Abstract
Olfactory dysfunctions affect a larger portion of population (up to 15% with partial olfactory loss, and 5% with complete olfactory loss) as compared to other sensory dysfunctions (e.g. auditory or visual) and have a negative impact on the life quality. The impairment of olfactory functions may happen at each stage of the olfactory system, from epithelium to cortex. Non-invasive neuroimaging techniques such as the magnetic resonance imaging (MRI) have advanced the understanding of the advent and progress of olfactory dysfunctions in humans. The current review summarizes recent MRI studies on human olfactory dysfunction to present an updated and comprehensive picture of the structural and functional alterations in the central olfactory system as a consequence of olfactory loss and regain. Furthermore, the review also highlights recent progress on optimizing the olfactory functional MRI as well as new approaches for data processing that are promising for future clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The Human Olfactory Dysfunction
Having received relatively little attention over the last 100 years, recent evidence suggests that the human sense of smell is not a negligible entity (McGann 2017), and plays an important role in food ingestion, harm avoidance, and social communication (Hummel et al. 2007; Stevenson 2010). The loss of olfactory functions can lead to a drastic change in the enjoyment of eating, changes in body weight, changes in daily activities, sexuality and disturbances in affective behavior, and, hence, a reduced quality of life (Miwa et al. 2001; Santos et al. 2004; Frasnelli and Hummel 2005; Croy et al. 2014). Population-based studies of olfactory loss indicate a prevalence of 22% (25 to 75 years) (Vennemann et al. 2008), 19% (≥ 20 years) (Bramerson et al. 2004), or 24% (≥ 53 years) (Murphy et al. 2002), with highest prevalence in older men.
Olfactory loss is characterized as a reduced ability to smell and to detect odors. Clinically, people with olfactory loss are classified as hyposmia (the sense of smell is partially reduced) or functional anosmia (the sense of smell is reduced to the extent that is not useful in daily life) (Hummel et al. 2016). Besides, approximately 1 in 8000 people are born without a sense of smell which is the congenital anosmia. Apart from age-related olfactory function decline, the major causes for olfactory loss include sinonasal disease, traumatic brain injury, upper respiratory tract infection, congenital anosmia, or idiopathic causes (Temmel et al. 2002). Moreover, olfactory loss is among the early symptoms of Parkinson’s disease (Hawkes et al. 1997; Haehner et al. 2007; Ross et al. 2008), Alzheimer’s disease (Marine and Boriana 2014), incipient dementia schizophrenia (Moberg et al. 1999), or depression (Croy and Hummel 2017). Hence, olfactory dysfunction is associated with multiple neurological disorders that may affect the overall health of the population.
The Central Olfactory System
Odor perception requires a functional peripheral sensory organ and central pathways. Odor molecules first arrive at the nasal epithelium and make contact with the sensory endings of olfactory receptor neurons. Axonal projections are then conveyed with a relay in the olfactory bulbs (OB) to the cortex and terminate in several areas in the basal frontal and medial temporal lobes, including the piriform cortex, peri and anterior amygdaloid cortex, and rostral entorhinal cortex (Gottfried 2010; Van Hartevelt and Kringelbach 2011). These cortical regions that receive direct input from the OB are collectively referred to as the ‘primary olfactory cortex’. The cortical targets of the primary olfactory cortex include various brain regions in the limbic lobe and frontal cortex, including the additional amygdala subnuclei, orbitofrontal cortex (OFC), hippocampus, parahippocampal gyrus, cingulate cortex, insula, striatum hypothalamus, and the mediodorsal thalamus (Gottfried and Zald 2005; Fjaeldstad et al. 2017; Zhou et al. 2019). Collectively, these areas are commonly referred to as the secondary olfactory cortex (Fig. 1).
Olfactory dysfunctions led to a significant decreased quality of life (Croy et al. 2014) as well as structural and functional alterations of the brain (Reichert and Schopf 2017). The magnetic resonance imaging (MRI), providing a non-invasive approach to investigate the structural and functional features of the working brain, has been applied in research on human olfaction and olfactory dysfunctions. The present review will provide a summary of the current state of MRI research on functional and structural changes in the central olfactory system due to olfactory dysfunction and will discuss the potential of MRI-based investigations in clinical routine.
Functional Changes After Olfactory Loss
Odor-Induced Brain Responses in Olfactory Loss
Chemosensory odor perception is partly the result of the interaction between the olfactory and the trigeminal systems. Whereas the olfactory system mediates the quality percept of an odor, the trigeminal system conveys sensations such as burning, pungency, or stinging, as well as touch, pressure, and temperature (Albrecht et al. 2010). Using MRI, a number of studies has investigated disrupted brain responses to odors in patients with olfactory loss. Compared to healthy controls, patients demonstrate widespread decrease of odor-induced brain activation in the olfactory related regions, including the piriform cortex, amygdala, OFC, insula, and anterior cingulate cortex (Levy et al. 1998; Levy et al. 1999a, b; Pellegrino et al. 2016; Han et al. 2018a, b; Moon et al. 2018). Due to intimate connections between the olfactory and trigeminal systems, the olfactory loss is also linked to alterations for cerebral processing of trigeminal or bimodal olfactory stimulation. In two fMRI studies, patients with olfactory loss exhibited reduced activation in the primary motor area and cerebellum in response to either trigeminal or bimodal odor stimulations (Iannilli et al. 2007, 2011).
Attenuated odor-induced brain responses were also seen in patients with neurodegenerative disorders, including Parkinson’s disease (Hummel et al. 2010, Takeda et al. 2010), Alzheimer’s disease (Vasavada et al. 2015, 2017) or Autism Spectrum Disorder (Koehler et al. 2018). Hummel et al. (2010) found different patterns for processing pleasant or unpleasant odors among patients with Parkinson’s disease. Li et al. (2010) demonstrated that patients with early-stage Alzheimer’s disease exhibited a blunted cross-adaptation response in the posterior piriform cortex after the sequential presentation of qualitatively similar (versus qualitatively different) odor pairs. This finding reflected a functional disruption of odor quality coding in this olfactory brain area, which may provide evidence for perceptual deficits in odor identification among those patients. Taken together, olfactory loss affects the central olfactory system and led to a blunted neural response to odor stimulation. However, the patients included in most previous studies were heterogeneous in terms of the cause for olfactory loss, which limited the detection of specific differences between groups. Moreover, few fMRI studies had been done among patients with olfactory loss focusing on olfactory sub-functions during odor perception, such as odor discrimination or identification.
