Abstract
Purpose
To estimate the effect of metabolic syndrome (MetS) on the prevalence of prostate cancer using a large retrospective cohort with a 5-year follow-up duration.
Methods
National Health Insurance Service health checkup cohort was used for the study. In total, 130,342 men included in the health checkup cohort in 2009 were divided into two groups according to the presence of prostate cancer. The prevalence of prostate cancer from 2009 to 2013 was cumulatively calculated from 2003. A generalized estimating equation was used to assess the effect of MetS and its component on the prevalence of prostate cancer after adjusting for other variables.
Results
Prostate cancer was present in 2369 men (1.8%) in 2009. The prevalence of prostate cancer was significantly higher in patients with MetS than in those without MetS throughout the entire follow-up duration. Multivariable analysis showed that in addition to year at evaluation and age, the presence of MetS was associated with an increased prevalence of prostate cancer. Alcohol consumption and smoking levels were negatively associated with the prevalence of prostate cancer. Among MetS components, decreased high density lipoprotein (HDL)-cholesterolemia and central obesity were associated with an increased prevalence of prostate cancer after adjusting for other variables.
Conclusion
MetS and its components, especially decreased HDL-cholesterol levels and central obesity, were related to the increased prevalence of prostate cancer. Preventing MetS, maintaining high HDL-cholesterol level, and maintaining low waist circumference might be useful ways for decreasing the prevalence of prostate cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the second most common cancer in men worldwide, and approximately 1.1 million men were diagnosed with prostate cancer in 2012 (Ferlay et al. 2015). Although unmodifiable variables, such as race, age, and family history, are established risk factors for prostate cancer, several studies have been performed to determine modifiable variables for preventing the development of prostate cancer (Lippman et al. 2009; Klein et al. 2011). As a result, some diets have been reported as possible risk factors for prostate cancer, although these results remain to be validated (Grönberg 2003). However, the current clinical guidelines do not recommend any specific lifestyle modification and/or treatment to reduce the risk of prostate cancer (Mottet et al. 2017).
Metabolic syndrome (MetS) is a cluster of several lifestyle-associated diseases, and the prevalence of MetS in the general population is reported to be 25–40% (Yoo et al. 2018). Interestingly, there has been emerging evidence supporting the positive association between MetS and the development of several types of cancer (Esposito et al. 2012). In addition, a recent large cohort study reported that the presence of MetS was associated with an increased risk of prostate cancer (Bhindi et al. 2015). Moreover, MetS was reported to worsen oncological outcomes of prostate cancer (Bhindi et al. 2016). However, other studies have reported opposite results (Gacci et al. 2017), and the effects of MetS on the risk of prostate cancer remain unclear. In addition, because MetS is a cluster of metabolic diseases as mentioned above, the effects of each MetS-related disease on the risk of prostate cancer remain unknown.
To accurately elucidate the relationships between prostate cancer and MetS and its components, a large prospective cohort study with extensive follow-up duration is considered to be needed; however, this could not be easily performed owing to cost and time consumption. Thus, we aimed to estimate the effects of MetS and its components on the prevalence of prostate cancer using a large retrospective cohort with a 5-year follow-up duration; the cohort was derived from the National Health Insurance Service (NHIS) health checkup cohort. Moreover, we also adjusted for some lifestyle variables, including smoking and drinking levels, because they are associated with the development of both MetS and several cancers (Cao et al. 2015; Alexandrov et al. 2016).
Methods
Patient cohort
In Korea, NHIS covers the medical costs spent by almost the entire Korean population of 50 million people, and NHIS provides biannual health checkups for those aged ≥ 40 years. NHIS offered a health checkup cohort database, which included > 510,000 individuals who underwent a health checkup between 2003 and 2013. A detailed explanation of the database and study cohort was previously described (Yoo et al. 2018). From these databases, we selected men who had adequate information regarding MetS and its components, and 130,342 men were ultimately included in the analysis. This study was approved by the Institutional Review Board of Boramae Medical Center.
