdominal adiposity is correlated with insulin resistance, glucose intolerance, dyslipidemia, and hypertension, perhaps more strongly than general adiposity measured by body mass index [52–55]. Our null findings for waist circumference, waist–hip ratio, and measures of visceral fat are in line with a meta-analysis, where the pooled effect-estimate for waist circumference was 1.03 in both prospective and case–control studies [30]. The studies included in that meta-analysis were based on incident cancers. A recent large prospective study, based on over 1 million person-years of follow-up, also found no association of waist circumference and waist–hip ratio with total prostate cancer, but these markers were positively associated with advanced prostate cancer (see also next paragraph) [18]. Our findings of no association of total and HDL-cholesterol with prostate cancer are in line with one other report [27] and with meta-analyses of trials and observational data, suggesting no association of cholesterol lowering statin therapy with prostate cancer [22]. One study reported higher HDL-cholesterol levels in men with prostate cancer (and higher total and LDL-cholesterol) [28], but this runs counter to the idea that the metabolic syndrome (characterized by low levels of HDL-cholesterol) may play a causal role in explaining international differences in prostate cancer between the western and non-western countries.
There was some evidence for an interaction of the association of metabolic syndrome with prostate cancer amongst strata defined by thirds of BMI, but the results were in the opposite direction to those of Pischon et al. [18], and these interactions probably arose by chance.
Our analysis shows no evidence of any association per standard deviation increase in body mass index, with point estimates of 0.98 for total, 0.98 for advanced, and 1.01 for fatal prostate cancers. Neither was there any strong evidence of associations of obesity with prostate cancer incidence, mortality, or survival. In contrast, a positive association of obesity with aggressive and fatal prostate cancer was a consistent finding amongst published studies recently reviewed by Hsing et al. [45] and Freedland and Platz [15], including strong evidence of a dose–response relationship of increasing degree of obesity in the Cancer Prevention Study II prospective cohort with over 4,000 cases [16]. Four large cohorts suggest a positive association of general adiposity with advanced prostate cancer: the Cancer Prevention Study I [56], Cancer Prevention Study II [16], a Swedish study [57], and the European Prospective Investigation into Cancer and Nutrition (EPIC) [18]. The numbers of advanced and fatal prostate cancers in our study were small and the effect estimates were imprecisely measured (wide confidence intervals), so we cannot rule out a positive association of BMI with more aggressive cancers. It is possible that change in weight from early to later life is important in prostate carcinogenesis [17].
Our findings do indicate the possibility that raised blood pressure is associated with prostate cancer incidence. Although associations of systolic and diastolic blood pressure were not always consistent with each other, this finding is in line with reports that hypertension was associated with a twofold increased risk of prostate cancer in African-Americans [19], with advanced prostate cancer [14], and with a reduced risk of prostate cancer associated with anti-hypertensive treatment [23]. It has been proposed that increased central sympathetic activity (which can occur with a raised blood pressure or heart rate) may result in androgen-mediated stimulation of prostate carcinogenesis [24], and our data are in line with this hypothesis. Misclassification of long-term exposure to high blood pressure levels by recent antihypertensive treatment may have attenuated the observed effect sizes toward the null. However, antihypertensive treatment was not associated with prostate cancer in our study. This finding warrants further investigation, because reports on the blood pressure association are few, null results have also been reported [24, 26] and prostate cancer may be more likely to be diagnosed among men being seen regularly for the treatment of hypertension.
In conclusion, several key components of the metabolic syndrome were not the risk factors for prostate cancer in our population-based cohort study. Our results, however, do not exclude a role for factors acting at the tissue level that are independent of measured intermediate phenotypes. For example, endogenous lipogenesis in prostate cancer cells may play a role in the accumulation of cholesterol and other lipid products in tumor cell membranes that may in turn regulate cancer cell growth and survival [25]. Neither can we exclude the presence of differential associations in different ethnic groups [19]. There was some evidence of a positive association of blood pressure with incident prostate cancer that warrants further investigation, as it supports a previously suggested hypothesis linking increased central sympathetic nervous activity with androgen-mediated stimulation of prostate cell growth [24].
