Abstract
The objective of this research was to compare the association of birthweight alone with gender-specific birthweight-for-gestational age on childhood cancer risk in a large population-based case–control study in Germany. Incident cases of childhood cancer (n = 2,024, diagnosed 1992–1994) were ascertained from the German Childhood Cancer Registry. Controls were randomly drawn from population registries. Parents reported risk factor information in a mailed questionnaire and telephone interview. The odds ratio for acute lymphoblastic leukemia (ALL) was 1.41 (95% confidence interval 1.08–1.84) in the high-birthweight category (>4 kg) and was 1.45 (1.07–1.97) in the large-for-gestational age (LGA) category compared to the normal birthweight (2.5–4 kg) and the appropriate-for-gestational age (AGA) categories, respectively. However, the agreement between the birthweight and birthweight-for-gestational age was only moderate. Subgroup analyses revealed elevated odds ratios for ALL and CNS tumors in first born’s who were LGA but of normal birth weight. Thus, two findings from this post-hoc analysis are worthy of note: (1) the use of birthweight-for-gestation age categories within birthweight sub-groups potentially identified new high-risk groups among firstborns for ALL tumors and among all children for CNS tumors; and (2) although the magnitudes of risk estimators for ALL were comparable in the traditional high-birthweight group and in the LGA, the same children were not jointly classified in the same newborn categories indicating two potentially different subsets of children at risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the past two decades, several studies have identified an association between high birthweight (>4,000 g) and risk of certain childhood cancers [1–3]. In a meta-analysis in 2003, a summary estimator of 26% increased risk for childhood acute lymphoblastic leukemia (ALL) was reported for the high birthweight compared to the newborns weighing <4,000 g [4]. High birthweight is one of the few established risk factors for Wilms’ tumor [5], while the evidence for an association between high birthweight and childhood brain tumors, particularly astrocytoma, may be somewhat weaker than for Wilms’ tumor [1, 6]. For other childhood cancers, results from epidemiological studies are equivocal [1].
The cutoff for high birthweight is 4,000 g and corresponds to a higher rate of distocia and difficult deliveries in large neonates [7]. Newborns weighing ≥4,500 g, not 4,000 g, are at increased risk for infant mortality [8]. Kramer et al. describe an increasing mean birthweight over time among neonates born ≥ 37 weeks gestation, who are classified as appropriate- (AGA) or large-for-gestational age (LGA) (AGA: between the 10th through the 90th percentiles and LGA: at >90th percentile of the gender-specific birthweight distribution within each gestational age in weeks respectively) [9, 10]. Moreover, the percentage of women who are overweight or obese before pregnancy and the rates of weight gain in pregnancy have increased over the time similar to the trend in larger fetal size [9]. Several decades before Kramer’s research, Yerushalmy [11] first proposed a birthweight for gestational age algorithm as a potentially more sensitive predictor of mortality in neonates. Yerushalmy compared infant mortality rates in the low birthweight at <2,500 g with rates in the <10th percentile of the gender-specific birthweight for gestational age in weeks (i.e., small-for-gestational age (SGA)), because not all low birthweight newborns were at greater risk of death than heavier newborns. Yerushalmy found the SGA were at higher risk of mortality than the low-birthweight group.
The Yerushalmy paradigm might provide a potentially powerful tool to define infants at risk of childhood cancers than birthweight alone. In this paper, we examine data from a large-scale case–control study of childhood cancer etiology conducted in Germany between 1992 and 1997 [12], to contrast the association between birthweight-for-gestational age and childhood cancer risk with the association of the traditional cutoffs for low and high birthweight and childhood cancer.
