Abstract
Aromatase inhibitors (AIs) are an effective therapy in treating estrogen receptor-positive breast cancer. Nonetheless, a significant percentage of patients either do not respond or become resistant to AIs. Decreased dependence on ER-signaling and increased dependence on growth factor receptor signaling pathways, particularly human epidermal growth factor receptor 2 (EGFR2/HER2), have been implicated in AI resistance. However, the role of growth factor signaling remains unclear. This current study investigates the possibility that signaling either through HER2 alone or through interplay between epidermal growth factor receptor 1 (EGFR/HER1) and HER2 mediates AI resistance by increasing the tumor initiating cell (TIC) subpopulation in AI-resistant cells via regulation of stem cell markers, such as breast cancer resistance protein (BCRP). TICs and BCRP are both known to be involved in drug resistance. Results from in vitro analyses of AI-resistant versus AI-sensitive cells and HER2-versus HER2+ cells, as well as from in vivo xenograft tumors, indicate that (1) AI-resistant cells overexpress both HER2 and BCRP and exhibit increased TIC characteristics compared to AI-sensitive cells; (2) inhibition of HER2 and/or BCRP decrease TIC characteristics in letrozole-resistant cells; and (3) HER2 and its dimerization partner EGFR/HER1 are involved in the regulation of BCRP. Overall, these results suggest that reducing or eliminating the TIC subpopulation with agents that target BCRP, HER2, EGFR/HER1, and/or their downstream kinase pathways could be effective in preventing and/or treating acquired AI resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inhibition of estrogen synthesis via aromatase inhibitors (AIs, i.e., letrozole, anastrozole, and exemestane) is highly effective in treating estrogen receptor-positive (ER+) breast cancer and preventing contra-lateral breast cancer [1]. A significant percentage of ER+ patients, however, either do not respond to AIs or become resistant to them during treatment [2, 3]. Previous work by our laboratory indicates that acquired AI resistance involves a switch from the dependence on ER signaling to the dependence on growth factor-mediated pathways, such as human epidermal growth factor receptor 2 (EGFR2)/HER2 and insulin-like growth factor receptor (IGFR) [2–4]. However, the mechanism by which growth factor signaling confers AI resistance remains unclear.
One possibility is that HER2 mediates expansion of the tumor initiating cell (TIC) population, as suggested in previous studies [5, 6]. TICs are a small distinct subset of cells within a heterogeneous tumor which have the ability to initiate and maintain tumor growth and to promote metastasis [7–12]. Pertinent to acquired AI resistance, TICs are known to play a role in radio- and chemo resistance [7–9], as the residual tumor cell population remaining after treatment with conventional chemotherapy or AIs exhibit a high proportion of TICs [7–9, 13–15]. The expansion of TICs or inability to eliminate them may contribute to acquire AI resistance in breast cancer.
HER2 may maintain and/or expand the TIC subpopulation within an AI-resistant tumor by regulating certain TIC effector genes, such as the breast cancer resistance protein (BCRP). BCRP maintains TICs in an undifferentiated state [13, 15]. It is also a membrane-associated transporter protein, the function of which is to efflux out various molecules from the cell, and has been linked to multi-drug chemoresistance of breast cancer cells [13, 15–17]. Furthermore, other studies have shown a correlation between BCRP and HER2 [6, 18–20] and ERα [21, 22]. Thus, the purpose of this current study was to (1) determine if the TIC subpopulation is increased in AI-resistant versus-sensitive cells; (2) analyze the TIC subpopulation in letrozole-resistant cells; (3) investigate the importance of HER2 and BCRP on the TIC phenotype in letrozole-resistant cells; (4) determine whether HER2 regulates BCRP; and (5) determine if EGFR/HER1 is also involved.
Materials and methods
Cell lines and reagents
Cell lines
Cell lines (and their ER/HER2 status) used are listed in Table 1. MCF-7Ca cells are MCF-7 cells stably transfected with the human aromatase gene (supplied by Dr. Chen, City of Hope, Duarte, CA) and maintained in DMEM 1× high glucose (Invitrogen) supplemented with 5 % fetal bovine serum (FBS), 1 % penicillin/streptomycin (P–S), and 700 μg/mL G418. Long-term letrozole-treated (LTLT-Ca) cells are letrozole-resistant cells isolated from MCF-7Ca mouse xenograft tumors treated for 56 weeks with letrozole, and maintained in phenol red-free (PRF) modified IMEM (Invitrogen) supplemented with 5 % charcoal dextran-treated FBS (CDT-FBS), 1 % P–S, 750 μg/mL G418, and 1 μM letrozole. MCF-7 cells (ATCC) were maintained in DMEM 1 × high glucose (Invitrogen) supplemented with 5 % FBS and 1 % P–S. MCF-7/HER2 cells are MCF-7 cells transfected with the HER2 gene (supplied by Ann Hambruger, University of Maryland Baltimore, UMB) maintained in DMEM 1× high glucose (Invitrogen) supplemented with 5 % FBS, 1 % P–S, and 500 μg/mL hygromycin. AC1 cells are MCF-7 cells stably transfected with the human aromatase maintained in DMEM 1× high glucose (Invitrogen) supplemented with 5 % FBS, 1 % P–S, and 800 μg/mL G418. AC1-exemestane resistant (AC1-ExR) cells are a exemestane-resistant cells isolated from AC1 mouse xenograft tumors treated for ~10 weeks with exemestane maintained in PRF modified IMEM (Invitrogen) supplemented with 5 % CDT-FBS, 1 % P–S, 800 μg/mL G418, and 5 μM exemestane.
Reagents
The following drugs were used: letrozole (Novartis); lapatinib (GlaxoSmithKline Pharmaceutical); trastuzumab (Genentech); BIBX1382 (Calbiochem); and BCRP inhibitors Ko143 and fumitremorgen C (FTC) were kindly provided by Dr. Douglas Ross (UMB). Use of Ko143 and FTC depended on availability from Dr. Ross’ laboratory. The following antibodies were used in western blot analyses: HER2 (EMD Millipore); BCRP (EMD Millipore); ERα (Santa Cruz Biotechnology); and phosphorylated and total ERK1/2 or Akt, phosphorylated and total EGFR/HER1, and β-actin (all obtained from Cell Signaling Technology).
