Abstract
Objective
To evaluate the effect of obesity on the presentation and course of disease in patients with gynecological cancers.
Study design
Records of patients with endometrial (n = 1180), cervical (n = 738), and ovarian cancer (n = 824) treated between 1986 and 2005 were reviewed. Body mass index (BMI) was analyzed in relation to tumor stage, tumor grading, and prognosis. Steroid hormone receptor status and growth fraction (MIB1; Ki-67-antigen) of tumors in relation to BMI were analyzed in subgroups with endometrial (n = 183) and advanced ovarian (n = 221) cancers. In the latter subgroup, tumor vascularization (CD31) and expression of bcl-2, c-erb-B2, fibronectin, and tumor markers (CA-125, CA15-3, CEA) were also evaluated. Statistical analyses included bivariate correlation, cross-tabulation, Kaplan-Meier-survival analyses, and multifactorial residual survival analyses.
Results
Obese patients with endometrial carcinoma were significantly younger (p < 0.001) and their tumors were less advanced at diagnosis (p = 0.001) and were better differentiated (p = 0.010). In the subgroups, neither steroid hormone receptor status nor MIB1-determined growth fraction correlated with BMI. For both endometrial and cervical carcinomas, a high BMI influenced overall survival favorably (p endometrial = 0.004 and p cervical = 0.026). In ovarian cancer, there was a trend toward improved survival in more obese patients (p = 0.053). Immunohistochemistry revealed that c-erb-B2 expression was slightly lower in tumors of obese patients (r = −0.142; p = 0.039), but BMI did not influence any other factor.
Conclusions
Although obesity increases the incidence of cancer, a high BMI does not seem to adversely influence the prognosis in patients with the mentioned gynecological malignancies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumorigenesis is generally considered to be a multistep procedure modulated by risk factors as well as protective factors. Obesity is of current interest in tumorigenesis since the percentage of overweight people is increasing steadily in the western world [1, 2]. Overweight has long been recognized as a risk factor for diabetes and cardiovascular diseases [3]. More recently, it has become clear that overeating and obesity may be the largest avoidable causes of cancer in nonsmokers, accounting for one in seven cancer deaths in men and one in five in women in the USA [4]. This relationship seems to hold true for many gynecologic cancers—in particular, ovarian and endometrial cancer [5, 6]. However, the role of obesity in cervical carcinomas is still undefined. Apart from that, obese women are less likely to participate in screening measures, to have more problems related to surgery, higher mortality from causes other than endometrial cancer, and experience more cutaneous but less gastrointestinal toxicity when receiving adjuvant radiation therapy [7–9].
Although recent studies have shown the influence of a high body mass index (BMI) on the biology of endometrial cancers [10–13], results for ovarian cancer are conflicting [14, 15]. In this study, we have endeavored to clarify the relationship between BMI and gynecological cancers by analyzing data from all patients with endometrial, cervical, and ovarian cancers who were treated at our clinic in the past 20 years.
Patients and methods
Cases
Clinical records of 1,180 patients with endometrial cancer, 738 with cervical cancer, and 824 with ovarian cancer were identified from the university’s cancer registry. These records were re-evaluated for BMI and common prognostic factors such as the patients’ age, tumor stage (FIGO), histological tumor grading, and for survival status or causes of death (cancer-associated versus cancer-independent) at the time of last routine follow-up (December 2006). (In our cancer centre, survival status of all patients is assessed once every two years. On average, we had complete follow-up of 93.6% of our patients across the disease groups. By calling up the patients’ family physicians or gynecologists, we investigated the survival status of those patients who did not attend our outpatient department for gynecological oncological aftercare. The system used for the management of patient data was the Giessen Tumor Dokumentation System, GTDS).
All patients referred to, treated, and followed up at the Department of Obstetrics and Gynecology of the Justus-Liebig-University Giessen between 1986 and 2005 were included in the analyses. There were no other criteria for inclusion than histological proof of the particular malignant tumor type. Patients’ characteristics are shown in Table 1. BMI was categorized according to the Deutsche Gesellschaft für Ernährung e.V. (German Society for Nutrition) as shown in Table 1. For the calculation of the BMI, we used the preoperative weight at diagnosis. When information on grading, tumor stage, etc. was not exactly reported, unclear, or conflicting, the data were classified as unknown or unclear.