Olfactory Loss and Top-Down Cognitive Modulation
Olfactory perception is modulated by higher levels of cognitive processing, such as memory or learning, which is known as the olfactory “top-down” modulation (Rolls 2011). Previous studies have shown the involvement of multiple olfactory brain regions in the olfactory “top-down” processing. For example, regions activated during odor perception such as the piriform cortex, OFC, and insula were also seen activation during olfactory imagery (Bensafi et al. 2003; Djordjevic et al. 2005; Bensafi et al. 2007) or odor expectation (Zelano et al. 2011). Besides, non-odorous but odor-related stimuli such as words (Gonzalez et al. 2006; Arshamian et al. 2013), metaphors (Pomp et al. 2018) or labels (de Araujo et al. 2005; Gonzalez et al. 2006; Pomp et al. 2018), as well as sniffing (Sobel et al. 1998; Kareken et al. 2004) recruited activation in brain regions including the piriform cortex, OFC, and insula, suggesting the role of these brain regions in semantic and odor coding integration (Olofsson and Gottfried 2015).
For patients with olfactory loss, two early fMRI studies investigated olfactory imagery among patients with hyposmia (Levy et al. 1999a, b; Henkin and Levy 2002). Both studies reported increased activation in olfactory regions following olfactory imagery. The activations were interpreted as a sign of preserved olfactory imagery capacity in patients with acquired olfactory loss. However, both studies suffered from methodological problems with few participants (n = 3) in the experimental condition (Levy et al. 1999a, b) or without having a control group (Henkin and Levy 2002).
Flohr et al. (2014) reported that olfactory loss leads to deficits in odor imagery. They found that patients with olfactory loss, compared to controls, experienced lower vividness when imaging odors, and had lower levels of brain activation in the hippocampus and insula. However, the patient group had a higher level of brain activation in the dorsal lateral prefrontal cortex (dlPFC), cerebellum and precuneus, regions that are related to working memory and autobiographical odor information retrieval (Dade et al. 2001; Curtis and D’Esposito 2003; Cavanna and Trimble 2006; Arshamian et al. 2013). Moreover, the level of the dlPFC activation was positively correlated with the duration of olfactory loss among patients (Flohr et al. 2014). These findings indicated that during odor imagery, patients were not able to image odors in a conventional way and needed more attention resources as the duration of odor deprivation increased.
During expectation of words with strong olfactory associations, Han et al. (2019) found that patients with acquired smell loss showed increased activation in the left inferior frontal gyrus extending to insular cortex and the bilateral angular gyrus, areas related to semantic knowledge retrieval and olfactory processing. This may indicate a higher effort and attention loads towards olfactory cues among patients, consequently from smell loss. Besides, during reading words with olfactory associations, patients and control participants with superior odor identification abilities showed reduced activation in the OFC and putamen, respectively. The lower brain activation may be linked to a higher degree of efficiency in information processing, a similar mechanism observed in olfactory experts during odor imagery (Plailly et al. 2012). However, for patients with congenital anosmia, less brain activation in the anterior cingulate cortex and the middle frontal gyrus was observed as compared to normal controls while reading of words with olfactory association (Yoshi et al. Unpublished). Based on these findings it can be hypothesized that prior olfactory experience, which differed between patients with acquired and congenital anosmia, had different impacts on the top-down processing of olfactory-related information.
Taken together, the olfactory-loss related deprivation of odor information input has a profound impact on both the bottom-up and top-down olfactory pathways. Moreover, it has to be taken into account that different causes of smell loss could have different impacts on the top-down olfactory modulation. A more central cause for the smell loss would therefore be likely to affect the top-down olfactory process more than a peripheral cause. Understanding of the top-down process in olfactory loss may help future direction for intervention or treatment such as olfactory training, which may drive associative learning-related brain plasticity in the olfactory system (Mandairon and Linster 2009; McGann 2015).
Changes of Functional Network Related to Olfactory Loss
Functional connectivity (FC) is a measurement of the temporal correlation of neuronal activity between anatomically separated brain regions. It reflects the functional communication between brain regions (Damoiseaux et al. 2006). The FC measured during resting state or during tasks are used to quantify the strength of inter-regional brain connectivity (van den Heuvel and Hulshoff Pol 2010).
During rest, FC has been shown between the primary olfactory regions (piriform cortex and OFC) and thalamus, medial prefrontal cortex, caudate, nucleus accumbens, parahippocampal gyrus and hippocampus (Tobia et al. 2016). Olfactory loss is associated with reduced FC in patients with Parkinson’s disease (Su et al. 2015; Yoneyama et al. 2018). Patients with hyposmia showed decreased FC within the olfactory related limbic or paralimbic regions, including the rectal gyrus and insula (Su et al. 2015). FC between the amygdala and inferior parietal lobule, lingual gyrus, and fusiform gyrus were associated with the severity of hyposmia (Yoneyama et al. 2018).
During passive odor smelling, dense connections between the primary (piriform cortex) and secondary olfactory regions (OFC, insula, and hippocampus) were identified (Nigri et al. 2013). With odor stimulation, disruption of the FC between the orbitofrontal cortex and medial temporal lobes, as part of the olfactory area, was observed in normal aging (Murphy et al. 2005), however, the olfactory functions were not reported for the group of elderly participants. Compared to people with normal olfaction, patients with anosmia caused by upper respiratory infection were found to have maintained but reduced number of FC in the somatosensory and integrative networks in response to odorous stimuli (Kollndorfer et al. 2015a, b). Applying the whole-brain network graph approach, Kollndorfer et al. (2015a, b) showed reduced FC of the olfactory brain areas including the anterior prefrontal cortex, anterior cingulate cortex, the entorhinal cortex and the cerebellum among patients with anosmia. Besides, a recent study showed the recruitment of a sensory processing network, as well as a cerebellar network and an occipital network during odor stimulation (Reichert et al. 2018), and the FC of these networks were correlated with olfactory functions measured by the Sniffin’ Sticks test. Besides, disrupted FC beyond the sensory or olfactory network had also been reported in patients with olfactory loss (Kollndorfer et al. 2015a, b; Su et al. 2015).
Taken together, olfactory dysfunction is related to a widespread reduction of FC in olfactory and non-olfactory networks. Future research needs to examine the links between the FC and specific olfactory functions (sensitivity, discrimination or identification), as well as the various of odor perceptual features (e.g. odor quality, intensity or valence). This could lead to further understanding of the interacting brain regions, rather than isolated regions that are involved in olfactory subset performances among patients with olfactory dysfunction.
Structural Brain Changes of Olfactory Loss
Olfactory Bulb Volume
As the first structural rely upon the olfactory pathway, the olfactory bulb (OB) integrates peripheral odor inputs and central activity of higher cortical regions. A large number of studies have demonstrated a positive correlation between the OB volume and olfactory function (Yousem et al. 1998; Buschhuter et al. 2008; Seubert et al. 2013; Mazal et al. 2016). Olfactory loss leading to a reduced sensory input to the OB is associated with atrophy of the OB. It has been demonstrated that the decreased olfactory function is associated with decreased OB volumes in patients suffering from a wide range of pathologies including post-traumatic olfactory disorder (Yousem et al. 1996; Rombaux et al. 2006a, b, c), post-infectious olfactory disorder (Mueller et al. 2005a, b; Rombaux et al. 2006a, b, c), sinonasal related olfactory disorders (Rombaux et al. 2008), idiopathic olfactory loss (Rombaux et al. 2010), and neurodegenerative diseases (Mueller et al. 2005a, b; Wang et al. 2011).