Side population (SP) analysis
SP analysis was performed either by Hoechst 33342 assay [6, 23] or using Vibrant DyeCycle Violet stain (Invitrogen). Briefly, after drug treatment, 1 × 106 cells/mL were suspended in prewarmed IMEM with 2 % FBS and 10 mM HEPES containing 5 μg of Hoechst 33342 (Sigma) or 1 μL of DyeCycle Violet stock. Cells were incubated at 37 °C for 40 min (Dye Cycle) or 90 min (Hoechst). Cells were acquired using BD-LSRII. Data was analyzed by means of FlowJo software. Cells treated with BCRP inhibitor Ko143 were included in each SP analysis set as a control to demonstrate inhibition of dye efflux.
Aldehyde dehydrogenase (ALDH) assay
The Aldefluor assay was performed using the Aldefluor Assay kit from Stem Cell Technologies. ALDH stained cells were identified in cells by comparing the same sample with and without the ALDH inhibitor DEAB (diethylaminobenzaldehyde). Cells were acquired using BD LSRII and FACS CANTO. Data were analyzed by means of FlowJo software.
Mammosphere assay
The mammosphere assay was performed using reagents from Stem Cell Technologies according to the manufacturer’s instructions. Single cells were suspended in complete Mammocult media as per the manufacturer’s instructions and plated in ultra-low-attachment plates (Corning) at a density of 10,000–20,000 cells/mL. Media was replenished every 3 days. Mammospheres were counted after at least 7 days and up to 3–4 weeks. Spheres with a colony count of at least 50 cells were considered mammospheres.
Immunofluorescence (IF)
IF staining for Oct-4 was performed on sorted LTLT-Ca cells kept under non-adherent conditions for 2–3 days prior to cytospinning. Pelleted cells were fixed with 4 % paraformaldehyde and incubated with OCT4 antibody (Santa Cruz Biotechnology) and the corresponding fluorochrome-tagged secondary antibody (Invitrogen). Images were obtained and analyzed by means of Image J software.
RT-PCR
RNA extraction and reverse transcription (RT)
RNA was extracted and purified using the RNeasy Mini Kit (Qiagen). RNA was reverse transcribed to complementary DNA (cDNA) using 200 U of Moloney murine leukemia virus reverse transcriptase (Invitrogen) and incubating at 37 °C for 1 h.
Real-Time PCR
mRNA expression analyses were carried out by real-time PCR using a DNA Opticon system (MJ Research) and using DyNAmo SYBR green qPCR mix (New England Biolabs). Standard curves were generated by serially diluting the sample expected to have the most amount of PCR product. The yield of product for each unknown sample was calculated by applying its threshold cycle, or C(T), value to the standard curve by means of the Opticon Monitor analysis software (version 1.01, MJ Research). Values were normalized to corresponding 18S rRNA values and expressed as the fold increase relative to controls. Primers for HER2, BCRP, BMI-1, Nanog, and Twist were obtained from Sigma or Qiagen.
Growth and treatment of MCF-7Ca mouse xenograft tumors
All animal studies were performed according to the guidelines and approval of the Animal Care Committee of UMB. MCF-7Ca tumor xenografts of MCF-7Ca cells were grown in ovariectomized athymic nude mice as previously described [24]. Briefly, each mouse received subcutaneous (sc) inoculations in one site per flank of 100 μL of cell suspension containing ~2.5 × 107 MCF-7Ca cells. All mice were supplemented throughout the experiment with 100 μg/day androstenedione (Δ4A) sc 5 days/week. Δ4A is converted to estrogen by aromatase expressed in MCF-7Ca cells. Tumor growth was monitored weekly and treatments began when the tumors reached ~300 mm3. Mice were then randomly divided into either control (100 μg/day Δ4A) or letrozole (100 μg/day Δ4A + 10 μg/day letrozole) treatment groups. Letrozole and Δ4A were prepared using 0.3 % Hydroxypropylcellulose in saline solution. Mice were injected sc five times weekly with the indicated drugs. Tumors were collected at necropsy either at previously designated times (weeks 4, 8, and 16), or when tumors reached 2,000 mm3 in size.
Western blot analysis
Cells
Plated cells were washed with ice-cold PBS and then lysed with radioimmunoprecipitation (RIPA) buffer containing protease and phosphatase inhibitors (Roche) by sonication and incubation for 20 min at 4 °C. Lysed samples were centrifuged at 14,000 rpm for 20 min at 4 °C to collect protein lysates (supernatant). 10–40 μg of protein underwent 10 % SDS–polyacrylamide gel electrophoresis and transferred to a polyvinylidene difluoride membrane (Fisher Scientific). The resulting blots were probed with specific mouse or rabbit primary antibodies and either goat anti-mouse or -rabbit secondary antibodies conjugated to horseradish peroxidase (Biorad), respectively. Blots were developed using SuperSignal West Pico Chemiluminescent Substrate (Thermo Scientific). Blots that were to be re-probed were stripped with Restore Western Blot Stripping Buffer (Thermo Scientific) for 40 min at room temperature before incubation with another primary antibody.
MCF-7Ca xenograft tumors
Tumor samples were first homogenized in ice-cold DPBS containing protease inhibitors and centrifuged. The resulting tumor homogenate pellets were lysed with RIPA buffer. Tumor protein lysates were then collected and subjected to the same western blot analyses as cells.
Statistical analysis
All experiments were carried out at least 2–3 times each with replicates. Statistical analyses were performed by Student’s t test (two samples), ANOVA (3+ samples) by means of Graph Pad Prism software.