Endometrial cancer
Most patients with endometrial carcinoma underwent primary surgery. Only patients with severe comorbidity received primary radiotherapy, which was followed by control curettage three months later. Patients with tumor stages Ia and Ib received vaginal high-dose-rate afterloading radiotherapy, while those with more advance tumor stages were treated with combined abdominal fields and intravaginal afterloading radiotherapy. Afterloading radiotherapy was carried out using iridium-192 as a source (high-dose-rate afterloading). In cases of primary radiotherapy, a one-tube applicator was chosen. We used hysterography with an indwelling applicator to exclude patients with uterine cavities that were unsuitable for this type of treatment. Postoperative radiotherapy was administered using an ovoid-shaped applicator. Low-risk cases (≤stage Ib, tumor grading ≤2, and absence of lymphangiosis carcinomatosa) received intravaginal afterloading radiotherapy (4 × 10 Gy or 5 × 8 Gy) only. All other patients underwent combined brachytherapy and teletherapy. A detailed overview of the therapeutic strategies used in our clinic has been published previously [16].
The histological types of endometrial cancer in these patients were as follows: adenocarcinoma, 59.4% (n = 701); serous papillary carcinoma, 14.7% (n = 174); adenosquamous carcinoma, 9.9% (n = 128); squamous cell carcinoma, 0.4% (n = 5); missing or unclear data 14.6% (n = 172).
In a subset of 183 patients with endometrial cancer in whom the estrogen and progesterone receptor expression and the growth fraction of tumor cells (MIB1, Ki-67 antigen) had already been determined by immunohistochemistry [17], these data were also correlated with the BMI. In this subgroup, a detailed histological workup was done.
Cervical cancer
Patients with cervical carcinomas who were initially seen at our department were evaluated critically for operability. The results of clinical examination and histological report determined whether they were managed by primary surgery or by radiotherapy. After 1998, radiotherapy was generally combined with platinum-containing chemotherapy. Patients who had been treated inadvertently by simple hysterectomy received secondary radiotherapy [18].
The general treatment plan for cervical carcinoma at this institution consisted of combined brachytherapy-teletherapy as follows: 2 × 10 Gy (surface dose) high-dose-rate afterloading to vaginal wall and 45 (−51) Gy by biaxial cobalt-60 pendulum irradiation (3 × 3 Gy/week) to the B-Line (parametria) or 46 Gy abdominal opposing fields (5 × 1.8–2 Gy/week), vaginal 50%-shield with or without paraortic chimney field by 18 MV beam. In some patients who showed a poor response to radiotherapy, the dose was increased to 60 Gy by opposing pelvic fields. Single doses were 2 Gy until the end of 1993; thereafter, they were reduced to 1.8 Gy. The histological types of carcinoma in this group of patients were as follows: squamous cell carcinoma 65.5% (n = 484), adenocarcinoma 11.5% (n = 85), carcinoma in situ 6.9% (n = 51), unclear or missing data16.1% (n = 119).
Ovarian cancer
All patients with ovarian carcinomas underwent surgery. Patients with tumors limited to the ovary (FIGO stages Ia and Ib) and low tumor grading (grades 1 and 2) received no adjuvant treatment. Patients with early disease were treated with intraperitoneal radiotherapy, using either chromic phosphate (P32) or radioactive gold and/or chemotherapy. Until 1996, we mainly used the PEC regimen (cisplatinum, 50 mg/m²; epirubicin, 60 mg/m2; and cyclophosphamide, 500 mg/m2; q28); thereafter, we used combined carboplatinum and paclitaxel. Patients with advanced-stage disease underwent chemotherapy combined with radiotherapy by open-field technique (2 × 15 Gy) before 1998. The histological types of carcinoma in these patients were as follows: serous papillary, 46.7% (n = 385); mucinous, 6.9% (n = 57); endometrioid, 7.5% (n = 62); clear cell, 1.2% (n = 10); others, missing, or unclear data, 37.6% (n = 310).
We also updated our data on an established group of 221 patients with invasive ovarian carcinomas. Their tumors were investigated immunohistochemically for various biological factors [19–22]. These factors included the following: the steroid hormone receptors of estrogen (ER) and progesterone (PR); the tumor markers, CA125, CA153, and CEA; angiogenesis by CD31; the tumor growth fraction by Ki-67 antigen/MIB1; the bcl-2 and c-erbB-2 oncoproteins and fibronectin. In this subgroup of patients, a detailed histological workup was undertaken.