The degree of the OB volume reduction is related to the severity of olfactory loss. For example, in both post-infectious and post-traumatic olfactory loss, OB volumes in patients with anosmia were found to be smaller than those of hyposmia (Rombaux et al. 2006a, b, c; Han et al. 2018a, b). Besides, OB volume reduction was also affected by the causes of olfactory loss. Trauma patients had smaller OB compared to chronic rhinosinusitis or post-infectious patients (Hummel et al. 2015), possibly due to the direct damage of the OB or adjunct regions during the traumatic brain injury. In another study, the OB volume in olfactory-loss patients with chronic rhinosinusitis did not show a significant difference as compared to controls (Han et al. 2017). This is possibly due to intermittent odor input to the OB among those patients that prevents long-term plastic remodeling (Han et al. 2017). It has also been reported that the OB volume change in olfactory-loss patients with sinonasal disease may be more sensitive to the degree of sinonasal inflammation (Rombaux et al. 2008) than the impaired olfactory function observed with psychophysical testing.
Grey Matter and White Matter
Olfactory loss also results in widespread structural alterations in higher-order brain areas. Studies applied voxel-based morphometry, a method that allows uncovering of regional differences in gray matter volume (GMV) from MR images, had demonstrated a decrease of GMV across the primary and secondary olfactory cortex in patients with olfactory losses due to various causes (Table 1). These structural changes are thought to result from diminished sensory input (Bitter et al. 2010a, b). Although there is overlap between studies regarding the brain regions with GMV reduction, apparent differences exist. For example, patients with olfactory loss due to traumatic brain injury were found to have wide-spread GMV reduction in multiple areas belonging to the primary and secondary olfactory cortex (Han et al. 2018a, b), whereas GMV reduction was only observed in a few secondary olfactory areas (e.g. insula, OFC) among patients with smell loss due to sinonasal disease (Han et al. 2017) or upper respiratory tract infection (Gellrich et al. 2018; Yao et al. 2018). This suggests that the etiology of olfactory loss entails a significant contribution to the structural alteration of the central olfactory system. However, direct comparison between studies is difficult due to the variability regarding the sample size, severity of olfactory loss, and the time since the onset of olfactory loss. Thus, further studies including larger samples and with a stronger focus on participant selection are necessary to extend the results and to better understand the etiology of specific structural changes following olfactory loss. Besides, a few studies have investigated the GMV of the olfactory system in patients with congenital anosmia. Compared to control participants, those patients showed an increased GMV of the olfactory cortex, such as the piriform cortex (Frasnelli et al. 2013; Karstensen et al. 2018) and superior frontal sulcus (Karstensen et al. 2018). Therefore, the lifelong olfactory deprivation seems to trigger different changes regarding the cortical GMV as compared to changes found in acquired olfactory loss.
In addition to the regional structural alterations, olfactory loss also leads to changes in the anatomical connections between distant brain regions. Diffusion-weighted MRI, which characterizes the fiber architecture of tissues within the white matter, had been applied to explore anatomical brain connections (Jones et al. 2013). Using this technique, the measurement of the structural network includes the integrity, degree (number of connections), strength (number of fibers) and percentage of fibers per connections (Fernandes et al. 2015). The Fractional anisotropy (FA) as the most widely used parameter, describing the directionality of the molecular diffusion, is thought to reflect axon integrity (Jones et al. 2013) (FA value ranges from 0 to 1, with higher values indicating greater directionality of diffusion and preserved microstructure) (Jones and Leemans 2011). Until now, only a few studies had focused on the structural connectivity in patients with olfactory loss. Patients with multiple sclerosis exhibited significantly reduced FA in olfactory brain regions related to impairment of the ability to identify odors (Erb et al. 2012; Erb-Eigner et al. 2014). A similar decline in olfactory performance due to normal aging was found to be correlated with low FA and mean diffusivity level in the corpus callosum and the superior longitudinal fasciculi (Segura et al. 2013). Ibarretxe-Bilbao et al. (2010) found that PD patients with olfactory loss showed FA decrease in areas adjacent to gyrus rectus and the primary olfactory area. The FA value in these areas was positively correlated with olfactory performances. Sobhani et al. (2019) observed positive associations between white matter connectivity and olfactory function in PD patients. Anatomical MRI could help to understand the substrates of olfaction dysfunctions and would, therefore, be a clinical marker in future studies.
MRI Studies of the Olfactory System with Olfactory Regain
Both functional and structural MRI had been used to assess the olfactory system in olfactory loss patients in relation to treatment of the disorder. MRI-based results indicated the high plasticity of the olfactory system. It was also demonstrated that olfactory training or treatment in individuals with olfactory deficits were accompanied by changes in the olfactory system. At a structural level, studies on olfactory loss patients with chronic rhinosinusitis have shown that improvement of olfactory function after surgical treatment was accompanied by increased OB volume (Gudziol et al. 2009), increased GMV in the primary and secondary olfactory brain regions (Whitcroft et al. 2018), as well as WM connectivity improvement in the anterior cingulate cortex and amygdala (Gullmar et al. 2017). Improvements in olfactory function (odor threshold) due to spontaneous recovery are related to the change of OB volume (Haehner et al. 2008). Besides, the “olfactory training”, i.e. systematic repeated exposure to odors, improved olfactory function and the volume of OB in patients with smell loss and was also shown to be associated with an increase in GMV (Gellrich et al. 2018). At the functional level, a 12-week “olfactory training” in a group of olfactory loss patients after upper respiratory infection helped to reestablish olfactory function, and restored the intensity of functional connectivity for the olfactory networks as well as the integrative and somatosensory networks (Kollndorfer et al. 2015a, b). In addition, olfactory training affected functional responses to odor stimulation, although brain activation may be driven by top-down processes (Pellegrino et al. 2019).
From Group Inference to Individual Prediction
Individual fMRI Biomarker for Olfactory Loss
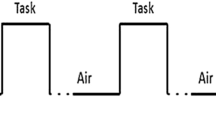
Searching for reliable brain activation patterns as a potential clinical biomarker is important for the future application of olfactory fMRI research (Frohner et al. 2019). The odor-induced fMRI signals, especially in the primary olfactory cortex, was argued to have low signal-to-noise ratio and high inter-individual variability and thus has major limitations for diagnosis and other clinical application (Morrot et al. 2013). However, a recent study found that the detectability and reproducibility of olfactory activation in the primary olfactory cortex was at the same level of that in the visual cortex (given the visual cortex activation as an ideal benchmark which produces the most robust fMRI data), and demonstrates the usefulness of this application to clinical studies as a reliable imaging tool (Lu et al. 2018). Besides, several studies reported the improvement of detectability and reproducibility of the olfactory fMRI signals in the olfactory cortex through the inclusion of short odor stimulation time (Kleinhans et al. 2019), rapid repetition time (< 1 s) during brain image acquisition (Georgiopoulos et al. 2018), or specific task protocols (e.g. synchronization of the breathing cycle with odor stimulation) (Kleinhans et al. 2019).