Results
Letrozole-resistant LTLT-Ca cells exhibit higher percentage of TICs compared to letrozole sensitive MCF-7Ca cells
The TIC subpopulation can be distinguished from other cells within a cancer cell population by several characteristics: (1) exclusion of Hoechst dye from cells and identification as “side population” (SP) cells [25–27]; (2) increased ALDH1 expression [28]; (3) ability to form mammospheres in culture [29]; and (4) expression of known stem cell markers, such as BCRP [13, 15, 30], Nanog [31], and BMI-1 [32]. Letrozole-resistant LTLT-Ca, derived from long-term letrozole treated MCF-7Ca xenograft tumors, and letrozole-sensitive parental MCF-7Ca cells were, therefore, compared to each other based on these TIC parameters. LTLT-Ca cells were found to have higher percentage of SP cells (9.17 ± 2.0 % LTLT-Ca vs. 0.02 ± 0.01 % MCF-7Ca, p < 0.01) and ALDH-expressing cells (3.9 % LTLT-Ca vs. 0.6 % MCF-7Ca, p < 0.01) than MCF-7Ca cells (Fig. 1a, b). LTLT-Ca cells also formed significantly more mammospheres in culture than MCF-7Ca cells (Fig. 1c, p < 0.05). Thus, letrozole-resistant LTLT-Ca cells express more TIC characteristics than parental, letrozole-sensitive MCF-7Ca cells.
Analysis of SP and ALDH in MCF-7Ca and LTLT-Ca cells. a Percentage of side population (SP) cells were analyzed in MCF-7Ca and LTLT-Ca cells by Hoechst staining and flow cytometry in the absence or presence of BCRP inhibitor Ko143. Plots show representative SP fractions as designated by polygons and quantified as percentages (n = 3 independent cell samples/group; p < 0.01). b Analysis of aldehyde dehydrogenase 1 (ALDH) by measuring the cellular fluorescence of bodipy-aminoacetate (BAAA) in the presence or absence of specific ALDH inhibitor DEAB. Plots show representative ALDH1-expressing cells, as designated by polygons and quantified as percentages (n = 3 independent cell samples/group; p < 0.05). c MCF-7Ca and LTLT-Ca cells were plated onto ultra-low-attachment plates containing mammosphere culture media. After 8 days in culture, formed mammospheres were imaged (top panel) and counted (bottom panel). Shown are representative images (top panel) and mean mammosphere counts. (Mean ± SEM, n = 9 independent cell samples/group, p < 0.05.)
The TIC subpopulation in LTLT-Ca cells was further analyzed through isolation of the highest and lowest 3–4 % ALDH1-expressing cells (Fig. 2). These were designated as ALDH1high (i.e., TICs) and ALDH1low cells, respectively, and their ALDH expression levels were confirmed by immunofluorescence (data not shown). These subpopulations were then compared for their ability to form mammospheres and their expression of known stem cell markers and HER2. As expected, ALDH1high cells formed significantly more mammospheres (164.7 ± 7.5 vs. 11 ± 1, p < 0.05; Fig. 2a) and they expressed higher levels of stem cell markers OCT-4 (as shown by immunofluorescence, Fig. 2b), BCRP, BMI-1, and Nanog (>2.5–>3.3-fold as shown by RT-PCR, Fig. 2c) compared to ALDH1low cells. In addition, ALDH1high cells expressed higher mRNA levels of TWIST, an epithelial–mesenchymal transition marker and transcription factor known to regulate BMI-1 and of HER2 (>1.3 and >2.5-fold vs. ALDH1low, Fig. 2c). HER2 overexpression in ALDH1high versus ALDH1low cells was additionally confirmed by flow cytometry (data not shown). Both HER2 and BCRP proteins were also increased in LTLT-Ca cells when compared overall to MCF-7Ca cells (Fig. 2d). These results demonstrate that the TIC population can be isolated from LTLT-Ca cells and that they express factors known to be involved in their regulation.
mRNA expression in ALDHlow and ALDHhigh LTLT-Ca cells and protein expression in LTLT-Ca versus MCF-7Ca cells. a LTLT-Ca cells were treated with aldefluor and then ALDH1low and ALDH1high cells (3–4 % lowest and highest) were sorted by fluorescence-activated cell sorting (FACS). Sorted cells were then plated under ultra-low-attachment conditions at a density of 10,000 cells/well. After ~3 weeks, formed mammospheres were counted. A representative graph of the average number of formed mammospheres (n = 3; p < 0.01) is shown. b ALDH1low- and ALDH1high-expressing LTLT-Ca cells were subjected to immunofluorescence with Oct-4 antibody (red) and DAPI nuclear stain (blue). Shown are representative immunofluorescence images. c Total mRNA was extracted from ALDH1low- and ALDH1high-expressing LTLT-Ca cells, and real-time RT-PCR analyses were done for HER2, BCRP, TWIST, Nanog, and BMI-1 mRNA and 18S rRNA. Real-time results are expressed as the fold change in mRNA levels compared with ALDH low after normalization to 18S rRNA (mean ± SEM, n = 2 pooled samples/group). d MCF-7Ca and LTLT-Ca cells were plated in their respective passage media. Total protein was extracted and HER2, BCRP, and β-actin protein were analyzed by western blot. Representative blots (n = 6 independent cell samples/group) are shown
EGFR/HER1, HER2, and BCRP are involved in regulating the TIC phenotype in LTLT-Ca cells
HER2 and BCRP are examples of TIC-regulating factors [9, 13, 15, 18, 30, 33, 34]. To assess the importance of HER2 in regulating the TIC phenotype, the effects of HER2 inhibitors lapatinib (a EGFR/HER1-HER2 tyrosine kinase inhibitor), and trastuzumab (a HER2-specific monoclonal antibody) [35] were determined. Lapatinib treatment, in particular, has been previously shown to reduce TIC characteristics in breast cancer cells obtained from patients [9]. Since HER2 can be ligand-dependently activated through dimerization with EGFR/HER1 [36], and lapatinib can inhibit both HER2 and EGFR/HER1, the effect of highly specific and potent (at nM concentrations) EGFR/HER1 kinase inhibitor BIBX1382 [37] was also analyzed. The percentage of SP cells in LTLT-Ca remained unchanged by HER2-specific trastuzumab or EGFR/HER1-specific BIBX1382, but was decreased by dual inhibitor lapatinib (7.3 vs. 12.9 % control, Fig. 3a). ALDH1 expression, however, was decreased in LTLT-Ca cells by lapatinib, trastuzumab, and BIBX1382 (1.87, 0.99, and 1.8 vs. 4.34 % of vehicle-treated, respectively; Fig. 3b). Finally, 48 h treatment with either lapatinib or trastuzumab before plating in ultra-low-attachment conditions significantly decreased LTLT-Ca mammosphere formation (p < 0.05; Fig. 4), with greater effects observed in lapatinib-treated cells. The inhibitory effects of these drugs on TIC characteristics was not due to induction of cell death in the overall LTLT-Ca cell population, as trypan blue cell viability assays showed no significant differences between vehicle- and drug-treated cells within the same 48 h time frame (data not shown).