Materials and methods
This population-based case–control study includes all cases of acute leukemia (acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML)), Non-Hodgkin’s lymphoma (NHL), tumors of the central nervous system (CNS), neuroblastoma, nephroblastoma, soft tissue sarcoma, or bone tumor in children aged ≤ 14 years who lived in West Germany at the age of diagnosis. Case ascertainment was performed by the nationwide German Childhood Cancer Registry (GCCR) at the University of Mainz, which is estimated to be more than 95% complete [13]. Incident cases were eligible, if their disease was diagnosed between October 1992 and September 1994. For each case, one control matched on gender, date of birth within one year, and community was randomly selected from complete files of local resident registration offices. If a control family could not be traced or refused to participate, a substitute family was sampled. An additional criteria for inclusion of cases and controls was that children, who were older than one year of age at diagnosis or the reference date, must have lived in the respective community for at least half a year. Because this criterion could be checked only after recruitment of participants, 3.4% of families who had already agreed to participate were excluded. More details about the study methodology have been published elsewhere [12].
Information on potential risk factors was collected by both self-administered questionnaire and subsequent telephone interview with parents. The questions about birthweight, gestational age, parental smoking, number and birth dates of siblings and of the parents were on the postal questionnaire. Socioeconomic status of a family was based on parental education, occupational training, and average monthly family net income as reported in the telephone interview. The fieldwork for the study was conducted from October 1992 until the end of 1997.
The calculations of SGA with the cutoff at <10th percentile, AGA from the 10th through the 90th percentiles, and LGA with the cut-off at >90th percentile were based on gender-specific percentiles for birthweight by gestation age in weeks from a large German birth cohort [14]. The SGA, AGA, and LGA were calculated for all 563,480-singleton live births in West Germany in 1992. A second survey of 80,000 twins born in Germany between 1990 and 1995 provided data to calculate SGA, AGA, and LGA for multiple births [15].
Statistical methods
Odds Ratios (OR) and 95 percent confidence intervals (95% CI) were computed by conditional logistic regression analysis for frequency-matched data sets, using Proc Phreg of SAS 6.1.2 [16]. With this approach, each diagnostic-specific model always included the total control group for comparison, regardless of an individually matched partner [17]. The frequency-matched logistic regression model was stratified by gender and age (groups of one year), resulting in strata of m:n matched cases and controls for the calculation of conditional maximum likelihood given the explanatory variables gender and age. Additional adjustments were made for degree of urbanization (urban, rural, mixed urban-rural) and for socioeconomic status (high, other).
Odds ratios were calculated for both the whole group and for singletons alone (but not separately for the small number of multiple births). In the tables presented in this manuscript, results are presented for singletons, although the results did not substantially differ with inclusion of multiple births (data not shown). Multiple gestations may be the result of infertility treatments, which can alone or via an inherited trait from a woman who had a history of subfecundity, place offspring at greater risk of cancer. In addition, the in utero environment for multiple gestations differs from that of singletons’, sufficiently so to justify the presentation of results for singletons alone. As Down’s syndrome is associated with a greatly increased risk of several childhood cancers and leukemia in particular, children with Down’s syndrome were excluded from the analysis [1]. In the model of birthweight and gestational age, the data were stratified by birth order (first versus later born) because growth factors and birthweight vary by parity [1].
The agreement between birthweight and birthweight-for-gestational age was evaluated with the kappa statistic [18]. The kappa statistic quantifies the extent of agreement beyond the expected level of agreement from chance alone. Kappa values range from 1 (perfect agreement), 0 (no agreement) to −1 (perfect disagreement), with values around 0.5 representing fair agreement. To be consistent, we excluded the same subjects from this analysis as from the risk analyses (including multiple births) and applied the same categorization for birthweight and birthweight-for-gestational age.
Results
In the 2,346 eligible families of childhood cancer patients, 60 (2.6%) were not contacted due to the physician’s preference. Of the remaining 2,286 contacted case families, 1,938 (84.8%) returned the questionnaire. Since specific eligibility criteria could only be checked from the questionnaire, certain participants were excluded a posteriori leaving 1,867 childhood cancer patients for analyses (see “Methods”). Among families of healthy control children, 2,126 (70.9%) of 2,998 eligible families returned the questionnaire and 2,057 fulfilled the eligibility criteria. Furthermore, we excluded cases and controls with trisomy 21, multiple births and subjects for whom birthweight and/or gestational age were not available (Table 1).