Currently, application of fMRI response patterns as individual “biomarker” for diagnosis of olfactory dysfunction is far from clinical routine. The principle is to have one or more stable and reliable brain activation patterns within and across individuals. Classical experimental research aims to minimize inter-individual variability by identifying robust generalizable group-level effects. For olfactory fMRI, the optimization of between-subject variance needs to consider factors such as odor selection, stimulation paradigm, or choice of contrasts for group inference. For example, passive odor exposure or active sniffing has a major influence on the BOLD signal in the primary olfactory area (Wang et al. 2014).
The intra-individual variability and stability are dependent on the regions of interest and tasks applied (Vetter et al. 2017). Moreover, research is also required to explore intra-individual reliability over time before they can be routinely applied for prediction or classification of patients with olfactory loss (Frohner et al. 2019). Ultimately, this may help in identifying paradigms, contrasts, and conditions yielding sufficiently high reliability for prediction and classification of individuals undergoing olfactory fMRI data.
Machine Learning in Olfactory Loss Research
Broadly speaking, machine learning explicitly focus on learning statistical functions using the computational strategy from multidimensional data sets to make generalizable predictions about individuals (Dwyer et al. 2018). Using MRI or fMRI data, machine learning has been used in clinical populations to identify individuals with psychiatric disorders, such as Alzheimer’s disease (Kloppel et al. 2008), depression (Fu et al. 2008), schizophrenia (Davatzikos et al. 2008), anxiety disorders (Lueken et al. 2015) and anorexia (Lavagnino et al. 2018). Using resting-state data, multivariate signatures that are valid at single-subject level could be used as biomarkers to monitor the progress of the olfactory loss or the effectiveness of treatment or training (Woo et al. 2017).
Machine learning has also been applied in different aspects of olfactory research [for a review, see Lotsch et al. (2019)]. For example, using psychophysical datasets, it was able to predict olfactory deficits and the underlying etiologies from olfactory subtest results (Lotsch et al. 2016). However, for olfaction, there has been no published paper using MRI or fMRI data involving machine learning. One barrier for this could be that the functional brain activation, even in the primary olfactory cortex, involves cognitive modulations, as discussed above. Besides, another barrier could be the small sample size and the limited number of stimulations per participant.
Summary
In this article, we have attempted to review and discuss the progress of research on human olfactory loss using MRI. To date, many studies have shown a multitude of changes in the central olfactory system following smell loss—on both functional and structural levels. However, many open questions and challenges remain which need future investigation. First, longitudinal studies focusing on the rehabilitation of olfactory functions are needed to distinguish more clearly between cause and effect of olfactory loss. Besides, research on the neural basis for specific olfactory dysfunctions (e.g. impairment regarding odor quality discrimination or identification, odor valence) could provide insights to the mechanism of some olfactory dysfunctions present in patients with certain disorders such as Parkinson’s disease or schizophrenia (Atanasova et al. 2008). Moreover, taking advantage of the close connection between brain structure and function, the joint analysis of the anatomical and functional MRI data (Hermundstad et al. 2013) will contribute to the detection of subtle reorganizations in the central olfactory system. From a clinical perspective, the establishment and validation of MRI-based biomarkers could help as a non-invasive method to achieve a better diagnosis and treatment of olfactory loss.
Change history
18 October 2019
The original version of this article unfortunately contained a mistake. The spelling of the Yoshi Akshita name was incorrect. The correct name should be Joshi Akshita The original article has been corrected.
18 October 2019
The original version of this article unfortunately contained a mistake. The spelling of the Yoshi Akshita name was incorrect. The correct name should be Joshi Akshita The original article has been corrected.
References
Albrecht J, Kopietz R, Frasnelli J, Wiesmann M, Hummel T, Lundstrom JN (2010) The neuronal correlates of intranasal trigeminal function-an ALE meta-analysis of human functional brain imaging data. Brain Res Rev 62:183–196
Arshamian A, Iannilli E, Gerber JC, Willander J, Persson J, Seo HS, Hummel T, Larsson M (2013) The functional neuroanatomy of odor evoked autobiographical memories cued by odors and words. Neuropsychologia 51:123–131
Atanasova B, Graux J, El Hage W, Hommet C, Camus V, Belzung C (2008) Olfaction: a potential cognitive marker of psychiatric disorders. Neurosci Biobehav Rev 32:1315–1325
Baba T, Kikuchi A, Hirayama K, Nishio Y, Hosokai Y, Kanno S, Hasegawa T, Sugeno N, Konno M, Suzuki K, Takahashi S, Fukuda H, Aoki M, Itoyama Y, Mori E, Takeda A (2012) Severe olfactory dysfunction is a prodromal symptom of dementia associated with Parkinson’s disease: a 3 year longitudinal study. Brain 135:161–169
Bensafi M, Porter J, Pouliot S, Mainland J, Johnson B, Zelano C, Young N, Bremner E, Aframian D, Khan R, Sobel N (2003) Olfactomotor activity during imagery mimics that during perception. Nat Neurosci 6:1142–1144
Bensafi M, Sobel N, Khan RM (2007) Hedonic-specific activity in piriform cortex during odor imagery mimics that during odor perception. J Neurophysiol 98:3254–3262
Bitter T, Bruderle J, Gudziol H, Burmeister HP, Gaser C, Guntinas-Lichius O (2010a) Gray and white matter reduction in hyposmic subjects—a voxel-based morphometry study. Brain Res 1347:42–47