Effect of HER2, BCRP, and/or EGFR inhibitors on percentage of side population (SP) cells and ALDH-expressing LTLT-Ca cells. a Percentage of side population (SP) cells were analyzed in MCF-7Ca and LTLT-Ca cells by Hoechst staining by flow cytometry after 48 h treatment with vehicle (control), 1 μM Ko143, 1 μM lapatinib, 500 μg/mL trastuzumab, or 10 nM BIBX 1382. Plots show representative SP fractions, as designated by polygons and quantified as percentages (n = 3 independent cell samples/group; p < 0.01). b Analysis of aldehyde dehydrogenase 1 (ALDH) by measuring the cellular fluorescence of bodipy-aminoacetate (BAAA) after 48 h treatment with vehicle (control), 1 μM lapatinib, 500 μg/mL trastuzumab, or 100 nM BIBX 1382. Plots show representative ALDH expressing cells, as designated by polygons and quantified as percentages (n = 3 independent cell samples/group; p < 0.05)
Effect of HER2, BCRP, and/or EGFR inhibitors on mammosphere formation in LTLT-Ca cells. After 48 h treatment with either vehicle (control), HER2 inhibitors (1 μM lapatinib or 500 μg/mL trastuzumab), or BCRP inhibitors (1 μM of either Ko1453 or FTC), LTLT-Ca cells were plated onto ultra-low-attachment plates containing mammosphere culture media. After 14 days in culture, formed mammospheres were imaged and counted. The mean mammosphere counts. (mean ± SEM, n = 3 independent cell samples/group, p < 0.01.) are shown
BCRP’s importance was similarly assessed using specific and potent BCRP inhibitors FTC or FTC’s less toxic, more potent analog Ko143 [38]. Consistent with studies in other breast cancer cell lines [6] and with BCRP’s known function as a membrane-associated transporter protein that effluxes from cells a variety of molecules (i.e., Hoechst dye and chemotherapeutic drugs) [16], Ko143 treatment significantly reduced the percentage of SP cells (0.02 % Ko143 vs. 9.17 % in Fig. 1a; 0.24 % Ko143 vs. 7.91 % vehicle in Fig. 3a). Both FTC and Ko143 significantly decreased mammosphere formation by ~75 % compared to vehicle-treated LTLT-Ca cells (p < 0.05, Fig. 4). Similar reduction in mammosphere formation was observed after treatment of LTLT-Ca cells with BCRP siRNA to reduce BCRP expression (Fig. 5). Neither Ko143 nor FTC had an effect on ALDH1 expression (data not shown). Overall, these results demonstrate that both HER2 and BCRP are involved in regulating the TIC phenotype of LTLT-Ca cells. BCRP is important in SP and mammosphere formation, whereas HER2 is required for ALDH1, SP, and mammosphere formation in LTLT-Ca cells. These results indicate that EGFR/HER1 may also have a role in TICs.
Effect of BCRP siRNA on BCRP mRNA expression and mammosphere formation in LTLT-Ca cells. a LTLT-Ca cells were plated in passage media and then treated with two siRNAs for BCRP for 48 h. Total mRNA was extracted and BCRP mRNA and 18S rRNA were analyzed by real-time RT-PCR. Real-time results are expressed as the fold change in mRNA levels compared with negative control after normalization to 18S rRNA (mean ± SEM, n = 6 samples/group; asterisk vs. vehicle, p < 0.01). b LTLT-Ca cells were plated in passage media and then treated with negative control siRNA or BCRP siRNA for 48 h. Cells were then collected and resuspended in mammosphere media on low-attachment cell culture wells. Results are expressed as number of mammospheres counted per 40,000 cells plated (mean ± SEM, n = 6 samples/group; asterisk vs. negative control, p < 0.01)
EGFR/HER1 and HER2 are involved in regulation of BCRP
Since HER2 and BCRP are both overexpressed in LTLT-Ca cells (Fig. 2) and are important in the TIC phenotype (Figs. 3, 4), another objective of this study was to determine whether HER2 regulates BCRP expression in LTLT-Ca cells and whether EGFR/HER1 was also involved. The role of HER2 is supported by several pieces of evidence. First, other HER2-expressing cell lines also had elevated BCRP levels. HER2-transfected MCF-7 (MCF-7/HER2) cells overexpressed BCRP protein compared to HER2-/low expressing cells (i.e., MCF-7 and SUM149), and at comparable levels to LTLT-Ca cells (Fig. 6a). In addition, compared to exemestane-sensitive, HER2-, parental AC1 cells, another AI (exemestane)-resistant cell line (AC1-ExR) had elevated levels of both HER2 and BCRP protein (Fig. 6b) and increased mammosphere formation (Fig. 6c). Even though ERα is also known to regulate BCRP [22], BCRP protein was elevated in both ERα-/HER2 + LTLT-Ca cells and in ERα+/HER2 + MCF-7/HER2 and AC1-ExR cells (Fig. 6a, b). It was also elevated in cell lines with (AC1-ExR cells) or without (LTLT-Ca) increased EGFR/HER1 phosphorylation compared to their parental cell lines (Fig. 6a, b). Thus, upregulation of BCRP occurs independently of ERα expression and EGFR/HER1 activation.