References
Parkin DM (2004) International variation. Oncogene 23(38):6329–6340. doi:10.1038/sj.onc.1207726
Yatani R, Shiraishi T, Nakakuki K et al (1988) Trends in frequency of latent prostate carcinoma in Japan from 1965–1979 to 1982–1986. J Natl Cancer Inst 80(9):683–687. doi:10.1093/jnci/80.9.683
Post PN, Straatman H, Kiemeney LA, Coebergh JW (1999) Increased risk of fatal prostate cancer may explain the rise in mortality in The Netherlands. Int J Epidemiol 28(3):403–408. doi:10.1093/ije/28.3.403
Janssen F, Kunst AE, for The Netherlands Epidemiology, Demography Compression of Morbidity research group (2005) Cohort patterns in mortality trends among the elderly in seven European countries, 1950–99. Int J Epidemiol 34(5):1149–1159. doi:10.1093/ije/dyi123
Yu H, Harris RE, Gao YT, Gao R, Wynder EL (1991) Comparative epidemiology of cancers of the colon, rectum, prostate and breast in Shanghai, China versus the United States. Int J Epidemiol 20(1):76–81. doi:10.1093/ije/20.1.76
Hsing AW, Devesa SS (2001) Trends and patterns of prostate cancer: What do they suggest? Epidemiol Rev 23(1):3–13
Reaven GM (1988) Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 37(12):1595–1607. doi:10.2337/diabetes.37.12.1595
Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C, for the Conference Participants (2004) Definition of metabolic syndrome: report of the national heart, lung, and blood institute/American heart association conference on scientific issues related to definition. Circulation 109(3):433–438. doi:10.1161/01.CIR.0000111245.75752.C6
Giovannucci E (2003) Nutrition, insulin, insulin-like growth factors and cancer. Horm Metab Res 35(11/12):694–704
Barnard RJ, Aronson WJ, Tymchuk CN, Ngo TH (2002) Prostate cancer: another aspect of the insulin-resistance syndrome? Obes Rev 3(4):303–308. doi:10.1046/j.1467-789X.2002.00081.x
Renehan AG, Zwahlen M, Minder C, O’Dwyer ST, Shalet SM, Egger M (2004) Insulin-like growth factor (IGF)-1, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet 363:1346–1353. doi:10.1016/S0140-6736(04)16044-3
Fan W, Yanase T, Morinaga H et al (2007) Insulin-like growth factor 1/insulin signaling activates androgen signaling through direct interactions of Foxo1 with androgen receptor. J Biol Chem 282(10):7329–7338. doi:10.1074/jbc.M610447200
Ford ES, Giles WH, Dietz WH (2002) Prevalence of the metabolic syndrome among US adults: findings from the third national health and nutrition examination survey. JAMA 287(3):356–359. doi:10.1001/jama.287.3.356
Hammarsten J, Hogstedt B (2004) Clinical, haemodynamic, anthropometric, metabolic and insulin profile of men with high-stage and high-grade clinical prostate cancer. Blood Press 13(1):47–55. doi:10.1080/08037050310025735
Freedland SJ, Platz EA (2007) Obesity and prostate cancer: making sense out of apparently conflicting data. Epidemiol Rev 29:88–97. doi:10.1093/epirev/mxm006
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 348(17):1625–1638. doi:10.1056/NEJMoa021423
Wright ME, Chang SC, Schatzkin A et al (2007) Prospective study of adiposity and weight change in relation to prostate cancer incidence and mortality. Cancer 109(4):675–684. doi:10.1002/cncr.22443
Pischon T, Boeing H, Weikert S et al (2008) Body size and risk of prostate cancer in the european prospective investigation into cancer and nutrition. Cancer Epidemiol Biomarkers Prev 17(11):3252–3261. doi:10.1158/1055-9965.EPI-08-0609
Beebe-Dimmer JL, Dunn RL, Sarma AV, Montie JE, Cooney KA (2007) Features of the metabolic syndrome and prostate cancer in African-American men. Cancer 109(5):875–881. doi:10.1002/cncr.22461
Wuermli L, Joerger M, Henz S et al (2005) Hypertriglyceridemia as a possible risk factor for prostate cancer. Prostate Cancer Prostatic Dis 8(4):316–320. doi:10.1038/sj.pcan.4500834
Lund Haheim L, Wisloff TF, Holme I, Nafstad P (2006) Metabolic syndrome predicts prostate cancer in a cohort of middle-aged Norwegian men followed for 27 years. Am J Epidemiol 164(8):769–774. doi:10.1093/aje/kwj284