Bitter T, Gudziol H, Burmeister HP, Mentzel HJ, Guntinas-Lichius O, Gaser C (2010b) Anosmia leads to a loss of gray matter in cortical brain areas. Chem Senses 35:407–415
Bramerson A, Johansson L, Ek L, Nordin S, Bende M (2004) Prevalence of olfactory dysfunction: the skovde population-based study. Laryngoscope 114:733–737
Braun JJ, Noblet V, Durand M, Scheidecker S, Zinetti-Bertschy A, Foucher J, Marion V, Muller J, Riehm S, Dollfus H, Kremer S (2014) Olfaction evaluation and correlation with brain atrophy in Bardet-Biedl syndrome. Clin Genet 86:521–529
Buschhuter D, Smitka M, Puschmann S, Gerber JC, Witt M, Abolmaali ND, Hummel T (2008) Correlation between olfactory bulb volume and olfactory function. Neuroimage 42:498–502
Campabadal A, Uribe C, Segura B, Baggio HC, Abos A, Garcia-Diaz AI, Marti MJ, Valldeoriola F, Compta Y, Bargallo N, Junque C (2017) Brain correlates of progressive olfactory loss in Parkinson’s disease. Parkinsonism Relat Disord 41:44–50
Cavanna AE, Trimble MR (2006) The precuneus: a review of its functional anatomy and behavioural correlates. Brain 129:564–583
Croy I, Hummel T (2017) Olfaction as a marker for depression. J Neurol 264:631–638
Croy I, Nordin S, Hummel T (2014) Olfactory disorders and quality of life—an updated review. Chem Senses 39:185–194
Curtis CE, D’Esposito M (2003) Persistent activity in the prefrontal cortex during working memory. Trends Cogn Sci 7:415–423
Dade LA, Zatorre RJ, Evans AC, Jones-Gotman M (2001) Working memory in another dimension: functional imaging of human olfactory working memory. Neuroimage 14:650–660
Damoiseaux JS, Rombouts SA, Barkhof F, Scheltens P, Stam CJ, Smith SM, Beckmann CF (2006) Consistent resting-state networks across healthy subjects. Proc Natl Acad Sci USA 103:13848–13853
Davatzikos C, Resnick SM, Wu X, Parmpi P, Clark CM (2008) Individual patient diagnosis of AD and FTD via high-dimensional pattern classification of MRI. Neuroimage 41:1220–1227
de Araujo IE, Rolls ET, Velazco MI, Margot C, Cayeux I (2005) Cognitive modulation of olfactory processing. Neuron 46:671–679
Djordjevic J, Zatorre RJ, Petrides M, Boyle JA, Jones-Gotman M (2005) Functional neuroimaging of odor imagery. Neuroimage 24:791–801
Dwyer DB, Falkai P, Koutsouleris N (2018) Machine learning approaches for clinical psychology and psychiatry. Annu Rev Clin Psychol 14:91–118
Erb K, Bohner G, Harms L, Goektas O, Fleiner F, Dommes E, Schmidt FA, Dahlslett B, Ludemann L (2012) Olfactory function in patients with multiple sclerosis: a diffusion tensor imaging study. J Neurol Sci 316:56–60
Erb-Eigner K, Bohner G, Goektas O, Harms L, Holinski F, Schmidt FA, Dahlslett B, Dommes E, Asbach P, Ludemann L (2014) Tract-based spatial statistics of the olfactory brain in patients with multiple sclerosis. J Neurol Sci 346:235–240
Fernandes HM, Van Hartevelt TJ, Boccard SG, Owen SL, Cabral J, Deco G, Green AL, Fitzgerald JJ, Aziz TZ, Kringelbach ML (2015) Novel fingerprinting method characterises the necessary and sufficient structural connectivity from deep brain stimulation electrodes for a successful outcome. New J Phys 17:015001
Fjaeldstad A, Fernandes HM, Van Hartevelt TJ, Gleesborg C, Moller A, Ovesen T, Kringelbach ML (2017) Brain fingerprints of olfaction: a novel structural method for assessing olfactory cortical networks in health and disease. Sci Rep 7:42534
Flohr EL, Arshamian A, Wieser MJ, Hummel C, Larsson M, Muhlberger A, Hummel T (2014) The fate of the inner nose: odor imagery in patients with olfactory loss. Neuroscience 268:118–127
Frasnelli J, Hummel T (2005) Olfactory dysfunction and daily life. Eur Arch Otorhinolaryngol 262:231–235
Frasnelli J, Fark T, Lehmann J, Gerber J, Hummel T (2013) Brain structure is changed in congenital anosmia. Neuroimage 83:1074–1080
Frohner JH, Teckentrup V, Smolka MN, Kroemer NB (2019) Addressing the reliability fallacy in fMRI: similar group effects may arise from unreliable individual effects. Neuroimage 195:174–189
Fu CH, Mourao-Miranda J, Costafreda SG, Khanna A, Marquand AF, Williams SC, Brammer MJ (2008) Pattern classification of sad facial processing: toward the development of neurobiological markers in depression. Biol Psychiatry 63:656–662
Gellrich J, Han P, Manesse C, Betz A, Junghanns A, Raue C, Schriever VA, Hummel T (2018) Brain volume changes in hyposmic patients before and after olfactory training. Laryngoscope 128:1531–1536
Georgiopoulos C, Witt ST, Haller S, Dizdar N, Zachrisson H, Engstrom M, Larsson EM (2018) Olfactory fMRI: implications of stimulation length and repetition time. Chem Senses 43:389–398
Gonzalez J, Barros-Loscertales A, Pulvermuller F, Meseguer V, Sanjuan A, Belloch V, Avila C (2006) Reading cinnamon activates olfactory brain regions. Neuroimage 32:906–912
Gottfried JA (2010) Central mechanisms of odour object perception. Nat Rev Neurosci 11:628–641
Gottfried JA, Zald DH (2005) On the scent of human olfactory orbitofrontal cortex: meta-analysis and comparison to non-human primates. Brain Res Rev 50:287–304
Gudziol V, Buschhuter D, Abolmaali N, Gerber J, Rombaux P, Hummel T (2009) Increasing olfactory bulb volume due to treatment of chronic rhinosinusitis—a longitudinal study. Brain 132:3096–3101
Gullmar D, Seeliger T, Gudziol H, Teichgraber UKM, Reichenbach JR, Guntinas-Lichius O, Bitter T (2017) Improvement of olfactory function after sinus surgery correlates with white matter properties measured by diffusion tensor imaging. Neuroscience 360:190–196
Haehner A, Hummel T, Hummel C, Sommer U, Junghanns S, Reichmann H (2007) Olfactory loss may be a first sign of idiopathic Parkinson’s disease. Mov Disord 22:839–842
Haehner A, Rodewald A, Gerber JC, Hummel T (2008) Correlation of olfactory function with changes in the volume of the human olfactory bulb. Arch Otolaryngol Head Neck Surg 134:621–624
Hagemeier J, Woodward MR, Rafique UA, Amrutkar CV, Bergsland N, Dwyer MG, Benedict R, Zivadinov R, Szigeti K (2016) Odor identification deficit in mild cognitive impairment and Alzheimer’s disease is associated with hippocampal and deep gray matter atrophy. Psychiatry Res 255:87–93