Definitions
MetS was defined based on the National Cholesterol Education Program-Adult Treatment Panel III guidelines (Grundy et al. 2004), and MetS status was determined by the same methods used in a previous study (Yoo et al. 2018). Men diagnosed with prostate cancer from 2003 to 2009 were considered as patients with prostate cancer at baseline. The presence of prostate cancer was defined using the Korean Classification of Diseases, 6th revision code of C61, which was modified based on the International Classification of Diseases, 10th revision. The prevalence of prostate cancer from 2009 to 2013 was calculated cumulatively from 2003 to 2009–2013, respectively. Weekly alcohol consumption and lifelong smoking history were assessed using questionnaires included in the health screening performed in 2009. Residence was classified into two groups (urban vs. rural), and income was also divided into two groups (low income vs. non-low income) as described in the previous study (Yoo et al. 2018).
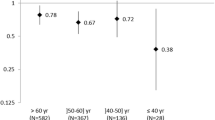
Statistical analysis
The study cohort was divided into two groups according to the presence of prostate cancer in 2009. Baseline characteristics in 2009 were represented and compared based on the presence of prostate cancer in 2009. The mean ± standard deviation or median and interquartile range were used for continuous variables. Frequency and percentage were used for categorical variables. Because the prevalence of prostate cancer was highly affected by age, the study population was divided into four groups according to age in 2009 (40 s vs. 50 s vs. 60 s vs. 70 s). The cumulative prevalence of prostate cancer according to the concomitant MetS status was presented and compared. In addition, the prevalence of prostate cancer from 2009 to 2013 was calculated according to the age categories. Before analysis, a square root transformation was performed for the level of alcohol consumption because of its skewed distribution. A generalized estimating equation was used to assess variables that showed a significant association with the prevalence of prostate cancer. Similarly, a generalized estimating equation was used to assess the effect of each MetS component on the prevalence of prostate cancer after adjusting for the year at the time of evaluation, residence, income, and smoking and alcohol consumption levels. All statistical analyses were performed using the SAS software version 9.4.2 (SAS institute, Cary, NC) and R software version 3.4.2 (http://www.r-project.org). p values < 0.05 were considered statistically significant.
Results
Baseline characteristics
From 2003 to 2009, prostate cancer was detected in 2369 men (1.8%). Men with prostate cancer were older (65.7 vs. 57.6 years, p < 0.001), and waist circumference in men with prostate cancer was higher than that in men without prostate cancer (85.0 vs. 84.4 cm, p < 0.001). Men with prostate cancer were more likely to live in a rural area than those without prostate cancer (33.0% vs. 32.1%, p = 0.034). On health checkup, systolic (125.9 vs. 126.5 mmHg, p = 0.049) and diastolic blood pressure (77.1 vs. 78.9 mmHg, p < 0.001) were significantly lower in men with prostate cancer than in men without prostate cancer. Serum triglyceride levels were lower in men with prostate cancer than in men without prostate cancer (132.9 vs. 152.2 mg/dL, p < 0.001). MetS was more common in men with prostate cancer than in men without prostate cancer (40.1% vs 34.4%, p < 0.001), and among MetS components, central obesity (27.4% vs. 23.7%, p < 0.001), hypertension (66.3% vs. 60.8%, p < 0.001), and decreased HDL-cholesterolemia (33.7% vs. 24.8%, p < 0.001) were more frequently observed in men with prostate cancer than in men without prostate cancer. However, the incidence of diabetes mellitus and triglyceridemia were equivalent between the two groups (Table 1).
Correlation between the prevalence of prostate cancer and MetS
The prevalence of prostate cancer was significantly higher in men with MetS than in those without MetS throughout the entire follow-up duration (2009: 2.12% vs. 1.66%; 2010: 2.31% vs. 1.84%; 2011: 2.51% vs. 2.02%; 2012: 2.78% vs. 2.22%; and 2013: 3.06% vs. 2.42%, p < 0.001 for all) (Table 2). After age stratification, the prevalence of prostate cancer was significantly higher in men with MetS only in those aged ≥ 70 years. This was observed throughout the entire study period (2009: 5.91% vs. 4.90%; 2010: 6.47% vs. 5.50%; 2011: 6.96% vs. 6.13%; 2012: 7.49% vs. 6.51%; and 2013: 8.08% vs. 7.01%, p < 0.05 for all). The prevalence of prostate cancer in men aged < 70 years was equivalent regardless of the presence of MetS.