Protein expression in HER2- and HER2+ cells and mammosphere formation in AC1-ExR cells. a MCF-7Ca (MC), SUM149 (S), MCF-7/HER2 (MH), and LTLT-Ca (LT) cells were plated in their respective passage media. Total protein was extracted and HER2, ERα, BCRP, and β-actin protein were analyzed by western blot. Representative blots (n = 6 independent cell samples/group) are shown. b AC1 (AC1), AC1-ExR (ExR), MCF-7Ca (MC), and LTLT-Ca (LT) cells were plated in their respective passage media. Total protein was extracted and HER2, phosphorylated EGFR/HER1 (p-EGFR/HER1), ERα, BCRP, and β-actin protein were analyzed by western blot. Representative blots (n = 3 samples/group) are shown. c AC1, AC1-ExR, and LTLT-Ca cells were resuspended and plated in mammosphere media onto ultra-low-attachment cell culture wells. After 8 days, formed mammospheres were counted. Results are expressed as number of mean mammospheres counted per 20,000 cells plated (mean ± SEM, n = 3 samples/group; asterisk vs. vehicle, p < 0.05 vs. AC1)
Second, inhibition of HER2 signaling decreased BCRP expression. LTLT-Ca cells were treated for 24 h with lapatinib alone, trastuzumab alone, BIBX1382 alone, or BIBX1382 and trastuzumab in combination (B + T). Cells were then subjected to western blot analyses to confirm efficacy and specificity of each treatment and to determine the effect of each on BCRP expression. Drug treatments affected HER2 and/or EGFR/HER1 expression and their downstream activation of MAPK (evidenced by p-ERK1/2) as expected: only cells treated with trastuzumab reduced HER2 protein expression; none affected EGFR/HER1 expression; and all decreased p-ERK1/2 protein expression with lapatinib alone and B + T having the greatest effects (Fig. 7a). Lapatinib and B + T were also the most effective treatments for reducing PI3K/Akt kinase pathway activation (as evidenced by p-Akt protein) and BCRP protein expression (Fig. 7a), consistent with other studies [20], RT-PCR analyses further showed that lapatinib’s inhibitory effects on BCRP expression also occurred at the mRNA level and regardless of letrozole treatment (Fig. 7b).
Effect of HER2 and EGFR inhibitors on protein and/or mRNA expression in LTLT-Ca cells. a LTLT-Ca cells were treated for 24 h with either vehicle (Veh), 1 μM lapatinib, 500 μg/mL trastuzumab (Trast), 100 nM BIBX 1382 (BIB), or BIBX 1382 and trastuzumab in combination (B + T). Total protein was extracted and HER2, EGFR/HER1, phosphorylated- (p-ERK1/2) and total-ERK1/2, phosphorylated- and total-Akt, BCRP, and β-actin were analyzed by western blot (n = 3 independent cell samples/group). Representative blots are shown. Dashed line indicates omitted lane in between BIB and B + T lanes of the same blots. b LTLT-Ca cells were treated with either DMSO/ethanol vehicle or 1 μM lapatinib and/or 1 μM letrozole or 24 h. Total RNA was extracted and BCRP mRNA and 18S rRNA were analyzed by real-time RT-PCR analysis. Real-time results are expressed as the fold-change in mRNA levels compared with vehicle after normalization to 18S rRNA (mean ± SEM, n = 6 samples/group)
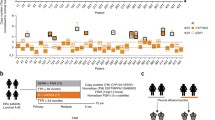
Third, HER2 and BCRP upregulation occurred concurrently and before tumors became resistant to letrozole’s growth inhibitory effects. Our previous studies have demonstrated that letrozole-treated MCF-7Ca xenografts acquire resistance to letrozole after 16–18 weeks of letrozole treatment [24]. This is preceded by upregulation of HER2 protein expression in tumors beginning at ~4 weeks of letrozole treatment [24]. In this current study, analysis of tumor samples acquired after 4 and 14 weeks of control treatment (Δ4A) demonstrated that BCRP protein levels remained unchanged (Fig. 8) despite significant growth of the tumor at this time (data not shown). In contrast, 4 weeks of letrozole treatment increased BCRP expression by 1.9- (not normalized) or 4.9-fold (normalized) compared control-treated tumors. BCRP expression increased even more compared to control after 8 and 24 weeks (3.5 or 4.9-fold and 3.7 or 4.1-fold vs. 4 weeks of control, respectively). Altogether, in vitro and in vivo results of this current study support a role for HER2, as well as EGFR/HER1 in the regulation of BCRP expression in LTLT-Ca cells.
Protein expression in xenograft MCF-7Ca tumors. Xenografts of MCF-7Ca cells were grown in mice as described in the Materials and Methods. After the tumors reached 300 mm3, mice were treated with either control (100 μg/day Δ4A) or letrozole (100 μg/day Δ4A + 10 μg/day letrozole). At various pre-designated times or when the tumors reached 2,000 mm3, tumors were collected at necropsy and BCRP and β-actin protein expression was analyzed by western blot
Discussion
It has been previously established that resistance of ERα+ breast cancer cells to AIs involves a switch from ERα-dependent growth to growth factor-dependent growth [2, 3, 24, 39]. Particularly, in letrozole- and exemestane-resistant breast cancers, this switch involves overexpression of HER2 (Figs. 2, 7). How HER2 contributes to resistance to AIs, however, was unknown.
One possibility explored in this study is that HER2 confers resistance by regulating stem cell markers that, in turn, increase TICs within the overall cancer cell population. TICs have been linked to tumor relapse, metastasis, and resistance to chemotherapy in several cancer types, including breast cancer [40]. However, their role in endocrine therapy resistance, particularly AI resistance, has not been well studied. Dubrovska et al. [41] has recently demonstrated that tamoxifen-resistant cells have higher BCRP and ALDH expression, and higher clonogenic potential and tumourigenicity in vivo compared to tamoxifen-sensitive MCF7 cells. Our current study provides support for the relevance of TICs in AI resistance. LTLT-Ca and/or AC1-ExR cells exhibited higher levels of TIC characteristics, including expression of known stem cell markers, than their AI-sensitive parental cell lines (Figs. 1, 2, 3, 6).
Expression of stem cell marker and drug efflux transporter BCRP [42] in letrozole and exemestane-resistant cells is of notable significance. LTLT-Ca cells expressed higher BCRP levels and SP percentage compared to letrozole-sensitive MCF-7Ca cells, and inhibition of BCRP function decreased LTLT-Ca cell mammosphere formation and SP % (Figs. 2, 3). While non-TIC cells can also express BCRP and be designated as SP cells, these characteristics tend to be enriched in the TIC subpopulation [43, 44]. Thus, acquired resistance to letrozole or exemestane may occur via increased effluxing of these AIs out of breast cancer cells, particularly TICs, and via increased presence of TICs in general.