Browning DR, Martin RM (2007) Statins and risk of cancer: a systematic review and metaanalysis. Int J Cancer 120(4):833–843. doi:10.1002/ijc.22366
Fitzpatrick AL, Daling JR, Furberg CD, Kronmal RA, Weissfeld JL (2001) Hypertension, heart rate, use of antihypertensives, and incident prostate cancer. Ann Epidemiol 11(8):534–542. doi:10.1016/S1047-2797(01)00246-0
Gann PH, Daviglus ML, Dyer AR, Stamler J (1995) Heart rate and prostate cancer mortality: results of a prospective analysis. Cancer Epidemiol Biomarkers Prev 4(6):611–616
Freeman MR, Solomon KR (2004) Cholesterol and prostate cancer. J Cell Biochem 91(1):54–69. doi:10.1002/jcb.10724
Friedman GD (1997) Blood pressure and heart rate: no evidence for a positive association with prostate cancer. Ann Epidemiol 7(7):486–489. doi:10.1016/S1047-2797(97)00083-5
Bidoli E, Talamini R, Bosetti C et al (2005) Macronutrients, fatty acids, cholesterol and prostate cancer risk. Ann Oncol 16(1):152–157. doi:10.1093/annonc/mdi010
Niemi M, Kervinen K, Kiviniemi H et al (2000) Apolipoprotein E phenotype, cholesterol and breast and prostate cancer. J Epidemiol Community Health 54(12):938–939. doi:10.1136/jech.54.12.938
MacInnis RJ, English DR, Gertig DM, Hopper JL, Giles GG (2003) Body size and composition and prostate cancer risk. Cancer Epidemiol Biomarkers Prev 12(12):1417–1421
MacInnis RJ, English DR (2006) Body size and composition and prostate cancer risk: systematic review and meta-regression analysis. Cancer Causes Control 17(8):989–1003. doi:10.1007/s10552-006-0049-z
Borugian MJ, Spinelli JJ, Sun Z et al (2007) Prediagnostic C-peptide and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev 16(10):2164–2165. doi:10.1158/1055-9965.EPI-07-0495
Moore SC, Leitzmann MF, Weinstein SJ et al (2007) Insulin resistance-related gene polymorphisms and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev 16(6):1315–1317. doi:10.1158/1055-9965.EPI-07-0191
National Cholesterol Education Program Expert Panel (2002) Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation 106(25):3143
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE (2002) Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 87(3):978–982. doi:10.1210/jc.87.3.978
Kom EL, Graubard BI, Midthune D (1997) Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 145(1):72–80
Zuccolo L, Harris R, Gunnell D et al (2008) Height and prostate cancer risk: a large nested case–control study (ProtecT) and meta-analysis. Cancer Epidemiol Biomarkers Prev 17(9):2325–2336. doi:10.1158/1055-9965.EPI-08-0342
Nilsen TI, Romundstad PR, Vatten LJ (2006) Recreational physical activity and risk of prostate cancer: a prospective population-based study in Norway (the HUNT study). Int J Cancer 119(12):2943–2947. doi:10.1002/ijc.22184
Makinen T, Karhunen P, Aro J, Lahtela J, Maattanen L, Auvinen A (2008) Assessment of causes of death in a prostate cancer screening trial. Int J Cancer 122(2):413–417. doi:10.1002/ijc.23126
Newschaffer CJ, Otani K, McDonald MK, Penberthy LT (2000) Causes of death in elderly prostate cancer patients and in a comparison nonprostate cancer cohort. J Natl Cancer Inst 92(8):613–621. doi:10.1093/jnci/92.8.613
Miller AB, Yurgalevitch S, Weissfeld L (2000) Death review process in the prostate, lung, colorectal and ovarian (PLCO) cancer screening trial. Control Clin Trials 21(6, supplement 1):400S–406S. doi:10.1016/S0197-2456(00)00095-7
Hernes E, Harvei S, Glattre E, Gjertsen F, Fossa SD (2005) High prostate cancer mortality in Norway: influence of cancer registry information? APMIS 113(7–8):542–549. doi:10.1111/j.1600-0463.2005.apm_245.x
Harvei S, Tretli S, Langmark F (1996) Quality of prostate cancer data in the cancer registry of Norway. Eur J Cancer 32(1):104–110. doi:10.1016/0959-8049(95)00501-3