Han P, Whitcroft KL, Fischer J, Gerber J, Cuevas M, Andrews P, Hummel T (2017) Olfactory brain gray matter volume reduction in patients with chronic rhinosinusitis. Int Forum Allergy Rhinol 7:551–556
Han P, Winkler N, Hummel C, Hahner A, Gerber J, Hummel T (2018a) Alterations of brain gray matter density and olfactory bulb volume in patients with olfactory loss after traumatic brain injury. J Neurotrauma 35:2632–2640
Han P, Winkler N, Hummel C, Hahner A, Gerber J, Hummel T (2018b) Impaired brain response to odors in patients with varied severity of olfactory loss after traumatic brain injury. J Neurol 265:2322–2332
Han P, Croy I, Raue C, Bensafi M, Larsson M, Cavazzana A, Hummel T (2019) Neural processing of odor-associated words: an fMRI study in patients with acquired olfactory loss. Brain Imaging Behav. https://doi.org/10.1007/s11682-019-00062-2
Hawkes CH, Shephard BC, Daniel SE (1997) Olfactory dysfunction in Parkinson’s disease. J Neurol Neurosurg Psychiatry 62:436–446
Henkin RI, Levy LM (2002) Functional MRI of congenital hyposmia: brain activation to odors and imagination of odors and tastes. J Comput Assist Tomogr 26:39–61
Hermundstad AM, Bassett DS, Brown KS, Aminoff EM, Clewett D, Freeman S, Frithsen A, Johnson A, Tipper CM, Miller MB, Grafton ST, Carlson JM (2013) Structural foundations of resting-state and task-based functional connectivity in the human brain. Proc Natl Acad Sci USA 110:6169–6174
Hummel T, Bensafi M, Nikolaus J, Knecht M, Laing DG, Schaal B (2007) Olfactory function in children assessed with psychophysical and electrophysiological techniques. Behav Brain Res 180:133–138
Hummel T, Fliessbach K, Abele M, Okulla T, Reden J, Reichmann H, Wullner U, Haehner A (2010) Olfactory FMRI in patients with Parkinson’s disease. Front Integr Neurosci 4:125
Hummel T, Urbig A, Huart C, Duprez T, Rombaux P (2015) Volume of olfactory bulb and depth of olfactory sulcus in 378 consecutive patients with olfactory loss. J Neurol 262:1046–1051
Hummel T, Whitcroft KL, Andrews P, Altundag A, Cinghi C, Costanzo RM, Damm M, Frasnelli J, Gudziol H, Gupta N, Haehner A, Holbrook E, Hong SC, Hornung D, Huttenbrink KB, Kamel R, Kobayashi M, Konstantinidis I, Landis BN, Leopold DA, Macchi A, Miwa T, Moesges R, Mullol J, Mueller CA, Ottaviano G, Passali GC, Philpott C, Pinto JM, Ramakrishnan VJ, Rombaux P, Roth Y, Schlosser RA, Shu B, Soler G, Stjarne P, Stuck BA, Vodicka J, Welge-Luessen A (2016) Position paper on olfactory dysfunction. Rhinology 56:1–30
Iannilli E, Gerber J, Frasnelli J, Hummel T (2007) Intranasal trigeminal function in subjects with and without an intact sense of smell. Brain Res 1139:235–244
Iannilli E, Bitter T, Gudziol H, Burmeister HP, Mentzel HJ, Chopra AP, Hummel T (2011) Differences in anosmic and normosmic group in bimodal odorant perception: a functional-MRI study. Rhinology 49:458–463
Ibarretxe-Bilbao N, Junque C, Marti MJ, Valldeoriola F, Vendrell P, Bargallo N, Zarei M, Tolosa E (2010) Olfactory impairment in Parkinson’s disease and white matter abnormalities in central olfactory areas: a voxel-based diffusion tensor imaging study. Mov Disord 25:1888–1894
Jones DK, Leemans A (2011) Diffusion tensor imaging. Magn Reson Neuroimaging 711:127–144
Jones DK, Knosche TR, Turner R (2013) White matter integrity, fiber count, and other fallacies: the do’s and don’ts of diffusion MRI. Neuroimage 73:239–254
Kareken DA, Sabri M, Radnovich AJ, Claus E, Foresman B, Hector D, Hutchins GD (2004) Olfactory system activation from sniffing: effects in piriform and orbitofrontal cortex. Neuroimage 22:456–465
Karstensen HG, Vestergaard M, Baare WFC, Skimminge A, Djurhuus B, Ellefsen B, Bruggemann N, Klausen C, Leffers AM, Tommerup N, Siebner HR (2018) Congenital olfactory impairment is linked to cortical changes in prefrontal and limbic brain regions. Brain Imaging Behav 12:1569–1582
Kjelvik G, Saltvedt I, White LR, Stenumgard P, Sletvold O, Engedal K, Skatun K, Lyngvaer AK, Steffenach HA, Haberg AK (2014) The brain structural and cognitive basis of odor identification deficits in mild cognitive impairment and Alzheimer’s disease. BMC Neurol 14:168
Kleinhans NM, Reilly M, Blake M, Greco G, Sweigert J, Davis GE, Velasquez F, Reitz F, Shusterman D, Dager SR (2019) FMRI correlates of olfactory processing in typically-developing school-aged children. Psychiatry Res Neuroimaging 283:67–76
Kloppel S, Stonnington CM, Chu C, Draganski B, Scahill RI, Rohrer JD, Fox NC, Jack CR Jr, Ashburner J, Frackowiak RS (2008) Automatic classification of MR scans in Alzheimer’s disease. Brain 131:681–689
Koehler L, Fournel A, Albertowski K, Roessner V, Gerber J, Hummel C, Hummel T, Bensafi M (2018) Impaired odor perception in autism spectrum disorder is associated with decreased activity in olfactory cortex. Chem Senses 43:627–634
Kollndorfer K, Fischmeister FP, Kowalczyk K, Hoche E, Mueller CA, Trattnig S, Schopf V (2015a) Olfactory training induces changes in regional functional connectivity in patients with long-term smell loss. Neuroimage Clin 9:401–410
Kollndorfer K, Jakab A, Mueller CA, Trattnig S, Schopf V (2015b) Effects of chronic peripheral olfactory loss on functional brain networks. Neuroscience 310:589–599
Lavagnino L, Mwangi B, Cao B, Shott ME, Soares JC, Frank GKW (2018) Cortical thickness patterns as state biomarker of anorexia nervosa. Int J Eat Disord 51:241–249
Lee EY, Eslinger PJ, Du G, Kong L, Lewis MM, Huang X (2014) Olfactory-related cortical atrophy is associated with olfactory dysfunction in Parkinson’s disease. Mov Disord 29:1205–1208
Levy LM, Henkin RI, Hutter A, Lin CS, Schellinger D (1998) Mapping brain activation to odorants in patients with smell loss by functional MRI. J Comput Assist Tomogr 22:96–103
Levy LM, Henkin RI, Lin CS, Finley A (1999a) Rapid imaging of olfaction by functional MRI (fMRI): identification of presence and type of hyposmia. J Comput Assist Tomogr 23:767–775
Levy LM, Henkin RI, Lin CS, Hutter A, Schellinger D (1999b) Odor memory induces brain activation as measured by functional MRI. J Comput Assist Tomogr 23:487–498