Increased TICs and BCRP in AI-resistant cells appear to be regulated by HER2, as well as EGFR1/HER1. This is consistent with studies demonstrating EGFR/HER1 and/or HER2 overexpression in tamoxifen-resistant and long-term estrogen-deprived cells, as well as in breast TICs [40]. Patients with EGFR1/HER1- and HER2-overexpression tumors also have poorer clinical outcomes with tamoxifen treatment [36]. EGFR/HER1’s role in AI-resistant breast cancer, however, appears to be secondary to that of HER2 and/or only in association with HER2 via dimerization. Its expression and activation was not consistently associated with letrozole- or exemestane-resistance or with BCRP expression (Fig. 6). Nevertheless, it cannot be ruled out that EGFR/HER1 may independently regulate stem cell markers and other TIC characteristics in AI-resistant cells not investigated in this study.
Taken together, the results of this study suggest that reducing or eliminating the TIC subpopulation with agents that target BCRP, HER2, EGFR/HER1, and/or their downstream kinase pathways (i.e., MAPK and PI3K/Akt pathways) could be effective in preventing and/or treating acquired AI resistance. Clinical studies have shown that treating patients with AIs in combination with either lapatinib or trastuzumab [45–47], or gefitinib (an EGFR tyrosine kinase inhibitor) [48] resulted in better clinical outcomes than treating with AIs alone. The number of such clinical studies are limited, however, and even fewer have directly compared these drugs to each other. One study has shown that trastuzumab combined with neoadjuvant anthracycline-taxane-based chemotherapy elicits a better pathological response in untreated ER-/HER2+ breast cancer patients than lapatinib combined with chemotherapy [49]. However, results of our current study suggests that the dual EGFR/HER1-HER2 kinase inhibitor lapatinib may be more effective than either HER2-specific trastuzumab or EGFR-specific gefitinib, or in treating ER+ breast cancer patients that have relapsed from AI treatment.
References
Chumsri S, Howes T, Bao T, Sabnis G, Brodie A (2011) Aromatase, aromatase inhibitors, and breast cancer. J Steroid Biochem Mol Biol 125(1–2): 13–22. doi:10.1016/j.jsbmb.2011.02.001
Johnston SR, Martin LA, Leary A, Head J, Dowsett M (2007) Clinical strategies for rationale combinations of aromatase inhibitors with novel therapies for breast cancer. J Steroid Biochem Mol Biol 106(1–5):180–186. doi:10.1016/j.jsbmb.2007.05.019
Sabnis G, Brodie A (2011) Adaptive changes results in activation of alternate signaling pathways and resistance to aromatase inhibitor resistance. Mol Cell Endocrinol 340(2):142–147. doi:10.1016/j.mce.2010.09.005
Macedo LF, Sabnis GJ, Goloubeva OG, Brodie A (2008) Combination of anastrozole with fulvestrant in the intratumoral aromatase xenograft model. Cancer Res 68(9): 3516–3522. doi:10.1158/0008-5472.CAN-07-6807
Magnifico A, Albano L, Campaner S, Delia D, Castiglioni F, Gasparini P, Sozzi G, Fontanella E, Menard S, Tagliabue E (2009) Tumor-initiating cells of HER2-positive carcinoma cell lines express the highest oncoprotein levels and are sensitive to trastuzumab. Clin Cancer Res 15(6):2010–2021. doi:10.1158/1078-0432.CCR-08-1327
Nakanishi T, Chumsri S, Khakpour N, Brodie AH, Leyland-Jones B, Hamburger AW, Ross DD, Burger AM (2010) Side-population cells in luminal-type breast cancer have tumour-initiating cell properties, and are regulated by HER2 expression and signalling. Br J Cancer 102(5):815–826. doi:10.1038/sj.bjc.6605553
Creighton CJ, Li X, Landis M, Dixon JM, Neumeister VM, Sjolund A, Rimm DL, Wong H, Rodriguez A, Herschkowitz JI, Fan C, Zhang X, He X, Pavlick A, Gutierrez MC, Renshaw L, Larionov AA, Faratian D, Hilsenbeck SG, Perou CM, Lewis MT, Rosen JM, Chang JC (2009) Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc Natl Acad Sci USA 106(33):13820–13825. doi:10.1073/pnas.0905718106
Phillips TM, McBride WH, Pajonk F (2006) The response of CD24(−/low)/CD44+ breast cancer-initiating cells to radiation. J Natl Cancer Inst 98(24):1777–1785. doi:10.1093/jnci/djj495
Li X, Lewis MT, Huang J, Gutierrez C, Osborne CK, Wu MF, Hilsenbeck SG, Pavlick A, Zhang X, Chamness GC, Wong H, Rosen J, Chang JC (2008) Intrinsic resistance of tumorigenic breast cancer cells to chemotherapy. J Natl Cancer Inst 100(9):672–679. doi:10.1093/jnci/djn123
Nicolini A, Ferrari P, Fini M, Borsari V, Fallahi P, Antonelli A, Berti P, Carpi A, Miccoli P (2011) Stem cells: their role in breast cancer development and resistance to treatment. Curr Pharm Biotechnol 12(2):196–205
van Rhenen A, Feller N, Kelder A, Westra AH, Rombouts E, Zweegman S, van der Pol MA, Waisfisz Q, Ossenkoppele GJ, Schuurhuis GJ (2005) High stem cell frequency in acute myeloid leukemia at diagnosis predicts high minimal residual disease and poor survival. Clin Cancer Res 11(18):6520–6527. doi:10.1158/1078-0432.CCR-05-0468
Al-Hajj M, Becker MW, Wicha M, Weissman I, Clarke MF (2004) Therapeutic implications of cancer stem cells. Curr Opin Genet Dev 14(1):43–47. doi:10.1016/j.gde.2003.11.007
Mehta K (1994) High levels of transglutaminase expression in doxorubicin-resistant human breast carcinoma cells. Int J Cancer 58(3):400–406