Giovannucci E, Liu Y, Platz EA, Stampfer MJ, Willett WC (2007) Risk factors for prostate cancer incidence and progression in the health professionals follow-up study. Int J Cancer 121(7):1571–1578. doi:10.1002/ijc.22788
Albertsen PC, Hanley JA, Fine J (2005) 20-Year outcomes following conservative management of clinically localized prostate cancer. J Am Med Assoc 293(17):2095–2101. doi:10.1001/jama.293.17.2095
Hsing AW, Sakoda LC, Chua SC Jr (2007) Obesity, metabolic syndrome, and prostate cancer. Am J Clin Nutr 86(3):S843–S857
Stattin P, Kaaks R (2003) Re: insulin resistance and prostate cancer risk. J Natl Cancer Inst 95(14):1086–1087
Stattin P, Soderberg S, Hallmans G et al (2001) Leptin is associated with increased prostate cancer risk: a nested case-referent study. J Clin Endocrinol Metab 86(3):1341–1345. doi:10.1210/jc.86.3.1341
Stocks T, Lukanova A, Rinaldi S et al (2007) Insulin resistance is inversely related to prostate cancer: a prospective study in Northern Sweden. Int J Cancer 120(12):2678–2686. doi:10.1002/ijc.22587
Tande AJ, Platz EA, Folsom AR (2006) The metabolic syndrome is associated with reduced risk of prostate cancer. Am J Epidemiol 164(11):1094–1102. doi:10.1093/aje/kwj320
Ness KK, Oakes JM, Punyko JA, Baker KS, Gurney JG (2005) Prevalence of the metabolic syndrome in relation to self-reported cancer history. Ann Epidemiol 15(3):202–206. doi:10.1016/j.annepidem.2004.07.092
Laukkanen JA, Laaksonen DE, Niskanen L, Pukkala E, Hakkarainen A, Salonen JT (2004) Metabolic syndrome and the risk of prostate cancer in Finnish men: a population-based study. Cancer Epidemiol Biomarkers Prev 13(10):1646–1650
Dalton M, Cameron AJ, Zimmet PZ et al (2003) Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med 254(6):555–563. doi:10.1111/j.1365-2796.2003.01229.x
Karter AJ, D’Agostino RB, Mayer-Davis EJ et al (2005) Abdominal obesity predicts declining insulin sensitivity in non-obese normoglycaemics: the insulin resistance atherosclerosis study (IRAS). Diabetes Obes Metab 7(3):230–238. doi:10.1111/j.1463-1326.2004.00441.x
Ohlson LO, Larsson B, Svardsudd K et al (1985) The influence of body fat distribution on the incidence of diabetes mellitus. 13.5 years of follow-up of the participants in the study of men born in 1913. Diabetes 34(10):1055–1058. doi:10.2337/diabetes.34.10.1055
Richelsen B, Pedersen SB (1995) Associations between different anthropometric measurements of fatness and metabolic risk parameters in non-obese, healthy, middle-aged men. Int J Obes Relat Metab Disord J Int Assoc Stud Obes 19(3):169–174
Rodriguez C, Patel AV, Calle EE, Jacobs EJ, Chao A, Thun MJ (2001) Body mass index, height, and prostate cancer mortality in two large cohorts of adult men in the United States. Cancer Epidemiol Biomarkers Prev 10(4):345–353
Andersson SO, Wolk A, Bergstrom R et al (1997) Body size and prostate cancer: a 20-year follow-up study among 135006 Swedish construction workers. J Natl Cancer Inst 89(5):385–389. doi:10.1093/jnci/89.5.385
Acknowledgments
The hypothesis was developed by RMM, DG, and LV. TILN did the statistical analysis with advice from PR. RMM wrote the first draft of the manuscript with input on the methods from TILN. RMM, DG, LV, PR, and TILN all critically commented on and edited earlier drafts and approved the final version of the article. TILN had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of interest
None to declare.
Funding
The study design, conduct, and data collection were supported by the Norwegian Research Council. Analysis and interpretation of the data, preparation, review, and approval of the article were unfunded.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martin, R.M., Vatten, L., Gunnell, D. et al. Components of the metabolic syndrome and risk of prostate cancer: the HUNT 2 cohort, Norway. Cancer Causes Control 20, 1181–1192 (2009). https://doi.org/10.1007/s10552-009-9319-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9319-x