Effect of MetS on the prevalence of prostate cancer
Multivariable analysis showed that MetS was associated with an increased prevalence of prostate cancer (odds ratio [OR]: 1.170, p = 0.002) after adjusting for the year at evaluation, age, residence, and smoking and alcohol consumption levels (Table 3). Alcohol consumption (OR: 0.972, p < 0.001) and smoking (OR: 0.996, p < 0.007) levels were negatively associated with the prevalence of prostate cancer. In addition, year at evaluation (OR: 1.118, p < 0.001) and age (OR: 1.094, p < 0.001) were related to an increased prevalence of prostate cancer. Among MetS components, decreased HDL-cholesterol levels (OR: 1.303, p < 0.001) was the strongest associated factor for the increased prevalence of prostate cancer after adjusting for other variables (Table 4). In addition, central obesity (OR: 1.149. p < 0.001) was another significantly related factor for the increased prevalence of prostate cancer.
Discussion
Prostate cancer is the most common solid cancer in Western men and is rapidly increasing in prevalence in Asian and developing countries (Stewart and Wild 2017). In the current study, prostate cancer incidence rate per year in Korean men aged ≥ 40 years was approximately 0.2%, which was similar to those in other Asian countries (Baade et al. 2013). Because the risk of prostate cancer dramatically increases with age (Baade et al. 2013), the incidence of prostate cancer is not considered to be decreased in the near future owing to increased life expectancy in modern society. If useful methods for preventing prostate cancer could be identified, a huge amount of socioeconomic costs would be saved, and the health of elderly men would be greatly improved. In this regard, more attention is needed to prevent prostate cancer. As described previously, MetS is another health issue that has recently become more widespread, and some studies have reported that MetS increases the risk of cancers, including prostate cancer, through several pathways (Cowey and Hardy 2006). However, the association between prostate cancer and MetS remain unclear, and more reliable studies that are focused on these associations are awaited. In this regard, we evaluated the effects of MetS and its components, in addition to other lifestyle factors, on the prevalence of prostate cancer using a large historical cohort.
In this large retrospective cohort study with a 5-year follow-up duration, we showed that the presence of MetS and the prevalence of prostate cancer were positively correlated, which was in concordance with that reported in a previous study (Gacci et al. 2015). Moreover, the results of the current study are considered to be useful because MetS status was associated with the increased prevalence of prostate cancer in the 5 years of follow-up. However, based on the results of the current study, the effects of MetS on the prevalence of prostate cancer are only significant in elderly men aged > 70 years. Although preventing MetS does not seem to be effective in decreasing the prevalence of prostate cancer in men aged < 70 years, it would be more appropriate to interpret these results because the effect of MetS on prostate cancer seemed to gradually and significantly increase with age. Moreover, because men in their 70 s showed an incidence of prostate cancer of > 5.0%, which was significantly higher than that in men in their 60 s or younger, a decrease in prostate cancer prevalence in men in their 70 s should not be underestimated. Based on the current study, the prevention of MetS using adequate exercise and/or diet improves general health and may also be a novel method to prevent prostate cancer. Although the causal relationship between the two diseases remains to be evaluated, several possible mechanisms between MetS and prostate cancer development have been suggested in previous studies (Rhee et al. 2016). The current study may be helpful in providing more reliable data for the correlation between MetS and prostate cancer, and future studies, which focus on the causal relationship between the two diseases, should be conducted based on the results of the current study.
Among MetS components, decreased HDL-cholesterol levels were determined to be the most significant factor associated with the increased prevalence of prostate cancer, which was similar to the results of previous studies (Ahn et al. 2009; Mondul et al. 2011; Van Hemelrijck et al. 2011). In a previous study, in addition to inhibition of oxidation and inflammation, cholesterol transportation from cells by HDL-cholesterol was suggested as a reason for the prevention of prostate cancer development by HDL-cholesterol.