Statistical analysis
SPSS software for Windows™, release 14.01, was used for data management and statistical analyses (bivariate correlation, cross-tabulation, Kaplan-Meier survival analyses, Kaplan-Meier multifactorial residual survival analyses, and Cox regression). A probability of error less than 5% was regarded as significant.
Ethical approval
The project was approved by the ethics committee of the Justus-Liebig-University, Giessen, on May 22nd, 2007 (application number 79/07).
Results
Endometrial cancer
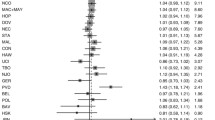
The strength of the established prognostic factors, tumor stage and histological grading, were confirmed (log rankstage = 221.2, df = 9, p < 0.001; log rankgrading = 70.6, df = 2, p < 0.001). Bivariate correlations showed that obese patients were likely to be younger (r age = −0.152, p < 0.001), to be diagnosed when their tumors were less advanced (r stage = −0.111, p = 0.001), and to have tumors that were well differentiated (r grading = −0.072, p = 0.010). Kaplan-Meier survival analysis showed that a high BMI had a favorable influence on overall survival (log rank = 15.3, df = 4, p = 0.004; Fig. 1). Kaplan-Meier multifactorial residual survival analysis incorporating age, tumor stage, and grading confirmed the independent prognostic value of BMI (log rank = 9.53, df = 4, p = 0.049; p beta < 0.001; R = 0.497; Fig. 2). The Cox Proportional Hazard model showed a strong trend (Table 2). A linear association between overall survival and BMI was found.
In the subset of 183 patients with endometrial cancer, we found no correlation between BMI and the expression of the estrogen and progesterone receptors or the tumor growth fraction.
Cervical cancer
The established prognostic factors, tumor stage and histological grading, were confirmed (log rankstage = 180.9, df = 10, p = 0.001; log rankgrading = 10.4, df = 2, p = 0.006). Bivariate correlations showed that obese patients were likely to be older (r = 0.168, p < 0.001). BMI had no influence on tumor stage, tumor grading, or histological type. Kaplan-Meier survival analysis showed that patients with a higher BMI had a better prognosis (Fig. 3; log rank = 11.1, df = 4, p = 0.026). Kaplan-Meier multifactorial residual survival analyses incorporating tumor stage and grading showed only a trend toward improved survival of obese patients and confirmed the prognostic value of BMI (p = 0.088; function of the regression model p beta < 0.001; R = 0.345). However, in the Cox Proportional Hazard model a significant favorable influence was found (Table 3).
Ovarian cancer
In the group of 824 ovarian carcinoma patients, the established prognostic factors, tumor stage and tumor grading, proved to be highly significant (log rankstage = 214.3, df = 9, p < 0.0001; log rankgrading = 59.9, df = 2, p < 0.001). Correlations between BMI and the patients’ age, tumor stage, tumor grading, and histological type showed only a weak relationship between BMI and the patients’ age at diagnosis (r = 0.095, p = 0.007). Cross-tabulation showed no influence of BMI on the histological tumor type. Kaplan-Meier survival analysis using the BMI categories of the German Society for Nutrition did not reveal a significant result. When we split the collective at the BMI value of 25 kg/m², we found a trend toward improved survival in obese patients (log rankstage = 3.74, df = 1, p = 0.053; Fig. 4). Restricting this analysis to patients with serous histology reveals a similar Kaplan-Meier survival curve; however, the result is not statistically significant. When the analysis was restricted to patients with various tumor stages with and without postoperative tumor residuals or patients with and without evidence of disease after completion of primary treatment, no significant results were found. Overall survival of patients, independent of tumor-associated deaths (birth until death, diagnosis of ovarian cancer until death), also showed no significant influence of obesity.
In a more detailed analysis of the subgroup of 221 cases, we correlated patients’ BMI with various molecular factors. Tumor growth fraction and angiogenesis, expression of ER, PR, bcl-2, c-erb-B2, and fibronectin as well as CA-125, CA15–3, and CEA showed no correlation with BMI, except for the expression of c-erb-B2 in tumor cells of obese patients, which was found less frequently (r = −0.142; p = 0.039). In this subgroup, multifactorial residual Kaplan-Meier analysis, incorporating all relevant prognostic factors including postoperative residual mass and treatment outcome, showed no adverse effect of obesity.