Li W, Howard JD, Gottfried JA (2010) Disruption of odour quality coding in piriform cortex mediates olfactory deficits in Alzheimer’s disease. Brain 133:2714–2726
Lotsch J, Hummel T, Ultsch A (2016) Machine-learned pattern identification in olfactory subtest results. Sci Rep 6:35688
Lotsch J, Kringel D, Hummel T (2019) Machine learning in human olfactory research. Chem Senses 44:11–22
Lu J, Wang X, Qing Z, Li Z, Zhang W, Liu Y, Yuan L, Cheng L, Li M, Zhu B, Zhang X, Yang QX, Zhang B (2018) Detectability and reproducibility of the olfactory fMRI signal under the influence of magnetic susceptibility artifacts in the primary olfactory cortex. Neuroimage 178:613–621
Lueken U, Straube B, Yang Y, Hahn T, Beesdo-Baum K, Wittchen HU, Konrad C, Strohle A, Wittmann A, Gerlach AL, Pfleiderer B, Arolt V, Kircher T (2015) Separating depressive comorbidity from panic disorder: a combined functional magnetic resonance imaging and machine learning approach. J Affect Disord 184:182–192
Mandairon N, Linster C (2009) Odor perception and olfactory bulb plasticity in adult mammals. J Neurophysiol 101:2204–2209
Marine N, Boriana A (2014) Olfactory markers of depression and Alzheimer’s disease. Neurosci Biobehav Rev 45:262–270
Mazal PP, Haehner A, Hummel T (2016) Relation of the volume of the olfactory bulb to psychophysical measures of olfactory function. Eur Arch Otorhinolaryngol 273:1–7
McGann JP (2015) Associative learning and sensory neuroplasticity: how does it happen and what is it good for? Learn Mem 22:567–576
McGann JP (2017) Poor human olfaction is a 19th-century myth. Science 356:597
Miwa T, Furukawa M, Tsukatani T, Costanzo RM, DiNardo LJ, Reiter ER (2001) Impact of olfactory impairment on quality of life and disability. Arch Otolaryngol Head Neck Surg 127:497–503
Moberg PJ, Agrin R, Gur RE, Gur RC, Turetsky BI, Doty RL (1999) Olfactory dysfunction in schizophrenia: a qualitative and quantitative review. Neuropsychopharmacology 21:325–340
Moon WJ, Park M, Hwang M, Kim JK (2018) Functional MRI as an objective measure of olfaction deficit in patients with traumatic anosmia. AJNR Am J Neuroradiol 39:2320–2325
Morrot G, Bonny JM, Lehallier B, Zanca M (2013) fMRI of human olfaction at the individual level: interindividual variability. J Magn Reson Imaging 37:92–100
Mueller A, Abolmaali ND, Hakimi AR, Gloeckler T, Herting B, Reichmann H, Hummel T (2005a) Olfactory bulb volumes in patients with idiopathic Parkinson’s disease a pilot study. J Neural Transm 112:1363–1370
Mueller A, Rodewald A, Reden J, Gerber J, von Kummer R, Hummel T (2005b) Reduced olfactory bulb volume in post-traumatic and post-infectious olfactory dysfunction. NeuroReport 16:475–478
Murphy C, Schubert CR, Cruickshanks KJ, Klein BE, Klein R, Nondahl DM (2002) Prevalence of olfactory impairment in older adults. JAMA 288:2307–2312
Murphy C, Jernigan TL, Fennema-Notestine C (2003) Left hippocampal volume loss in Alzheimer’s disease is reflected in performance on odor identification: a structural MRI study. J Int Neuropsychol Soc 9:459–471
Murphy C, Cerf-Ducastel B, Calhoun-Haney R, Gilbert PE, Ferdon S (2005) ERP, fMRI and functional connectivity studies of brain response to odor in normal aging and Alzheimer’s disease. Chem Senses 30(Suppl 1):i170–171
Nigri A, Ferraro S, D’Incerti L, Critchley HD, Bruzzone MG, Minati L (2013) Connectivity of the amygdala, piriform, and orbitofrontal cortex during olfactory stimulation: a functional MRI study. NeuroReport 24:171–175
Olofsson JK, Gottfried JA (2015) The muted sense: neurocognitive limitations of olfactory language. Trends Cogn Sci 19:314–321
Pellegrino R, Hahner A, Bojanowski V, Hummel C, Gerber J, Hummel T (2016) Olfactory function in patients with hyposmia compared to healthy subjects—an fMRI study. Rhinology 54:374–381
Pellegrino R, Han P, Reither N, Hummel T (2019) Effectiveness of olfactory training on different severities of posttraumatic loss of smell. Laryngoscope. https://doi.org/10.1002/lary.27832
Peng P, Gu H, Xiao W, Si LF, Wang JF, Wang SK, Zhai RY, Wei YX (2013) A voxel-based morphometry study of anosmic patients. Br J Radiol 86:20130207
Plailly J, Delon-Martin C, Royet JP (2012) Experience induces functional reorganization in brain regions involved in odor imagery in perfumers. Hum Brain Mapp 33:224–234
Pomp J, Bestgen AK, Schulze P, Muller CJ, Citron FMM, Suchan B, Kuchinke L (2018) Lexical olfaction recruits olfactory orbitofrontal cortex in metaphorical and literal contexts. Brain Lang 179:11–21
Reichert JL, Schopf V (2017) Olfactory loss and regain: lessons for neuroplasticity. Neuroscientist. https://doi.org/10.1177/1073858417703910
Reichert JL, Postma EM, Smeets PAM, Boek WM, de Graaf K, Schopf V, Boesveldt S (2018) Severity of olfactory deficits is reflected in functional brain networks—an fMRI study. Hum Brain Mapp 39:3166–3177
Rolls ET (2011) Chemosensory learning in the cortex. Front Syst Neurosci 5:78
Rombaux P, Mouraux A, Bertrand B, Nicolas G, Duprez T, Hummel T (2006a) Olfactory function and olfactory bulb volume in patients with postinfectious olfactory loss. Laryngoscope 116:436–439
Rombaux P, Mouraux A, Bertrand B, Nicolas G, Duprez T, Hummel T (2006b) Retronasal and orthonasal olfactory function in relation to olfactory bulb volume in patients with posttraumatic loss of smell. Laryngoscope 116:901–905
Rombaux P, Weitz H, Mouraux A, Nicolas G, Bertrand B, Duprez T, Hummel T (2006c) Olfactory function assessed with orthonasal and retronasal testing, olfactory bulb volume, and chemosensory event-related potentials. Arch Otolaryngol Head Neck Surg 132:1346–1351
Rombaux P, Potier H, Bertrand B, Duprez T, Hummel T (2008) Olfactory bulb volume in patients with sinonasal disease. Am J Rhinol 22:598–601
Rombaux P, Potier H, Markessis E, Duprez T, Hummel T (2010) Olfactory bulb volume and depth of olfactory sulcus in patients with idiopathic olfactory loss. Eur Arch Otorhinolaryngol 267:1551–1556
Ross GW, Petrovitch H, Abbott RD, Tanner CM, Popper J, Masaki K, Launer L, White LR (2008) Association of olfactory dysfunction with risk for future Parkinson’s disease. Ann Neurol 63:167–173