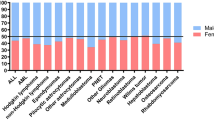
Since more control than case families were high SES, all analyses were adjusted for SES (Table 1). The mean birthweight was 3,417 g (95% CI 3,394–3,441) in all controls compared to 3,427 g (95% CI 3,401–3,454) in all childhood cancer patients. In the healthy controls, 86% were normal birthweight (2,500–4,000 g), three percent were low birthweight (<2,500 g) and the remaining 11% high birthweight (>4 kg). Using the birthweight-for-gestation age algorithm, 80% of all controls were AGA, 11% SGA, and 8% LGA. The differences in mean birthweight across childhood cancer diagnostic groups were minor. Finally, among controls, the percent high birthweight was higher in boys than girls (15% vs. 9%), children of nonsmoking mothers compared to mothers who smoked (14% vs. 7%), birth order of two or higher compared to firstborns (16% vs. 9%), and older mothers (13% vs. 10% vs. 2% for age groups ≥ 30 years, 20–29 years, and <20 years at delivery).
In a comparison of the adjusted ORs of childhood cancers for SGA and LGA to the AGA as well as a comparison of low and high birthweight to the normal birthweight, the LGA had a higher risk ranging from 18% to 57% for ALL, AML, NHL, CNS tumors, neuroblastoma, and nephroblastoma, with a statistically significantly higher odds for ALL. The higher risk in the high-birthweight ranged from 34 % to 65 % for the same set of cancer diagnostic groups, except the bone tumor patients also experienced a higher risk in the high birthweight, not the LGA, and the NHL experienced a higher risk in the LGA only. In contrast, no significant associations were seen for SGA; indeed when an elevated OR appeared in the SGA, the magnitudes were much lower than the ones observed in the low birthweight even though the number of cases and controls who were SGA were larger than the number of low birthweight. The adjusted ORs of all case groups were elevated in the low birthweight, with a significantly higher OR for NHL. Also, there were four childhood cancer groups in which the OR for SGA was below one and, therefore, in the opposite direction than for low birthweight, notably AML, CNS tumors, nephroblastoma, and bone tumors.
Birth order, maternal smoking during pregnancy and maternal age at delivery were considered potential confounders, because a woman in her first pregnancy has higher hormone-levels than in subsequent pregnancies (in particular, estrogen and its metabolites are correlated with pregnancies in a woman [19]) and maternal age is correlated with parity [20]. Higher insulin-growth factor-1 levels were higher in cord blood of infants who later developed childhood cancer than healthy controls [21]. Maternal smoking is assumed to be a risk factor for certain childhood cancers and maternal smoking is known to be associated with a lower birthweight [1]. Thus birth order, maternal smoking and maternal age were tested as confounding factors by inspecting the changes in the risk estimates. Adjustment for these factors marginally changed the results (data not shown), thus, we kept the final statistical model in Table 2 as simple as possible. For ALL, we examined risk by age group, but did not see any clear pattern. The association with high birthweight was slightly stronger in the youngest children (up to two years of age at diagnosis) compared to the two ≤ six years old and 6+ years old children, however, the odds ratios were 1.64, 1.33, and 1.41 and the confidence intervals fully overlapped. With respect to LGA, odds ratios were 1.12, 1.38, and 1.59 for the same three age groups, so the trend was reverse, but again the differences were in line with random variation.
Since the magnitude of the odds ratios for LGA and high birthweight were similar, we examined the extent to which birthweight and birthweight for gestational age were related. Among the controls, 63% of the high birthweight newborns were LGA, while 84% of LGA babies had a high birthweight. The agreement between the two measures was fair, as shown by a kappa of 0.44 (95% CI 0.39–0.49). Among ALL patients, the respective figures were 62% and 81%, with a kappa of 0.45 (95% CI 0.37–0.53). Hence, as there were differences in the proportion of newborns who were classified by birthweight alone versus birthweight for gestational age, we examined the following exposure categories: LGA babies who were classified as normal or low birthweight; heavy babies (>4 kg) who were not categorized as LGA; and LGA babies who weighed >4 kg at birth. Since ALL and CNS tumor patients had large sample sizes, the risk estimates were calculated separately for firstborn versus children of higher birth order (Table 3). An over five-fold higher odds of ALL was observed in first, but not later born children, who were categorized as LGA, weighing ≤ 4 kg, compared to the first born who were AGA ≤4 kg. A similar pattern to that observed for ALL, was seen for CNS tumor patients who were first-born, but the 95% CI included one. Those born LGA and weighing >4 kg had a 40% elevated odds ratio of ALL. Finally for all the CNS tumor patients, who were high birthweight, but not LGA, their odds ratios were elevated by 81% compared to the AGA, ≤4 kg.