(Kwiterovich 2000). Although some other studies showed opposite results (Mondul et al. 2011), these controversies could be owing to incomplete information regarding serum HDL-cholesterol level and medication usage. Because the current study used the medication usage data from the NHIS database and serum HDL-cholesterol level from the NHIS health checkup database, the results of the current study are thought to be reliable with regard to this aspect, although racial differences could be another reason. In addition, the presence of central obesity was determined to be associated with an increased prevalence of prostate cancer, which was in accordance with that reported in a previous study (Parikesit et al. 2016). Although the detailed pathophysiology remains unknown, adipokines may be the molecular mediator between the diseases, as reported previously (Mistry et al. 2007).
Alcohol consumption per week was determined as a negatively associated factor with the prevalence of prostate cancer, which is supported by previous studies (Schoonen et al. 2005; Zuccolo et al. 2013). However, because other studies suggested a positive association between alcohol consumption and prostate cancer, including advanced prostate cancer (Sawada et al. 2014; Dickerman et al. 2016), it is not appropriate to consume alcohol to prevent prostate cancer. Although the pathophysiology of alcohol consumption on prostate cancer has not been completely understood, a previous study reported that alcohol consumption could deplete testosterone levels (Oremosu and Akang 2015), and this could be a possible explanation for our findings. However, the association between alcohol consumption and prostate cancer in this study could be affected by the early detection of prostate cancer in men who have a greater interest in their health status. In other words, the characteristics of men with a high level of interest in their health could be interpreted as factors related to the prevalence of prostate cancer. Similarly, although the increased amount of smoking was also determined to be a factor associated with a decreased risk of prostate cancer with an upper limit of 95% confidence interval of nearly 1.000, these results should be carefully interpreted.
The limitation of the current study was its retrospective design, although the current study included a large number of men (over 130,000) and had a follow-up duration of 5 years. In addition, the prevalence of prostate cancer could be underestimated because the prevalence of prostate cancer in 2009 was calculated from 2003. Another limitation is the lack of data regarding the severity of prostate cancer, such as pretreatment prostate-specific antigen level, Gleason score, and/or clinical/ pathologic stage. In other words, there might be a chance to early detection of prostate cancer in men with MetS because these men with MetS might have more opportunity to visit clinics and more interests on their health status. However, despite these limitations, the current study could be useful for clinicians to educate and manage their patients, especially men who had a high risk for prostate cancer.
In conclusions, based on this large retrospective cohort study with 5-year follow-up, MetS and its components, including decreased HDL-cholesterol levels and central obesity, were determined to be variables associated with an increased prevalence of prostate cancer. Preventing MetS and maintaining HDL-cholesterol level and waist circumference might be useful ways for decreasing the prevalence of prostate cancer, although these findings remain to be validated in future studies.