Discussion
Our analysis showed that the BMI has no adverse influence on poor prognostic factors or prognosis in patients with endometrial, cervical, and ovarian carcinomas. In contrast, it showed a weak but significant advantage in survival affects in obese patients. Interestingly, the impact of age, tumor stage, and grading differ in patients with endometrial and cervical cancer. While obese patients with endometrial cancers tend to be younger, the opposite seems to be true for those with cervical cancer. A comparison of the results shows that the favorable effects of obesity are more pronounced in patients with endometrial cancer and cervical but least evident in those with ovarian cancer.
The retrospective design of this study has imposed some limitations. Not all cofactors (e.g., residual tumor mass in the case of ovarian cancer) could be analyzed in all cases in the groups. Furthermore, few lymphadenectomies were undertaken, especially in the older patients, and this could have led to an underestimation of tumor stages. However, our study has other important strengths. Our institution was the only one offering chemotherapy and radiotherapy in the region of Giessen for large parts of the study period; thus, selection bias was low. The follow-up of patients, which is crucial for Kaplan-Meier survival analyses, was done very thoroughly at our institution. In general, routine assessments of survival status were completed every year and these assessments also tried to ascertain the exact causes of death. It has also been shown that retrospective analyses may well be able to determine the extent and quality of treatment effects [23]. In addition, the present study is of great interest since it is, to our knowledge, the first detailed analysis of the influence of BMI on tumor biology, and, in particular, on cervical cancer where we succeeded to prove that high BMI may also be an independent favorable prognostic factor.
Since the correlation coefficients with BMI are low, the better differentiation and lower stages of endometrial carcinomas may only partially explain the more favorable prognosis of obese patients. These findings agree with those in earlier studies [12, 13, 24]. However, we have shown that BMI is a prognostic factor that is independent of age, tumor stage and grading in one of two multifactorial analyses. Temkin et al. [13] did not succeed with this, but it may result from the fact that our study group is almost three times larger.
It seems that the at least partially hormonally responsive ovarian carcinomas do not differ from other tumor entities regarding the influence of obesity on survival that has previously been suggested in smaller and less comprehensive studies [15, 25]. Regarding the histological tumor type, our data agree with those of other workers, who found no relationship between tumor type and BMI or fat intake [26, 27]. When we analyzed various molecular factors in ovarian carcinomas, we found that only the tumor expression of c-erb-B2 was significantly less likely in obese patients. Since c-erb-B2 expression is associated with more advanced stages of ovarian cancer [28], obesity alone may not represent a negative prognostic factor.
In general, a higher BMI has proved to be a favorable prognostic factor in many tumor entities, including ovarian cancer, gastric cancer, esophageal cancer, and clear cell renal cell carcinoma [14, 29–31]. Apart from the possible influences of obesity on tumor biology, obese patients definitely have better nutritional resources to withstand longer the problems associated with metastatic disease and tumor cachexia [32]. This finding also corresponds well with the fact that early nutritional interventions and parenteral nutrition have a positive influence on the survival of cancer patients [33]. There are a few exceptions to this general rule, but these still need to be explained. For example, in breast cancer, some studies and our own unpublished data show that obese patients have a significantly poorer prognosis [34, 35]. However, underweight patients are known to have a poorer prognosis as well [36].
Obesity is associated with overproduction of steroid hormones that increases the incidence of ovarian and endometrial cancer. However, its role in the incidence of cervical cancer still remains to be defined. It has been shown that tumor-inducing factors may exert different roles in relation to tumor incidence and the course of disease. Examples of this are BRCA1 mutations, which lead to a higher incidence of ovarian cancer but are linked with a better prognosis [37, 38], and parity, which reduces the incidence of ovarian cancers but worsens the patients’ prognosis [39, 40]. This paradox has been explained by the threshold model, which suggests that under the influence of cancer-promoting factors the development of disease takes less time, fewer gene mutations and leads to more tumors. In the case of the tumor, however, it is probably more aggressive than that which develops in a regular situation and under the influence of protective factors [39].