In a trend analysis for every 100 g of additional birthweight in those weighing ≥ 4 kg at birth, the odds of ALL increased by 5% (95% CI 0.99–1.12), compared to a referent of birthweight ranging from 2.5 kg to 4 kg. For CNS tumors, the respective figure was 1.00 (95% CI 0.93–1.09). Gender-specific analysis revealed slightly stronger associations between high birthweight and risk of ALL for boys than for girls, but this difference was within random variation (data not shown).
Discussion
In a large population-based case–control study of childhood cancer, the association of birthweight alone was compared with gender-specific birthweight-for-gestation age categories on risk of cancer. Children who were high birthweight or LGA had a 41–45% higher adjusted odds of ALL compared to the normal birthweight and the AGA, respectively, but 16% of LGA babies were not classified high birthweight and 36% of the heavy babies were not classified as LGA among the controls. A similar proportion of the ALL cases, to the controls, were not jointly classified in both categories of large newborns. In a trend analysis, 100 g increments in birthweight increased the odds of ALL, but not CNS tumors. Children who were low birthweight had over a 2 ½ fold higher adjusted odds of NHL, but no association was observed in the SGA even though 11% and 13% of the NHL patients and controls were SGA, respectively. Since there were differences in the proportion classified by birthweight alone in contrast with birthweight-for-gestation age, we examined the effects of the two factors in one analysis model. When we examined risk by birthweight and birthweight-for-gestation age categories in the first born, the LGA who were ≤4 kg at birth had a 5.2-fold higher odds of ALL compared to the AGA weighing ≤4 kg. In CNS tumor patients, those who weighed >4 kg but were not LGA had an 80% higher odds than those who weighted ≤4 kg. Thus, two results of this post-hoc analysis are worthy of discussion: notably, the use of birthweight-for-gestation age categories within birthweight subgroups potentially identified a new high risk group among firstborns for ALL and for all CNS tumor patients; and the magnitude of the odds ratios for the traditional high birthweight group and the LGA were similar for ALL but the same children were not jointly classified in the large newborn categories.
The largest ORs appeared for ALL in the newborns who were LGA, but not high birthweight, and who were first rather than later born children. These newborns would not have been identified using the traditional cut-offs for birthweight alone. The large size of these newborns compared to those born in the same gestational weeks might be due to a higher fetal growth rate [9]. Their fetal growth rate occurred relative to a modestly increasing mean birthweight for the AGA, i.e., the referent group. The work of Lof et al. and of Chellakooty et al. demonstrated an association of maternal basal metabolic rate and IGF-1 levels in larger fetal size [22, 23]. Insulin-like growth factor 1 (IGF-1) is a mitotic hormone and is antiapoptotic [21] and has been proposed to have a role in the relation of large newborn size and childhood cancer [2]. The elevated risk in ALL patients who are first rather than later borns may or may not reflect the combination of larger fetal size and later exposure to infectious pathogens incurred more frequently in the first born child [24].
The 80% elevated OR for CNS tumors in those weighing > 4 kg but not LGA might not be due to the same mechanisms as in ALL patients, because the OR was not appreciably different from the null with 100 g increments of birthweight in the trend analysis. In the CNS tumors, regulators of embryonic brain development, like Twist a transcription factor responsible for closing the neural tubes and migration of neural crest cells, might remain upregulated in the presence of IGF-1 [25–27]. Indeed Twist is overexpressed in human pediatric osteosarcomas, in N-Myc-amplified neuroblastomas to override the p53 pathway, and is a target of transcriptional deregulation in experimental nephroblastoma [28–30]. Other potential candidates for a similar role are members of the Snail and Slug family genes that enhance carniosynostosis associated with Saethre-Chotezen Syndrome [31, 32].