References
Ahn J, Lim U, Weinstein SJ, Schatzkin A, Hayes RB, Virtamo J, Albanes D (2009) Prediagnostic total and high-density lipoprotein cholesterol and risk of cancer. Cancer Epidemiol Prev Biomark 18:1055–9965. (EPI-1008-1248)
Alexandrov LB et al (2016) Mutational signatures associated with tobacco smoking in Human Cancer. Science 354:618–622
Baade PD, Youlden DR, Cramb SM, Dunn J, Gardiner RA (2013) Epidemiology of prostate cancer in the Asia–Pacific region. Prostate Int 1:47–58
Bhindi B et al (2015) Dissecting the association between metabolic syndrome and prostate cancer risk: analysis of a large clinical cohort. Eur Urol 67:64–70
Bhindi B et al (2016) Influence of metabolic syndrome on prostate cancer stage, grade, and overall recurrence risk in men undergoing radical prostatectomy. Urology 93:77–85
Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL (2015) Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ 351:h4238
Cowey S, Hardy RW (2006) The metabolic syndrome: a high-risk state for cancer? Am J Pathol 169:1505–1522
Dickerman BA, Markt SC, Koskenvuo M, Pukkala E, Mucci LA, Kaprio J (2016) Alcohol intake, drinking patterns, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control 27:1049–1058
Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D (2012) Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care 35:2402–2411
Ferlay J et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012 Int J Cancer 136: E359–E386
Gacci M et al (2015) Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int 115:24–31
Gacci M et al (2017) Meta-analysis of metabolic syndrome and prostate cancer. Prostate Cancer Prostatic Dis 20:146
Grönberg H (2003) Prostate cancer epidemiology. Lancet 361:859–864
Grundy SM et al (2004) Implications of recent clinical trials for the national cholesterol education program adult treatment panel III guidelines. Circulation 110:227–239. https://doi.org/10.1161/01.cir.0000133317.49796.0e
Klein EA et al (2011) Vitamin E and the risk of prostate cancer: the selenium and vitamin E cancer prevention trial (SELECT). JAMA 306:1549–1556
Kwiterovich PO Jr (2000) The metabolic pathways of high-density lipoprotein, low-density lipoprotein, and triglycerides: a current review. Am J Cardiol 86:5 l–10 l
Lippman SM et al (2009) Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the selenium and vitamin E cancer prevention trial (SELECT). JAMA 301:39–51
Mistry T, Digby JE, Desai KM, Randeva HS (2007) Obesity and prostate cancer: a role for adipokines. Eur Urol 52:46–53. https://doi.org/10.1016/j.eururo.2007.03.054
Mondul AM, Weinstein SJ, Virtamo J, Albanes D (2011) Serum total and HDL cholesterol and risk of prostate cancer. Cancer Causes Control 22:1545
Mottet N et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71:618–629
Oremosu AA, Akang EN (2015) Impact of alcohol on male reproductive hormones, oxidative stress and semen parameters in Sprague–Dawley rats. Middle East Fertil Soc J 20:114–118
Parikesit D, Mochtar CA, Umbas R, Hamid ARAH (2016) The impact of obesity towards prostate diseases. Prostate Int 4:1–6. https://doi.org/10.1016/j.prnil.2015.08.001
Rhee H, Vela I, Chung E (2016) Metabolic syndrome and prostate cancer: a review of complex interplay amongst various endocrine factors in the pathophysiology and progression of prostate cancer. Horm Cancer 7:75–83
Sawada N, Inoue M, Iwasaki M, Sasazuki S, Yamaji T, Shimazu T, Tsugane S (2014) Alcohol and smoking and subsequent risk of prostate cancer in Japanese men: the Japan Public Health Center-based prospective study. Int J Cancer 134:971–978
Schoonen WM, Salinas CA, Kiemeney LA, Stanford JL (2005) Alcohol consumption and risk of prostate cancer in middle-aged men. Int J Cancer 113:133–140
Stewart B, Wild CP (eds) (2017) World cancer report 2014. International Agency for Research on Cancer, Lyon (ISBN: 978-92-832-0429-9)
Van Hemelrijck M et al (2011) Low levels of apolipoprotein AI and HDL are associated with risk of prostate cancer in the Swedish AMORIS study. Cancer Causes Control 22:1011–1019
Yoo S, Oh S, Park J, Cho SY, Cho MC, Jeong H, Son H (2018) The impacts of metabolic syndrome and life style on the prevalence of benign prostatic hyperplasia requiring treatment: historical cohort study using 130,454 men. BJU Int. https://doi.org/10.1111/bju.14528
Zuccolo L, Lewis SJ, Donovan JL, Hamdy FC, Neal DE, Smith GD (2013) Alcohol consumption and PSA-detected prostate cancer risk—a case-control nested in the ProtecT study. Int J Cancer 132:2176–2185
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animal
Not applicable.
Informed consent
Informed consent waive by IRB.
Rights and permissions
About this article
Cite this article
Yoo, S., Oh, S., Park, J. et al. Effects of metabolic syndrome on the prevalence of prostate cancer: historical cohort study using the national health insurance service database. J Cancer Res Clin Oncol 145, 775–780 (2019). https://doi.org/10.1007/s00432-019-02842-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-02842-1