In conclusion, obese patients do not seem to have a poorer prognosis than their nonobese counterparts in cases of carcinomas of the uterus or the ovary. We found some evidence that the opposite may be true, which raises the question of whether lean patients with gynecological cancers and advanced disease should be advised to gain some weight to improve their survival chances in case of recurrence. However, patients with a favorable prognosis are well advised to normalize their weight to avoid the well-known negative general consequences of obesity.
References
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM (2006) Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 295:1549–1555
Haenle MM, Brockmann SO, Kron M et al (2006) for the EMIL-Study group. Overweight, physical activity, tobacco and alcohol consumption in a cross-sectional random sample of German adults. BMC Public Health 6:233
Douketis JD, Sharma AM (2005) Obesity and cardiovascular disease: pathogenic mechanisms and potential benefits of weight reduction. Semin Vasc Med 5:25–33
Calle EE, Thun MJ (2004) Obesity and cancer. Oncogene 23:6365–6378
Olsen CM, Green AC, Whiteman DC, Sadeghi S, Kolahdooz F, Webb PM (2007) Obesity and the risk of epithelial ovarian cancer: a systematic review and meta-analysis. Eur J Cancer 43:690–709
Bray F, Dos Santos Silva I, Moller H, Weiderpass E (2005) Endometrial cancer incidence trends in Europe: underlying determinants and prospects for prevention. Cancer Epidemiol Biomarkers Prev 14:1132–1142
Wee CC, Phillips RS, McCarthy EP (2005) BMI and cervical cancer screening among white, African-American, and hispanic women in the United States. Obes Res 13:1275–1280
Alexander CI, Liston WA (2006) Operating on the obese woman—a review. BJOG 113:1167–1172
von Gruenigen VE, Tian C, Frasure H, Waggoner S, Keys H, Barakat RR (2006) Treatment effects, disease recurrence, and survival in obese women with early endometrial carcinoma: a Gynecologic Oncology Group study. Cancer 107:2786–2791
Erkanli S, Kayaselcuk F, Bagis T, Kuscu E (2006) Impact of morbid obesity in surgical management of endometrial cancer: surgical morbidity, clinical and pathological aspects. Eur J Gynaecol Oncol 27:401–404
Everett E, Tamimi H, Greer B, Swisher E, Paley P, Mandel L, Goff B (2003) The effect of body mass index on clinical/pathologic features, surgical morbidity, and outcome in patients with endometrial cancer. Gynecol Oncol 90:150–157
McCourt CK, Mutch DG, Gibb RK et al (2007) Body mass index: Relationship to clinical, pathologic and features of microsatellite instability in endometrial cancer. Gynecol Oncol 104:535–539
Temkin SM, Pezzullo JC, Hellmann M, Lee YC, Abulafia O (2007) Is body mass index an independent risk factor of survival among patients with endometrial cancer? Am J Clin Oncol 30:8–14
Münstedt K, von Georgi R, Franke FE (2007) Effect of obesity on survival in epithelial ovarian cancer. Cancer 109:811–812
Pavelka JC, Brown RS, Karlan BY et al (2006) Effect of obesity on survival in epithelial ovarian cancer. Cancer 107:1520–1524
Vahrson H (1991) Die Strahlentherapie des Korpuskarzinoms. In: Künzel W, Kirschbaum M (eds) Giessener Gynäkologische Fortbildung 1991. Springer, Berlin, Heidelberg, New York, pp. 163–179
Brohn S, Kullmer U, Knoblauch B, Adam K, Münstedt K (2004) Prognosefaktoren des Endometriumkarzinoms—Ein Vergleich klinischer und immunhistochemisch bestimmter Parameter. Geburtsh Frauenheilk 64:618–622
Münstedt K, Johnson P, von Georgi R, Vahrson H, Tinneberg H-R (2004) Consequences of inadvertent, suboptimal primary surgery in carcinoma of the uterine cervix. Gynecol Oncol 94:515–520
Münstedt K, Steen J, Knauf AG, Buch T, von Georgi R, Franke FE (2000) Steroid hormone receptors and long term survival in invasive ovarian cancer. Cancer 89:1783–1791
von Georgi R, Franke FE, Münstedt K (2003) The influence of tumorbiology, surgery, and postoperative therapy on patient prognosis in advanced ovarian carcinomas. Eur J Obstet Gynecol Reprod Biol 111:189–196