The strength of the German case–control study is its population base. Cases were ascertained by a nationwide cancer registry and controls were sampled from population registries. Given the overall participation rates of 85% for cases and 71% for controls, we adjusted for factors that were associated with control participation, particularly SES and parental age, wherein controls had fewer families of lower SES and families of younger ages [33]. Also parental recall of early life exposures were more detailed in parents of patients than in parents of healthy control children as described earlier [34]. Hence, potential effects of selection bias and recall bias, which are joint drawbacks of all questionnaire-based case–control studies [35], have to be mentioned in the context of the results. Finally, our birth-order specific findings are based on small subgroups and may be a chance finding. It needs to be stressed that our present analysis is a post-hoc analysis of existing study material and no new data were gathered [12], thus, the results may be valid but could have arisen by chance. Consequently, the results should rather be regarded as hypothesis generating. We are currently involved in a similar analysis of birthweight-for-gestational age in an international pooling project of childhood ALL.
In a previous case–control study on childhood cancer in Germany, we compared birthweights abstracted from obstetric records with those reported by parents [36]. The same questionnaire was used in the latter and the current study [37]. Of 633 subjects with data from parental-reported and record abstraction, only 69 (11%) had a birthweight difference of more than 100 g. After categorization at <2.5 kg and >4 kg, the agreement between the data sources revealed a kappa of 0.95 (95% CI 0.92–0.98). A very good agreement for birthweight was also observed in a similar U.S. study [38]; thus the validity of maternal-reported birthweight is high. Because data on gestational age is likely to be less accurate, as demonstrated by a kappa of 0.6 in a US study [38], recall bias may play a role in our birthweight-by-gestational age analysis.
The distribution of birthweight from the birth registry of the University of Mainz was compared to the distribution in our control group [39]. Although this birth registry covers part of our study region, it is appropriate for a comparison, since substantial regional variation in birthweight has not been identified in West Germany [14, 39]. From this registry, we calculated the birthweight distribution by weeks of gestation for all singleton live births of children born in 1990–1992. The rates of low birthweight (i.e., <2.5 kg) over the same birth years were 6.0% (95% CI 5.6%–6.5%) in the registry and 3.2% (95% CI 1.8%–4.6%) in singleton births of our control group. Likewise, the percent of short pregnancies (<37 weeks) of singleton births in our control group was 3.4% (95% CI 1.9%–4.8%) compared to 6.4% (95% CI 5.9%–6.8%) in the birth registry cohort. For high birthweight (>4 kg), on the other hand, the prevalence rates of the two groups were similar, notably 10.4% (95% CI 9.8%–11.0%) in the birth registry cohort and 11.7% (95% CI 9.2%–14.2%) in our control group. In contrast, the rate of high birthweight was 17.0% (95% CI 12.2%–21.7%) among the ALL singletons born 1990–1992. Thus, these data indicate that our associations of low birthweight and childhood cancer risk are likely to be biased, while it strengthens the plausibility of our findings for high birthweight.
In conclusion, in a large population-based case–control study of childhood cancer, children who were high birthweight or LGA had a 41–45% higher adjusted odds of ALL compared to the normal birthweight and the AGA, respectively, thus, the results are similar to those from a 2003 meta-analysis on birthweight and ALL risk [4]. When we examined risk by birthweight and birthweight-for-gestational age categories in the first born, the LGA who were ≤4 kg at birth had a 5.2 fold higher odds of ALL compared to the AGA weighing <4 kg. In a trend analysis, 100 g increments in birthweight increased the odds of ALL. Application of birthweight-for-gestational age categories identified new high-risk groups for ALL in LGA first-born children, who weighed ≤4 kg at birth, and in CNS tumor patients who weighed >4 kg but were not LGA. In an international pooling project, we have the opportunity to test the algorithm for ALL for evidence of consistent associations.