Santos DV, Reiter ER, DiNardo LJ, Costanzo RM (2004) Hazardous events associated with impaired olfactory function. Arch Otolaryngol Head Neck Surg 130:317–319
Segura B, Baggio HC, Solana E, Palacios EM, Vendrell P, Bargallo N, Junque C (2013) Neuroanatomical correlates of olfactory loss in normal aged subjects. Behav Brain Res 246:148–153
Seubert J, Freiherr J, Frasnelli J, Hummel T, Lundstrom JN (2013) Orbitofrontal cortex and olfactory bulb volume predict distinct aspects of olfactory performance in healthy subjects. Cereb Cortex 23:2448–2456
Sobel N, Prabhakaran V, Desmond JE, Glover GH, Goode RL, Sullivan EV, Gabrieli JD (1998) Sniffing and smelling: separate subsystems in the human olfactory cortex. Nature 392:282–286
Sobhani S, Rahmani F, Aarabi MH, Sadr AV (2019) Exploring white matter microstructure and olfaction dysfunction in early parkinson disease: diffusion MRI reveals new insight. Brain Imaging Behav 13:210–219
Stevenson RJ (2010) An initial evaluation of the functions of human olfaction. Chem Senses 35:3–20
Su M, Wang S, Fang W, Zhu Y, Li R, Sheng K, Zou D, Han Y, Wang X, Cheng O (2015) Alterations in the limbic/paralimbic cortices of Parkinson’s disease patients with hyposmia under resting-state functional MRI by regional homogeneity and functional connectivity analysis. Parkinsonism Relat Disord 21:698–703
Takeda A, Saito N, Baba T, Kikuchi A, Sugeno N, Kobayashi M, Hasegawa T, Itoyama Y (2010) Functional imaging studies of hyposmia in Parkinson’s disease. J Neurol Sci 289:36–39
Temmel AF, Quint C, Schickinger-Fischer B, Klimek L, Stoller E, Hummel T (2002) Characteristics of olfactory disorders in relation to major causes of olfactory loss. Arch Otolaryngol Head Neck Surg 128:635–641
Tobia MJ, Yang QX, Karunanayaka P (2016) Intrinsic intranasal chemosensory brain networks shown by resting-state functional MRI. NeuroReport 27:527–531
van den Heuvel MP, Hulshoff Pol HE (2010) Exploring the brain network: a review on resting-state fMRI functional connectivity. Eur Neuropsychopharmacol 20:519–534
Van Hartevelt TJ, Kringelbach ML (2011) The olfactory system. In: Mai JK, Paxinos G (eds) The human nervous system. Academic Press, San Diego, pp 1219–1238
Vasavada MM, Wang J, Eslinger PJ, Gill DJ, Sun X, Karunanayaka P, Yang QX (2015) Olfactory cortex degeneration in Alzheimer’s disease and mild cognitive impairment. J Alzheimers Dis 45:947–958
Vasavada MM, Martinez B, Wang J, Eslinger PJ, Gill DJ, Sun X, Karunanayaka P, Yang QX (2017) Central olfactory dysfunction in Alzheimer’s disease and mild cognitive impairment: a functional MRI study. J Alzheimers Dis 59:359–368
Vennemann MM, Hummel T, Berger K (2008) The association between smoking and smell and taste impairment in the general population. J Neurol 255:1121–1126
Vetter NC, Steding J, Jurk S, Ripke S, Mennigen E, Smolka MN (2017) Reliability in adolescent fMRI within two years—a comparison of three tasks. Sci Rep 7:2287
Wang J, You H, Liu JF, Ni DF, Zhang ZX, Guan J (2011) Association of olfactory bulb volume and olfactory sulcus depth with olfactory function in patients with Parkinson disease. AJNR Am J Neuroradiol 32:677–681
Wang J, Sun X, Yang QX (2014) Methods for olfactory fMRI studies: implication of respiration. Hum Brain Mapp 35:3616–3624
Whitcroft KL, Fischer J, Han P, Raue C, Bensafi M, Gudziol V, Andrews P, Hummel T (2018) Structural plasticity of the primary and secondary olfactory cortices: increased gray matter volume following surgical treatment for chronic rhinosinusitis. Neuroscience 395:22–34
Woo CW, Chang LJ, Lindquist MA, Wager TD (2017) Building better biomarkers: brain models in translational neuroimaging. Nat Neurosci 20:365–377
Wu X, Yu C, Fan F, Zhang K, Zhu C, Wu T, Li K, Chan P (2011) Correlation between progressive changes in piriform cortex and olfactory performance in early Parkinson’s disease. Eur Neurol 66:98–105
Yoshi A, Han P, Faria V, Hummel T (Unpublished) Top-down processing of olfactory associated information in congenital anosmia: an fMRI study
Yao L, Pinto JM, Yi X, Li L, Peng P, Wei Y (2014) Gray matter volume reduction of olfactory cortices in patients with idiopathic olfactory loss. Chem Senses 39:755–760
Yao L, Yi X, Pinto JM, Yuan X, Guo Y, Liu Y, Wei Y (2018) Olfactory cortex and olfactory bulb volume alterations in patients with post-infectious olfactory loss. Brain Imaging Behav 12:1355–1362
Yoneyama N, Watanabe H, Kawabata K, Bagarinao E, Hara K, Tsuboi T, Tanaka Y, Ohdake R, Imai K, Masuda M, Hattori T, Ito M, Atsuta N, Nakamura T, Hirayama M, Maesawa S, Katsuno M, Sobue G (2018) Severe hyposmia and aberrant functional connectivity in cognitively normal Parkinson’s disease. PLoS ONE 13:e0190072
Yousem DM, Geckle RJ, Bilker WB, McKeown DA, Doty RL (1996) Posttraumatic olfactory dysfunction: MR and clinical evaluation. AJNR Am J Neuroradiol 17:1171–1179
Yousem DM, Geckle RJ, Bilker WB, Doty RL (1998) Olfactory bulb and tract and temporal lobe volumes. Normative data across decades. Ann N Y Acad Sci 855:546–555
Zelano C, Mohanty A, Gottfried JA (2011) Olfactory predictive codes and stimulus templates in piriform cortex. Neuron 72:178–187
Zhou G, Lane G, Cooper SL, Kahnt T, Zelano C (2019) Characterizing functional pathways of the human olfactory system. Elife 8:e47177
Author information
Authors and Affiliations
Corresponding author
Additional information
Handling Editor: Christoph M. Michel.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This is one of several papers published together in Brain Topography on the ‘‘Special Issue: Current Opinions in Brain Imaging Methods and Applications".
The original version of this article was revised: The spelling of the Joshi Akshita name was incorrectly published. It has been corrected.
Rights and permissions
About this article
Cite this article
Han, P., Zang, Y., Akshita, J. et al. Magnetic Resonance Imaging of Human Olfactory Dysfunction. Brain Topogr 32, 987–997 (2019). https://doi.org/10.1007/s10548-019-00729-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10548-019-00729-5