Calcagno AM, Salcido CD, Gillet JP, Wu CP, Fostel JM, Mumau MD, Gottesman MM, Varticovski L, Ambudkar SV (2010) Prolonged drug selection of breast cancer cells and enrichment of cancer stem cell characteristics. J Natl Cancer Inst 102(21): 1637–1652. doi:10.1093/jnci/djq361
Dontu G, Al-Hajj M, Abdallah WM, Clarke MF, Wicha MS (2003) Stem cells in normal breast development and breast cancer. Cell Prolif 36(Suppl 1):59–72
Doyle LA, Ross DD (2003) Multidrug resistance mediated by the breast cancer resistance protein BCRP (ABCG2). Oncogene 22(47):7340–7358. doi:10.1038/sj.onc.1206938
Liu H, Cheng D, Weichel AK, Osipo C, Wing LK, Chen B, Louis TE, Jordan VC (2006) Cooperative effect of gefitinib and fumitremorgin c on cell growth and chemosensitivity in estrogen receptor alpha negative fulvestrant-resistant MCF-7 cells. Int J Oncol 29(5):1237–1246
Meyer zu Schwabedissen HE, Grube M, Dreisbach A, Jedlitschky G, Meissner K, Linnemann K, Fusch C, Ritter CA, Volker U, Kroemer HK (2006) Epidermal growth factor-mediated activation of the map kinase cascade results in altered expression and function of ABCG2 (BCRP). Drug Metab Dispos 34(4):524–533. doi:10.1124/dmd.105.007591
Zhang W, Ding W, Chen Y, Feng M, Ouyang Y, Yu Y, He Z (2011) Up-regulation of breast cancer resistance protein plays a role in HER2-mediated chemoresistance through PI3K/Akt and nuclear factor-kappa B signaling pathways in MCF7 breast cancer cells. Acta Biochim Biophys Sin (Shanghai) 43(8):647–653. doi:10.1093/abbs/gmr050
Perry J, Ghazaly E, Kitromilidou C, McGrowder EH, Joel S, Powles T (2010) A synergistic interaction between lapatinib and chemotherapy agents in a panel of cell lines is due to the inhibition of the efflux pump BCRP. Mol Cancer Ther 9(12): 3322–3329. doi:10.1158/1535-7163.MCT-10-0197
Wang H, Zhou L, Gupta A, Vethanayagam RR, Zhang Y, Unadkat JD, Mao Q (2006) Regulation of BCRP/ABCG2 expression by progesterone and 17beta-estradiol in human placental BeWo cells. Am J Physiol Endocrinol Metab 290(5):E798–E807. doi:10.1152/ajpendo.00397.2005
Zhang Y, Zhou G, Wang H, Zhang X, Wei F, Cai Y, Yin D (2006) Transcriptional upregulation of breast cancer resistance protein by 17beta-estradiol in ERalpha-positive MCF-7 breast cancer cells. Oncology 71(5–6):446–455. doi:10.1159/000108594
Goodell MA (2002) Multipotential stem cells and ‘side population’ cells. Cytotherapy 4(6):507–508. doi:10.1080/146532402761624638
Jelovac D, Sabnis G, Long BJ, Macedo L, Goloubeva OG, Brodie AM (2005) Activation of mitogen-activated protein kinase in xenografts and cells during prolonged treatment with aromatase inhibitor letrozole. Cancer Res 65(12):5380–5389. doi:10.1158/0008-5472.CAN-04-4502
Patrawala L, Calhoun T, Schneider-Broussard R, Zhou J, Claypool K, Tang DG (2005) Side population is enriched in tumorigenic, stem-like cancer cells, whereas ABCG2+ and ABCG2- cancer cells are similarly tumorigenic. Cancer Res 65(14):6207–6219. doi:10.1158/0008-5472.CAN-05-0592
Christgen M, Ballmaier M, Bruchhardt H, von Wasielewski R, Kreipe H, Lehmann U (2007) Identification of a distinct side population of cancer cells in the Cal-51 human breast carcinoma cell line. Mol Cell Biochem 306(1–2):201–212. doi:10.1007/s11010-007-9570-y
Goodell MA, Rosenzweig M, Kim H, Marks DF, DeMaria M, Paradis G, Grupp SA, Sieff CA, Mulligan RC, Johnson RP (1997) Dye efflux studies suggest that hematopoietic stem cells expressing low or undetectable levels of CD34 antigen exist in multiple species. Nat Med 3(12):1337–1345
Korkaya H, Paulson A, Iovino F, Wicha MS (2008) HER2 regulates the mammary stem/progenitor cell population driving tumorigenesis and invasion. Oncogene 27(47):6120–6130. doi:10.1038/onc.2008.207
Dontu G, Jackson KW, McNicholas E, Kawamura MJ, Abdallah WM, Wicha MS (2004) Role of notch signaling in cell-fate determination of human mammary stem/progenitor cells. Breast Cancer Res 6(6):R605–R615. doi:10.1186/bcr920
Calcagno AM, Salcido CD, Gillet JP, Wu CP, Fostel JM, Mumau MD, Gottesman MM, Varticovski L, Ambudkar SV (2010) Prolonged drug selection of breast cancer cells and enrichment of cancer stem cell characteristics. J Natl Cancer Inst 102(21):1637–1652. doi:10.1093/jnci/djq361
Jeter CR, Liu B, Liu X, Chen X, Liu C, Calhoun-Davis T, Repass J, Zaehres H, Shen JJ, Tang DG (2011) NANOG promotes cancer stem cell characteristics and prostate cancer resistance to androgen deprivation. Oncogene 30(36): 3833–3845. doi:10.1038/onc.2011.114
Liu S, Dontu G, Mantle ID, Patel S, Ahn NS, Jackson KW, Suri P, Wicha MS (2006) Hedgehog signaling and Bmi-1 regulate self-renewal of normal and malignant human mammary stem cells. Cancer Res 66(12):6063–6071. doi:10.1158/0008-5472.CAN-06-0054
Nakanishi T, Chumsri S, Khakpour N, Brodie AH, Leyland-Jones B, Hamburger AW, Ross DD, Burger AM (2010) Side-population cells in luminal-type breast cancer have tumour-initiating cell properties, and are regulated by HER2 expression and signalling. Br J Cancer 102(5):815–826. doi:10.1038/sj.bjc.6605553
Chen JS, Pardo FS, Wang-Rodriguez J, Chu TS, Lopez JP, Aguilera J, Altuna X, Weisman RA, Ongkeko WM (2006) EGFR regulates the side population in head and neck squamous cell carcinoma. Laryngoscope 116(3):401–406. doi:10.1097/01.mlg.0000195075.14093.fb