Abbreviations
- ALL:
-
Acute lymphoblastic leukemia
- AML:
-
Acute myeloblastic leukemia
- CNS:
-
Central nervous system
- NHL:
-
Non-Hodgkin’s lymphoma
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- AGA:
-
Appropriate-for-gestational age
- LGA:
-
Large-for-gestational age
- SGA:
-
Small-for-gestational age
References
Little J (1990) Epidemiology of childhood cancer. IARC Scientific Publications No149. Lyon, France
Ross JA, Perentesis JP, Robison LL, Davies SM (1997) Big babies and infant leukemia: a role for insulin-like growth factor-1? Cancer Causes Control 7:553–559
Hjalgrim LL, Rostgaard K, Hjalgrim H et al (2004) Birth weight and risk for childhood leukemia in Denmark, Sweden, Norway, and Iceland. J Natl Cancer Inst 96:1549–1556
Hjalgrim LL, Westergaard T, Rostgaard K et al (2003) Birthweight as a risk factor for childhood leukemia: a meta-analysis of 18 epidemiologic studies. Am J Epidemol 158:724–735
Schüz J, Kaletsch U, Meinert R, Kaatsch P, Michaelis J (2001) High birthweight and other risk factors for Wilms’ tumour: results of a population-based case-control study. Eur J Pediatr 160:333–338
von Behren J, Reynolds P (2003) Birth characteristics and brain cancers in young children. Int J Epidemiol 32:248–256
Grassi AE, Giuliano MA (2000) The neonate with macrosomia. Clin Obstetr Gynecol 43:340–348
Godfrey KM (2001) The ‘Gold Standard’ for optimal fetal growth and development. J Pedatri Endocrinol Metab 14:1507–1514
Kramer MS, Morin I, Yang H et al (2002) Why are babies getting bigger? Temporal trends in fetal growth and its determinants. J Pediatr 141:538–542
Ventura SJ, Hamilton BE, Mathews TJ, Chandra A (2003) Trends and variations in smoking during pregnancy and low birth weight: evidence from the birth certificate, 1990–2000. Pediatrics 111:1176–1180
Yerushalmy J (1967) The classification of newborn infants by birth weight and gestational age. J Pediatr 71:164–172
Schüz J, Kaatsch P, Kaletsch U, Meinert R, Michaelis J (1999) Association of childhood cancer with factors related to pregnancy and birth. Int J Epidemiol 28:631–639
Kaatsch P, Haaf G, Michaelis J (1995) Childhood malignancies in Germany- methods and results of a nationwide registry. Eur J Cancer 31A:993–999
Voigt M, Schneider KTM, Jährig K (1996) Analyse des Geburtengutes des Jahrgangs 1992 der Bundesrepublik Deutschland [Analysis of the total number of births in 1992 in the Federal Republic of Germany] (in German). Geburtshilfe Frauenheilkd 56:550–558
Voigt M, Schneider KTM, Friese K, Hesse V, Jährig K (1999) Analyse des Geburtengutes der Bundesrepublik Deutschland. Teil 3: Perzentilwerte für das Geburtsgewicht, die Geburtslänge und den Kopfumfang deutscher Zwillinge (in German). Geburtshilfe Frauenheilkd 59:346–354
Stokes ME, Davis CS, Koch GG (1995) Categorical data analysis using the SAS System. SAS Institute Inc., Cary, NC, USA
Brookmeyer R, Liang KY, Linet M (1986) Matched case-control designs and overmatched analyses. Am J Epidemiol 124:693–701
Landis JR, Koch GG (1997) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Bernstein L, Depue RH, Ross RK, Judd HL, Pike MC, Henderson BE (1986) Higher maternal levels of free estradiol in first compared to second pregnancy: early gestational differences. J Natl Cancer Inst 76:1035–1039
Bernstein L, Depue RH, Ross RK, Judd HL, Pike MC, Henderson BE (1986) Higher maternal levels of free estradiol in first compared to second pregnancy: early gestational differences. J Natl Cancer Inst 76:1035–1039
Yu H, Rohan T (2000) Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst 92:1472–1489
Lof M, Olausson H, Bostrom K, Janerot-Sjoberg B, Sohlstrom A, Forsum E (2005) Changes in basal metabolic rate during pregnancy in relation to changes in body weight and composition, cardiac output, insulin-like growth factor I, and thyroid hormones and in relation to fetal growth. Am J Clin Nutr 81:678–685