Franke FE, von Georgi R, Zygmunt M, Münstedt K (2003) Association between fibronectin expression and prognosis in ovarian carcinoma. Anticancer Res 23:4261–4268
Münstedt K, von Georgi R, Franke FE (2004) Correlation between MIB1-determined tumor growth fraction and incidence of tumor recurrence in early ovarian carcinomas. Cancer Invest 22:185–194
Benson K, Hartz AJ (2000) A comparison of observational studies and randomized, controlled trials. N Engl J Med 342:1878–1886
Gates EJ, Hirschfield L, Matthews RP, Yap OW (2006) Body mass index as a prognostic factor in endometrioid adenocarcinoma of the endometrium. J Natl Med Assoc 98:1814–1822
Kjaerbye-Thygesen A, Frederiksen K, Hogdall EV et al (2006) Smoking and overweight: negative prognostic factors in stage III epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev 15:798–803
Lacey JV Jr, Leitzmann M, Brinton LA et al (2006) Weight, height, and body mass index and risk for ovarian cancer in a cohort study. Ann Epidemiol 16:869–876
Parazzini F, Chiaffarino F, Negri E et al (2004) Risk factors for different histological types of ovarian cancer. Int J Gynecol Cancer 14:431–436
Harlozinska A, Bar JK, Sobanska E, Goluda M (1998) Epidermal growth factor receptor and c-erbB-2 oncoproteins in tissue and tumor effusion cells of histopathologically different ovarian neoplasms. Tumour Biol 19:364–373
Alici S, Kaya S, Izmirli M, Tuncer I, Dogan E, Ozbek H, Sayarlioglu H (2006) Analysis of survival factors in patients with advanced-stage gastric adenocarcinoma. Med Sci Monit 12:CR221–CR229
Lecleire S, Di Fiore F, Antonietti M et al (2006) Undernutrition is predictive of early mortality after palliative self-expanding metal stent insertion in patients with inoperable or recurrent esophageal cancer. Gastrointest Endosc 64:479–484
Parker AS, Lohse CM, Cheville JC, Thiel DD, Leibovich BC, Blute ML (2006) Greater body mass index is associated with better pathologic features and improved outcome among patients treated surgically for clear cell renal cell carcinoma. Urology 68:741–746
Van Cutsem E, Arends J (2005) The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs 9(suppl 2):S51–S63
Shang E, Weiss C, Post S, Kaehler G (2006) The influence of early supplementation of parenteral nutrition on quality of life and body composition in patients with advanced cancer. J Parenter Enteral Nutr 30:222–230
Abrahamson PE, Gammon MD, Lund MJ et al (2006) General and abdominal obesity and survival among young women with breast cancer. Cancer Epidemiol Biomarkers Prev 15:1871–1877
Carmichael AR (2006) Obesity and prognosis of breast cancer. Obes Rev 7:333–340
Marret H Perrotin F, Bougnoux P et al (2001) Low body mass index is an independent predictive factor for local recurrence after conservative treatment for breast cancer. Breast Cancer Res Treatment 66:17–23
Ramus SJ, Fishman A, Pharoah PD, Yarkoni S, Altaras M, Ponder BA (2001) Ovarian cancer survival in Ashkenazi Jewish patients with BRCA1 and BRCA2 mutations. Eur J Surg Oncol 27:278–281
Narod SA, Sun P, Ghadirian P et al (2001) Tubal ligation and risk of ovarian cancer in carriers of BRCA1 or BRCA2 mutations: a case-control study. Lancet 357:1467–1470
von Georgi R, Schubert K, Franke FE, Münstedt K (2002) Auswirkungen soziomedizinischer Risikofaktoren auf den Verlauf des Ovarialkarzinoms. Dtsch Med Wochenschr 127:2001–2005
Modan B, Hartge P, Hirsh-Yechezkel G et al (2001) For the National Israel Ovarian Cancer Study Group. Parity, oral contraceptives, and the risk of ovarian cancer among carriers and noncarriers of a BRCA1 or BRCA2 mutation. N Engl J Med 345:235–240
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Münstedt, K., Wagner, M., Kullmer, U. et al. Influence of body mass index on prognosis in gynecological malignancies. Cancer Causes Control 19, 909–916 (2008). https://doi.org/10.1007/s10552-008-9152-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-008-9152-7