Ahn ER, Vogel CL (2012) Dual HER2-targeted approaches in HER2-positive breast cancer. Breast Cancer Res Treat 131(2): 371–383. doi:10.1007/s10549-011-1781-y
Saxena R, Dwivedi A (2012) ErbB family receptor inhibitors as therapeutic agents in breast cancer: current status and future clinical perspective. Med Res Rev 32(1): 166–215. doi:10.1002/med.20209
Solca FF, Baum A, Langkopf E, Dahmann G, Heider KH, Himmelsbach F, van Meel JC (2004) Inhibition of epidermal growth factor receptor activity by two pyrimidopyrimidine derivatives. J Pharmacol Exp Ther 311(2):502–509. doi:10.1124/jpet.104.069138
Allen JD, van Loevezijn A, Lakhai JM, van der Valk M, van Tellingen O, Reid G, Schellens JH, Koomen GJ, Schinkel AH (2002) Potent and specific inhibition of the breast cancer resistance protein multidrug transporter in vitro and in mouse intestine by a novel analogue of fumitremorgin C. Mol Cancer Ther 1(6):417–425
Masri S, Phung S, Wang X, Chen S (2010) Molecular characterization of aromatase inhibitor-resistant, tamoxifen-resistant and LTEDaro cell lines. J Steroid Biochem Mol Biol 118(4–5): 277–282. doi:10.1016/j.jsbmb.2009.10.011
O’Brien CS, Farnie G, Howell SJ, Clarke RB (2011) Breast cancer stem cells and their role in resistance to endocrine therapy. Horm Cancer 2(2):91–103. doi:10.1007/s12672-011-0066-6
Dubrovska A, Hartung A, Bouchez LC, Walker JR, Reddy VA, Cho CY, Schultz PG (2012) CXCR4 activation maintains a stem cell population in tamoxifen-resistant breast cancer cells through AhR signalling. Br J Cancer. doi:10.1038/bjc.2012.105
Konecny G, Pauletti G, Pegram M, Untch M, Dandekar S, Aguilar Z, Wilson C, Rong HM, Bauerfeind I, Felber M, Wang HJ, Beryt M, Seshadri R, Hepp H, Slamon DJ (2003) Quantitative association between HER-2/neu and steroid hormone receptors in hormone receptor-positive primary breast cancer. J Natl Cancer Inst 95(2):142–153
Hirschmann-Jax C, Foster AE, Wulf GG, Nuchtern JG, Jax TW, Gobel U, Goodell MA, Brenner MK (2004) A distinct “side population” of cells with high drug efflux capacity in human tumor cells. Proc Natl Acad Sci USA 101(39):14228–14233. doi:10.1073/pnas.0400067101
Natarajan K, Xie Y, Baer MR, Ross DD (2012) Role of breast cancer resistance protein (BCRP/ABCG2) in cancer drug resistance. Biochem Pharmacol 83(8): 1084–1103. doi:10.1016/j.bcp.2012.01.002
Johnston S, Pippen J Jr, Pivot X, Lichinitser M, Sadeghi S, Dieras V, Gomez HL, Romieu G, Manikhas A, Kennedy MJ, Press MF, Maltzman J, Florance A, O’Rourke L, Oliva C, Stein S, Pegram M (2009) Lapatinib combined with letrozole versus letrozole and placebo as first-line therapy for postmenopausal hormone receptor-positive metastatic breast cancer. J Clin Oncol 27(33):5538–5546. doi:10.1200/JCO.2009.23.3734
Fleeman N, Bagust A, Boland A, Dickson R, Dundar Y, Moonan M, Oyee J, Blundell M, Davis H, Armstrong A, Thorp N (2011) Lapatinib and trastuzumab in combination with an aromatase inhibitor for the first-line treatment of metastatic hormone receptor-positive breast cancer which over-expresses human epidermal growth factor 2 (HER2): a systematic review and economic analysis. Health Technol Assess 15(42):1–93, iii–iv. doi:10.3310/hta15420
Koeberle D, Ruhstaller T, Jost L, Pagani O, Zaman K, von Moos R, Oehlschlegel C, Crowe S, Pilop C, Thuerlimann B (2011) Combination of trastuzumab and letrozole after resistance to sequential trastuzumab and aromatase inhibitor monotherapies in patients with estrogen receptor-positive, HER-2-positive advanced breast cancer: a proof-of-concept trial (SAKK 23/03). Endocr Relat Cancer 18(2):257–264. doi:10.1530/ERC-10-0317
Cristofanilli M, Valero V, Mangalik A, Royce M, Rabinowitz I, Arena FP, Kroener JF, Curcio E, Watkins C, Bacus S, Cora EM, Anderson E, Magill PJ (2010) Phase II, randomized trial to compare anastrozole combined with gefitinib or placebo in postmenopausal women with hormone receptor-positive metastatic breast cancer. Clin Cancer Res 16(6):1904–1914. doi:10.1158/1078-0432.CCR-09-2282
Untch M, Loibl S, Bischoff J, Eidtmann H, Kaufmann M, Blohmer JU, Hilfrich J, Strumberg D, Fasching PA, Kreienberg R, Tesch H, Hanusch C, Gerber B, Rezai M, Jackisch C, Huober J, Kuhn T, Nekljudova V, von Minckwitz G (2012) Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline-taxane-based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol 13(2):135–144. doi:10.1016/S1470-2045(11)70397-7
Acknowledgments
This research was supported in part by RO1 CA 62483 and a Komen Scholars award to Angela Brodie. The authors would like to thank Dr Ferenc Livak for his help with flow cytometry.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Rabia A. Gilani and Armina A. Kazi contributed equally to this study.
Rights and permissions
About this article
Cite this article
Gilani, R.A., Kazi, A.A., Shah, P. et al. The importance of HER2 signaling in the tumor-initiating cell population in aromatase inhibitor-resistant breast cancer. Breast Cancer Res Treat 135, 681–692 (2012). https://doi.org/10.1007/s10549-012-2148-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2148-8