Chellakooty M, Vangsgaard K, Larsen T et al (2004) A longitudinal study of intrauterine growth and the placental growth hormone (GH)-insulin-like growth factor I axis in maternal circulation: association between placental GH and fetal growth. J Clin Endocrinol Metab 89:384–391
Greaves M (2002) Childhood leukemia. BMJ 324:283–287
Castanon I, Baylies MK (2002) A Twist in fate: evolutionary comparison of Twist structure and function. Gene 287:11–22
Kang Y, Massague J (2004) Epithelial-mesenchymal transitions: twist in development and metastasis. Cell 118:277–279
Yang J, Mani SA, Donaher JL et al (2004) Twist, a master regulator of morphogenesis, plays an essential role in tumour metastasis. Cell 117:927–939
Pajer P, Pecenka V, Karafiat V, Kralova J, Horejsi Z, Dvorak M (2003) The twist gene is a common target of retroviral integration and transcriptional deregulation in experimental nephroblastoma. Oncogene 22:665–673
Valsesia-Wittmann S, Magdeleine M, Dupasquier S et al (2004) Oncogenic cooperation between H-Twist and N-Myc overrides failsafe programs in cancer cells. Cancer Cell 6:625–630
Entz-Werle N, Stoetzel C, Berard-Marec P et al (2005) Frequent genomic abnormalities at TWIST in human pediatric osteosarcomas. Int J Cancer May 117:349–355
Oram KF, Gridley T (2005) Mutations in snail family genes enhance craniosynostosis of Twist1 haplo-insufficient mice: implications for Saethre-Chotzen Syndrome. Genetics 170:971–974
de Heer IM, de Klein A, van den Ouweland AM et al (2005) Clinical and genetic analysis of patients with Saethre-Chotzen syndrome. Plast Reconstr Surg 115:1894–1902
Schüz J (2003) Non-response bias as a likely cause for the association between young maternal age at the time of delivery and the risk of cancer in the offspring. Paediatr Perinat Epidemiol 17:106–112
Schüz J, Spector LF, Ross JA (2003) Bias in studies of parental self-reported occupational exposures and childhood cancer. Am J Epidemiol 158:710–716
Linet MS, Wacholder S, Zahm SH (2003) Interpreting epidemiologic research: lessons from studies of childhood cancer. Pediatrics 112:218–232
von Kries R, Göbel U, Hachmeister A, Kaletsch U, Michaelis J (1996) Vitamin K and childhood cancer: a population based case-control study in Lower Saxony, Germany. BMJ 313:199–203
Kaatsch P, Kaletsch U, Meinert R et al (1998) German case control study on childhood leukemia–basic considerations, methodology and summary of the results. Klin Padiatr 210:185–191
Olson JE, Shu XO, Ross JA, Pendergrass T, Robison LL (1997) Medical record validation of maternally reported birth characteristics and pregnancy-related events: a report from the Children’s Cancer Group. Am J Epidemiol 145:58–67
Queisser-Luft A, Stolz G, Wiesel A, Schlaefer K, Spranger J (2002) Malformations in newborn: results based on 30,940 infants and fetuses from the Mainz congenital birth defect monitoring system (1990–1998). Arch Gynecol Obstet 266:163–167
Acknowledgments
The authors like to thank Dr Susanne Queißer-Luft (University of Mainz) and Klaus Schlaefer (German Cancer Research Center) for providing data from the Mainzer birth registry. Furthermore, the authors like to thank Drs Peter Kaatsch and Jörg Michaelis for the provision of the data of the German case–control study to perform these additional analyses.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sponsored by the Intramural Research Program of the NIH, National Cancer Institute, and by The Danish Cancer Society. J. Schüz and M.R. Forman contributed equally to the preparation of the manuscript
Rights and permissions
About this article
Cite this article
Schüz, J., Forman, M.R. Birthweight by gestational age and childhood cancer. Cancer Causes Control 18, 655–663 (2007). https://doi.org/10.1007/s10552-007-9011-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-007-9011-y